Six Commonly Used Postoperative Radiographic Alignment Parameters Do Not Predict Clinical Outcome Scores after Unrestricted Caliper-Verified Kinematically Aligned TKA
Abstract
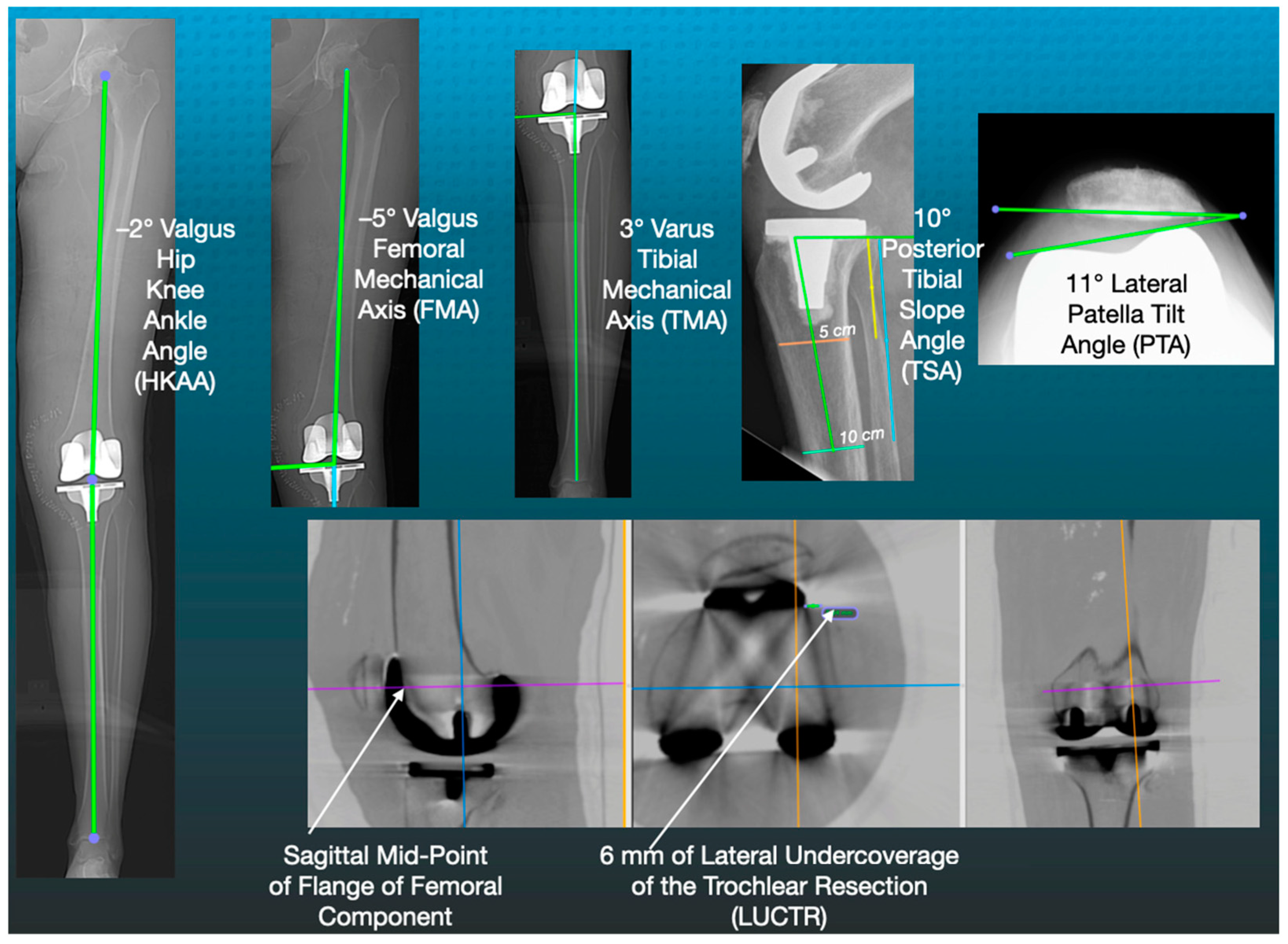
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nedopil, A.J.; Delman, C.; Howell, S.M.; Hull, M.L. Restoring the Patient’s Pre-Arthritic Posterior Slope Is the Correct Target for Maximizing Internal Tibial Rotation When Implanting a PCL Retaining TKA with Calipered Kinematic Alignment. J. Pers. Med. 2021, 11, 516. [Google Scholar] [CrossRef] [PubMed]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. What mechanisms are associated with tibial component failure after kinematically-aligned total knee arthroplasty? Int. Orthop. 2017, 41, 1561–1569. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Singh, A.K.; Howell, S.M.; Hull, M.L. Does calipered kinematically aligned TKA restore native left to right symmetry of the lower limb and improve function? J. Arthroplast. 2018, 33, 398–406. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Hess, S.; Behrend, H.; Amsler, F.; Leclercq, V.; Moser, L.B. Phenotyping of hip-knee-ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1378–1384. [Google Scholar] [CrossRef] [PubMed]
- Howell, S.M.; Gill, M.; Shelton, T.J.; Nedopil, A.J. Reoperations are few and confined to the most valgus phenotypes 4 years after unrestricted calipered kinematically aligned TKA. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 948–957. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wen, L.; Zhang, L.; Ma, D.; Dong, X.; Qu, T. Undercoverage of lateral trochlear resection is correlated with the tibiofemoral alignment parameters in kinematically aligned TKA: A retrospective clinical study. BMC Musculoskelet. Disord. 2021, 22, 196. [Google Scholar] [CrossRef] [PubMed]
- Koh, D.T.S.; Woo, Y.L.; Yew, A.K.S.; Yeo, S.-J. Kinematic aligned femoral rotation leads to greater patella tilt but similar clinical outcomes when compared to traditional femoral component rotation in total knee arthroplasty. A propensity score matched study. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Calek, A.K.; Hochreiter, B.; Hess, S.; Amsler, F.; Leclerq, V.; Hirschmann, M.T.; Behrend, H. High inter- and intraindividual differences in medial and lateral posterior tibial slope are not reproduced accurately by conventional TKA alignment techniques. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Howell, S.M.; Bini, S.A.; Steele, G.D. Calipered Kinematically Aligned Total Knee Arthroplasty Performed with Specific Manual Instrumentation, Verification Checks, and a Decision Tree. In Calipered Kinematically Aligned Total Knee Arthroplasty: Theory, Surgical Techniques, Perspectives, 1st ed.; Howell, S.M., Bini, S.A., Steele, G.D., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; Volume 1, p. 7. [Google Scholar]
- Howell, S.M.; Nedopil, A.J.; Hull, M.L. Negligible effect of surgeon experience on the accuracy and time to perform unrestricted caliper verified kinematically aligned TKA with manual instruments. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2966–2974. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Zamora, T.; Delman, C.; Howell, S.M.; Hull, M.L. Which Asymmetric Tibial Component Is Optimally Designed for Calipered Kinematically Aligned Total Knee Arthroplasty? J. Knee Surg. 2021. [Google Scholar] [CrossRef] [PubMed]
- Meneghini, R.M.; Mont, M.A.; Backstein, D.B.; Bourne, R.B.; Dennis, D.A.; Scuderi, G.R. Development of a Modern Knee Society Radiographic Evaluation System and Methodology for Total Knee Arthroplasty. J. Arthroplast. 2015, 30, 2311–2314. [Google Scholar] [CrossRef]
- Bartlett, J.W.; Frost, C. Reliability, repeatability and reproducibility: Analysis of measurement errors in continuous variables. Ultrasound Obs. Gynecol 2008, 31, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Mugnai, R.; Zambianchi, F.; Digennaro, V.; Marcovigi, A.; Tarallo, L.; Del Giovane, C.; Catani, F. Clinical outcome is not affected by total knee arthroplasty alignment. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3339–3345. [Google Scholar] [CrossRef] [PubMed]
- Slevin, O.; Amsler, F.; Hirschmann, M.T. No correlation between coronal alignment of total knee arthroplasty and clinical outcomes: A prospective clinical study using 3D-CT. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3892–3900. [Google Scholar] [CrossRef]
- Nishida, K.; Matsumoto, T.; Takayama, K.; Ishida, K.; Nakano, N.; Matsushita, T.; Kuroda, R.; Kurosaka, M. Remaining mild varus limb alignment leads to better clinical outcome in total knee arthroplasty for varus osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3488–3494. [Google Scholar] [CrossRef] [PubMed]
- Vanlommel, L.; Vanlommel, J.; Claes, S.; Bellemans, J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2325–2330. [Google Scholar] [CrossRef]
- Roth, J.D.; Howell, S.M.; Hull, M.L. Kinematically aligned total knee arthroplasty limits high tibial forces, differences in tibial forces between compartments, and abnormal tibial contact kinematics during passive flexion. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1589–1601. [Google Scholar] [CrossRef] [PubMed]
- Roth, J.D.; Howell, S.M.; Hull, M.L. Tibial forces are more useful than varus-valgus laxities for identifying and correcting overstuffing in kinematically aligned total knee arthroplasty. J. Orthop. Res. 2021, 39, 1271–1280. [Google Scholar] [CrossRef]
- Shelton, T.J.; Howell, S.M.; Hull, M.L. A total knee arthroplasty is stiffer when the intraoperative tibial force is greater than the native knee. J. Knee Surg. 2019, 32, 1008–1014. [Google Scholar] [CrossRef]
- Shelton, T.J.; Howell, S.M.; Hull, M.L. Is there a force target that predicts early patient-reported outcomes after kinematically aligned TKA? Clin. Orthop. Relat. Res. 2019, 477, 1200. [Google Scholar] [CrossRef]
- Shelton, T.J.; Nedopil, A.J.; Howell, S.M.; Hull, M.L. Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? Limb and joint line alignment after kinematically aligned total knee arthroplasty. Bone Jt. J. 2017, 99-B, 1319–1328. [Google Scholar] [CrossRef]
- Riley, J.; Roth, J.D.; Howell, S.M.; Hull, M.L. Internal-external malalignment of the femoral component in kinematically aligned total knee arthroplasty increases tibial force imbalance but does not change laxities of the tibiofemoral joint. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1618–1628. [Google Scholar] [CrossRef] [PubMed]
- Riley, J.; Roth, J.D.; Howell, S.M.; Hull, M.L. Increases in tibial force imbalance but not changes in tibiofemoral laxities are caused by varus–valgus malalignment of the femoral component in kinematically aligned TKA. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3238–3248. [Google Scholar] [CrossRef] [PubMed]
- Nedopil, A.J.; Dhaliwal, A.; Howell, S.M.; Hull, M.L. A Surgeon That Switched to Unrestricted Kinematic Alignment with Manual Instruments Has a Short Learning Curve and Comparable Resection Accuracy and Outcomes to Those of an Experienced Surgeon. J. Pers. Med. 2022, 12, 1152. [Google Scholar] [CrossRef]
- Naveen, N.B.; Deckard, E.R.; Ziemba-Davis, M.; Hanson, L.F.; Warth, L.C.; Meneghini, R.M. Patellar tilt does not affect patient reported outcomes after modern total knee arthroplasty. Knee 2022, 34, 167–177. [Google Scholar] [CrossRef]


| Preoperative Characteristics | Values ± Standard Deviation (Range) |
|---|---|
| Age | 70 ± 8 years (54 to 84) |
| Sex | 21 females and 22 males |
| Body mass index | 32 ± 7 kg/m2 (21 to 52) |
| Extension | 8 ± 7° (0 to 29°) |
| Flexion | 113 ± 6° (100 to 125°) |
| Type of osteoarthritic knee deformity | 67% varus, 26% valgus, and 7% patellofemoral |
| Radiographic knee deformity (+varus, −valgus) | −1 ± 7 (14 to −17) |
| Kellgren–Lawrence classification | 2% II, 35% III, and 63% IV |
| Oxford knee score (48 is best and 0 is worst) | 21 ± 8 points (6 to 39) |
| KOOS Jr (100 is best and 0 is worst) | 43 ± 14 points (16 to 73) |
| Postoperative Alignment Parameter | Interobserver Intraclass Correlation | Intraobserver Intraclass Correlation | Repeatability |
|---|---|---|---|
| Femoral mechanical angle (FMA) | ICC = 0.92 * | ICC = 0.92 * | 0.5° |
| Tibial mechanical angle (TMA) | ICC = 0.94 * | ICC = 0.94 * | 0.5° |
| Hip–knee–ankle angle (HKAA) | ICC = 0.95 * | ICC = 0.95 * | 0.6° |
| Tibial slope angle (TSA) | ICC = 0.82 # | ICC = 0.83 # | 0.8° |
| Patella tilt angle (PTA) | ICC = 0.88 # | ICC = 0.89 # | 0.9° |
| Lateral undercoverage of the trochlear resection (LUCTR) | ICC = 0.92 * | ICC = 0.93 * | 0.5 mm |
| Postoperative Alignment Parameter | Minimum to Maximum Mean ± SD | Varus and Slope MA Outlier Type or Range | Valgus and Slope MA Outlier Type or Range |
|---|---|---|---|
| Femoral mechanical angle (FMA) | 2° varus to −9° valgus −3° ± 2.4° | 0% varus | 53% valgus (<−3°) |
| Tibial mechanical angle (TMA) | 10° varus to −9° valgus 4° ± 2.6° | 63% varus (<87°) | 0% valgus |
| Hip–knee–ankle angle (HKAA) | 10° varus to −7° valgus 1° ± 3.9° | 26% varus (>3°) | 14% valgus (<−3°) |
| Tibial slope angle (TSA) | −4° anterior to 11° posterior 5° ± 3.8° | 28% within 0–3° | 16% within 0–3° |
| Patella tilt angle (PTA) | −3° medial to 11° lateral 3° ± 3.1° | ||
| Lateral undercoverage of the trochlear resection (LUCTR) | 2 to 9 mm 4 ± 1.5 mm | 60% within 3–6 mm | 30% > 6 mm |
| Postoperative Alignment Parameter | Forgotten Joint Score | Oxford Knee Score | KOOS Jr |
|---|---|---|---|
| Femoral mechanical angle (FMA) | r = −0.093 p = 0.552 | r = −0.107 p = 0.494 | r = −0.106 p = 0.946 |
| Tibial mechanical angle (TMA) | r = 0.138 p = 0.376 | r = 0.059 p = 0.7091 | r = 0.265 p = 0.086 |
| Hip–knee–ankle angle (HKAA) | r = 0.133 p = 0.403 | r = 0.082 p = 0.608 | r = −0.099 p = 0.535 |
| Tibial slope angle (TSA) | r = −0.157 p = 0.316 | r = −0.281 p = 0.068 | r = −0.205 p = 0.187 |
| Patella tilt angle (PTA) | r = 0.107 p = 0.498 | r = 0.122 p = 0.4430 | r = 0.214 p = 0.173 |
| Lateral undercoverage of the trochlear resection (LUCTR) | r = 0.088 p = 0.5739 | r = 0.007 p = 0.966 | r = −0.041 p = 0.797 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhaliwal, A.; Zamora, T.; Nedopil, A.J.; Howell, S.M.; Hull, M.L. Six Commonly Used Postoperative Radiographic Alignment Parameters Do Not Predict Clinical Outcome Scores after Unrestricted Caliper-Verified Kinematically Aligned TKA. J. Pers. Med. 2022, 12, 1468. https://doi.org/10.3390/jpm12091468
Dhaliwal A, Zamora T, Nedopil AJ, Howell SM, Hull ML. Six Commonly Used Postoperative Radiographic Alignment Parameters Do Not Predict Clinical Outcome Scores after Unrestricted Caliper-Verified Kinematically Aligned TKA. Journal of Personalized Medicine. 2022; 12(9):1468. https://doi.org/10.3390/jpm12091468
Chicago/Turabian StyleDhaliwal, Anand, Tomas Zamora, Alexander J. Nedopil, Stephen M. Howell, and Maury L. Hull. 2022. "Six Commonly Used Postoperative Radiographic Alignment Parameters Do Not Predict Clinical Outcome Scores after Unrestricted Caliper-Verified Kinematically Aligned TKA" Journal of Personalized Medicine 12, no. 9: 1468. https://doi.org/10.3390/jpm12091468






