Abstract
The aim of this study was to assess the safety and functional outcomes of excessive sagittal alignment in the unrestricted kinematic alignment technique for total knee arthroplasty (TKA). A retrospective, single-center study was conducted between 2018 and 2020, including patients undergoing primary TKA with a minimum 2-year follow-up. EOS imaging conducted before and after surgery was reviewed for overall alignment, and a number of measurements were taken, including sagittal tibial slope and other tibia and femur component positioning. Patients were interviewed and asked to fill out several questionnaires including a visual analog scale, the Oxford Knee Score, and the Knee Injury and Osteoarthritis Outcome Score. Overall, 225 patients (66.7%) had a sagittal tibial slope angle above 5° (excessive) and 112 (33.3%) patients had an angle under 5° (moderate). A significant improvement in pain and function scores was observed in both groups following the surgery (p < 0.001). There were no significant differences between the moderate and excessive groups in the average VAS, OKS or the various subtypes of the KOOS score. However, there was a slight but significant difference in the number of patients achieving MCID in KOOS symptoms. There were no cases of early failure or loosening. Unrestricted KA and the excessive sagittal alignment of the tibial component seem to be reliable and safe in terms of restoring daily function and alleviating pain after a minimum of 2 years following the surgery.
1. Introduction
Total knee arthroplasty (TKA) is considered the gold standard treatment for end-stage knee osteoarthritis [1]. During the surgery, osteoarthritic components are replaced with the aim of achieving a functional and pain-free knee. Although TKA is generally successful, dissatisfaction following TKA is a well-known phenomenon with an estimated rate of 20% following surgery [2,3,4,5,6].
In the last decade, a paramount effort was made to improve the functional outcomes and decrease the dissatisfaction rate following TKA, with the main emphasis on component alignment. Kinematic alignment (KA) was suggested as an alternative technique to traditional mechanical alignment (MA), recreating the pre-arthritic knee’s anatomical alignment with minimal soft tissue manipulation [7], thus promoting more native femur–tibia cycle gait motion.
In recent studies, the employment of KA for TKA has demonstrated promising results in terms of functional outcomes, patient satisfaction, and safety as compared to MA [8,9,10,11]. However, debates in the literature still persist regarding the proper tibial cut technique in the sagittal plane and the need to set a specific cutting limit to avoid excessive posterior tibial slope, with potential subsequent early tibial tray loosening [7,12,13].
In the last 5 years, our institution transitioned from the MA technique to caliper-based nonrestricted KA using the linked technique in which the femur and soft tissue guide the tibial cut [14]; thus, the tibial cut is performed without any restraints. The aim of this study was to evaluate the medium-term safety and patients’ functional outcomes employing this technique and to assess the clinical difference between patients with a tibial cut above and below what is considered excessive in terms of sagittal alignment.
2. Materials and Methods
A retrospective, single-center, population-based cohort study was performed between January 2018 and March 2020 to allow for a minimum 2-year follow-up. The extracted data from the hospital electronic registry included all primary TKAs performed by 3 fellowship-trained surgeons during the years the study was conducted. Revision cases, as well as valgus knee arthroplasty cases (n = 51), were excluded in this study. Electronic medical records were reviewed for patient age, body mass index (BMI), comorbidities (using the Charlson Comorbidity Index), type of anesthesia (spinal versus general), operative time and length of stay (LOS).
2.1. Technique
Starting in January 2018, our institution transitioned from mechanical axis (MA)-based TKA to calipered kinematic alignment (KA) using the linked technique, which we have previously described in detail [14]. In short, the technique involves resurfacing the femur using a conventional calipered technique, which thereafter serves as a guide to cutting the tibia in the coronal plane. Prior to performing the tibial cut, the tibial plateau is thoroughly examined for cartilage remnant. A round and flattened stylus is used as a footprint on an area of cartilage wear in the middle of the medial plateau (where the majority of contact between the femur and tibia occurs) to evaluate the plane of the native slope. A notch is made in the aforementioned orientation and the plane is recreated during the tibial cut. All surgeries were performed with a medial pivot knee design from the same manufacturer. Either cruciate-retaining or cruciate-sacrificing polyethylene was used for all surgeries. No stems or constrained implants were used.
2.2. Radiographic Analysis
The preoperative standard protocol included EOS imaging at preadmission testing (2–3 weeks from surgery) at the first follow-up visit after surgery and a two-week following hospital discharge (Figure 1). A number of measurements were performed, including the posterior tibial slope (PTS), medial proximal tibia angle (MPTA), lateral distal femoral angle (LDFA), hip–knee angle (HKA) and tibia bone resorption (TBR) [15,16]. The PTS was measured on a lateral EOS radiograph as the angle between a line perpendicular to the anterior tibial cortex and a line parallel to the tibial plateau/component [17]. Radiographic analysis was performed by 3 orthopedic residents (AE, SH, GL) who were blinded to the clinical outcome assessment. To confirm interobserver reliability, 20 overlapping cases were examined showing a correlation (kappa) of 0.88 (95% confidence interval, 0.79 to 0.96).
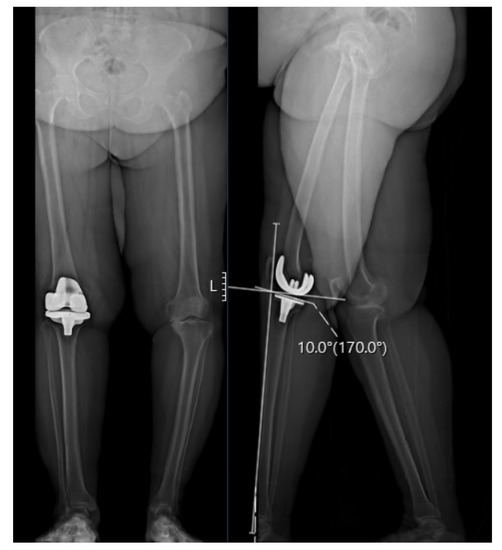
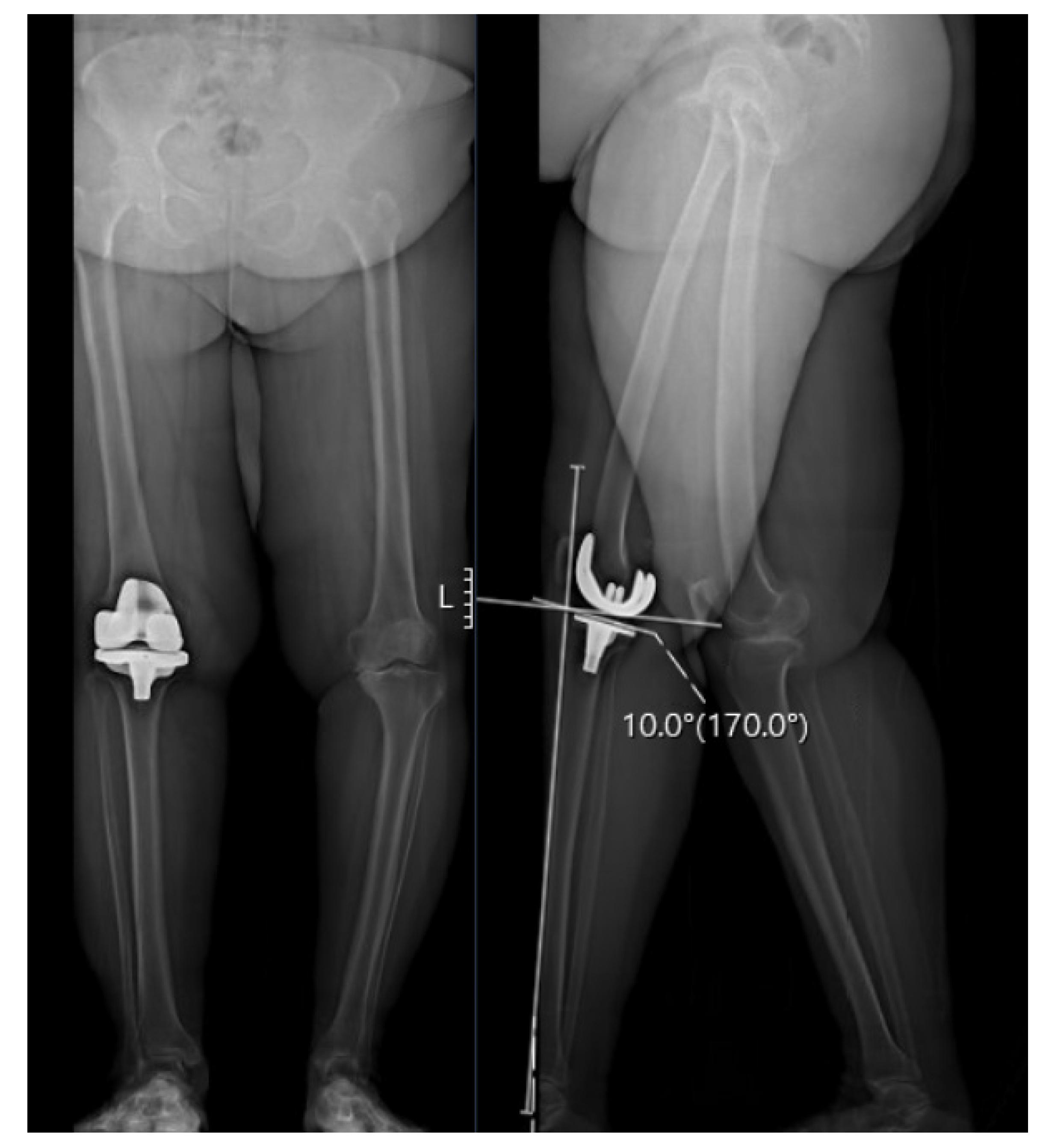
Figure 1.
A 73-year-old female with a postoperative PTS of 10°, an MPTA of 81°and an LDFA of 84°. Preoperative VAS was 9, OKS was 20 and overall KOOS was 52 (symptoms 13, pain 32, function 41 and QOL 28). Postoperative scores improved to a VAS of 2, OKS of 45, and overall KOOS of 81 (symptoms 75, pain 89, function 81 and QOL 75) at 2.4 years following surgery.
2.3. Follow-Up Examination
All patients operated on between January 2018 and March 2020 were invited to the follow-up clinic. Those who were not able to attend were phone-interviewed by 3 medical students. A number of patient-reported outcome scores were gathered, including; the visual analog scale (VAS), Oxford Knee Score (OKS), and the Knee Injury and Osteoarthritis Outcome Score (KOOS). Minimal clinical differences for OKS and KOOS were used based on the prior literature [18,19]. Patients were also asked about readmissions and reoperations associated with the operated joint. Range of motion was documented at the most recent clinic visit.
2.4. Statistical Analysis
Tibia slope tray angles on the sagittal plane were grouped into 2 categories: moderate (PTS between 0 and 5 degrees) and excessive (PTS above 5 degrees) based on prior publications indicating that 5 degrees is the upper limit for PTS [20,21,22]. Descriptive statistics were calculated for all background characteristics, univariable analysis was conducted using the Chi-square test for nominal data and interval data were analyzed with a T-test for normally distributed data (determined with the Kolmogorov–Smirnoff test) or the Man–Whitney U test (if not normally distributed). The intra- and inter-class coefficients (kappa) were calculated to evaluate the reliability and reproducibility between and within the readers. All analysis was performed using the SPSS packages (version 28.0.1).
The study protocol was approved by the institutional review board as a retrospective medical file study.
3. Results
The database search retrieved 385 patients. After excluding patients who did not meet the inclusion criteria, the study’s final cohort included 337 patients. Of these 337 patients, 112 (33.2%) had PTS between 0 and 5 degrees (moderate) and 225 patients (66.8%) had a PTS above 5 degrees (excessive). The time to follow-up was 3.47 years (SD 0.74) for the moderate group and 3.26 years (SD 0.8) for the excessive group (p = 0.02). Preoperative pain and functional questionnaires, including VAS, OKS and KOOS scores, were similar in both groups (p > 0.05). Additional demographic characteristics, comorbidities and ranges of motion are described in detail in Table 1.

Table 1.
Baseline characteristics, operative factors and patient-reported outcomes in the moderate versus excessive groups.
Patients in the moderate group had a smaller mean PTS (9.6, SD 5.4) prior to surgery compared to patients in the excessive group (11.79, SD 5.4) (p = 0.001). The average preoperative MPTA, LDFA and HKA were similar in both groups (p > 0.5) (Table 2). After surgery, the mean PTS changed to 2.87 (SD 1.8) in the moderate group and to 9.19 (SD 2.9) in the excessive group. (Table 2) In addition, mean LDFA and HKA were significantly higher in the moderate group compared to the excessive group (moderate: LDFA 85.64 SD 4.7 and HKA 2.91 SD 2.9, excessive: LDFA 84.22 SD 3.7 and HKA 1.92 SD 3.44, p < 0.05). (Table 2)

Table 2.
Preoperative and postoperative alignment in the moderate and excessive groups.
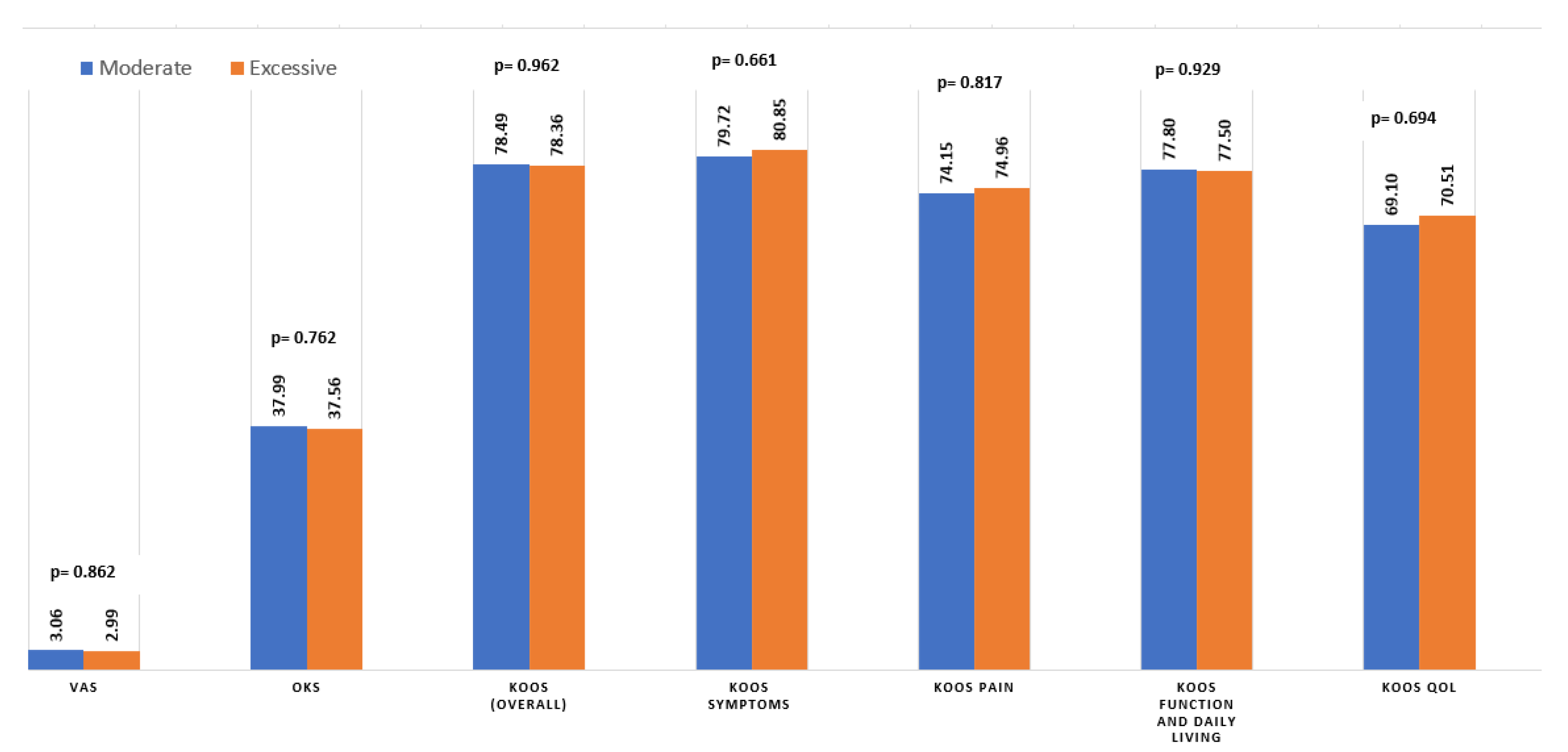
A significant improvement in pain and function scores was observed in both groups following the surgery (p < 0.001). There were no significant differences between the moderate and excessive groups in the average VAS, OKS or various subtypes of the KOOS (Figure 2). However, there was a slight but significant difference in the number of patients achieving MCID in the KOOS symptoms, as demonstrated in Table 3.
Figure 2.
Average patient-reported outcome scores in the moderate versus excessive PTS groups, postoperatively. Abbreviations: (KOOS) Knee Injury and Osteoarthritis Outcome Score; (OKS) Oxford Knee Score; (VAS) visual analog scale; (QOL) quality of life.

Table 3.
Number and percentage of patients achieving minimal clinical differences (MCID) of the Oxford Knee Score (OKS) and the Knee Injury and Osteoarthritis Outcome Score (KOOS) subcategories in the restricted versus excessive groups.
There were also no significant differences in ranges of motion between the two groups; mean extension and flexion ranged between 2.41 (SD 3.81) to 112.58 (SD 13.23) in the moderate group compared to 1.94 (SD 4.16) and 116.25 (SD 15.49) in the extensive group (p = 0.495 and 0.146 respectively).
During the study period, two patients required reoperation, one from the moderate group and one from the excessive group (0.4%, p = 0.555), due to periprosthetic joint infections. There were no cases of aseptic loosening and the TBR was 2.35 mm (SD 2.21) in the moderate group compared to 3.48 mm (SD 3.58) in the excessive group (p = 0.082). There were no cases of instability.
4. Discussion
The aim of this study was to assess the functional outcomes and the safety of the excessive sagittal alignment of the tibial component during TKA. To the best of our knowledge, this is the largest study to date to include patients with a PTS larger than 5 degrees. In this study, the employing of excessive sagittal positioning of the tibial component with a PTS above 5 degrees in the KA technique proved to be safe, with comparable objective and subjective patient satisfaction outcomes as reflected by the patient-reported outcome scores, with a mean follow-up time of 3.26 years after surgery.
An optimal prosthetic alignment is mandatory to achieve a stable and functional knee. Unlike the coronal plane alignment, the literature remains heterogenous, with no clear consensus regarding the optimal tibia slope restoration [23,24,25]. The native tibial slope varies between individuals with an average of 3–10 degrees; consequently, attempting a uniform restoration in TKA may lead to unfavorable results [26]. Singh et al., evaluating the impact of preoperative and postoperative PTS differences on postoperative knee flexion, found that a difference larger than 2 degrees in PTS restoration may lead to decreased postoperative knee flexion (<100 degrees) [26]. Catani et al., assessing the stability of tibia implants in regards to the increased difference between the preoperative and postoperative tibial slope, found a negative correlation with tibial component subsidence [27]. Adıyeke et al. compared patients with excessive (>10) and moderate (<5) PTS angles in mobile-bearing TKA and found similar long-term safety profiles and patient-reported outcomes [28]. On the contrary, Nedopil et al., evaluating eight cases of unrestricted KA in a matched case–control study, found a significant association between extreme excessive PTS (>10) and implant failure. However, this study was hindered by a very small study sample and limited confounder control [29]. Still, the literature is very limited regarding safety and patient-reported outcomes regarding native tibia slope restoration, specifically in cases requiring excessive sagittal alignment (above 5 degrees).
The calipered unrestricted KA technique employed in this study is performed using the linked technique. Prior to performing the tibial cut, the tibial plateau is thoroughly examined for cartilage remnants [30,31,32]. A round and flattened stylus is used as a footprint on an area of cartilage wear in the middle of the medial plateau to evaluate the plane of the native slope. A notch is made in the aforementioned orientation and the plane is recreated during the tibial cut. This resulted in the largest cohort to date of patients who underwent excessive sagittal alignment, as 225/337 patients (66.8%) had PTS above 5 degrees.
The findings in this study support the medium-term safety of unrestricted KA technique in general and, in particular, the employment of excessive PTS and native tibia slope restoration in TKA. Restricted KA is usually performed by setting a cutting limit within 5 degrees of the mechanical axis, and HKA must always fall within 3° of neutral in the coronal plane. As for the sagittal plane, a common 3–7-degree limit is employed [33,34]. However, there are no clear, evidence-based principles or specific criteria regarding the optimal sagittal alignment or tibia slope cutting limit present in the literature. This restriction aims to prevent the restoration of extreme outliers in anatomies to, presumably, prevent possible imbalance and early implant failure. However, according to several biomechanical studies, the tibial slope is closely related to the range of motion and patellofemoral alignment; hence, its restoration may lead to improved function and patient-reported outcomes [20,35]. This was demonstrated by Kang et al., using a computational model showing that the maximum force on the quadriceps and the patellofemoral contact stress was decreased as a function of an increased PTS, allowing the patients to feel more comfortable in terms of their knee joint range of motion [20,36]. The results of this study support the medium-term safety and functionality of native PTS restoration in the unrestricted KA technique, with no significant difference in ranges of motion between the moderate and excessive groups.
This study’s advantages include its relatively large study sample of patients with excessive PTS and the number of readers. All measurements were conducted in double-blind settings, thus minimizing the possible reader bias frequently encountered in this type of study.
Study Limitations
The study’s main limitation is related to its retrospective design and possible recall bias. The only technique employed in this study was KA; consequently, these findings cannot support the safety of excessive PTS in other techniques. Although the follow-up time was limited to 2 years at minimum, with a mean of 3.26 years for the excessive group, it still was not enough time to address and properly evaluate all possible long-term outcomes; hence, the results in this study should be considered preliminary, as a longer follow-up time is needed. Another limitation is related to the fact that all surgeries were performed using the medial pivot prosthetic design of a single manufacturer; thus, further research is needed regarding other manufacturers. Finally, all patients in this study underwent nonrestricted KA surgery, so a comparison of functional results with other alignment techniques is not applicable.
In conclusion, unrestricted KA and the excessive sagittal alignment of the tibial component seem to be reliable and safe in terms of restoring daily function and alleviating pain after a minimum of 2 years following surgery.
Author Contributions
Conceptualization, Y.B.Z. and A.E.; methodology, Y.B.Z., N.S. and A.E.; software, G.L., S.K. and A.E.; formal analysis, A.E. and N.S.; data curation, A.E., K.L., G.L., S.K., Y.B.S. and O.R.; writing—original draft preparation, A.E.; writing—review and editing, N.S. and Y.B.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of theDeclaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) ofAssaf Harofeh Medical Center (protocol code ASF-0304-19, Date 11 November 2019).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study and lack of interventions outside of standard follow-up.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical reasons.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Varacallo, M.; Luo, T.D.; Johanson, N.A. Total Knee Arthroplasty Techniques. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499896/ (accessed on 5 August 2022).
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Klit, J.; Jacobsen, S.; Rosenlund, S.; Sonne-Holm, S.; Troelsen, A. Total knee arthroplasty in younger patients evaluated by alternative outcome measures. J. Arthroplast. 2014, 29, 912–917. [Google Scholar] [CrossRef] [PubMed]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.J.K.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Scott, C.E.; Oliver, W.M.; MacDonald, D.; Wade, F.A.; Moran, M.; Breusch, S.J. Predicting dissatisfaction following total knee arthroplasty in patients under 55 years of age. Bone Jt. J. 2016, 98-B, 1625–1634. [Google Scholar] [CrossRef] [PubMed]
- Nam, D.; Nunley, R.M.; Barrack, R.L. Patient dissatisfaction following total knee replacement: A growing concern? Bone Jt. J. 2014, 96-B, 96–100. [Google Scholar] [CrossRef]
- Nisar, S.; Palan, J.; Rivière, C.; Emerton, M.; Pandit, H. Kinematic alignment in total knee arthroplasty. EFORT Open Rev. 2020, 5, 380–390. [Google Scholar] [CrossRef]
- Calliess, T.; Bauer, K.; Stukenborg-Colsman, C.; Windhagen, H.; Budde, S.; Ettinger, M. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: A prospective, randomized study. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1743–1748. [Google Scholar] [CrossRef]
- Yoon, J.R.; Han, S.B.; Jee, M.K.; Shin, Y.S. Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty: A meta-analysis. Medicine 2017, 96, e8157. [Google Scholar] [CrossRef]
- Howell, S.M.; Roth, J.D.; Hull, M.L. Kinematic Alignment in Total Knee Arthroplasty; Elsevier: Philadelphia, PA, USA, 2012. [Google Scholar]
- Sappey-Marinier, E.; Pauvert, A.; Batailler, C.; Swan, J.; Cheze, L.; Servien, E.; Lustig, S. Kinematic versus mechanical alignment for primary total knee arthroplasty with minimum 2 years follow-up: A systematic review. SICOT J. 2020, 6, 18. [Google Scholar] [CrossRef]
- Vendittoli, P.A.; Martinov, S.; Blakeney, W.G. Restricted Kinematic Alignment, the Fundamentals, and Clinical Applications. Front. Surg. 2021, 8, 697020. [Google Scholar] [CrossRef]
- Laforest, G.; Kostretzis, L.; Kiss, M.O.; Vendittoli, P.A. Restricted kinematic alignment leads to uncompromised osseointegration of cementless total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 705–712. [Google Scholar] [CrossRef] [PubMed]
- The “Linked Soft Tissue Guided Technique”: A Novel Method for Cutting the Tibia While Performing a Kinematic Femoral Alignment in Total Knee Arthroplasty-Bar-Ziv-Annals of Joint [Internet]. Available online: https://aoj.amegroups.com/article/view/5377/html (accessed on 9 May 2022).
- Paley, D. Normal Lower Limb Alignment and Joint Orientation. In Principles of Deformity Correction; Springer: Berlin/Heidelberg, Germany, 2002; pp. 1–18. [Google Scholar] [CrossRef]
- Liu, C.; Zhao, G.; Chen, K.; Lyu, J.; Chen, J.; Shi, J.; Huang, G.; Chen, F.; Wei, Y.; Wang, S.; et al. Tibial component coverage affects tibial bone resorption and patient-reported outcome measures for patients following total knee arthroplasty. J. Orthop. Surg. Res. 2021, 16, 134. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Bin, S.I.; Kim, J.M. The Correlation between Posterior Tibial Slope and Maximal Angle of Flexion after Total Knee Arthroplasty. Knee Surg. Relat. Res. 2012, 24, 158–163. [Google Scholar] [CrossRef]
- Lyman, S.; Lee, Y.Y.; McLawhorn, A.S.; Islam, W.; MacLean, C.H. What Are the Minimal and Substantial Improvements in the HOOS and KOOS and JR Versions after Total Joint Replacement? Clin. Orthop. 2018, 476, 2432–2441. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; MacDonald, D.; Simpson, A.H.R.W. The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1933–1939. [Google Scholar] [CrossRef]
- Okamoto, S.; Mizu-uchi, H.; Okazaki, K.; Hamai, S.; Nakahara, H.; Iwamoto, Y. Effect of Tibial Posterior Slope on Knee Kinematics, Quadriceps Force, and Patellofemoral Contact Force After Posterior-Stabilized Total Knee Arthroplasty. J. Arthroplast. 2015, 30, 1439–1443. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Shen, B.; Kang, P.; Yang, J.; Zhou, Z.; Pei, F. The effect of posterior tibial slope on knee flexion in posterior-stabilized total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2696–2703. [Google Scholar] [CrossRef] [PubMed]
- Kansara, D.; Markel, D.C. The effect of posterior tibial slope on range of motion after total knee arthroplasty. J. Arthroplast. 2006, 21, 809–813. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, A.V., Jr.; Berend, K.R.; Aziz-Jacobo, J.; Davis, M.B. Balancing the flexion gap: Relationship between tibial slope and posterior cruciate ligament release and correlation with range of motion. J. Bone Jt. Surg. Am. 2008, 90 (Suppl. 4), 121–132. [Google Scholar] [CrossRef] [PubMed]
- Nunley, R.M.; Nam, D.; Johnson, S.R.; Barnes, C.L. Extreme variability in posterior slope of the proximal tibia: Measurements on 2395 CT scans of patients undergoing UKA? J. Arthroplast. 2014, 29, 1677–1680. [Google Scholar] [CrossRef]
- Yoo, J.H.; Chang, C.B.; Shin, K.S.; Seong, S.C.; Kim, T.K. Anatomical references to assess the posterior tibial slope in total knee arthroplasty: A comparison of 5 anatomical axes. J. Arthroplast. 2008, 23, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Tan, J.H.; Sng, B.Y.; Awiszus, F.; Lohmann, C.H.; Nathan, S.S. Restoring the anatomical tibial slope and limb axis may maximise post-operative flexion in posterior-stabilised total knee replacements. Bone Jt. J. 2013, 95-B, 1354–1358. [Google Scholar] [CrossRef] [PubMed]
- Catani, F.; Leardini, A.; Ensini, A.; Cucca, G.; Bragonzoni, L.; Toksvig-Larsen, S.; Giannini, S. The stability of the cemented tibial component of total knee arthroplasty: Posterior cruciate-retaining versus posterior-stabilized design. J. Arthroplast. 2004, 19, 775–782. [Google Scholar] [CrossRef]
- Adıyeke, L.; Kafadar, A.B.; Erdoğan, Ö.; Gündüz, Ç.D. The effect of tibial slope angle on clinical and functional results after mobile bearing total knee arthroplasty. J. Orthop. Trauma Rehabil. 2022, 29, 22104917221075828. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. What mechanisms are associated with tibial component failure after kinematically-aligned total knee arthroplasty? Int. Orthop. 2017, 41, 1561–1569. [Google Scholar] [CrossRef]
- Ciliberti, F.K.; Cesarelli, G.; Guerrini, L.; Gunnarsson, A.E.; Forni, R.; Aubonnet, R.; Recenti, M.; Jacob, D.; Jónsson, J.H.; Cangiano, V.; et al. The role of bone mineral density and cartilage volume to predict knee cartilage degeneration. Eur. J. Transl. Myol. 2022, 32, 10678. [Google Scholar] [CrossRef] [PubMed]
- Ciliberti, F.K.; Guerrini, L.; Gunnarsson, A.E.; Recenti, M.; Jacob, D.; Cangiano, V.; Tesfahunegn, Y.A.; Islind, A.S.; Tortorella, F.; Tsirilaki, M.; et al. CT- and MRI-Based 3D Reconstruction of Knee Joint to Assess Cartilage and Bone. Diagnostics. 2022, 12, 279. [Google Scholar] [CrossRef]
- Recenti, M.; Ricciardi, C.; Edmunds, K.; Gislason, M.K.; Gargiulo, P. Machine learning predictive system based upon radiodensitometric distributions from mid-thigh CT images. Eur. J. Transl. Myol. 2020, 30, 8892. [Google Scholar] [CrossRef]
- Brooks, P. Seven cuts to the perfect total knee. Orthopedics 2009, 32, e1000642. [Google Scholar] [CrossRef]
- Matsumoto, T.; Takayama, K.; Ishida, K.; Hayashi, S.; Hashimoto, S.; Kuroda, R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Jt. J. 2017, 99, 640–646. [Google Scholar] [CrossRef]
- Chambers, A.W.; Wood, A.R.; Kosmopoulos, V.; Sanchez, H.B.; Wagner, R.A. Effect of posterior tibial slope on flexion and anterior-posterior tibial translation in posterior cruciate-retaining total knee arthroplasty. J. Arthroplast. 2016, 31, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.T.; Kwon, S.K.; Son, J.; Kwon, O.R.; Lee, J.S.; Koh, Y.G. The increase in posterior tibial slope provides a positive biomechanical effect in posterior-stabilized total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3188–3195. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).