The Doctor Is In(ternet): The Mediating Role of Health Anxiety in the Relationship between Somatic Symptoms and Cyberchondria
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Statistical Analyses
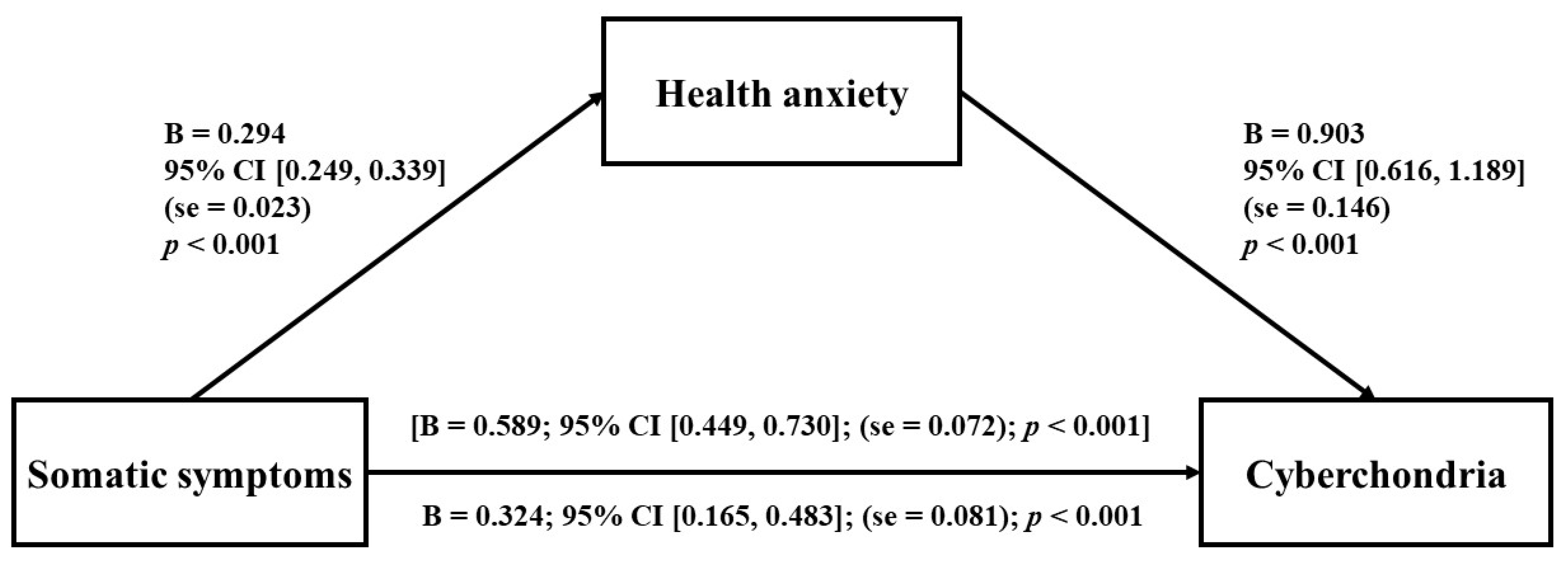
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Starcevic, V. Cyberchondria: Challenges of problematic online searches for health-related information. Psychother. Psychosom. 2017, 86, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Starcevic, V.; Berle, D.; Arnáez, S. Recent insights into cyberchondria. Curr. Psychiatry Rep. 2020, 22, 56. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar] [CrossRef]
- World Health Organization International. Mental, Behavioural or Neurodevelopmental Disorders. Available online: https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f334423054 (accessed on 6 August 2022).
- Vismara, M.; Caricasole, V.; Starcevic, V.; Cinosi, E.; Dell’Osso, B.; Martinotti, G.; Fineberg, N.A. Is cyberchondria a new transdiagnostic digital compulsive syndrome? A systematic review of the evidence. Compr. Psychiatry 2020, 99, 152167. [Google Scholar] [CrossRef] [PubMed]
- Baggio, S.; Starcevic, V.; Billieux, J.; King, D.L.; Gainsbury, S.M.; Eslick, G.D.; Berle, D. Testing the spectrum hypothesis of problematic online behaviors: A network analysis approach. Addict. Behav. 2022, 135, 107451. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, M. A “components” model of addiction within a biopsychosocial framework. J. Subst. Use 2005, 10, 191–197. [Google Scholar] [CrossRef]
- Young, K.S. Internet addiction: The emergence of a new clinical disorder. Cyberpsychol. Behav. 1998, 1, 237–244. [Google Scholar] [CrossRef]
- Chiriţă, V.; Chiriţă, R.; Stefănescu, C.; Chele, G.; Ilinca, M. Computer use and addiction in Romanian children and teenagers—An observational study. Rev. Med. Chir. Soc. Med. Nat. Iasi 2006, 110, 526–532. [Google Scholar]
- Poli, R.; Agrimi, E. Internet addiction disorder: Prevalence in an Italian student population. Nord. J. Psychiatry 2012, 66, 55–59. [Google Scholar] [CrossRef]
- Zboralski, K.; Orzechowska, A.; Talarowska, M.; Darmosz, A.; Janiak, A.; Janiak, M.; Florkowski, A.; Gałecki, P. The prevalence of computer and Internet addiction among pupils. Postepy Hig. Med. Dosw. 2009, 63, 8–12. [Google Scholar]
- Kardefelt-Winther, D. A conceptual and methodological critique of Internet addiction research: Towards a model of compensatory Internet use. Comput. Hum. Behav. 2014, 31, 351–354. [Google Scholar] [CrossRef]
- Kardefelt-Winther, D.; Heeren, A.; Schimmenti, A.; van Rooij, A.; Maurage, P.; Carras, M.; Edman, J.; Blaszczynski, A.; Khazaal, Y.; Billieux, J. How can we conceptualize behavioural addiction without pathologizing common behaviours? Addiction 2017, 112, 1709–1715. [Google Scholar] [CrossRef] [PubMed]
- Musetti, A.; Manari, T.; Billieux, J.; Starcevic, V.; Schimmenti, A. Problematic social networking sites use and attachment: A systematic review. Comput. Hum. Behav. 2022, 131, 107199. [Google Scholar] [CrossRef]
- Santoro, G.; Midolo, L.R.; Costanzo, A.; Cassarà, M.S.; Russo, S.; Musetti, A.; Schimmenti, A. From parental bonding to problematic gaming: The mediating role of adult attachment styles. Mediterr. J. Clin. Psychol. 2021, 9. [Google Scholar] [CrossRef]
- Schimmenti, A.; Musetti, A.; Costanzo, A.; Terrone, G.; Maganuco, N.R.; Aglieri Rinella, C.; Gervasi, A.M. The unfabulous four: Maladaptive personality functioning, insecure attachment, dissociative experiences, and problematic Internet use among young adults. Int. J. Ment. Health Addict. 2021, 19, 447–461. [Google Scholar] [CrossRef]
- Di Blasi, M.; Giardina, A.; Giordano, C.; Lo Coco, G.; Tosto, C.; Billieux, J.; Schimmenti, A. Problematic video game use as an emotional coping strategy: Evidence from a sample of MMORPG gamers. J. Behav. Addict. 2019, 8, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Ma, J.-L. Adult attachment style, emotion regulation, and social networking sites addiction. Front. Psychol. 2019, 10, 2352. [Google Scholar] [CrossRef]
- Russo, A.; Santoro, G.; Schimmenti, A. Interpersonal guilt and problematic online behaviors: The mediating role of emotion dysregulation. Clin. Neuropsychiatry 2022, 19, 236–247. [Google Scholar] [CrossRef]
- Gervasi, A.M.; La Marca, L.; Costanzo, A.; Pace, U.; Guglielmucci, F.; Schimmenti, A. Personality and Internet gaming disorder: A systematic review of recent literature. Curr. Addict. Rep. 2017, 4, 293–307. [Google Scholar] [CrossRef]
- Musetti, A.; Mancini, T.; Corsano, P.; Santoro, G.; Cavallini, M.C.; Schimmenti, A. Maladaptive personality functioning and psychopathological symptoms in problematic video game players: A person-centered approach. Front. Psychol. 2019, 10, 2559. [Google Scholar] [CrossRef]
- Guglielmucci, F.; Monti, M.; Franzoi, I.G.; Santoro, G.; Granieri, A.; Billieux, J.; Schimmenti, A. Dissociation in problematic gaming: A systematic review. Curr. Addict. Rep. 2019, 6, 1–14. [Google Scholar] [CrossRef]
- Fergus, T.A.; Spada, M.M. Cyberchondria: Examining relations with problematic internet use and metacognitive beliefs. Clin. Psychol. Psychother. 2017, 24, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Durak-Batigun, A.; Gor, N.; Komurcu, B.; Senkal-Erturk, I. Cyberchondria Scale (CS): Development, validity and reliability study. Dusunen Adam J. Psychiatry Neurol. Sci. 2018, 31, 148–162. [Google Scholar] [CrossRef]
- Selvi, Y.; Turan, S.G.; Sayin, A.A.; Boysan, M.; Kandeger, A. The Cyberchondria Severity Scale (CSS): Validity and reliability study of the Turkish version. Sleep Hypn. 2018, 20, 241–246. [Google Scholar] [CrossRef]
- Fergus, T.A.; Dolan, S.L. Problematic Internet use and Internet searches for medical information: The role of health anxiety. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Arsenakis, S.; Chatton, A.; Penzenstadler, L.; Billieux, J.; Berle, D.; Starcevic, V.; Viswasam, K.; Khazaal, Y. Unveiling the relationships between cyberchondria and psychopathological symptoms. J. Psychiatr. Res. 2021, 143, 254–261. [Google Scholar] [CrossRef]
- Bajcar, B.; Babiak, J. Self-esteem and cyberchondria: The mediation effects of health anxiety and obsessive–compulsive symptoms in a community sample. Curr. Psychol. 2021, 40, 2820–2831. [Google Scholar] [CrossRef]
- Zangoulechi, Z.; Yousefi, Z.; Keshavarz, N. The role of anxiety sensitivity, intolerance of uncertainty, and obsessive-compulsive symptoms in the prediction of cyberchondria. Adv. Biosci. Clin. Med. 2018, 6, 1–6. [Google Scholar] [CrossRef]
- Bajcar, B.; Babiak, J. Neuroticism and cyberchondria: The mediating role of intolerance of uncertainty and defensive pessimism. Personal. Individ. Diff. 2020, 162, 110006. [Google Scholar] [CrossRef]
- Norr, A.M.; Albanese, B.J.; Oglesby, M.E.; Allan, N.P.; Schmidt, N.B. Anxiety sensitivity and intolerance of uncertainty as potential risk factors for cyberchondria. J. Affect. Disord. 2015, 174, 64–69. [Google Scholar] [CrossRef]
- Fergus, T.A. Anxiety sensitivity and intolerance of uncertainty as potential risk factors for cyberchondria: A replication and extension examining dimensions of each construct. J. Affect. Disord. 2015, 184, 305–309. [Google Scholar] [CrossRef]
- Airoldi, S.; Kolubinski, D.C.; Nikčević, A.V.; Spada, M.M. The relative contribution of health cognitions and metacognitions about health anxiety to cyberchondria: A prospective study. J. Clin. Psychol. 2022, 78, 809–820. [Google Scholar] [CrossRef] [PubMed]
- Fergus, T.A.; Spada, M.M. Moving toward a metacognitive conceptualization of cyberchondria: Examining the contribution of metacognitive beliefs, beliefs about rituals, and stop signals. J. Anxiety Disord. 2018, 60, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Nadeem, F.; Malik, N.I.; Atta, M.; Ullah, I.; Martinotti, G.; Pettorruso, M.; Vellante, F.; Di Giannantonio, M.; De Berardis, D. Relationship between health-anxiety and cyberchondria: Role of metacognitive beliefs. J. Clin. Med. 2022, 11, 2590. [Google Scholar] [CrossRef]
- Zheng, H.; Kyung Kim, H.; Joanna Sin, S.-C.; Theng, Y.-L. A theoretical model of cyberchondria development: Antecedents and intermediate processes. Telemat. Inform. 2021, 63, 101659. [Google Scholar] [CrossRef]
- Starcevic, V.; Berle, D. Cyberchondria: Towards a better understanding of excessive health-related internet use. Expert Rev. Neurother. 2013, 13, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Pilowsky, I. Dimensions of hypochondriasis. Br. J. Psychiatry 1967, 113, 89–93. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Starcevic, V. Hypochondriasis and health anxiety: Conceptual challenges. Br. J. Psychiatry 2013, 202, 7–8. [Google Scholar] [CrossRef]
- Kumar, V.; Avasthi, A.; Grover, S. Correlates of worry and functional somatic symptoms in generalized anxiety disorder. Ind. Psychiatry J. 2019, 28, 29. [Google Scholar] [CrossRef]
- Lee, S.; Creed, F.H.; Ma, Y.-L.; Leung, C.M. Somatic symptom burden and health anxiety in the population and their correlates. J. Psychosom. Res. 2015, 78, 71–76. [Google Scholar] [CrossRef]
- den Boeft, M.; Twisk, J.W.R.; Terluin, B.; Penninx, B.W.J.H.; van Marwijk, H.W.J.; Numans, M.E.; van der Wouden, J.C.; van der Horst, H.E. The association between medically unexplained physical symptoms and health care use over two years and the influence of depressive and anxiety disorders and personality traits: A longitudinal study. BMC Health Serv. Res. 2016, 16, 100. [Google Scholar] [CrossRef] [Green Version]
- Fergus, T.A.; Kelley, L.P.; Griggs, J.O. The combination of health anxiety and somatic symptoms: A prospective predictor of healthcare usage in primary care. J. Behav. Med. 2019, 42, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Berle, D.; Starcevic, V.; Khazaal, Y.; Viswasam, K.; Hede, V.; McMullan, R.D. Relationships between online health information seeking and psychopathology. Gen. Hosp. Psychiatry 2020, 62, 96–97. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.-J.; Wang, D.-F.; Yuan, M.; Long, J.; Chen, S.-B.; Wu, Q.-X.; Wang, X.-Y.; Liu, T.-Q. The mediating effect of health anxiety in the relationship between functional somatic symptoms and illness behavior in chinese inpatients with depression. BMC Psychiatry 2019, 19, 260. [Google Scholar] [CrossRef] [PubMed]
- McElroy, E.; Shevlin, M. The development and initial validation of the Cyberchondria Severity Scale (CSS). J Anxiety Disord. 2014, 28, 259–265. [Google Scholar] [CrossRef] [PubMed]
- McElroy, E.; Kearney, M.; Touhey, J.; Evans, J.; Cooke, Y.; Shevlin, M. The CSS-12: Development and validation of a short-form version of the Cyberchondria Severity Scale. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 330–335. [Google Scholar] [CrossRef]
- Soraci, P.; Lagattolla, F.; Parente, G.; Guaitoli, E.; Cimaglia, R.; Del Fante, E.; Puoti, C. Analisi esplorativa della Cyberchondria Severity Scale Forma Breve (CSS-12) nel contesto italiano. Mente Cura 2019/2020, 184–206. [Google Scholar]
- Conti, L. Repertorio Delle Scale Di Valutazione in Psichiatria; S.E.E. Società Editrice Europea: Firenze, Italy, 2008. [Google Scholar]
- Fossati, A.; Borroni, S.; Del Corno, F. Livello 2—Sintomi Somatici—Adulto; Raffaello Cortina Editore: Milano, Italy, 2015. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom. Med. 2002, 64, 258–266. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2013. [Google Scholar]
- Kellner, R. Functional somatic symptoms and hypochondriasis: A survey of empirical studies. Arch. Gen. Psychiatry 1985, 42, 821–833. [Google Scholar] [CrossRef]
- Kellner, R. Hypochondriasis and somatization. JAMA Netw. 1987, 258, 2718–2722. [Google Scholar] [CrossRef]
- Groen, R.N.; van Gils, A.; Emerencia, A.C.; Bos, E.H.; Rosmalen, J.G.M. Exploring temporal relationships among worrying, anxiety, and somatic symptoms. J. Psychosom. Res. 2021, 146, 110293. [Google Scholar] [CrossRef]
- Murphy, K.M.; McGuire, A.P.; Erickson, T.M.; Mezulis, A.H. Somatic symptoms mediate the relationship between health anxiety and health-related quality of life over eight weeks. Stress Health 2017, 33, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Fergus, T.A. The Cyberchondria Severity Scale (CSS): An examination of structure and relations with health anxiety in a community sample. J. Anxiety Disord. 2014, 28, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Gibler, R.C.; Jastrowski Mano, K.E.; O’Bryan, E.M.; Beadel, J.R.; McLeish, A.C. The role of pain catastrophizing in cyberchondria among emerging adults. Psychol. Health Med. 2019, 24, 1267–1276. [Google Scholar] [CrossRef]
- McMullan, R.D.; Berle, D.; Arnáez, S.; Starcevic, V. The Relationships between health anxiety, online health information seeking, and cyberchondria: Systematic review and meta-analysis. J. Affect. Disord. 2019, 245, 270–278. [Google Scholar] [CrossRef]
- Starcevic, V.; Baggio, S.; Berle, D.; Khazaal, Y.; Viswasam, K. Cyberchondria and its relationships with related constructs: A network analysis. Psychiatr. Q. 2019, 90, 491–505. [Google Scholar] [CrossRef] [PubMed]
- Lamahewa, K.; Buszewicz, M.; Walters, K.; Marston, L.; Nazareth, I. Persistent unexplained physical symptoms: A prospective longitudinal cohort study in UK primary care. Br. J. Gen. Pract. 2019, 69, e246–e253. [Google Scholar] [CrossRef]
- Midolo, L.R.; Santoro, G.; Ferrante, E.; Pellegriti, P.; Russo, S.; Costanzo, A.; Schimmenti, A. Childhood trauma, attachment and psychopathology: A correlation network approach. Mediterr. J. Clin. Psychol. 2020, 8, 1–25. [Google Scholar] [CrossRef]
- MacSwain, K.L.H.; Sherry, S.B.; Stewart, S.H.; Watt, M.C.; Hadjistavropoulos, H.D.; Graham, A.R. Gender differences in health anxiety: An investigation of the interpersonal model of health anxiety. Personal. Individ. Diff. 2009, 47, 938–943. [Google Scholar] [CrossRef]
- Vismara, M.; Varinelli, A.; Pellegrini, L.; Enara, A.; Fineberg, N.A. New challenges in facing cyberchondria during the Coronavirus disease pandemic. Curr. Opin. Behav. Sci. 2022, 46, 101156. [Google Scholar] [CrossRef]
- Eslami, B.; Rosa, M.D.; Barros, H.; Torres-Gonzalez, F.; Stankunas, M.; Ioannidi-Kapolou, E.; Lindert, J.; Soares, J.J.F.; Lamura, G.; Melchiorre, M.G. Lifetime abuse and somatic symptoms among older women and men in europe. PLoS ONE 2019, 14, e0220741. [Google Scholar] [CrossRef]
- Kocalevent, R.-D.; Hinz, A.; Brähler, E. Standardization of a screening instrument (PHQ-15) for somatization syndromes in the general population. BMC Psychiatry 2013, 13, 91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerolimatos, L.A.; Edelstein, B.A. Predictors of health anxiety among older and young adults. Int. Psychogeriatr. 2012, 24, 1998–2008. [Google Scholar] [CrossRef] [PubMed]
- Diviani, N.; van den Putte, B.; Giani, S.; van Weert, J.C. Low health literacy and evaluation of online health information: A systematic review of the literature. J. Med. Internet Res. 2015, 17, e4018. [Google Scholar] [CrossRef]
- Starcevic, V.; Schimmenti, A.; Billieux, J.; Berle, D. Cyberchondria in the time of the COVID-19 pandemic. Hum. Behav. Emerg. Technol. 2021, 3, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.; Björgvinsson, T. Health anxiety and hypochondriasis: Description and treatment issues highlighted through a case illustration. Bull. Menninger. Clin. 2010, 74, 122–140. [Google Scholar] [CrossRef] [PubMed]
- McManus, F.; Surawy, C.; Muse, K.; Vazquez-Montes, M.; Williams, J.M.G. A randomized clinical trial of mindfulness-based cognitive therapy versus unrestricted services for health anxiety (hypochondriasis). J. Consult. Clin. Psychol. 2012, 80, 817–828. [Google Scholar] [CrossRef] [PubMed]
- Shires, A.; Sharpe, L.; Davies, J.N.; Newton-John, T.R.O. The efficacy of mindfulness-based interventions in acute pain: A systematic review and meta-analysis. Pain 2020, 161, 1698–1707. [Google Scholar] [CrossRef]
| Full Sample | Males | Females | |||||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 431) | (n = 158) | (n = 273) | |||||||
| M | (SD) | Range | M | (SD) | M | (SD) | t(429) | p | |
| Age | 34.64 | (12.01) | 18–74 | 35.78 | (12.20) | 34.01 | (11.88) | 1.48 | 0.14 |
| Years of education | 16.49 | (2.88) | 8–21 | 16.15 | (3.03) | 16.69 | (2.77) | −1.89 | 0.06 |
| Somatic symptoms | 7.59 | (5.07) | 0–24 | 5.16 | (4.26) | 9.00 | (4.97) | −8.12 | <0.01 |
| Health anxiety | 3.84 | (2.65) | 0–14 | 3.34 | (2.50) | 4.14 | (2.70) | −3.06 | <0.01 |
| Cyberchondria | 22.67 | (7.58) | 12–48 | 21.10 | (7.63) | 23.58 | (7.40) | −3.31 | <0.01 |
| 2. | 3. | 4. | 5. | |
|---|---|---|---|---|
| 1. Age | 0.08 | −0.17 ** | −0.17 ** | 0.06 |
| 2. Years of Education | ─ | −0.03 | −0.08 | −0.11 * |
| 3. Somatic symptoms | ─ | 0.55 ** | 0.40 ** | |
| 4. Health anxiety | ─ | 0.44 ** | ||
| 5. Cyberchondria | ─ |
| B | SE | Partial r | t | p | |
|---|---|---|---|---|---|
| Gender | 0.68 | 0.72 | 0.05 | 0.95 | 0.34 |
| Age | 0.03 | 0.03 | 0.05 | 0.98 | 0.33 |
| Years of education | −0.24 | 0.11 | −0.10 | −2.14 | 0.03 |
| Somatic symptoms | 0.32 | 0.08 | 0.19 | 4.00 | <0.01 |
| Health anxiety | 0.90 | 0.15 | 0.29 | 6.19 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santoro, G.; Starcevic, V.; Scalone, A.; Cavallo, J.; Musetti, A.; Schimmenti, A. The Doctor Is In(ternet): The Mediating Role of Health Anxiety in the Relationship between Somatic Symptoms and Cyberchondria. J. Pers. Med. 2022, 12, 1490. https://doi.org/10.3390/jpm12091490
Santoro G, Starcevic V, Scalone A, Cavallo J, Musetti A, Schimmenti A. The Doctor Is In(ternet): The Mediating Role of Health Anxiety in the Relationship between Somatic Symptoms and Cyberchondria. Journal of Personalized Medicine. 2022; 12(9):1490. https://doi.org/10.3390/jpm12091490
Chicago/Turabian StyleSantoro, Gianluca, Vladan Starcevic, Andrea Scalone, Josephin Cavallo, Alessandro Musetti, and Adriano Schimmenti. 2022. "The Doctor Is In(ternet): The Mediating Role of Health Anxiety in the Relationship between Somatic Symptoms and Cyberchondria" Journal of Personalized Medicine 12, no. 9: 1490. https://doi.org/10.3390/jpm12091490
APA StyleSantoro, G., Starcevic, V., Scalone, A., Cavallo, J., Musetti, A., & Schimmenti, A. (2022). The Doctor Is In(ternet): The Mediating Role of Health Anxiety in the Relationship between Somatic Symptoms and Cyberchondria. Journal of Personalized Medicine, 12(9), 1490. https://doi.org/10.3390/jpm12091490








