Cardiovascular Risk Prediction Models and Scores in the Era of Personalized Medicine
Abstract
:1. Introduction
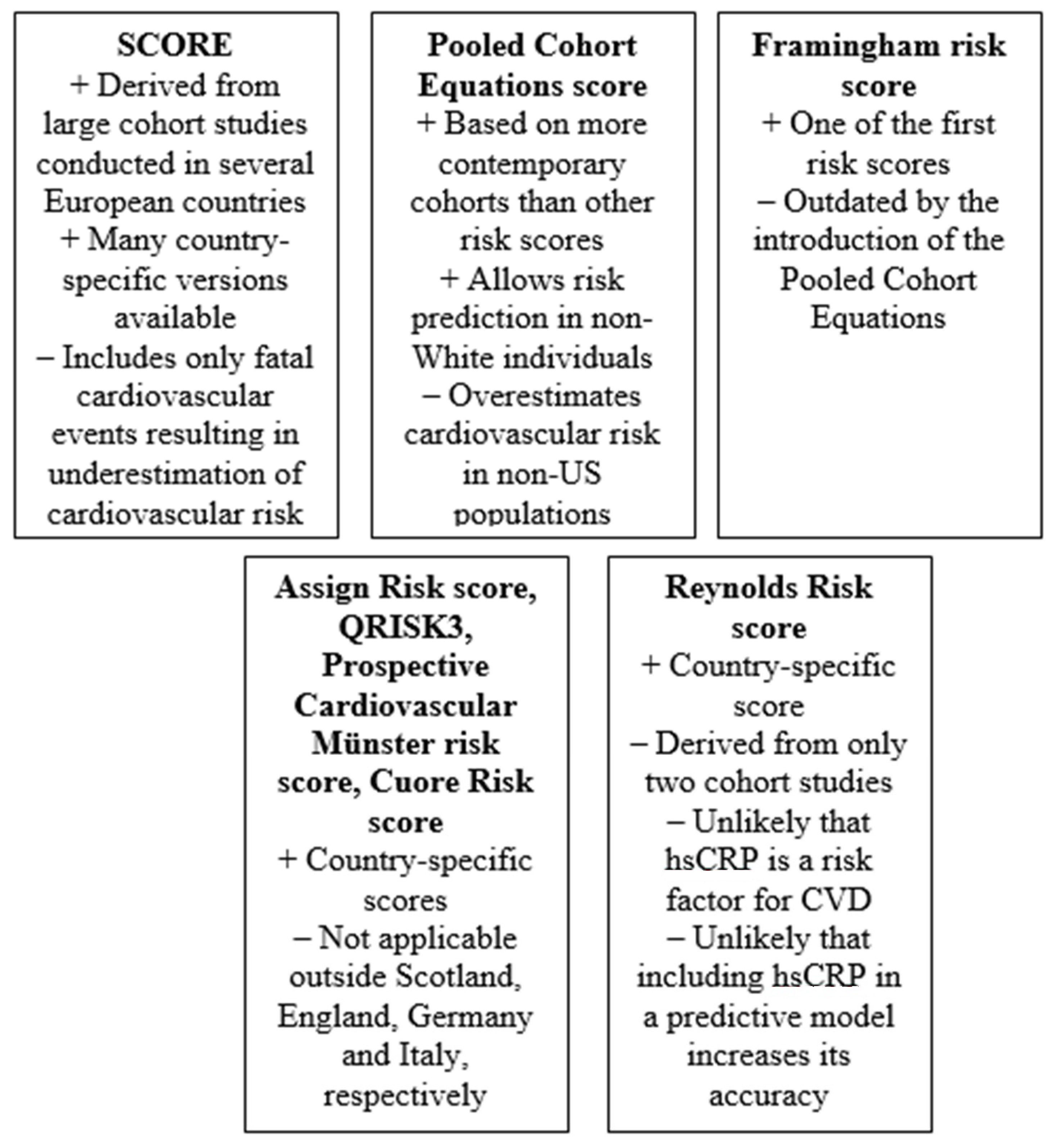
2. Systematic Coronary Risk Evaluation (SCORE)
3. Pooled Cohort Equations Calculator
4. Framingham Risk Score
5. Assign Risk Score
6. QRISK3 Score
7. Prospective Cardiovascular Münster (PROCAM) Risk Score
8. CUORE Risk Score
9. Reynolds Risk Score
10. Imaging Markers
11. Circulating Biomarkers and Genetics
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Townsend, N.; Nichols, M.; Scarborough, P.; Rayner, M. Cardiovascular disease in Europe—Epidemiological update 2015. Eur. Heart J. 2015, 36, 2696–2705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Law, M.R.; Morris, J.K.; Wald, N.J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009, 338, b1665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cholesterol Treatment Trialists’ (CTT) Collaboration; Baigent, C.; Blackwell, L.; Emberson, J.; Holland, L.E.; Reith, C.; Bhala, N.; Peto, R.; Barnes, E.H.; Keech, A.; et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010, 376, 1670–1681. [Google Scholar] [PubMed] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J. Hypertens. 2018, 36, 2284–2309. [Google Scholar] [CrossRef] [Green Version]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Conroy, R.M.; Pyörälä, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; De Backer, G.; De Bacquer, D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- Mortensen, M.B.; Falk, E. Limitations of the SCORE-guided European guidelines on cardiovascular disease prevention. Eur. Heart J. 2017, 38, 2259–2263. [Google Scholar] [CrossRef] [Green Version]
- van der Heijden, A.A.; Ortegon, M.M.; Niessen, L.W.; Nijpels, G.; Dekker, J.M. Prediction of coronary heart disease risk in a general, pre-diabetic, and diabetic population during 10 years of follow-up: Accuracy of the Framingham, SCORE, and UKPDS risk functions: The Hoorn Study. Diabetes Care 2009, 32, 2094–2098. [Google Scholar] [CrossRef] [Green Version]
- Cañón-Barroso, L.; Muro, E.C.; Herrera, N.D.; Ochoa, G.F.; Hueros, J.I.C.; Buitrago, F. Performance of the Framingham and SCORE cardiovascular risk prediction functions in a non-diabetic population of a Spanish health care centre: A validation study. Scand. J. Prim. Health Care 2010, 28, 242–248. [Google Scholar] [CrossRef]
- Sehestedt, T.; Jeppesen, J.; Hansen, T.; Rasmussen, S.; Wachtell, K.; Ibsen, H.; Torp-Pedersen, C.; Olsen, M.H. Risk stratification with the risk chart from the European Society of Hypertension compared with SCORE in the general population. J. Hypertens 2009, 27, 2351–2357. [Google Scholar] [CrossRef]
- Pandya, A.; Weinstein, M.C.; Gaziano, T.A. A comparative assessment of non-laboratory-based versus commonly used laboratory-based cardiovascular disease risk scores in the NHANES III population. PLoS ONE 2011, 6, e20416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheltens, T.; Verschuren, W.M.; Boshuizen, H.C.; Hoes, A.W.; Zuithoff, N.P.; Bots, M.L.; Grobbee, D.E. Estimation of cardiovascular risk: A comparison between the Framingham and the SCORE model in people under 60 years of age. Eur. J. Cardiovasc. Prev. Cardiol. 2008, 15, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Mainous, A.G., 3rd; Koopman, R.J.; Diaz, V.A.; Everett, C.J.; Wilson, P.W.; Tilley, B.C. A coronary heart disease risk score based on patient-reported information. Am. J. Cardiol. 2007, 99, 1236–1241. [Google Scholar] [CrossRef] [Green Version]
- Schneer, S.; Bachar, G.N.; Atar, E.; Koronowski, R.; Dicker, D. Evaluation of framingham and systematic coronary risk evaluation scores by coronary computed tomographic angiography in asymptomatic adults. Am. J. Cardiol. 2013, 111, 700–704. [Google Scholar] [CrossRef]
- Sehestedt, T.; Jeppesen, J.; Hansen, T.W.; Wachtell, K.; Ibsen, H.; Torp-Petersen, C.; Hildebrandt, P.; Olsen, M.H. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur. Heart J. 2010, 31, 883–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verweij, L.; Peters, R.J.G.; Scholte Op Reimer, W.J.M.; Boekholdt, S.M.; Luben, R.M.; Wareham, N.J.; Khaw, K.T.; Latour, C.H.M.; Jorstad, H.T. Validation of the Systematic COronary Risk Evaluation—Older Persons (SCORE-OP) in the EPIC-Norfolk prospective population study. Int. J. Cardiol. 2019, 293, 226–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll Cardiol. 2014, 63, 2935–2959. [Google Scholar] [CrossRef] [Green Version]
- The ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: Design and objectives. Am. J. Epidemiol. 1989, 129, 687–702. [Google Scholar] [CrossRef]
- Fried, L.P.; Borhani, N.O.; Enright, P.; Furberg, C.D.; Gardin, J.M.; Kronmal, R.A.; Kuller, L.H.; Manolio, T.A.; Mittelmark, M.B.; Newman, A.; et al. The Cardiovascular Health Study: Design and rationale. Ann. Epidemiol. 1991, 1, 263–276. [Google Scholar] [CrossRef]
- Friedman, G.D.; Cutter, G.R.; Donahue, R.P.; Hughes, G.H.; Hulley, S.B.; Jacobs, D.R., Jr.; Liu, K.; Savage, P.J. CARDIA: Study design, recruitment, and some characteristics of the examined subjects. J. Clin. Epidemiol. 1988, 41, 1105–1116. [Google Scholar] [CrossRef]
- Dawber, T.R.; Kannel, W.B.; Lyell, L.P. An approach to longitudinal studies in a community: The Framingham Study. Ann. N. Y. Acad. Sci. 1963, 107, 539–556. [Google Scholar] [CrossRef] [PubMed]
- Kannel, W.B.; Feinleib, M.; McNamara, P.M.; Garrison, R.J.; Castelli, W.P. An investigation of coronary heart disease in families. The Framingham offspring study. Am. J. Epidemiol. 1979, 110, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Muntner, P.; Colantonio, L.; Cushman, M.; Goff, D.C.; Howard, G.; Howard, V.J.; Kissela, B.; Levitan, E.; Lloyd-Jones, D.; Safford, M.M. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA 2014, 311, 1406–1415. [Google Scholar] [CrossRef] [PubMed]
- DeFilippis, A.P.; Young, R.; Carrubba, C.J.; McEvoy, M.J.W.; Budoff, M.J.; Blumenthal, R.S.; Kronmal, R.A.; McClelland, R.L.; Nasir, K.; Blaha, M.J. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann. Intern. Med. 2015, 162, 266–275. [Google Scholar] [CrossRef] [Green Version]
- Emdin, C.A.; Khera, A.V.; Natarajan, P.; Klarin, D.; Baber, U.; Mehran, R.; Rader, D.J.; Fuster, V.; Kathiresan, S. Evaluation of the Pooled Cohort Equations for Prediction of Cardiovascular Risk in a Contemporary Prospective Cohort. Am. J. Cardiol. 2017, 119, 881–885. [Google Scholar] [CrossRef]
- Rospleszcz, S.; Thorand, B.; Gala, T.D.L.H.; Meisinger, C.; Holle, R.; Koenig, W.; Mansmann, U.; Peters, A. Temporal trends in cardiovascular risk factors and performance of the Framingham Risk Score and the Pooled Cohort Equations. J. Epidemiol. Comm. Health 2019, 73, 19–25. [Google Scholar] [CrossRef] [Green Version]
- Mora, S.; Wenger, N.K.; Cook, N.R.; Liu, J.; Howard, B.V.; Limacher, M.C.; Liu, S.; Margolis, K.; Martin, L.W.; Paynter, N.P.; et al. Evaluation of the Pooled Cohort Risk Equations for Cardiovascular Risk Prediction in a Multiethnic Cohort from the Women’s Health Initiative. JAMA Intern. Med. 2018, 178, 1231–1240. [Google Scholar] [CrossRef]
- Nanna, M.G.; Peterson, E.D.; Wojdyla, D.; Navar, A.M. The Accuracy of Cardiovascular Pooled Cohort Risk Estimates in U.S. Older Adults. J. Gen. Intern. Med. 2019, 35, 1701–1708. [Google Scholar] [CrossRef]
- Ridker, P.M.; Cook, N.R. Statins: New American guidelines for prevention of cardiovascular disease. Lancet 2013, 382, 1762–1765. [Google Scholar] [CrossRef]
- Maddox, T.M.; Borden, W.B.; Tang, F.; Virani, S.S.; Oetgen, W.J.; Mullen, J.B.; Chan, P.S.; Casale, P.N.; Douglas, P.S.; Masoudi, F.A.; et al. Implications of the 2013 ACC/AHA cholesterol guidelines for adults in contemporary cardiovascular practice: Insights from the NCDR PINNACLE registry. J. Am. Coll. Cardiol. 2014, 64, 2183–2192. [Google Scholar] [CrossRef] [Green Version]
- DeFilippis, A.P.; Young, R.; McEvoy, J.W.; Michos, E.D.; Sandfort, V.; Kronmal, R.A.; McClelland, R.L.; Blaha, M.J. Risk score overestimation: The impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur. Heart J. 2017, 38, 598–608. [Google Scholar] [PubMed]
- Zhang, Z.; Gillespie, C.; Bowman, B.; Yang, Q. Prediction of atherosclerotic cardiovascular disease mortality in a nationally representative cohort using a set of risk factors from pooled cohort risk equations. PLoS ONE 2017, 12, e0175822. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhang, R.; Liu, G.; Liu, L.; Wang, Y.; Wang, Y. External Validation of Pooled Cohort Risk Equations to Predict 1-Year Clinical Outcome in Ischemic Stroke Patients. Med. Sci. Monit. 2017, 23, 4415–4421. [Google Scholar] [CrossRef] [Green Version]
- Topel, M.L.; Shen, J.; Morris, A.A.; Al Mheid, I.; Sher, S.; Dunbar, S.B.; Vaccarino, V.; Sperling, L.S.; Gibbons, G.H.; Martin, G.S.; et al. Comparisons of the Framingham and Pooled Cohort Equation Risk Scores for Detecting Subclinical Vascular Disease in Blacks Versus Whites. Am. J. Cardiol. 2018, 121, 564–569. [Google Scholar] [CrossRef]
- Celik, M.; Yuksel, U.C.; Yildirim, E.; Gursoy, E.; Koklu, M.; Yasar, S.; Gormel, S.; Gungor, M.; Bugan, B.; Barcin, C. The relationship between blood pressure variability and Pooled Cohort Risk Assessment Equations 10-year cardiovascular risk score. Blood Press Monit. 2016, 21, 282–287. [Google Scholar] [CrossRef]
- Nooe, A.; Edwards, M.K.; Addoh, O.; Loprinzi, P.D. Convergent validity of the ACC/AHA pooled cohort equations in associating with health-related quality of life among adults in the United States. Health Promot. Perspect. 2017, 7, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.M.; Wilson, P.W.; Odell, P.M.; Kannel, W.B. An updated coronary risk profile. A statement for health professionals. Circulation 1991, 83, 356–362. [Google Scholar] [CrossRef] [Green Version]
- Wilson, P.W.F.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of coronary heart disease using risk factor categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef] [Green Version]
- D’Agostino, R.B.S.; Grundy, S.; Sullivan, L.M.; Wilson, P.; CHD Risk Prediction Group. Validation of the Framingham Coronary Heart Disease Prediction Scores: Results of a Multiple Ethnic Groups Investigation. JAMA 2001, 286, 180–187. [Google Scholar] [CrossRef]
- D’Agostino, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham heart study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [Green Version]
- Hense, H.-W.; Schulte, H.; Löwel, H.; Assmann, G.; Keil, U. Framingham risk function overestimates risk of coronary heart disease in men and women from Germany—results from the MONICA Augsburg and the PROCAM cohorts. Eur. Heart J. 2003, 24, 937–945. [Google Scholar] [CrossRef]
- Brindle, P.; Jonathan, E.; Lampe, F.; Walker, M.; Whincup, P.; Fahey, T.; Ebrahim, S. Predictive accuracy of the Framingham coronary risk score in British men: Prospective cohort study. BMJ 2003, 327, 1267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marrugat, J.; D’Agostino, R.; Sullivan, L.; Elosua, R.; Wilson, P.; Ordovas, J.; Solanas, P.; Cordón, F.; Ramos, R.; Sala, J.; et al. An adaptation of the Framingham coronary heart disease risk function to European Mediterranean areas. J. Epidemiol. Community Health 2003, 57, 634–638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.; Hong, Y.; D’Agostino, S.R.B.; Wu, Z.; Wang, W.; Sun, J.; Wilson, P.W.F.; Kannel, W.B.; Zhao, D. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA 2004, 291, 2591–2599. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Buring, J.E.; Rifai, N.; Cook, N.R. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: The Reynolds Risk Score. JAMA 2007, 297, 611–619. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Leip, E.P.; Larson, M.; D’Agostino, R.B.; Beiser, A.; Wilson, P.W.; Wolf, P.A.; Levy, D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 2006, 113, 791–798. [Google Scholar] [CrossRef]
- Pencina, M.J.; D’Agostino, R.B.; Larson, M.G.; Massaro, J.M.; Vasan, R.S. Predicting the 30-year risk of cardiovascular disease: The Framingham Heart Study. Circulation 2009, 119, 3078–3084. [Google Scholar] [CrossRef] [Green Version]
- Tunstall-Pedoe, H.; Woodward, M.; Tavendale, R.; Brook, R.A.; McCluskey, M.K. Comparison of the prediction by 27 different factors of coronary heart disease and death in men and women of the Scottish heart health study: Cohort study. BMJ 1997, 315, 722–729. [Google Scholar] [CrossRef] [Green Version]
- Woodward, M.; Brindle, P.; Tunsfall-Pedoe, H. Adding social deprivation and family history to cardiovascular risk assessment: The ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC). Heart 2007, 93, 172–176. [Google Scholar] [CrossRef] [Green Version]
- Home—ASSIGN Score—Prioritising Prevention of Cardiovascular Disease. Available online: http://www.assign-score.com/ (accessed on 14 June 2022).
- De La Iglesia, B.; Potter, J.F.; Poulter, N.R.; Robins, M.M.; Skinner, J. Performance of the ASSIGN cardiovascular disease risk score on a UK cohort of patients from general practice. Heart 2011, 97, 491–499. [Google Scholar] [CrossRef]
- Hippisley-Cox, J.; Coupland, C.; Vinogradova, Y.; Robson, J.; May, M.; Brindle, P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: Prospective open cohort study. BMJ 2007, 335, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hippisley-Cox, J.; Coupland, C.; Brindle, P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: Prospective cohort study. BMJ 2017, 357, j2099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Department of Health. Putting Prevention First—NHS Health Check: Vascular Risk Assessment and Management Best Practice Guidance; Department of Health: London, UK, 2008.
- Thompson, I.M.; Tangen, C.M.; Goodman, P.J.; Moinpour, C.; Coltman, C.A. Erectile Dysfunction and Subsequent Cardiovascular Disease. JAMA 2005, 294, 2996–3002. [Google Scholar] [CrossRef] [Green Version]
- Shamloul, R.; Ghanem, H. Erectile dysfunction. Lancet 2013, 381, 153–165. [Google Scholar] [CrossRef]
- Kurth, T.; Winter, A.C.; Eliassen, A.H.; Dushkes, R.; Mukamal, K.J.; Rimm, E.B.; Willett, W.C.; Manson, J.E.; Rexrode, K. Migraine and risk of cardiovascular disease in women: Prospective cohort study. BMJ 2016, 353, i2610. [Google Scholar] [CrossRef] [Green Version]
- Rothwell, P.M.; Howard, S.C.; Dolan, E.; O’Brien, E.; Dobson, J.E.; Dahlöf, B.; Sever, P.S.; Poulter, N.R. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010, 375, 895–905. [Google Scholar] [CrossRef]
- Collins, G.S.; Altman, D.G. An independent and external validation of QRISK2 cardiovascular disease risk score: A prospective open cohort study. BMJ 2010, 340, c2442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, G.S.; Altman, D.G. Predicting the 10 year risk of cardiovascular disease in the United Kingdom: Independent and external validation of an updated version of QRISK2. BMJ 2012, 344, e4181. [Google Scholar] [CrossRef] [Green Version]
- Hippisley-Cox, J.; Coupland, C.; Vinogradova, Y.; Robson, J.; Minhas, R.; Sheikh, A.; Brindle, P. Predicting cardiovascular risk in England and Wales: Prospective derivation and validation of QRISK2. BMJ 2008, 336, 1475–1482. [Google Scholar] [CrossRef] [Green Version]
- Assmann, G.; Cullen, P.; Schulte, H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the Prospective Cardiovascular Münster (PROCAM) study. Circulation 2002, 105, 310–315. [Google Scholar] [CrossRef] [Green Version]
- Assmann, G.; Cullen, P.; Schulte, H. The Munster Heart Study (PROCAM). Results of follow-up at 8 years. Eur. Heart J. 1998, 19 (Suppl. A), A2–A11. [Google Scholar] [PubMed]
- Assmann, G.; Schulte, H.; Cullen, P.; Seedorf, U. Assessing risk of myocardial infarction and stroke: New data from the Prospective Cardiovascular Münster (PROCAM) study. Eur. J. Clin. Investig. 2007, 37, 925–932. [Google Scholar] [CrossRef] [PubMed]
- Giampaoli, S.; Palmieri, L.; Donfrancesco, C.; Panico, S.; Vanuzzo, D.; Pilotto, L.; Ferrario, M.; Cesana, G.; Mattiello, A.; The CUORE Project Research Group. Cardiovascular risk assessment in Italy: The CUORE Project risk score and risk chart. Ital. J. Public Health 2007, 5, 102–109. [Google Scholar]
- Ridker, P.M.; Cook, N.R.; Lee, I.-M.; Gordon, D.; Gaziano, J.M.; Manson, J.E.; Hennekens, C.H.; Buring, J.E. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N. Engl. J. Med. 2005, 352, 1293–1304. [Google Scholar] [CrossRef]
- Ridker, P.M.; Paynter, N.P.; Rifai, N.; Gaziano, J.M.; Cook, N.R. C-reactive protein and parental history improve global cardiovascular risk prediction: The Reynolds risk score for men. Circulation 2008, 118, 2243–2251. [Google Scholar] [CrossRef] [Green Version]
- C Reactive Protein Coronary Heart Disease Genetics Collaboration (CCGC). Association between C reactive protein and coronary heart disease: Mendelian randomisation analysis based on individual participant data. BMJ 2011, 342, d548. [Google Scholar] [CrossRef] [Green Version]
- Emerging Risk Factors Collaboration; Kaptoge, S.; Di Angelantonio, E.; Pennells, L.; Wood, A.M.; White, I.R.; Gao, P.; Walker, M.; Thompson, A.; Sarwar, N.; et al. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N. Engl. J. Med. 2012, 367, 1310–1320. [Google Scholar]
- Yeboah, J.; McClelland, R.L.; Polonsky, T.S.; Burke, G.L.; Sibley, C.T.; O’Leary, D.; Carr, J.; Goff, D.C.; Greenland, P.; Herrington, D.M. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012, 308, 788–795. [Google Scholar] [CrossRef] [Green Version]
- Peters, S.A.E.; Den Ruijter, H.M.; Bots, M.L.; Moons, K.G.M. Improvements in risk stratification for the occurrence of cardiovascular disease by imaging subclinical atherosclerosis: A systematic review. Heart 2012, 98, 177–184. [Google Scholar] [CrossRef]
- Nakao, Y.M.; Miyamoto, Y.; Higashi, M.; Noguchi, T.; Ohishi, M.; Kubota, I.; Tsutsui, H.; Kawasaki, T.; Furukawa, Y.; Yoshimura, M.; et al. Sex differences in impact of coronary artery calcification to predict coronary artery disease. Heart 2018, 104, 1118–1124. [Google Scholar] [CrossRef]
- Den Ruijter, H.M.; Peters, S.A.; Anderson, T.J. Common carotid intima-media thickness measurements in cardiovascular risk prediction: A meta-analysis. JAMA 2012, 308, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Ankle Brachial Index Collaboration; Fowkes, F.G.; Murray, G.D.; Butcher, I.; Heald, C.L.; Lee, R.J.; Chambless, L.E.; Folsom, A.R.; Hirsch, A.T.; Dramaix, M.; et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: A meta-analysis. JAMA 2008, 300, 197–208. [Google Scholar] [PubMed] [Green Version]
- Willeit, P.; Kaptoge, S.; Welsh, P.; Butterworth, A.S.; Chowdhury, R.; Spackman, S.A.; Pennells, L.; Gao, P.; Burgess, S.; Freitag, D.F.; et al. Natriuretic peptides and integrated risk assessment for cardiovascular disease: An individual-participant-data meta-analysis. Lancet Diabetes Endocrinol. 2016, 4, 840–849. [Google Scholar] [CrossRef] [Green Version]
- Zhu, F.; Arshi, B.; Leening, M.J.; Aribas, E.; Ikram, M.A.; Boersma, E.; Kavousi, M. Sex-Specific Added Value of Cardiac Biomarkers for 10-Year Cardiovascular Risk Prediction. Eur. J. Prev. Cardiol. 2022. [Google Scholar] [CrossRef]
- Neumann, J.T.; Riaz, M.; Bakshi, A.; Polekhina, G.; Thao, L.T.; Nelson, M.R.; Woods, R.L.; Abraham, G.; Inouye, M.; Reid, C.M.; et al. Prognostic Value of a Polygenic Risk Score for Coronary Heart Disease in Individuals Aged 70 Years and Older. Circ. Genom. Precis. Med. 2022, 15, e003429. [Google Scholar] [CrossRef]
- Elliott, J.; Bodinier, B.; Bond, T.A.; Chadeau-Hyam, M.; Evangelou, E.; Moons, K.G.M.; Dehghan, A.; Muller, D.; Elliott, P.; Tzoulaki, I. Predictive Accuracy of a Polygenic Risk Score-Enhanced Prediction Model vs a Clinical Risk Score for Coronary Artery Disease. JAMA 2020, 323, 636–645. [Google Scholar] [CrossRef]

| Risk Equation | Parameters Used to Estimate Risk | Predicted Outcome |
|---|---|---|
| Systematic Coronary Risk Evaluation | Age, sex, SBP, TC and smoking status | 10-year risk of cardiovascular mortality |
| Pooled Cohort Equations Calculator | Age, sex, SBP, treatment for hypertension, TC, HDL-C, history of T2DM and smoking status | 10-year risk of a nonfatal MI, CHD death and fatal or nonfatal stroke |
| Framingham Risk Score | Age, sex, SBP, TC, T2DM and smoking | 10-year risk of a nonfatal MI and CHD death |
| Assign risk score | Age, sex, SBP, TC, T2DM, smoking, social deprivation and family history of CVD | 10-year risk of cardiovascular events |
| QRISK3 score | Age, sex, SBP, TC/HDL-C ratio, T2DM, smoking status, ethnicity, social deprivation, body mass index, family history of CHD in a first-degree relative younger than 60 years, treated hypertension, rheumatoid arthritis, atrial fibrillation, stage 4 or 5 chronic kidney disease, migraine, corticosteroid use, systemic lupus erythematosus, treatment with atypical antipsychotic medications, severe mental illness, erectile dysfunction and variability of blood pressure | 10-year risk of cardiovascular events |
| Prospective Cardiovascular Münster risk score | Age, SBP, LDL-C, HDL-C, triglycerides, presence of T2DM, family history of MI and smoking status | 10-year risk of fatal or nonfatal CHD event |
| CUORE risk score | Age, sex, SBP, TC, HDL-C, presence of T2DM, treatment for hypertension and smoking status | 10-year risk of CHD and cerebrovascular events |
| Reynolds Risk score | Age, sex, SBP, TC, HDL-C, HbA1c if diabetic, smoking, hsCRP and parental history of MI before the age of 60 years | 10-year risk of cardiovascular events |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sofogianni, A.; Stalikas, N.; Antza, C.; Tziomalos, K. Cardiovascular Risk Prediction Models and Scores in the Era of Personalized Medicine. J. Pers. Med. 2022, 12, 1180. https://doi.org/10.3390/jpm12071180
Sofogianni A, Stalikas N, Antza C, Tziomalos K. Cardiovascular Risk Prediction Models and Scores in the Era of Personalized Medicine. Journal of Personalized Medicine. 2022; 12(7):1180. https://doi.org/10.3390/jpm12071180
Chicago/Turabian StyleSofogianni, Areti, Nikolaos Stalikas, Christina Antza, and Konstantinos Tziomalos. 2022. "Cardiovascular Risk Prediction Models and Scores in the Era of Personalized Medicine" Journal of Personalized Medicine 12, no. 7: 1180. https://doi.org/10.3390/jpm12071180
APA StyleSofogianni, A., Stalikas, N., Antza, C., & Tziomalos, K. (2022). Cardiovascular Risk Prediction Models and Scores in the Era of Personalized Medicine. Journal of Personalized Medicine, 12(7), 1180. https://doi.org/10.3390/jpm12071180







