Multimorbidity in Difficult Asthma: The Need for Personalised and Non-Pharmacological Approaches to Address a Difficult Breathing Syndrome
Abstract
1. Introduction
- The challenging case of Mrs T: when the best clinical practice fails to lead to the best clinical outcomes for a patient with difficult-to-treat asthma.
1.1. Difficult-to-Treat Asthma in Context
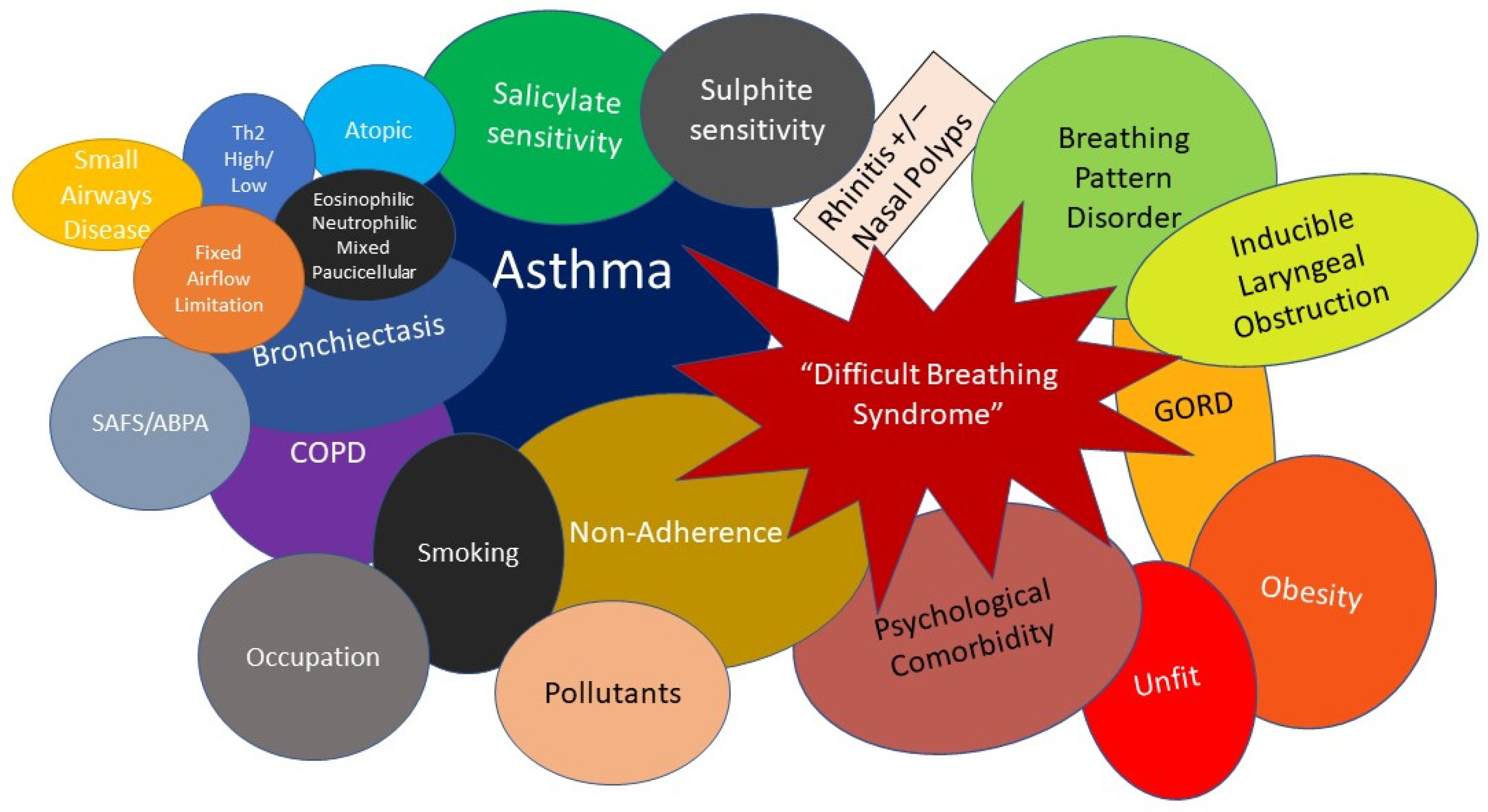
1.2. Difficult Asthma as Part of a Multimorbidity Difficult Breathing Syndrome—The Concept of Treatable Traits
1.3. Structured Multi-Disciplinary Team Approaches to Difficult Asthma Care
1.4. The MDT Components of Specialist Difficult Asthma Care
2. Review Methods
3. Non-Pharmacological Approaches to Extrapulmonary and Behavioural Traits within the Difficult Breathing Syndrome
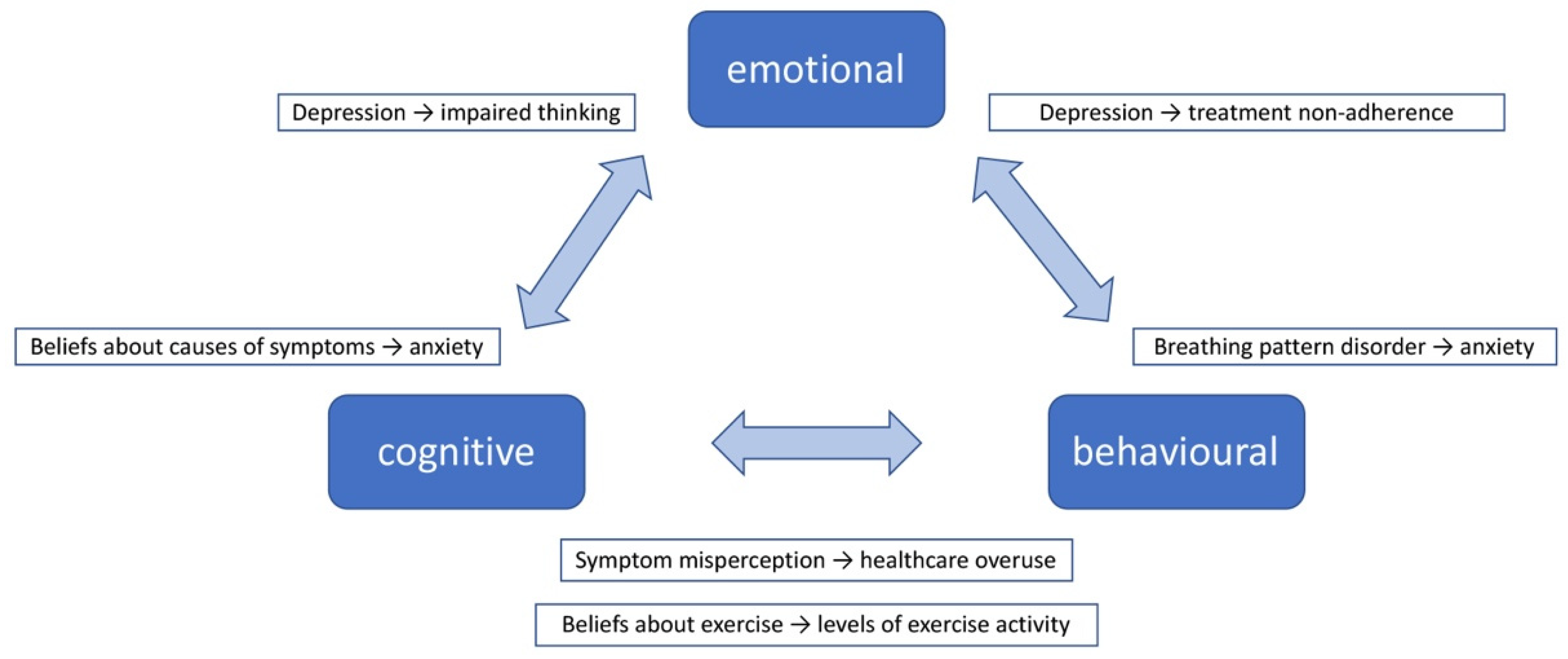
3.1. Biopsychosocial Processes in DBS
3.1.1. Emotion-Focused Approaches
3.1.2. Behavioural Approaches
3.1.3. Educational Approaches
3.1.4. Interventions Combining Emotion-Focused, Behavioural and Educational Approaches
3.1.5. Other Non-Pharmacological Approaches
3.1.6. Telehealth
- How did we use current best practice in the treatment of Mrs T?
4. What Can We Learn from Multimorbidity Research for the Clinical Management of People Living with DBS?
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- The Global Asthma Report 2018. Available online: http://globalasthmareport.org/resources/resources.php (accessed on 1 August 2021).
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2021. Available online: www.ginasthma.org (accessed on 1 August 2021).
- Israel, E.; Reddel, H.K. Severe and Difficult-to-Treat Asthma in Adults. N. Engl. J. Med. 2017, 377, 965–976. [Google Scholar] [CrossRef] [PubMed]
- World Allergy Organization: The Management of Severe Asthma. Economic Analysis of the Cost of Treatments for Severe Asthma. Available online: https://www.worldallergy.org/educational_programs/world_allergy_forum/anaheim2005/blaiss.php (accessed on 1 August 2021).
- Woodruff, P.G.; Modrek, B.; Choy, D.F.; Jia, G.; Abbas, A.R.; Ellwanger, A.; Arron, J.R.; Koth, L.L.; Fahy, J.V. T-helper Type 2–driven Inflammation Defines Major Subphenotypes of Asthma. Am. J. Respir. Crit Care Med. 2009, 180, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Fong, W.C.G.; Azim, A.; Knight, D.; Mistry, H.; Freeman, A.; Felongco, M.; Kyyaly, A.; Harvey, M.; Dennison, P.; Zhang, H.; et al. Real-world Omalizumab and Mepolizumab treated difficult asthma phenotypes and their clinical outcomes. Clin. Exp. Allergy 2021, 51, 1019–1032. [Google Scholar] [CrossRef] [PubMed]
- Heaney, L.G.; Perez de Llano, L.; Al-Ahmad, M.; Backer, V.; Busby, J.; Canonica, G.W.; Christoff, G.C.; Cosio, B.G.; FitzGerald, J.M.; Heffler, E.; et al. Eosinophilic and Noneosinophilic Asthma: An Expert Consensus Framework to Characterize Phenotypes in a Global Real-Life Severe Asthma Cohort. Chest 2021, 160, 814–830. [Google Scholar] [CrossRef] [PubMed]
- Azim, A.; Newell, C.; Barber, C.; Harvey, M.; Knight, D.; Freeman, A.; Fong, W.C.G.; Dennison, P.; Haitchi, H.M.; Djukanovic, R.; et al. Clinical evaluation of type 2 disease status in a real-world population of difficult to manage asthma using historic electronic healthcare records of blood eosinophil counts. Clin. Exp. Allergy 2021, 51, 811–820. [Google Scholar] [CrossRef] [PubMed]
- GINA: Global Initiative for Asthma Pocket Guide For Health Professionals: Difficult to Treat and Severe Asthma in Adolescent and Adult Patients: Diagnosis and Management. 2019. Available online: https://ginasthma.org/wp-content/uploads/2019/04/GINA-Severe-asthma-Pocket-Guide-v2.0-wms-1.pdf (accessed on 1 August 2022).
- Asthma UK. Living in Limbo: The Scale of Unmet Need in Difficult and Severe Asthma; Asthma UK: London, UK, 2019. [Google Scholar]
- O’Neill, S.; Sweeney, J.; Patterson, C.C.; Menzies-Gow, A.; Niven, R.; Mansur, A.H.; Bucknall, C.; Chaudhuri, R.; Thomson, N.C.; Brightling, C.E.; et al. The cost of treating severe refractory asthma in the UK: An economic analysis from the British Thoracic Society Difficult Asthma Registry. Thorax 2015, 70, 376–378. [Google Scholar] [CrossRef]
- Tay, T.R.; Hew, M. Comorbid “treatable traits” in difficult asthma: Current evidence and clinical evaluation. Allergy 2018, 73, 1369–1382. [Google Scholar] [CrossRef]
- Tay, T.R.; Radhakrishna, N.; Hore-Lacy, F.; Smith, C.; Hoy, R.; Dabscheck, E.; Hew, M. Comorbidities in difficult asthma are independent risk factors for frequent exacerbations, poor control and diminished quality of life. Respirology 2016, 21, 1384–1390. [Google Scholar] [CrossRef]
- Chung, K.F.; Wenzel, S.E.; Brozek, J.L.; Bush, A.; Castro, M.; Sterk, P.J.; Adcock, I.M.; Bateman, E.D.; Bel, E.H.; Bleecker, E.R.; et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur. Respir. J. 2014, 43, 343–373. [Google Scholar] [CrossRef]
- von Bülow, A.; Backer, V.; Bodtger, U.; Søes-Petersen, N.U.; Vest, S.; Steffensen, I.; Porsbjerg, C. Differentiation of adult severe asthma from difficult-to-treat asthma—Outcomes of a systematic assessment protocol. Respir. Med. 2018, 145, 41–47. [Google Scholar] [CrossRef]
- Hekking, P.W.; Wener, R.R.; Amelink, M.; Zwinderman, A.H.; Bouvy, M.L.; Bel, E.H. The prevalence of severe refractory asthma. J. Allergy Clin. Immunol. 2015, 135, 896–902. [Google Scholar] [CrossRef]
- Pavord, I.D.; Beasley, R.; Agusti, A.; Anderson, G.P.; Bel, E.; Brusselle, G.; Cullinan, P.; Custovic, A.; Ducharme, F.M.; Fahy, J.V.; et al. After asthma: Redefining airways diseases. Lancet 2018, 391, 350–400. [Google Scholar] [CrossRef]
- Agusti, A.; Bel, E.; Thomas, M.; Vogelmeier, C.; Brusselle, G.; Holgate, S.; Humbert, M.; Jones, P.; Gibson, P.G.; Vestbo, J.; et al. Treatable traits: Toward precision medicine of chronic airway diseases. Eur. Respir. J. 2016, 47, 410–419. [Google Scholar] [CrossRef]
- Freitas, P.D.; Xavier, R.F.; McDonald, V.M.; Gibson, P.G.; Cordova-Rivera, L.; Furlanetto, K.C.; de Oliveira, J.M.; Carvalho-Pinto, R.M.; Cukier, A.; Stelmach, R.; et al. Identification of asthma phenotypes based on extrapulmonary treatable traits. Eur. Respir. J. 2021, 57, 2000240. [Google Scholar] [CrossRef]
- McDonald, V.M.; Hiles, S.A.; Godbout, K.; Harvey, E.S.; Marks, G.B.; Hew, M.; Peters, M.; Bardin, P.G.; Reynolds, P.N.; Upham, J.W.; et al. Treatable traits can be identified in a severe asthma registry and predict future exacerbations. Respirology 2019, 24, 37–47. [Google Scholar] [CrossRef]
- Simpson, A.J.; Hekking, P.P.; Shaw, D.E.; Fleming, L.J.; Roberts, G.; Riley, J.H.; Bates, S.; Sousa, A.R.; Bansal, A.T.; Pandis, I.; et al. Treatable traits in the European U-BIOPRED adult asthma cohorts. Allergy 2019, 74, 406. [Google Scholar] [CrossRef]
- Poitras, M.-E.; Maltais, M.-E.; Bestard-Denommé, L.; Stewart, M.; Fortin, M. What are the effective elements in patient-centered and multimorbidity care? A scoping review. BMC Health Serv. Res. 2018, 18, 446. [Google Scholar] [CrossRef]
- Kenning, C.; Coventry, P.A.; Bower, P. Self-management interventions in patients with long-term conditions: A structured review of approaches to reporting inclusion, assessment, and outcomes in multimorbidity. J. Comorbidity 2014, 4, 37–45. [Google Scholar] [CrossRef]
- Xu, X.; Mishra, G.D.; Jones, M. Evidence on multimorbidity from definition to intervention: An overview of systematic reviews. Ageing Res. Rev. 2017, 37, 53–68. [Google Scholar] [CrossRef]
- Albreht, T.; Dyakova, M.; Schellevis, F.G.; Van den Broucke, S. Many diseases, one model of care? J. Comorbidity 2016, 6, 12–20. [Google Scholar] [CrossRef]
- Tay, T.R.; Lee, J.; Radhakrishna, N.; Hore-Lacy, F.; Stirling, R.; Hoy, R.; Dabscheck, E.; O’Hehir, R.; Hew, M. A Structured Approach to Specialist-referred Difficult Asthma Patients Improves Control of Comorbidities and Enhances Asthma Outcomes. J. Allergy Clin. Immunol. Pract. 2017, 5, 956–964. [Google Scholar] [CrossRef]
- McDonald, V.M.; Clark, V.L.; Cordova-Rivera, L.; Wark, P.A.B.; Baines, K.J.; Gibson, P.G. Targeting treatable traits in severe asthma: A randomised controlled trial. Eur. Respir. J. 2020, 55, 1901509. [Google Scholar] [CrossRef]
- Azim, A.; Mistry, H.; Freeman, A.; Barber, C.; Newell, C.; Gove, K.; Thirlwall, Y.; Harvey, M.; Bentley, K.; Knight, D.; et al. Protocol for the Wessex AsThma CoHort of difficult asthma (WATCH): A pragmatic real-life longitudinal study of difficult asthma in the clinic. BMC Pulm. Med. 2019, 19, 99. [Google Scholar] [CrossRef] [PubMed]
- Azim, A.; Freeman, A.; Lavenu, A.; Mistry, H.; Haitchi, H.M.; Newell, C.; Cheng, Y.; Thirlwall, Y.; Harvey, M.; Barber, C.; et al. New Perspectives on Difficult Asthma; Sex and Age of Asthma-Onset Based Phenotypes. J. Allergy Clin. Immunol. Pract. 2020, 8, 3396–3406. [Google Scholar] [CrossRef] [PubMed]
- NHS Specialised Respiratory Services (Adult)—Severe Asthma. Available online: https://www.england.nhs.uk/publication/specialised-respiratory-services-adult-severe-asthma/ (accessed on 1 August 2021).
- Gibeon, D.; Heaney, L.G.; Brightling, C.E.; Niven, R.; Mansur, A.H.; Chaudhuri, R.; Bucknall, C.E.; Menzies-Gow, A.N. Dedicated Severe Asthma Services Improve Health-care Use and Quality of Life. Chest 2015, 148, 870–876. [Google Scholar] [CrossRef] [PubMed]
- Denton, E.; Lee, J.; Tay, T.R.; Radhakrishna, N.; Hore-Lacy, F.; Mackay, A.; Hoy, R.; Dabscheck, E.; O’Hehir, R.E.; Hew, M. Systematic Assessment for Difficult and Severe Asthma Improves Outcomes and Halves Oral Corticosteroid Burden Independent of Monoclonal Biologic Use. J. Allergy Clin. Immunol. Pract. 2020, 8, 1616–1624. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.; Murphy, A.; Stallberg, B.; Baxter, N.; Heaney, L.G. ‘SIMPLES’: A structured primary care approach to adults with difficult asthma. Prim. Care Respir. J. 2013, 22, 365–373. [Google Scholar] [CrossRef]
- Maltby, S.; Gibson, P.G.; Reddel, H.K.; Smith, L.; Wark, P.A.B.; King, G.G.; Upham, J.W.; Clark, V.L.; Hew, M.; Owens, L.; et al. Severe Asthma Toolkit: An online resource for multidisciplinary health professionals—needs assessment, development process and user analytics with survey feedback. BMJ Open 2020, 10, e032877. [Google Scholar] [CrossRef]
- Hew, M.; Menzies-Gow, A.; Hull, J.H.; Fleming, L.; Porsbjerg, C.; Brinke, A.T.; Allen, D.; Gore, R.; Tay, T.R. Systematic Assessment of Difficult-to-Treat Asthma: Principles and Perspectives. J Allergy Clin Immunol Pract. 2020, 7, 2222–2233. [Google Scholar] [CrossRef]
- McDonald, V.M.; Vertigan, A.E.; Gibson, P.G. How to set up a severe asthma service. Respirology 2011, 16, 900–911. [Google Scholar] [CrossRef]
- McDonald, V.M.; Harrington, J.; Clark, V.L.; Gibson, P.G. Multidisciplinary care in chronic airway diseases: The Newcastle model. ERJ Open Res. 2022, 15, 00215–2022. [Google Scholar] [CrossRef]
- Smith, S.M.; Wallace, E.; Clyne, B.; Boland, F.; Fortin, M. Interventions for improving outcomes in patients with multimorbidity in primary care and community setting: A systematic review. Syst. Rev. 2021, 10, 271. [Google Scholar] [CrossRef]
- Stoll, C.R.T.; Izadi, S.; Fowler, S.; Philpott-Streiff, S.; Green, P.; Suls, J.; Winter, A.C.; Colditz, G.A. Multimorbidity in randomized controlled trials of behavioral interventions: A systematic review. Health Psychol. 2019, 38, 831–839. [Google Scholar] [CrossRef]
- Yii, A.C.A.; Koh, M.S. A review of psychological dysfunction in asthma: Affective, behavioral and cognitive factors. J. Asthma 2013, 50, 915–921. [Google Scholar] [CrossRef]
- Caulfield, J.I. Anxiety, depression, and asthma: New perspectives and approaches for psychoneuroimmunology research. Brain, Behav. Immun.—Health 2021, 18, 100360. [Google Scholar] [CrossRef]
- Ye, G.; Baldwin, D.S.; Hou, R. Anxiety in asthma: A systematic review and meta-analysis. Psychol. Med. 2021, 51, 11–20. [Google Scholar] [CrossRef]
- Vinkers, C.H.; Kuzminskaite, E.; Lamers, F.; Giltay, E.J.; Penninx, B.W.J.H. An integrated approach to understand biological stress system dysregulation across depressive and anxiety disorders. J. Affect. Disord. 2021, 283, 139–146. [Google Scholar] [CrossRef]
- Zhang, L.; Zhang, X.; Zheng, J.; Liu, Y.; Wang, J.; Wang, G.; Zhang, H.P.; Kang, D.Y.; Peng, Z.G.; Ji, Y.L.; et al. Depressive symptom-associated IL-1β and TNF-α release correlates with impaired bronchodilator response and neutrophilic airway inflammation in asthma. Clin. Exp. Allergy 2019, 49, 770–780. [Google Scholar] [CrossRef]
- Roohi, E.; Jaafari, N.; Hashemian, F. On inflammatory hypothesis of depression: What is the role of IL-6 in the middle of the chaos? J. Neuroinflamm. 2021, 18, 45. [Google Scholar] [CrossRef]
- Van Lieshout, R.J.; MacQueen, G. Psychological Factors in Asthma. Allergy Asthma Clin. Immunol. 2008, 4, 12. [Google Scholar] [CrossRef]
- Gao, X.; Xiao, Y.; Lv, P.; Zhang, W.; Gong, Y.; Wang, T.; Gong, Q.; Ji, Y.; Lui, S. Altered brain network integrity in patients with asthma: A structural connectomic diffusion tensor imaging study. Respir. Physiol. Neurobiol. 2019, 266, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Se, E.; Hopkins, C.; Clark, A.; Anari, S.; Robertson, A.; Sunkaraneni, S.; Ja, W.; Beezhold, J.; Cm, P.; Erskine, S.E. Chronic rhinosinusitis and mood disturbance. Rhinology 2017, 55, 113–119. [Google Scholar] [CrossRef]
- Bedolla-Barajas, M.; Morales-Romero, J.; Fonseca-López, J.C.; Pulido-Guillén, N.A.; Larenas-Linnemann, D.; Hernández-Colín, D.D. Anxiety and depression in adult patients with asthma: The role of asthma control, obesity and allergic sensitization. J. Asthma 2020, 58, 1058–1066. [Google Scholar] [CrossRef] [PubMed]
- Labor, M.; Labor, S.; Jurić, I.; Fijačko, V.; Grle, S.P.; Plavec, D. Mood disorders in adult asthma phenotypes. J. Asthma 2018, 55, 57–65. [Google Scholar] [CrossRef]
- Stanescu, S.; Kirby, S.E.; Thomas, M.; Yardley, L.; Ainsworth, B. A systematic review of psychological, physical health factors, and quality of life in adult asthma. NPJ Prim. Care Respir. Med. 2019, 29, 37. [Google Scholar] [CrossRef]
- Lin, H.; Xiao, S.; Shi, L.; Zheng, X.; Xue, Y.; Yun, Q.; Ouyang, P.; Wang, D.; Zhu, H.; Zhang, C. Impact of Multimorbidity on Symptoms of Depression, Anxiety, and Stress in Older Adults: Is There a Sex Difference? Front. Psychol. 2021, 12, 5904. [Google Scholar] [CrossRef]
- Birk, J.L.; Kronish, I.M.; Moise, N.; Falzon, L.; Yoon, S.; Davidson, K.W. Depression and multimorbidity: Considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychol. 2019, 38, 802. [Google Scholar] [CrossRef]
- Heaney, L.G.; Conway, E.; Kelly, C.; Gamble, J. Prevalence of psychiatric morbidity in a difficult asthma population: Relationship to asthma outcome. Respir. Med. 2005, 99, 1152–1159. [Google Scholar] [CrossRef]
- Thomas, M.; Bruton, A.; Moffatt, M.; Cleland, J. Asthma and psychological dysfunction. Nat. Publ. Gr. 2011, 20, 250–256. [Google Scholar] [CrossRef]
- De Carvalho-Pinto, R.M.; Cukier, A.; Angelini, L.; Antonangelo, L.; Mauad, T.; Dolhnikoff, M.; Rabe, K.F.; Stelmach, R. Clinical characteristics and possible phenotypes of an adult severe asthma population. Respir. Med. 2012, 106, 47–56. [Google Scholar] [CrossRef]
- Yorke, J.; Fleming, S.L.; Shuldham, C. Psychological interventions for adults with asthma. Cochrane Database Syst. Rev. 2006, 1, CD002982. [Google Scholar] [CrossRef]
- Yorke, J.; Fleming, S.; Shuldham, C.; Rao, H.; Smith, H.E. Nonpharmacological interventions aimed at modifying health and behavioural outcomes for adults with asthma: A critical review. Clin. Exp. Allergy 2015, 45, 1750–1764. [Google Scholar] [CrossRef]
- Cooley, C.; Park, Y.; Ajilore, O.; Leow, A.; Nyenhuis, S.M. Impact of interventions targeting anxiety and depression in adults with asthma. J. Asthma 2020, 59, 273–287. [Google Scholar] [CrossRef]
- Beck, A.T. A 60-Year Evolution of Cognitive Theory and Therapy. Perspect. Psychol. Sci. 2019, 14, 16–20. [Google Scholar] [CrossRef]
- Brent, D.A.; Kolko, D.J. Psychotherapy: Definitions, mechanisms of action, and relationship to etiological models. J. Abnorm. Child Psychol. 1998, 26, 17–25. [Google Scholar] [CrossRef]
- Ainsworth, B.; Patel, A.; Eyles, C.; Davies, G.E.; Kurukulaaratchy, R.; Thomas, M. Feasibility and Acceptability of a Group Mindfulness Intervention in a Difficult Asthma Clinic. Mindfulness 2020, 11, 1734–1746. [Google Scholar] [CrossRef]
- Brown, E.S.; Vigil, L.; Khan, D.A.; Liggin, J.D.M.; Carmody, T.J.; Rush, A.J. A Randomized Trial of Citalopram versus Placebo in Outpatients with Asthma and Major Depressive Disorder: A Proof of Concept Study. Biol. Psychiatry 2005, 58, 865–870. [Google Scholar] [CrossRef]
- Bardin, P.G.; Rangaswamy, J.; Yo, S.W. Managing comorbid conditions in severe asthma. Med. J. Aust. 2018, 209, S11–S17.e3. [Google Scholar] [CrossRef]
- Freeman, A.; Cellura, D.; Minnion, M.; Fernandez, B.O.; Spalluto, C.M.; Levett, D.; Bates, A.; Wallis, T.; Watson, A.; Jack, S.; et al. Exercise Training Induces a Shift in Extracellular Redox Status with Alterations in the Pulmonary and Systemic Redox Landscape in Asthma. Antioxidants 2021, 10, 1926. [Google Scholar] [CrossRef]
- Juel, C.T.B.; Ali, Z.; Nilas, L.; Ulrik, C.S. Asthma and obesity: Does weight loss improve asthma control? a systematic review. J. Asthma Allergy 2012, 5, 21. [Google Scholar] [CrossRef]
- Dias-Júnior, S.A.; Reis, M.; De Carvalho-Pinto, R.M.; Stelmach, R.; Halpern, A.; Cukier, A. Effects of weight loss on asthma control in obese patients with severe asthma. Eur. Respir. J. 2014, 43, 1368–1377. [Google Scholar] [CrossRef]
- Eneli, I.U.; Skybo, T.; Camargo, C.A. Weight loss and asthma: A systematic review. Thorax 2008, 63, 671–676. [Google Scholar] [CrossRef]
- Okoniewski, W.; Lu, K.D.; Forno, E. Weight loss for children and adults with obesity and asthma a systematic review of randomized controlled trials. Ann. Am. Thorac. Soc. 2019, 16, 613–625. [Google Scholar] [CrossRef]
- Adeniyi, F.B.; Young, T. Weight loss interventions for chronic asthma. Cochrane Database Syst. Rev. 2012, 7, CD009339. [Google Scholar] [CrossRef] [PubMed]
- Nyenhuis, S.; Dixon, A.E.; Ma, J. Impact of Lifestyle Interventions Targeting Healthy Diet, Physical Activity and Weight Loss on Asthma in Adults: What is the evidence? J. Allergy Clin. Immunol. Pract. 2018, 6, 751–763. [Google Scholar] [CrossRef] [PubMed]
- Scott, H.A.; Wood, L.G.; Williams, E.J.; Weaver, N.; Upham, J.W. Comparing the Effect of Acute Moderate and Vigorous Exercise on Inflammation in Adults with Asthma: A Randomized Controlled Trial. Ann. Am. Thorac. Soc. 2022, 8. online ahead of print. Available online: https://doi.org/10.1513/AnnalsATS.202109-1053OC (accessed on 19 July 2022). [CrossRef] [PubMed]
- Tyson, L.; Hardeman, W.; Marquette, M.; Semlyen, J.; Stratton, G.; Wilson, A.M. A systematic review of the characteristics of interventions that promote physical activity in adults with asthma. J. Health Psychol. 2021, 135910532110593. [Google Scholar] [CrossRef] [PubMed]
- Coelho, C.M.; Reboredo, M.; Martins Valle, F.; Malaguti, C.; Campos, L.A.; Mendes Nascimento, L.; Carvalho, E.V.; César, J.; Oliveira, A.; Pinheiro, B.V.; et al. Effects of an unsupervised pedometer-based physical activity program on daily steps of adults with moderate to severe asthma: A randomized controlled trial. J. Sports Sci. 2017, 36, 1186–1193. [Google Scholar] [CrossRef]
- Bricca, A.; Harris, L.K.; Jäger, M.; Smith, S.M.; Juhl, C.B.; Skou, S.T. Benefits and harms of exercise therapy in people with multimorbidity: A systematic review and meta-analysis of randomised controlled trials. Ageing Res. Rev. 2020, 63, 101166. [Google Scholar] [CrossRef]
- Perret, J.L.; Bonevski, B.; McDonald, C.F.; Abramson, M.J. Smoking cessation strategies for patients with asthma: Improving patient outcomes. J. Asthma Allergy 2016, 9, 117. [Google Scholar] [CrossRef]
- Stead, L.F.; Buitrago, D.; Preciado, N.; Sanchez, G.; Hartmann-Boyce, J.; Lancaster, T. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2013, 5, CD000165. [Google Scholar] [CrossRef]
- Stead, L.F.; Lancaster, T. Behavioural interventions as adjuncts to pharmacotherapy for smoking cessation. Cochrane Database Syst. Rev. 2012, 12, CD009670. [Google Scholar] [CrossRef]
- Lancaster, T.; Stead, L.F. Individual behavioural counselling for smoking cessation. Cochrane Database Syst. Rev. 2017, CD001292. [Google Scholar] [CrossRef]
- Burgess, J.; Ekanayake, B.; Lowe, A.; Dunt, D.; Thien, F.; Dharmage, S.C. Systematic review of the effectiveness of breathing retraining in asthma management. Expert Rev. Respir. Med. 2011, 5, 789–807. [Google Scholar] [CrossRef]
- Freitas, D.A.; Holloway, E.A.; Bruno, S.S.; Chaves, G.S.S.; Fregonezi, G.A.F.; Mendonça, K.M.P.P. Breathing exercises for adults with asthma. Cochrane Database Syst. Rev. 2013, 10, CD001277. [Google Scholar] [CrossRef]
- Harper, V.; Trayer, J. Breathing exercises for adults with asthma. Clin. Exp. Allergy 2022, 52, 732–734. [Google Scholar] [CrossRef]
- Connett, G.J.; Thomas, M. Dysfunctional breathing in children and adults with asthma. Front. Pediatr. 2018, 6, 406. [Google Scholar] [CrossRef]
- Bruton, A.; Lee, A.; Yardley, L.; Raftery, J.; Arden-Close, E.; Kirby, S.; Zhu, S.; Thiruvothiyur, M.; Webley, F.; Taylor, L.; et al. Physiotherapy breathing retraining for asthma: A randomised controlled trial. Lancet Respir. Med. 2018, 6, 19–28. [Google Scholar] [CrossRef]
- Bandura, A. Social cognitive theory in cultural context. Appl. Psychol. 2002, 51, 269–290. [Google Scholar] [CrossRef]
- Bidad, N.; Barnes, N.; Griffiths, C.; Horne, R. Understanding patients’ perceptions of asthma control: A qualitative study. Eur. Respir. J. 2018, 51, 1701346. [Google Scholar] [CrossRef]
- Kaptein, A.A.; Klok, T.; Moss-Morris, R.; Brand, P.L. Illness perceptions: Impact on self-management and control in asthma. Curr. Opin. Allergy Clin. Immunol. 2010, 10, 194–199. [Google Scholar] [CrossRef]
- Harris, G.S.; Harris, D.G.; Shearer, A.G. Beliefs That Support the Behavior of People with Asthma: A Qualitative Investigation. J. Asthma 2015, 38, 427–434. [Google Scholar] [CrossRef]
- Ross, C.J.M.; Williams, B.A.; Low, G.; Vethanayagam, D. Perceptions about self-management among people with severe asthma. J. Asthma 2010, 47, 330–336. [Google Scholar] [CrossRef]
- Unni, E.; Shiyanbola, O.O. Clustering medication adherence behavior based on beliefs in medicines and illness perceptions in patients taking asthma maintenance medications. Curr. Med. Res. Opin. 2015, 32, 113–121. [Google Scholar] [CrossRef]
- Horne, R.; Weinman, J. Self-regulation and Self-management in Asthma: Exploring The Role of Illness Perceptions and Treatment Beliefs in Explaining Non-adherence to Preventer Medication. Psychol. Health 2002, 17, 17–32. [Google Scholar] [CrossRef]
- Miles, C.; Arden-Close, E.; Thomas, M.; Bruton, A.; Yardley, L.; Hankins, M.; Kirby, S.E. Barriers and facilitators of effective self-management in asthma: Systematic review and thematic synthesis of patient and healthcare professional views. NPJ Prim. Care Respir. Med. 2017, 27, 57. [Google Scholar] [CrossRef]
- Dhruve, H. Management of asthma: Adherence, inhaler technique and self-management. Pract. Nurs. 2018, 29, 465–468. [Google Scholar] [CrossRef][Green Version]
- Tan, D.J.; Burgess, J.A.; Perret, J.L.; Bui, D.S.; Abramson, M.J.; Dharmage, S.C.; Walters, E.H. Non-pharmacological management of adult asthma in Australia: Cross-sectional analysis of a population-based cohort study. J. Asthma 2020, 57, 105–112. [Google Scholar] [CrossRef]
- Schuers, M.; Chapron, A.; Guihard, H.; Bouchez, T.; Darmon, D. Impact of non-drug therapies on asthma control: A systematic review of the literature. Eur. J. Gen. Pract. 2019, 25, 65–76. [Google Scholar] [CrossRef]
- Smith, H.E.; Jones, C.J. Psychological Interventions in Asthma. Curr. Treat. Options Allergy 2015, 2, 155–168. [Google Scholar] [CrossRef]
- Put, C.; van den Bergh, O.; Lemaigre, V.; Demedts, M.; Verleden, G. Evaluation of an individualised asthma programme directed at behavioural change. Eur. Respir. J. 2003, 21, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.R.; Mugford, M.; Holland, R.; Noble, M.J.; Harrison, B.D.W. Psycho-educational interventions for adults with severe or difficult asthma: A systematic review. J. Asthma 2007, 44, 219–241. [Google Scholar] [CrossRef] [PubMed]
- Ayres, J.G.; Gabbott, P.L.A. Vocal cord dysfunction and laryngeal hyperresponsiveness: A function of altered autonomic balance? Thorax 2002, 57, 284–285. [Google Scholar] [CrossRef]
- Gimenez, L.M.; Zafra, H. Vocal cord dysfunction: An update. Ann. Allergy Asthma Immunol. 2011, 106, 267–274. [Google Scholar] [CrossRef]
- Hicks, M.; Brugman, S.M.; Katial, R. Vocal Cord Dysfunction/Paradoxical Vocal Fold Motion. Prim. Care—Clin. Off. Pract. 2008, 35, 81–103. [Google Scholar] [CrossRef]
- Dunn, N.M.; Katial, R.K.; Hoyte, F.C.L. Vocal cord dysfunction: A review. Asthma Res. Pract. 2015, 1, 9. [Google Scholar] [CrossRef]
- Halvorsen, T.; Walsted, E.S.; Bucca, C.; Bush, A.; Cantarella, G.; Friedrich, G.; Herth, F.J.F.; Hull, J.H.; Jung, H.; Maat, R.; et al. Inducible laryngeal obstruction: An official joint European Respiratory Society and European Laryngological Society statement. Eur. Respir. J. 2017, 50, 1602221. [Google Scholar] [CrossRef]
- Lacy, T.J.; McManis, S.E. Psychogenic stridor. Gen. Hosp. Psychiatry 1994, 16, 213–223. [Google Scholar] [CrossRef]
- Hyland, M.E.; Lanario, J.W.; Wei, Y.; Jones, R.C.; Masoli, M. Evidence for similarity in symptoms and mechanism: The extra-pulmonary symptoms of severe asthma and the polysymptomatic presentation of fibromyalgia. Immunity Inflamm. Dis. 2019, 7, 239–249. [Google Scholar] [CrossRef]
- Spathis, A.; Booth, S.; Moffat, C.; Hurst, R.; Ryan, R.; Chin, C.; Burkin, J. The Breathing, Thinking, Functioning clinical model: A proposal to facilitate evidence-based breathlessness management in chronic respiratory disease. NPJ Prim. Care Respir. Med. 2017, 27, 27. [Google Scholar] [CrossRef]
- Federman, A.D.; Wolf, M.S.; Sofianou, A.; Martynenko, M.; O’Connor, R.; Halm, E.A.; Leventhal, H.; Wisnivesky, J.P. Self-Management Behaviors in Older Adults with Asthma: Associations with Health Literacy. J. Am. Geriatr. Soc. 2014, 62, 872–879. [Google Scholar] [CrossRef]
- Foley, L.; Hynes, L.; Murphy, A.W.; Molloy, G.J. ‘Just keep taking them, keep hoping they’ll work’: A qualitative study of adhering to medications for multimorbidity. Br. J. Health Psychol. 2021, 27, 691–715. [Google Scholar] [CrossRef]
- Maffoni, M.; Traversoni, S.; Costa, E.; Midão, L.; Kardas, P.; Kurczewska-Michalak, M.; Giardini, A. Medication adherence in the older adults with chronic multimorbidity: A systematic review of qualitative studies on patient’s experience. Eur. Geriatr. Med. 2020, 11, 369–381. [Google Scholar] [CrossRef]
- Hall, C.; Nici, L.; Sood, S.; ZuWallack, R.; Castro, M. Nonpharmacologic Therapy for Severe Persistent Asthma. J. Allergy Clin. Immunol. Pract. 2017, 5, 928–935. [Google Scholar] [CrossRef]
- Zampogna, E.; Spanevello, A.; Visca, D. Pulmonary rehabilitation: Promising nonpharmacological approach for treating asthma? Curr. Opin. Allergy Clin. Immunol. 2020, 20, 80–84. [Google Scholar] [CrossRef]
- Chaaban, T.A. Bariatric surgery: A potential cure for asthma? Eur. Respir. Rev. 2019, 28, 190003. [Google Scholar] [CrossRef]
- Hossain, N.; Arhi, C.; Borg, C.M. Is Bariatric Surgery Better than Nonsurgical Weight Loss for Improving Asthma Control? A systematic review. Obes. Surg. 2021, 31, 1810–1832. [Google Scholar] [CrossRef]
- Jumbe, S.; Hamlet, C.; Meyrick, J. Psychological Aspects of Bariatric Surgery as a Treatment for Obesity. Curr. Obes. Rep. 2017, 6, 71–78. [Google Scholar] [CrossRef]
- Kalarchian, M.A.; Marcus, M.D. Psychosocial Interventions Pre and Post Bariatric Surgery. Eur. Eat. Disord. Rev. 2015, 23, 457–462. [Google Scholar] [CrossRef]
- Rudolph, A.; Hilbert, A. Post-operative behavioural management in bariatric surgery: A systematic review and meta-analysis of randomized controlled trials. Obes. Rev. 2013, 14, 292–302. [Google Scholar] [CrossRef]
- Wileman, S.M.; McCann, S.; Grant, A.M.; Krukowski, Z.H.; Bruce, J. Medical versus surgical management for gastro-oesophageal reflux disease (GORD) in adults. Cochrane Database Syst. Rev. 2010, 3, CD003243. [Google Scholar] [CrossRef]
- Dibley, L.B.; Norton, C.; Jones, R. Non-pharmacological intervention for gastro-oesophageal reflux disease in primary care. Br. J. Gen. Pract. 2010, 60, e459–e465. [Google Scholar] [CrossRef] [PubMed]
- Haines, J.; Hull, J.H.; Fowler, S.J. Clinical presentation, assessment, and management of inducible laryngeal obstruction. Curr. Opin. Otolaryngol. Head Neck Surg. 2018, 26, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, P.; Daines, L.; Campbell, C.; Mckinstry, B.; Weller, D.; Pinnock, H. Telehealth Interventions to Support Self-Management of Long-Term Conditions: A Systematic Metareview of Diabetes, Heart Failure, Asthma, Chronic Obstructive Pulmonary Disease, and Cancer. J. Med. Internet Res. 2017, 19, e172. [Google Scholar] [CrossRef]
- Morrison, D.; Mair, F.S.; Yardley, L.; Kirby, S.; Thomas, M. Living with asthma and chronic obstructive airways disease: Using technology to support self-management—An overview. Chron. Respir. Dis. 2017, 14, 407–419. [Google Scholar] [CrossRef]
- Hui, C.Y.; McKinstry, B.; Fulton, O.; Buchner, M.; Pinnock, H. Patients’ and Clinicians’ Visions of a Future Internet-of-Things System to Support Asthma Self-Management: Mixed Methods Study. J. Med. Internet Res. 2021, 23, e22432. [Google Scholar] [CrossRef]
- Kok, G. A practical guide to effective behaviour change. Eur. Health Psychol. 2015, 16, 156–170. [Google Scholar] [CrossRef]
- West, R.; Michie, S. Applying the Behaviour Change Wheel a Very Brief Guide. 2015. Available online: www.behaviourchangewheel.com (accessed on 15 July 2022).
- Michie, S.; Prestwich, A. Are interventions theory-based? Development of a theory coding scheme. Health Psychol. 2010, 29, 1–8. [Google Scholar] [CrossRef]
- Smith, S.M.; Bayliss, E.A.; Mercer, S.W.; Gunn, J.; Vestergaard, M.; Wyke, S.; Salisbury, C.; Fortin, M. How to Design and Evaluate Interventions to Improve Outcomes for Patients with Multimorbidity. J. Comorbidity 2013, 3, 10–17. [Google Scholar] [CrossRef]
- Coventry, P.A.; Meader, N.; Melton, H.; Temple, M.; Dale, H.; Wright, K.; Cloitre, M.; Karatzias, T.; Bisson, J.; Roberts, N.P.; et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: Systematic review and component network meta-analysis. PLoS Med. 2020, 17, e1003262. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Institute for Futures Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Carver, C.S.; Scheier, M.F. On the Self-Regulation of Behaviour, 1st ed.; Cambridge University Press: Cambridge, UK, 1998. [Google Scholar]
- Grimmett, C.; Bates, A.; West, M.; Leggett, S.; Varkonyi-Sepp, J.; Campbell, A.; Davis, J.; Wootton, S.; Shaw, C.; Barlow, R.; et al. SafeFit Trial: Virtual clinics to deliver a multimodal intervention to improve psychological and physical well-being in people with cancer. Protocol of a COVID-19 targeted non-randomised phase III trial. BMJ Open 2021, 11, e048175. [Google Scholar] [CrossRef]
- Department of Health. Comorbidities—A Framework of Principles for System-Wide Action. 2014. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/307143/Comorbidities_framework.pdf (accessed on 25 July 2022).
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J. Med. Internet Res. 2015, 17, e30. [Google Scholar] [CrossRef]
- O’Cathain, A.; Croot, L.; Duncan, E.; Rousseau, N.; Sworn, K.; Turner, K.M.; Yardley, L.; Hoddinott, P. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019, 9, e029954. [Google Scholar] [CrossRef]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef]
- Yardley, L.; Ainsworth, B.; Arden-Close, E.; Muller, I. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasibility Stud. 2015, 1, 37. [Google Scholar] [CrossRef]
- Lawrence, W.; Baird, J.; Thompson, S.; Jarman, M.; Tinati, T.; Barker, M.; Nutbeam, D.; Davies, J.; Vogel, C.; Begum, R.; et al. Translating Developmental Origins: Improving the Health of Women and Their Children Using a Sustainable Approach to Behaviour Change. Healthcare 2017, 5, 17. [Google Scholar] [CrossRef]
- Lawrence, W.; Black, C.; Tinati, T.; Cradock, S.; Begum, R.; Jarman, M.; Pease, A.; Margetts, B.; Davies, J.; Inskip, H.; et al. “Making every contact count”: Evaluation of the impact of an intervention to train health and social care practitioners in skills to support health behaviour change. J. Health Psychol. 2016, 21, 138–151. [Google Scholar] [CrossRef]
- Black, C.; Lawrence, W.; Cradock, S.; Ntani, G.; Tinati, T.; Jarman, M.; Begum, R.; Inskip, H.; Cooper, C.; Barker, M.; et al. Healthy conversation skills: Increasing competence and confidence in front-line staff. Public Health Nutr. 2014, 17, 700–707. [Google Scholar] [CrossRef]
- Lawrence, W.; Watson, D.; Barker, H.; Vogel, C.; Rahman, E.; Barker, M. Meeting the UK Government’s prevention agenda: Primary care practitioners can be trained in skills to prevent disease and support self-management. Perspect. Public Health 2022, 143, 158–166. [Google Scholar] [CrossRef]
- Hollis, J.L.; Kocanda, L.; Seward, K.; Collins, C.; Tully, B.; Hunter, M.; Foureur, M.; Lawrence, W.; MacDonald-Wicks, L.; Schumacher, T. The impact of Healthy Conversation Skills training on health professionals’ barriers to having behaviour change conversations: A pre-post survey using the Theoretical Domains Framework. BMC Health Serv. Res. 2021, 21, 880. [Google Scholar] [CrossRef]
- Tinati, T.; Lawrence, W.; Ntani, G.; Black, C.; Cradock, S.; Jarman, M.; Pease, A.; Begum, R.; Inskip, H.; Cooper, C.; et al. Implementation of new Healthy Conversation Skills to support lifestyle changes—what helps and what hinders? Experiences of Sure Start Children’s Centre staff. Health Soc. Care Community 2012, 20, 430–437. [Google Scholar] [CrossRef]
- The NHS Long Term Plan. 2019. Available online: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan-june-2019.pdf (accessed on 5 July 2022).
- Ivbijaro, G.; Goldberg, D.; Enum, Y.; Kolkiewicz, L. Comorbidity, Multi-Morbidity, Stepped Care and Skill Mix in the Care of the Older Population. In Primary Care Mental Health in Older People; Springer: Cham, Switzerland, 2019; pp. 45–49. [Google Scholar] [CrossRef]
- Sampalli, T.; Dickson, R.; Hayden, J.; Edwards, L.; Salunkhe, A. Meeting the needs of a complex population: A functional health-and patient-centered approach to managing multimorbidity. J. Comorbidity 2016, 6, 76–84. [Google Scholar] [CrossRef]
- Gunn, J. Designing care for people with mixed mental and physical multimorbidity. BMJ 2015, 350, h712. [Google Scholar] [CrossRef]
- Garvey, J.; Connolly, D.; Boland, F.; Smith, S.M. OPTIMAL, an occupational therapy led self-management support programme for people with multimorbidity in primary care: A randomized controlled trial. BMC Fam. Pract. 2015, 16, 59. [Google Scholar] [CrossRef]
- Elston, J.; Gradinger, F.; Asthana, S.; Lilley-Woolnough, C.; Wroe, S.; Harman, H.; Byng, R. Does a social prescribing “holistic” link-worker for older people with complex, multimorbidity improve well-being and frailty and reduce health and social care use and costs? A 12-month before-and-after evaluation. Prim. Health Care Res. Dev. 2019, 20, e135. [Google Scholar] [CrossRef] [PubMed]
- Boehmer, K.R.; Guerton, N.M.; Soyring, J.; Hargraves, I.; Dick, S.; Montori, V.M. Capacity Coaching: A New Strategy for Coaching Patients Living With Multimorbidity and Organizing Their Care. Mayo Clin. Proc. 2019, 94, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Crossman-Barnes, C.J.; Peel, A.; Fong-Soe-Khioe, R.; Sach, T.; Wilson, A.; Barton, G. Economic evidence for nonpharmaco-logical asthma management interventions: A systematic review. Allergy 2018, 73, 1182–1195. [Google Scholar] [CrossRef] [PubMed]
- Mosnaim, G.; Safioti, G.; Brown, R.; DePietro, M.; Szefler, S.J.; Lang, D.M.; Portnoy, J.M.; Bukstein, D.A.; Bacharier, L.B.; Merchant, R.K. Digital Health Technology in Asthma: A Comprehensive Scoping Review. J. Allergy Clin. Immunol. Pract. 2021, 9, 2377–2398. [Google Scholar] [CrossRef] [PubMed]


| Referral Route & Care Co-Ordination | Individual Referral to Each Specialist Decided by Asthma Physician Who also Co-Ordinates Care | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention provider | |||||||||
| Intervention level | CBT | Counselling | Relaxation | Exercise | Diet | Breathing training | Speech therapy | Smoking cessation | Psycho- education |
| Specialist | Clinical Psychologist | Clinical Psychologist/ Asthma Physician | Clinical Psychologist | Physiotherapist | Dietician | Physiotherapist | Speech Therapist | Specialist Behaviour Services-smoking/ Asthma Physician | Clinical Psychologist/ Nurse |
| Referral Route & Care Co-Ordination | Multidisciplinary Care Plan Drawn up in Collaboration with Patient, Based on Holistic Needs Assessment, Patient and Clinician Preferences. Dedicated Care Co-Ordinator Ensures Agility and Flexibility with Periodic Multidisciplinary Needs Review | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention provider | |||||||||
| Intervention level (needs based) | CBT | Counselling | Relaxation | Exercise | Diet | Breathing training | Speech therapy | Smoking cessation | Psycho- education |
| Specialist | Clinical Psychologist | Clinical Psychologist | Clinical Psychologist | Physiotherapist | Dietician | Physiotherapist | Speech Therapist | Specialist Behaviour Services-smoking | Clinical Psychologist/ Nurse |
| Targeted | CBT therapist/ Psychological Wellbeing Practitioner | Counsellor/ Psychological Wellbeing Practitioner | Counsellor/ Nurse/ Psychological Wellbeing Practitioner | Personal Trainer | Dietician/Specialist Behaviour Services -weight loss | Personal Trainer | Speech Therapist | Specialist Behaviour Services-smoking | Nurse/ Health Coach |
| Universal | Telehealth/ Self-help | Telehealth/ Self-help/ Asthma Physician | Telehealth/ Social Prescriber/ Health Coach | Self-help/ Social Prescriber/ Health Coach | Self-help/ Social Prescriber/ Health Coach | Telehealth | Speech Therapist | Self-help/ Social Prescriber/ Health Coach/ Asthma Physician | Telehealth/ Social Prescriber/ Health Coach/ Asthma Physician |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Varkonyi-Sepp, J.; Freeman, A.; Ainsworth, B.; Kadalayil, L.P.; Haitchi, H.M.; Kurukulaaratchy, R.J. Multimorbidity in Difficult Asthma: The Need for Personalised and Non-Pharmacological Approaches to Address a Difficult Breathing Syndrome. J. Pers. Med. 2022, 12, 1435. https://doi.org/10.3390/jpm12091435
Varkonyi-Sepp J, Freeman A, Ainsworth B, Kadalayil LP, Haitchi HM, Kurukulaaratchy RJ. Multimorbidity in Difficult Asthma: The Need for Personalised and Non-Pharmacological Approaches to Address a Difficult Breathing Syndrome. Journal of Personalized Medicine. 2022; 12(9):1435. https://doi.org/10.3390/jpm12091435
Chicago/Turabian StyleVarkonyi-Sepp, Judit, Anna Freeman, Ben Ainsworth, Latha Perunthadambil Kadalayil, Hans Michael Haitchi, and Ramesh J. Kurukulaaratchy. 2022. "Multimorbidity in Difficult Asthma: The Need for Personalised and Non-Pharmacological Approaches to Address a Difficult Breathing Syndrome" Journal of Personalized Medicine 12, no. 9: 1435. https://doi.org/10.3390/jpm12091435
APA StyleVarkonyi-Sepp, J., Freeman, A., Ainsworth, B., Kadalayil, L. P., Haitchi, H. M., & Kurukulaaratchy, R. J. (2022). Multimorbidity in Difficult Asthma: The Need for Personalised and Non-Pharmacological Approaches to Address a Difficult Breathing Syndrome. Journal of Personalized Medicine, 12(9), 1435. https://doi.org/10.3390/jpm12091435







