Efficacy and Safety of Setmelanotide, a Melanocortin-4 Receptor Agonist, for Obese Patients: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Data Extraction Search Strategy
2.4. Outcomes and Subgroup Analysis
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
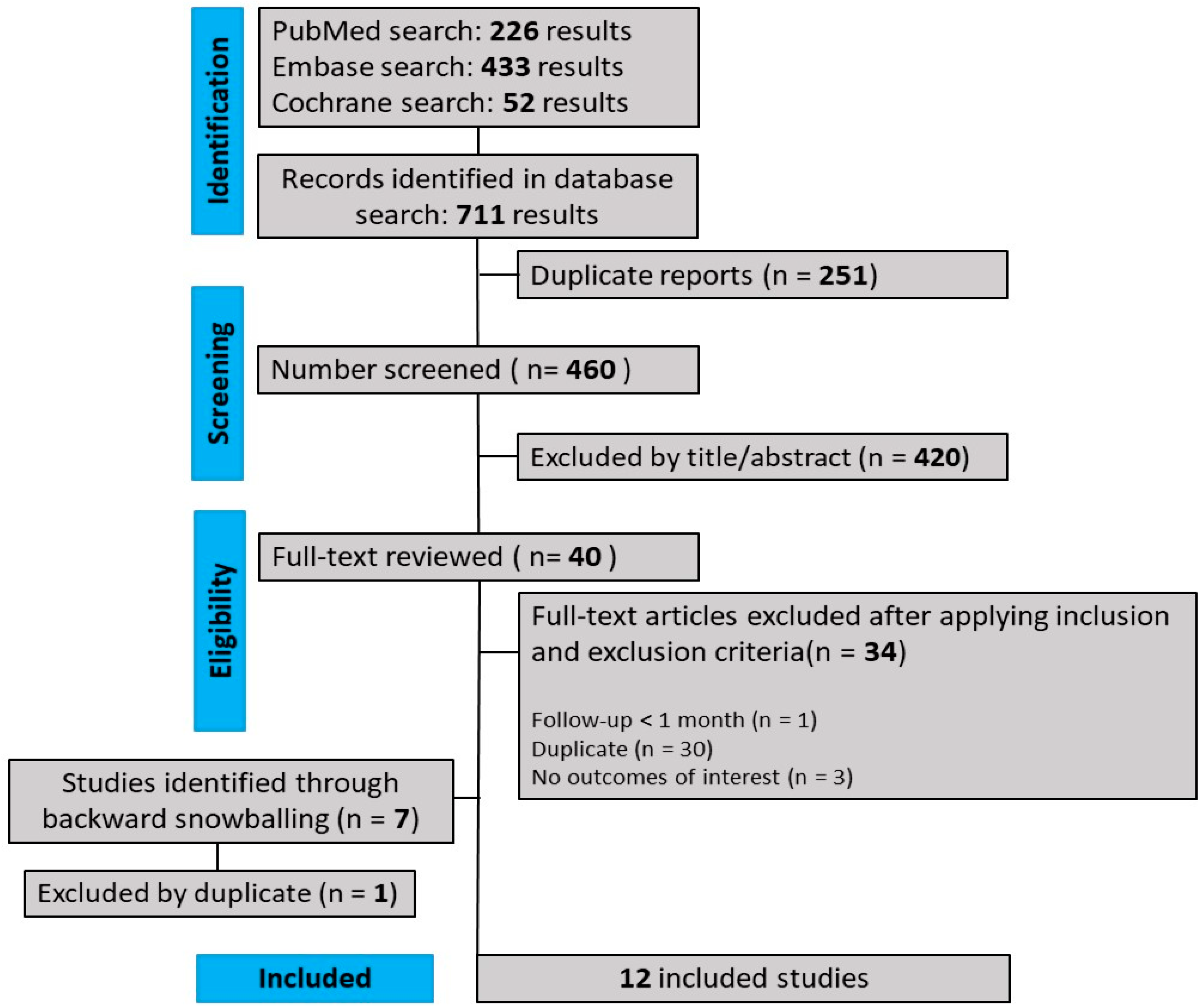
3.1. Study Selection and Baseline Characteristics
3.2. Pooled Analyses of All Studies
3.2.1. Effectiveness
Weight Loss
Average Weight and BMI Reduction
Hunger Score
3.2.2. Safety
3.3. Quality Assessment
3.4. Sensitivity Analysis
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Mayoral, L.-C.; Andrade, G.; Mayoral, E.-C.; Huerta, T.; Canseco, S.; Rodal Canales, F.; Cabrera-Fuentes, H.; Cruz, M.; Pérez Santiago, A.; Alpuche, J.; et al. Obesity Subtypes, Related Biomarkers & Heterogeneity. Indian J. Med. Res. 2020, 151, 11. [Google Scholar] [CrossRef] [PubMed]
- Dia Mundial da Obesidade 2022: Acelerar Ação Para Acabar Com a Obesidade—OPAS/OMS|Organização Pan-Americana da Saúde. Available online: https://www.paho.org/pt/noticias/4-3-2022-dia-mundial-da-obesidade-2022-acelerar-acao-para-acabar-com-obesidade (accessed on 22 March 2023).
- World Obesity Day Atlases|Obesity Atlas 2023. Available online: https://data.worldobesity.org/publications/?cat=19 (accessed on 9 September 2023).
- Melchior, V.; Fuchs, S.; Scantamburlo, G. Obesity and eating disorders. Rev. Med. Liege 2021, 76, 134–139. [Google Scholar] [PubMed]
- De Lorenzo, A.; Romano, L.; Di Renzo, L.; Di Lorenzo, N.; Cenname, G.; Gualtieri, P. Obesity: A Preventable, Treatable, but Relapsing Disease. Nutr. Burbank Los Angel. Cty. Calif 2020, 71, 110615. [Google Scholar] [CrossRef] [PubMed]
- Cignarella, A.; Busetto, L.; Vettor, R. Pharmacotherapy of Obesity: An Update. Pharmacol. Res. 2021, 169, 105649. [Google Scholar] [CrossRef] [PubMed]
- Clément, K.; van den Akker, E.; Argente, J.; Bahm, A.; Chung, W.K.; Connors, H.; De Waele, K.; Farooqi, I.S.; Gonneau-Lejeune, J.; Gordon, G.; et al. Efficacy and Safety of Setmelanotide, an MC4R Agonist, in Individuals with Severe Obesity Due to LEPR or POMC Deficiency: Single-Arm, Open-Label, Multicentre, Phase 3 Trials. Lancet Diabetes Endocrinol. 2020, 8, 960–970. [Google Scholar] [CrossRef]
- Haqq, A.M.; Chung, W.K.; Dollfus, H.; Haws, R.M.; Martos-Moreno, G.Á.; Poitou, C.; Yanovski, J.A.; Mittleman, R.S.; Yuan, G.; Forsythe, E.; et al. Efficacy and Safety of Setmelanotide, a Melanocortin-4 Receptor Agonist, in Patients with Bardet-Biedl Syndrome and Alström Syndrome: A Multicentre, Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial with an Open-Label Period. Lancet Diabetes Endocrinol. 2022, 10, 859–868. [Google Scholar] [CrossRef]
- Ju, S.H.; Yun, H.; Oh, Y.; Choi, Y.; Sohn, J.-W. Melanocortin-4 Receptors Activate Sympathetic Preganglionic Neurons and Elevate Blood Pressure via TRPV1. Cell Rep. 2022, 41, 111579. [Google Scholar] [CrossRef]
- Stutzmann, F.; Tan, K.; Vatin, V.; Dina, C.; Jouret, B.; Tichet, J.; Balkau, B.; Potoczna, N.; Horber, F.; O’Rahilly, S.; et al. Prevalence of Melanocortin-4 Receptor Deficiency in Europeans and Their Age-Dependent Penetrance in Multigenerational Pedigrees. Diabetes 2008, 57, 2511–2518. [Google Scholar] [CrossRef]
- Farooqi, I.S.; Keogh, J.M.; Yeo, G.S.H.; Lank, E.J.; Cheetham, T.; O’Rahilly, S. Clinical Spectrum of Obesity and Mutations in the Melanocortin 4 Receptor Gene. N. Engl. J. Med. 2003, 348, 1085–1095. [Google Scholar] [CrossRef]
- Collet, T.-H.; Dubern, B.; Mokrosinski, J.; Connors, H.; Keogh, J.M.; Mendes de Oliveira, E.; Henning, E.; Poitou-Bernert, C.; Oppert, J.-M.; Tounian, P.; et al. Evaluation of a Melanocortin-4 Receptor (MC4R) Agonist (Setmelanotide) in MC4R Deficiency. Mol. Metab. 2017, 6, 1321–1329. [Google Scholar] [CrossRef]
- Pressley, H.; Cornelio, C.K.; Adams, E.N. Setmelanotide: A Novel Targeted Treatment for Monogenic Obesity. J. Pharm. Technol. JPT Off. Publ. Assoc. Pharm. Tech. 2022, 38, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Ottawa Hospital Research Institute. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 10 August 2023).
- Argente, J.; Beales, P.; Clément, K.; Dollfus, H.; Forsythe, E.; Haqq, A.; Haws, R.; Martos-Moreno, G.; Mittleman, R.; Yanovski, J.; et al. ODP606 Long-Term Efficacy of Setmelanotide in Patients With Bardet-Biedl Syndrome. J. Endocr. Soc. 2022, 6, A14. [Google Scholar] [CrossRef]
- Argente, J.; Farooqi, S.; Chung, W.; Wabitsch, M.; Scimia, C.; Srinivasan, M.; Hu, S. RF24|PSUN91 Body Mass Index and Weight Reduction in Patients With SH2B1 Genetic Variant Obesity After One Year of Setmelanotide. J. Endocr. Soc. 2022, 6, A35. [Google Scholar] [CrossRef]
- Clément, K.; van den Akker, E.L.T.; Gordon, G.; Yuan, G.; Kühnen, P. Timing of Onset of Adverse Events With Setmelanotide, an MC4R Agonist, in Patients with Severe Obesity Due to LEPR or POMC Deficiency|Journal of the Endocrine Society|Oxford Academic. Available online: https://academic.oup.com/jes/article/5/Supplement_1/A30/6240595 (accessed on 27 August 2023).
- Farooqi, S.; Miller, J.; Ohayan, O.; Scimia, C.; Still, C.; Yohn, M.; Yuan, G.; Argente, J.; Buckley, B. OR10-1 Body Mass Index and Weight Reductions in Patients with Obesity Due to Heterozygous Variants in POMC, PCSK1, and LEPR after 1 Year of Setmelanotide. J. Endocr. Soc. 2022, 6, A15. [Google Scholar] [CrossRef]
- Farooqi, S.; Miller, J.L.; Ohayon, O.; Yuan, G.; Stewart, M.; Scimia, C.; Yanovski, J. Effects of Setmelanotide in Patients With POMC, PCSK1, or LEPR Heterozygous Deficiency Obesity in a Phase 2 Study. J. Endocr. Soc. 2021, 5, A669–A670. [Google Scholar] [CrossRef]
- Martos-Moreno, G.Á.; Argente, J.; Scimia, C.; Ohayan, O.; Yuan, G.; Farooqi, S. ODP605 Body Mass Index and Weight Reductions in Patients With SRC1 Genetic Variant Obesity after 1 Year of Setmelanotide. J. Endocr. Soc. 2022, 6, A13–A14. [Google Scholar] [CrossRef]
- Clément, K.; Biebermann, H.; Farooqi, I.S.; Van Der Ploeg, L.; Wolters, B.; Poitou, C.; Puder, L.; Fiedorek, F.; Gottesdiener, K.; Kleinau, G.; et al. MC4R Agonism Promotes Durable Weight Loss in Patients with Leptin Receptor Deficiency. Nat. Med. 2018, 24, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Haws, R.; Brady, S.; Davis, E.; Fletty, K.; Yuan, G.; Gordon, G.; Stewart, M.; Yanovski, J. Effect of Setmelanotide, a Melanocortin-4 Receptor Agonist, on Obesity in Bardet-Biedl Syndrome. Diabetes Obes. Metab. 2020, 22, 2133–2140. [Google Scholar] [CrossRef]
- RoB 2: A Revised Cochrane Risk-of-Bias Tool for Randomized Trials|Cochrane Bias. Available online: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed on 27 January 2023).
- GRADEpro. Available online: https://www.gradepro.org/ (accessed on 4 May 2023).
- OpenMeta[Analyst]—CEBM @ Brown. Available online: http://www.cebm.brown.edu/openmeta/ (accessed on 10 August 2023).
- Gordon, G.; Valles-Sukkar, A.; Yuan, G.; Stewart, M. A Randomized Trial of a Once-Weekly Formulation of Setmelanotide in Individuals with Obesity|Cochrane Library. Available online: https://www.cochranelibrary.com/central/doi/10.1002/central/CN-02259856/full (accessed on 5 May 2023).
- Kanti, V.; Puder, L.; Jahnke, I.; Krabusch, P.M.; Kottner, J.; Vogt, A.; Richter, C.; Andruck, A.; Lechner, L.; Poitou, C.; et al. A Melanocortin-4 Receptor Agonist Induces Skin and Hair Pigmentation in Patients with Monogenic Mutations in the Leptin-Melanocortin Pathway. Skin Pharmacol. Physiol. 2021, 34, 307–316. [Google Scholar] [CrossRef]
- Angelidi, A.M.; Belanger, M.J.; Kokkinos, A.; Koliaki, C.C.; Mantzoros, C.S. Novel Noninvasive Approaches to the Treatment of Obesity: From Pharmacotherapy to Gene Therapy. Endocr. Rev. 2022, 43, 507–557. [Google Scholar] [CrossRef]
- Loos, R.J.F.; Janssens, A.C.J.W. Predicting Polygenic Obesity Using Genetic Information. Cell Metab. 2017, 25, 535–543. [Google Scholar] [CrossRef]
- Variability in the Heritability of Body Mass Index: A Systematic Review and Meta-Regression—PMC. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3355836/ (accessed on 27 August 2023).
- Kühnen, P.; Clément, K.; Wiegand, S.; Blankenstein, O.; Gottesdiener, K.; Martini, L.L.; Mai, K.; Blume-Peytavi, U.; Grüters, A.; Krude, H. Proopiomelanocortin Deficiency Treated with a Melanocortin-4 Receptor Agonist. N. Engl. J. Med. 2016, 375, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.H. Drugs for Treating Obesity. Handb. Exp. Pharmacol. 2022, 274, 387–414. [Google Scholar] [CrossRef] [PubMed]
- Yanovski, S.Z.; Yanovski, J.A. Progress in Pharmacotherapy for Obesity. JAMA 2021, 326, 129–130. [Google Scholar] [CrossRef]
- Khera, R.; Murad, M.H.; Chandar, A.K.; Dulai, P.S.; Wang, Z.; Prokop, L.J.; Loomba, R.; Camilleri, M.; Singh, S. Association of Pharmacological Treatments for Obesity with Weight Loss and Adverse Events. JAMA 2016, 315, 2424–2434. [Google Scholar] [CrossRef]
- Smits, M.M.; Van Raalte, D.H. Safety of Semaglutide. Front. Endocrinol. 2021, 12, 645563. [Google Scholar] [CrossRef] [PubMed]
- Wilding, J.P.H.; Batterham, R.L.; Calanna, S.; Davies, M.; Van Gaal, L.F.; Lingvay, I.; McGowan, B.M.; Rosenstock, J.; Tran, M.T.D.; Wadden, T.A.; et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021, 384, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- Ladenheim, E.E. Liraglutide and Obesity: A Review of the Data so Far. Drug Des. Devel. Ther. 2015, 9, 1867–1875. [Google Scholar] [CrossRef]
- Lin, C.-H.; Shao, L.; Zhang, Y.-M.; Tu, Y.-J.; Zhang, Y.; Tomlinson, B.; Chan, P.; Liu, Z. An Evaluation of Liraglutide Including Its Efficacy and Safety for the Treatment of Obesity. Expert Opin. Pharmacother. 2020, 21, 275–285. [Google Scholar] [CrossRef]
- O’Neil, P.M.; Birkenfeld, A.L.; McGowan, B.; Mosenzon, O.; Pedersen, S.D.; Wharton, S.; Carson, C.G.; Jepsen, C.H.; Kabisch, M.; Wilding, J.P.H. Efficacy and Safety of Semaglutide Compared with Liraglutide and Placebo for Weight Loss in Patients with Obesity: A Randomised, Double-Blind, Placebo and Active Controlled, Dose-Ranging, Phase 2 Trial. Lancet 2018, 392, 637–649. [Google Scholar] [CrossRef]
- Rubino, D.M.; Greenway, F.L.; Khalid, U.; O’Neil, P.M.; Rosenstock, J.; Sørrig, R.; Wadden, T.A.; Wizert, A.; Garvey, W.T.; STEP 8 Investigators; et al. Effect of Weekly Subcutaneous Semaglutide vs Daily Liraglutide on Body Weight in Adults with Overweight or Obesity Without Diabetes: The STEP 8 Randomized Clinical Trial. JAMA 2022, 327, 138. [Google Scholar] [CrossRef] [PubMed]
- Forsythe, E.; Haws, R.M.; Argente, J.; Beales, P.; Martos-Moreno, G.Á.; Dollfus, H.; Chirila, C.; Gnanasakthy, A.; Buckley, B.C.; Mallya, U.G.; et al. Quality of Life Improvements Following One Year of Setmelanotide in Children and Adult Patients with Bardet–Biedl Syndrome: Phase 3 Trial Results. Orphanet J. Rare Dis. 2023, 18, 12. [Google Scholar] [CrossRef] [PubMed]
- Rhythm Pharmaceuticals Optimizes Design of EMANATE and DAYBREAK Clinical Trials to Advance Setmelanotide for Rare Genetic Diseases of Obesity|Rhythm Pharmaceuticals, Inc. Available online: https://ir.rhythmtx.com/news-releases/news-release-details/rhythm-pharmaceuticals-optimizes-design-emanate-and-daybreak/ (accessed on 20 August 2023).

| Study (Years) | Follow-Up (Weeks) | Age, Years (Mean) | Sex n (%) | Syndromes | Weight, kg (Mean) | BMI, kg/m2 (Mean) | BMI Score kg/m2 (Mean) | N. of Patients (Int./Placebo) | Total | Doses (mg) | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Argente I 2022 *a [15] | 78–104 | NA | NA | BBS | 132 (20.9) | 42.2 (9.2) | 3.5 (0.76) | 54/- | 54 | NA | 8 |
| Argente II 2022 *a [16] | 26–52 | NA | NA | SH2B1/16p11.2 | 139.7 (35.4) | 47.2 (12.8) | 3.56 (0.60) | 35/- | 35 | NA | 8 |
| Clément 2018 [21] | 45–61 | 19.66 (4.93) | Male: 2 (67) Fem.: 1 (33) | POMC/LEPR | 124.43 (5.39) | 41.6 (2.28) | NA | 3/- | 3 | 0.5–2.5 | 8 |
| Clément 2020 *b [7] | 52 | 21.1 (7.74) | Male: 8 (38) Fem.: 13 (62) | POMC/LEPR | 126.3 (32.0) | 44.4 (10.3) | NA | 21/21 *c | 21 | 0.5–3 | 9 |
| Clément 2021 *b [17] | 12–52 | NA | NA | POMC/PCSK /LEPR | NA | NA | NA | 35/- | 35 | 0.25–3 | 9 |
| Collet 2017 [12] | 4 | NA | NA | POMC | 110.64 (23.39) | NA | NA | 11/5 | 16 | 0.01 kg/dia | - |
| Farooqi 2021 *d [19] | 4–12 | 39.5 (17.6) | NA | POMC/PCSK1/LEPR | NA | 50.3 (9.4) | NA | 35/- | 35 | 3 | 8 |
| Farooqi 2022 *a [18] | 26–52 | NA | NA | POMC/PCSK1/LEPR | 142.97 (28.70) | 50.2 (9.41) | 4.04 (0.65) | 35/- | 35 | NA | 8 |
| Gordon 2020 [26] | 12 | 40.5 (8.5) | Male: 22 (26) Fem.: 63 (74) | POMC/LEPR/BBS/ALSTROM | 126.6 (20.8) | 45.7 (5.6) | NA | 61/24 | 85 | 2 mg QD 30 mg QW | - |
| Haqq 2022 [8] | 52 | 19.8 (10.2) | Male: 5 (39) Fem.: 23 (61) | BBS/ ALSTROM | 111.7 (30.4) | 42.3 (11.0) | NA | 19/19 | 38 | 3 | - |
| Haws 2020 *d [22] | 52 | 22.5 (14.7) | Male: 4 (40) Fem.: 6 (60) | BBS | 128.1 (28.6) | 44.8 (4.1) | NA | 10/- | 10 | 0.5–3 | 8 |
| Moreno 2022 *a [20] | 26–52 | NA | NA | SRC1 | 139.7 (25.1) | 45.4 (11.3) | 2.99 (0.63) | 30/- | 30 | NA | 8 |
| Outcomes | Studies | No. of Patients | MD or OR | 95% CI | Heterogeneity | |||
|---|---|---|---|---|---|---|---|---|
| Tau2 | df | p-Value | I2 (%) | |||||
| Weight loss | 11 | 197 | −6.915 | [−8.489, −5.341] | 3.939 | 10 | <0.001 | 92.043 |
| BMI (kg/m2) | 7 | 72 | −10.55 | [−12.954, −8.161] | 4.002 | 6 | 0.126 | 39.756 |
| BMIscore (kg/m2) | 6 | 45 | −0.610 | [−1.372, 0.152] | 0.863 | 5 | 0.126 | 99.156 |
| Adverse events | ||||||||
| Hunger score | 5 | 115 | −35.61 | [−60.61, −10.61] | 779.89 | 4 | <0.001 | 97.727 |
| Hyperpigmentation | 6 | 131 | 0.692 | [0.575, 0.809] | 0.013 | 5 | 0.008 | 67.811 |
| Headache | 5 | 50 | 0.277 | [0.122, 0.433] | 0.025 | 4 | <0.001 | 81.383 |
| Nausea | 6 | 85 | 0.390 | [0.248, 0.533] | 0.024 | 5 | <0.001 | 77.048 |
| Vomiting | 5 | 38 | 0.207 | [0.103, 0.312] | 0.009 | 4 | 0.029 | 62.957 |
| ISRs | 4 | 78 | 0.816 | [0.616, 1.017] | 0.028 | 2 | <0.001 | 88.714 |
| Sexual dysfunction | 4 | 12 | 0.074 | [0.014, 0.135] | 0.002 | 3 | 0.149 | 43.679 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferraz Barbosa, B.; Aquino de Moraes, F.C.; Bordignon Barbosa, C.; Palavicini Santos, P.T.K.; Pereira da Silva, I.; Araujo Alves da Silva, B.; Cristine Marques Barros, J.; Rodríguez Burbano, R.M.; Pereira Carneiro dos Santos, N.; Rodrigues Fernandes, M. Efficacy and Safety of Setmelanotide, a Melanocortin-4 Receptor Agonist, for Obese Patients: A Systematic Review and Meta-Analysis. J. Pers. Med. 2023, 13, 1460. https://doi.org/10.3390/jpm13101460
Ferraz Barbosa B, Aquino de Moraes FC, Bordignon Barbosa C, Palavicini Santos PTK, Pereira da Silva I, Araujo Alves da Silva B, Cristine Marques Barros J, Rodríguez Burbano RM, Pereira Carneiro dos Santos N, Rodrigues Fernandes M. Efficacy and Safety of Setmelanotide, a Melanocortin-4 Receptor Agonist, for Obese Patients: A Systematic Review and Meta-Analysis. Journal of Personalized Medicine. 2023; 13(10):1460. https://doi.org/10.3390/jpm13101460
Chicago/Turabian StyleFerraz Barbosa, Bárbara, Francisco Cezar Aquino de Moraes, Camila Bordignon Barbosa, Plínio Takashi Karubi Palavicini Santos, Izael Pereira da Silva, Bruno Araujo Alves da Silva, Jamile Cristine Marques Barros, Rommel Mario Rodríguez Burbano, Ney Pereira Carneiro dos Santos, and Marianne Rodrigues Fernandes. 2023. "Efficacy and Safety of Setmelanotide, a Melanocortin-4 Receptor Agonist, for Obese Patients: A Systematic Review and Meta-Analysis" Journal of Personalized Medicine 13, no. 10: 1460. https://doi.org/10.3390/jpm13101460










