Urinary Liver-Type Fatty Acid Binding Protein, a Biomarker for Disease Progression, Dialysis and Overall Mortality in Chronic Kidney Disease
Abstract
:1. Introduction
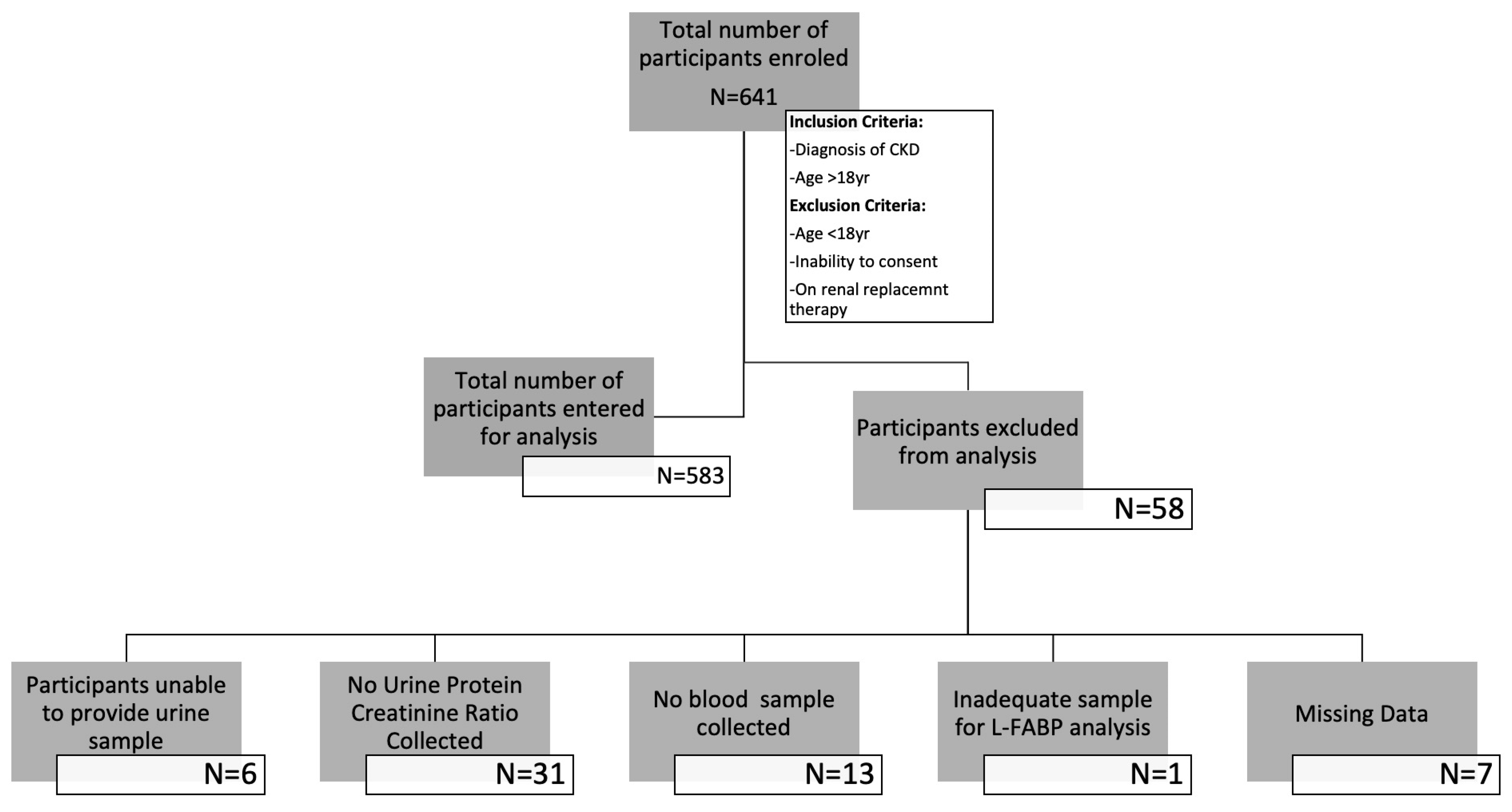
2. Materials and Methods
2.1. Definitions
2.2. Study Population Size
2.3. Data Collection
2.4. Blood Sampling, eGFR Calculation and CKD Classification
2.5. Urine Sampling and Analysis
2.6. ELISA Analysis for the Measurement of uL-FABP Levels
2.7. Statistical Analysis
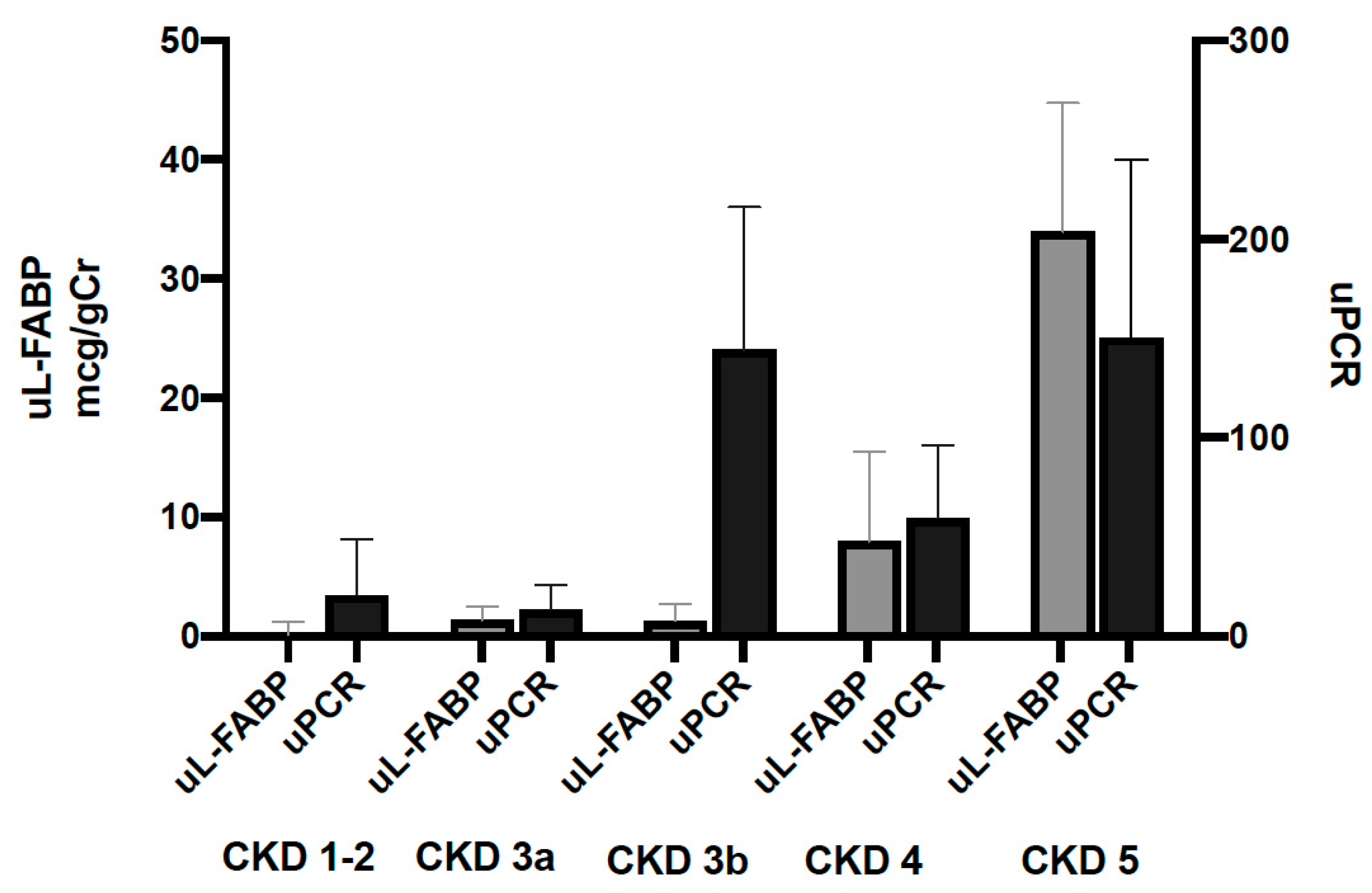
3. Results
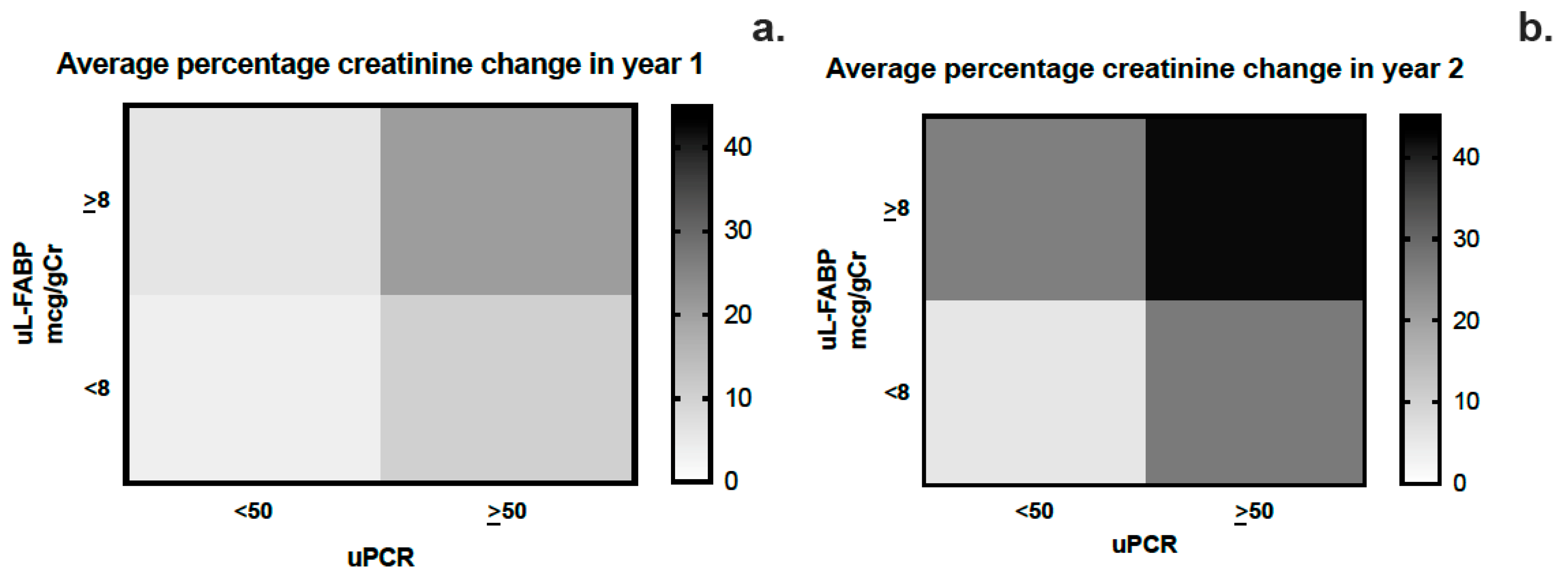
3.1. Year 1 and 2 Analysis
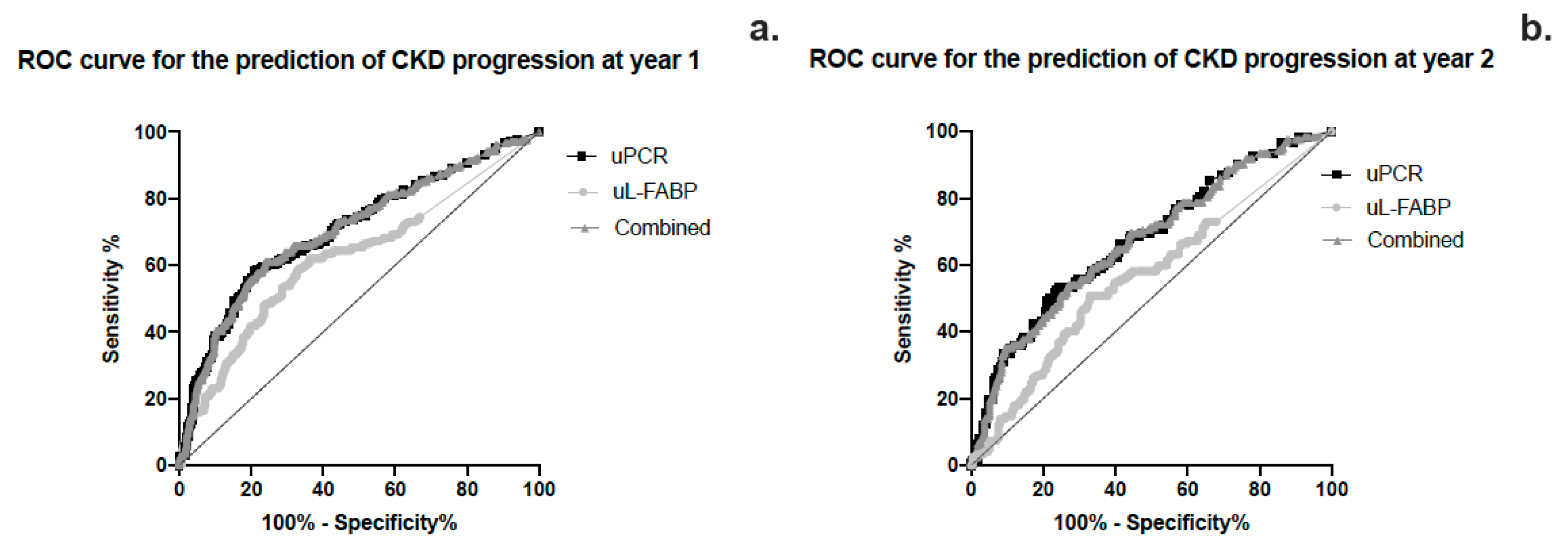
3.2. Sensitivity and Specificity
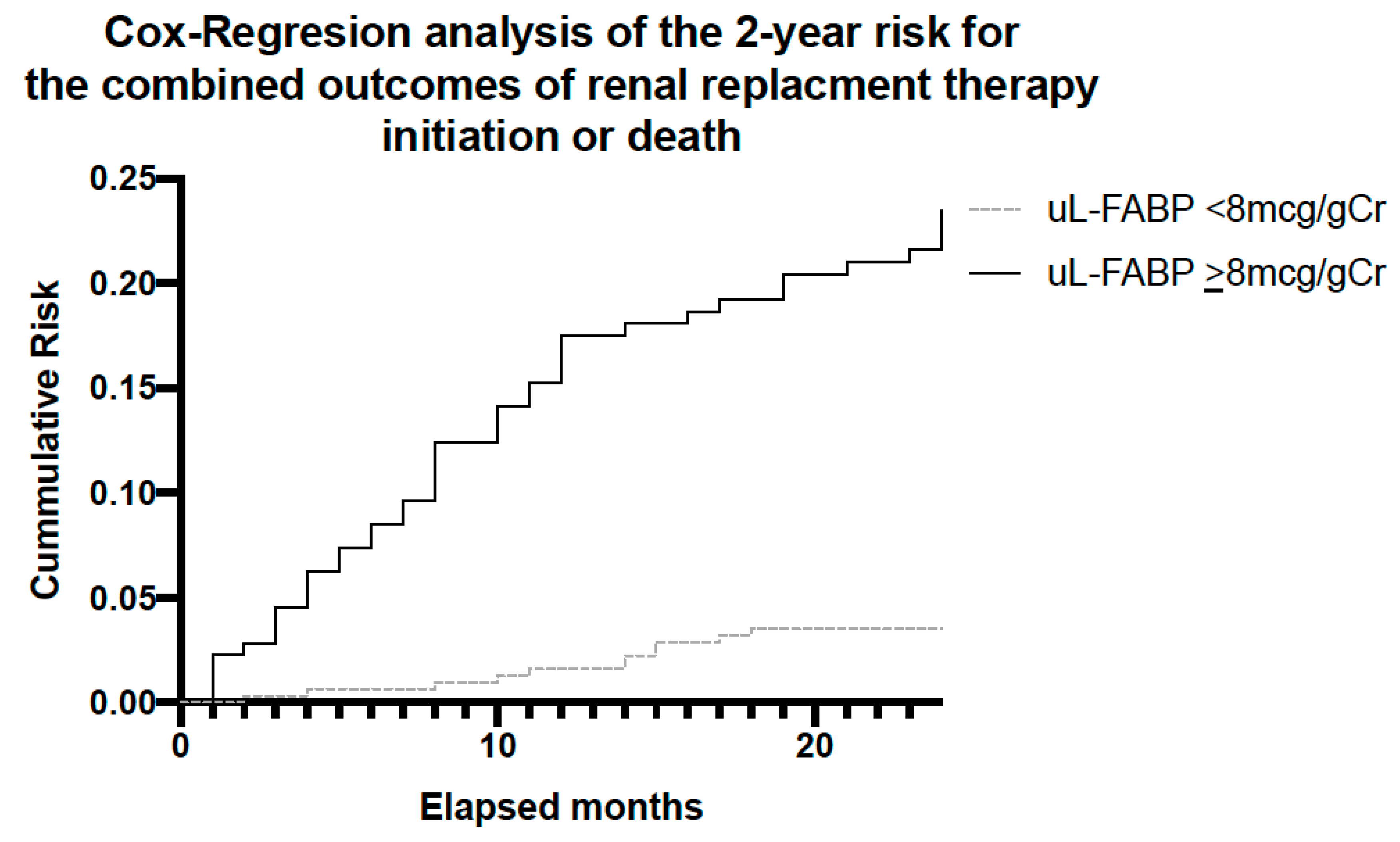
3.3. Mortality and RRT Initiation Risk Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- James, M.T.; Hemmelgarn, B.R.; Tonelli, M. Early recognition and prevention of chronic kidney disease. Lancet 2010, 375, 1296–1309. [Google Scholar] [CrossRef]
- NICE. Chronic Kidney Disease in Adults: Assessment and Management|Guidance and Guidelines|NICE. Chronic Kidney Dis. Adults Assess. Manag. 2014, 1–63. Available online: https://www.nice.org.uk/guidance/cg182/chapter/1-Recommendations#referral-criteria (accessed on 24 July 2017).
- Recommendations|Chronic Kidney Disease: Assessment and Management|Guidance|NICE. Available online: https://www.nice.org.uk/guidance/ng203/chapter/Recommendations#managing-anaemia (accessed on 6 October 2023).
- Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M.; et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- De Nicola, L.; Zoccali, C. Chronic kidney disease prevalence in the general population: Heterogeneity and concerns. Nephrol. Dial. Transplant. 2016, 31, 331–335. [Google Scholar] [CrossRef]
- Inker, L.A.; Astor, B.C.; Fox, C.H.; Isakova, T.; Lash, J.P.; Peralta, C.A.; Kurella Tamura, M.; Feldman, H.I. KDOQI US Commentary on the 2012 KDIGO Clinical Practice Guideline for the Evaluation and Management of CKD. Am. J. Kidney Dis. 2014, 63, 713–735. [Google Scholar] [CrossRef]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A More Accurate Method to Estimate Glomerular Filtration Rate from Serum Creatinine: A New Prediction Equation. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Zhang, A.-H.; Tam, P.; LeBlanc, D.; Zhong, H.; Chan, C.T.; Bargman, J.M.; Oreopoulos, D.G. Natural history of CKD stage 4 and 5 patients following referral to renal management clinic. Int. Urol. Nephrol. 2009, 41, 977–982. [Google Scholar] [CrossRef]
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D.R. Global Prevalence of Chronic Kidney Disease—A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef]
- Eriksen, B.; Ingebretsen, O. The progression of chronic kidney disease: A 10-year population-based study of the effects of gender and age. Kidney Int. 2006, 69, 375–382. [Google Scholar] [CrossRef]
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.-M.; Yang, C.-W. Chronic kidney disease: Global dimension and perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef]
- Garg, A.X.; Clark, W.F.; Haynes, R.B.; House, A.A. Moderate renal insufficiency and the risk of cardiovascular mortality: Results from the NHANES I. Kidney Int. 2002, 61, 1486–1494. [Google Scholar] [CrossRef] [PubMed]
- Weiner, D.E.; Tighiouart, H.; Amin, M.G.; Stark, P.C.; MacLeod, B.; Griffith, J.L.; Salem, D.N.; Levey, A.S.; Sarnak, M.J. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: A pooled analysis of community-based studies. J. Am. Soc. Nephrol. 2004, 15, 1307–1315. [Google Scholar] [CrossRef] [PubMed]
- Fassett, R.G.; Venuthurupalli, S.K.; Gobe, G.C.; Coombes, J.S.; Cooper, M.A.; Hoy, W.E. Biomarkers in chronic kidney disease: A review. Kidney Int. 2011, 80, 806–821. [Google Scholar] [CrossRef]
- Cameron, S. Proteinuria and Progression in Human Glomerular Diseases. Am. J. Nephrol. 1990, 10, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Keane, W.F.; Brenner, B.M.; de Zeeuw, D.; Grunfeld, J.-P.; McGill, J.; Mitch, W.E.; Ribeiro, A.B.; Shahinfar, S.; Simpson, R.L.; Snapinn, S.M.; et al. The risk of developing end-stage renal disease in patients with type 2 diabetes and nephropathy: The RENAAL Study. Kidney Int. 2003, 63, 1499–1507. [Google Scholar] [CrossRef]
- Levey, A.S.; Cattran, D.; Friedman, A.; Miller, W.G.; Sedor, J.; Tuttle, K.; Kasiske, B.; Hostetter, T. Proteinuria as a Surrogate Outcome in CKD: Report of a Scientific Workshop Sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am. J. Kidney Dis. 2009, 54, 205–226. [Google Scholar] [CrossRef]
- Ichikawa, D.; Kamijo-Ikemori, A.; Sugaya, T.; Shibagaki, Y.; Yasuda, T.; Hoshino, S.; Katayama, K.; Igarashi-Migitaka, J.; Hirata, K.; Kimura, K. Human liver-type fatty acid–binding protein protects against tubulointerstitial injury in aldosterone-induced renal injury. Am. J. Physiol. Physiol. 2015, 308, F114–F121. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Xie, Y.; Shao, X.; Ni, Z.; Mou, S. L-FABP: A novel biomarker of kidney disease. Clin. Chim. Acta 2015, 445, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Susantitaphong, P.; Siribamrungwong, M.; Doi, K.; Noiri, E.; Terrin, N.; Jaber, B.L. Performance of Urinary Liver-Type Fatty Acid–Binding Protein in Acute Kidney Injury: A Meta-analysis. Am. J. Kidney Dis. 2013, 61, 430–439. [Google Scholar] [CrossRef]
- Suzuki, G.; Ichibayashi, R.; Yamamoto, S.; Nakamichi, Y.; Watanabe, M.; Honda, M. Clinical significance of urinary L-FABP in the emergency department. Int. J. Emerg. Med. 2019, 12, 24. [Google Scholar] [CrossRef] [PubMed]
- Kamijo-Ikemori, A.; Sugaya, T.; Ichikawa, D.; Hoshino, S.; Matsui, K.; Yokoyama, T.; Yasuda, T.; Hirata, K.; Kimura, K. Urinary liver type fatty acid binding protein in diabetic nephropathy. Clin. Chim. Acta 2013, 424, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Kamijo-Ikemori, A.; Sugaya, T.; Yasuda, T.; Kawata, T.; Ota, A.; Tatsunami, S.; Kaise, R.; Ishimitsu, T.; Tanaka, Y.; Kimura, K. Clinical significance of urinary liver-type fatty acid-binding protein in diabetic nephropathy of type 2 diabetic patients. Diabetes Care 2011, 34, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Ngan, D.T.T.; Binh, N.G.; Lan, L.T.H.; Nguyen, C.T.T.; Huong, P.T. Evaluation of urinary L-FABP as an early marker for diabetic nephropathy in type 2 diabetic patients. J. Med. Biochem. 2019, 39, 224–230. [Google Scholar] [CrossRef]
- Kamijo, A.; Sugaya, T.; Hikawa, A.; Yamanouchi, M.; Hirata, Y.; Ishimitsu, T.; Numabe, A.; Takagi, M.; Hayakawa, H.; Tabei, F.; et al. Urinary liver-type fatty acid binding protein as a useful biomarker in chronic kidney disease. Mol. Cell. Biochem. 2006, 284, 175–182. [Google Scholar] [CrossRef]
- Katoh, H.; Nozue, T.; Kimura, Y.; Nakata, S.; Iwaki, T.; Kawano, M.; Kawashiri, M.-A.; Michishita, I.; Yamagishi, M. Elevation of urinary liver-type fatty acid-binding protein as predicting factor for occurrence of contrast-induced acute kidney injury and its reduction by hemodiafiltration with blood suction from right atrium. Heart Vessel. 2013, 29, 191–197. [Google Scholar] [CrossRef]
- Shingai, N.; Morito, T.; Najima, Y.; Igarashi, A.; Kobayashi, T.; Doki, N.; Kakihana, K.; Ohashi, K.; Ando, M. Urinary Liver-Type Fatty Acid-Binding Protein Linked with Increased Risk of Acute Kidney Injury after Allogeneic Stem Cell Transplantation. Biol. Blood Marrow Transplant. 2014, 20, 2010–2014. [Google Scholar] [CrossRef]
- Davies, S.J.; Russell, L.; Bryan, J.; Phillips, L.; Russell, G.I. Comorbidity, urea kinetics, and appetite in continuous ambulatory peritoneal dialysis patients: Their interrelationship and prediction of survival. Am. J. Kidney Dis. 1995, 26, 353–361. [Google Scholar] [CrossRef]
- National Kidney Foundation. K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Clasification and Stratification. Am. J. Kidney Dis. 2002, 39 (Suppl. S1), S1–S266. [Google Scholar]
- Tangri, N.; Stevens, L.A.; Griffith, J.; Tighiouart, H.; Djurdjev, O.; Naimark, D.; Levin, A.; Levey, A.S. A Predictive Model for Progression of Chronic Kidney Disease to Kidney Failure. JAMA 2011, 305, 1553–1559. [Google Scholar] [CrossRef]
- Viswanathan, G.; Upadhyay, A. Assessment of Proteinuria. Adv. Chronic Kidney Dis. 2011, 18, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Cravedi, P.; Remuzzi, G. Pathophysiology of proteinuria and its value as an outcome measure in CKD. Br. J. Clin. Pharmacol. 2013, 76, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Sarnak, M.J.; Astor, B.C. Implications of Proteinuria: CKD Progression and Cardiovascular Outcomes. Adv. Chronic Kidney Dis. 2011, 18, 258–266. [Google Scholar] [CrossRef]
- Pajek, J.; Škoberne, A.; Šosterič, K.; Adlešič, B.; Leskošek, B.; Pajek, M.B.; Osredkar, J.; Lindič, J. Non-inferiority of creatinine excretion rate to urinary L-FABP and NGAL as predictors of early renal allograft function. BMC Nephrol. 2014, 15, 117. [Google Scholar] [CrossRef]
- Zeng, X.-F.; Li, J.-M.; Tan, Y.; Wang, Z.-F.; He, Y.; Chang, J.; Zhang, H.; Zhao, H.; Bai, X.; Xie, F.; et al. Performance of urinary NGAL and L-FABP in predicting acute kidney injury and subsequent renal recovery: A cohort study based on major surgeries. Clin. Chem. Lab. Med. 2014, 52, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Holzscheiter, L.; Beck, C.; Rutz, S.; Manuilova, E.; Domke, I.; Guder, W.G.; Hofmann, W. NGAL, L-FABP, and KIM-1 in comparison to established markers of renal dysfunction. Clin. Chem. Lab. Med. 2014, 52, 537–546. [Google Scholar] [CrossRef]
- Fufaa, G.D.; Weil, E.J.; Nelson, R.G.; Hanson, R.L.; Bonventre, J.V.; Sabbisetti, V.; Waikar, S.S.; Mifflin, T.E.; Zhang, X.; Xie, D.; et al. Association of urinary KIM-1, L-FABP, NAG and NGAL with incident end-stage renal disease and mortality in American Indians with type 2 diabetes mellitus. Diabetologia 2015, 58, 188–198. [Google Scholar] [CrossRef]
- Parr, S.K.; Clark, A.J.; Bian, A.; Shintani, A.K.; Wickersham, N.E.; Ware, L.B.; Ikizler, T.A.; Siew, E.D. Urinary L-FABP predicts poor outcomes in critically ill patients with early acute kidney injury. Kidney Int. 2015, 87, 640–648. [Google Scholar] [CrossRef]
- Parikh, C.R.; Thiessen-Philbrook, H.; Garg, A.X.; Kadiyala, D.; Shlipak, M.G.; Koyner, J.L.; Edelstein, C.L.; Devarajan, P.; Patel, U.D.; Zappitelli, M.; et al. Performance of kidney injury molecule-1 and liver fatty acid-binding protein and combined biomarkers of AKI after cardiac surgery. Clin. J. Am. Soc. Nephrol. 2013, 8, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Kokot, M.; Biolik, G.; Ziaja, D.; Fojt, T.; Kedzierski, L.; Antoniak, K.; Janowska, M.; Pawlicki, K.; Ziaja, K.; Dulawa, J. Assessment of subclinical acute kidney injury after abdominal aortic aneurysm surgery using novel markers: L-FABP and H-FABP. Nefrologia 2014, 34, 628–636. [Google Scholar]
- Hwang, Y.J.; Hyun, M.C.; Choi, B.S.; Chun, S.Y.; Cho, M.H. Acute kidney injury after using contrast during cardiac catheterization in children with heart disease. J. Korean Med. Sci. 2014, 29, 1102–1107. [Google Scholar] [CrossRef] [PubMed]
- Kamijo, A.; Kimura, K.; Sugaya, T.; Yamanouchi, M.; Hikawa, A.; Hirano, N.; Hirata, Y.; Goto, A.; Omata, M. Urinary fatty acid–binding protein as a new clinical marker of the progression of chronic renal disease. J. Lab. Clin. Med. 2004, 143, 23–30. [Google Scholar] [CrossRef] [PubMed]

| Demographics | Baseline | 1 Year | 2 Year | |
|---|---|---|---|---|
| N | 583 | 484 | 335 | |
| CKD stage | 1–2 | 14.6% | 13.6% | 7.8% |
| 3A | 13.3% | 12.8% | 15.6% | |
| 3B | 24.8% | 24.8% | 29.0% | |
| 4 | 32.8% | 33.5% | 38.3% | |
| 5 | 14.6% | 15.3% | 9.3% | |
| Age (yrs) | 65 (51; 75) | 65 (51; 74) | 65 (52; 74) | |
| Sex: Male | 56% | 55.8% | 54.0% | |
| Ethnicity | White | 78.3% | 78.3% | 79.4% |
| Black | 3.8% | 3.7% | 3.6% | |
| Asian | 8.5% | 9.1% | 9.0% | |
| Chinese | 1.0% | 1.2% | 1.2% | |
| Other | 6.6% | 6.0% | 5.7% | |
| Unspecified | 1.7% | 1.7% | 1.2% | |
| Primary CKD Pathology | ADPKD | 8.1% | 8.5% | 9.0% |
| Diabetic Nephropathy | 10.7% | 10.7% | 9.6% | |
| Glomerulonepgritis | 16.5% | 17.6% | 17.3% | |
| Acute/Chronic TIN | 3.3% | 3.7% | 4.8% | |
| Obstructive/Stones/Reflux | 10.7% | 10.7% | 10.4% | |
| Renovascular/HTN/Ischaemic | 12.8% | 12.4% | 11.3% | |
| Vasculitis/SLE | 9.9% | 11.0% | 13.4% | |
| Myeloma | 1.4% | 1.4% | 1.2% | |
| Hereditary Nephropathy | 0.7% | 0.8% | 0.6% | |
| Other | 9.4% | 8.3% | 9.0% | |
| Uncertain Aetiology | 16.5% | 14.9% | 13.4% | |
| Cardiovascular Disease | 21.5% | 20.2% | 18.8% | |
| Diabetes Mellitus | 29.1% | 28.5% | 26.9% | |
| Davies’ Comorbidity Score | 1 (1; 2) | 1 (1; 2) | 1 (1; 2) | |
| Number of Medications | 7 (4; 9) | 7 (4; 9) | 7 (4; 9) | |
| Number of Blood Pressure Medications | 2 (1; 3) | 2 (1; 3) | 2 (1; 3) | |
| ACEi/ARB | ACEi | 33.4% | 34.1% | 34.4% |
| ARB | 21.5% | 22.3% | 25.4% | |
| Both | 2.4% | 2.5% | 2.4% | |
| Aldosterone Inhibitors | 2.6% | 2.1% | 2.4% | |
| Serum Creatinine (mmol/L) | 173 (199; 265) | 174 (124; 268) | 169 (126; 238) | |
| MDRD eGFR (mL/min/1.73 m2) | 31 (19; 46) | 30 (18; 46) | 31 (21; 46) | |
| uPCR mg/gCr | 40 (11; 147) | 42 (12; 152) | 36 (11; 128) | |
| uL-FABP ELISA (mcg/gCr) | 2.79 (0; 19.4) | 3.49 (0; 19.6) | 2.68 (0; 16.4) | |
| Outcome: MDRD eGFR (Log10 eGFR) | ||||||
|---|---|---|---|---|---|---|
| Unadjusted (R2 = 0.169) | +Age (R2 = 0.313) | +Age, Sex (R2 = 0.317) | ||||
| Beta (95% CI) | Sig | Beta (95% CI) | Sig | Beta (95% CI) | Sig | |
| uPCR | −0.178 (−0.257; −0.096) | <0.001 * | −0.216 (−0.228; −0.140) | <0.001 * | −0.216 (−0.289; −0.141) | <0.001 * |
| uL-FABP | −0.313 (−0.392; −0.231) | <0.001 * | −0.300 (−0.372; −0.225) | <0.001 * | −0.300 (−0.372; −0.225) | <0.001 * |
| Outcome: Serum Creatinine (Log10 serum creatinine) | ||||||
| Unadjusted (R2 = 0.173) | +Age (R2 = 0.268) | +Age, Sex (R2 = 0.312) | ||||
| Beta (95% CI) | Sig | Beta (95% CI) | Sig | Beta (95% CI) | Sig | |
| uPCR | 0.185 (0.104; 0.265) | <0.001 * | 0.216 (0.139; 0.291) | <0.001 * | 0.211 (0.135; 0.284) | <0.001 * |
| uL-FABP | 0.312 (0.230; 0.392) | <0.001 * | 0.302 (0.225; 0.377) | <0.001 * | 0.307 (0.231; 0.379) | <0.001 * |
| Demographics | CKD Progression | No CKD Progression | p-Value | |
|---|---|---|---|---|
| N | 208 | 276 | ||
| CKD stage | 1–2 | 8.5% | 11.3% | <0.001 * |
| 3A | 7.5% a | 17.7% | ||
| 3B | 18.5% | 31.3% | ||
| 4 | 40.5% | 30.6% | ||
| 5 | 25.0% b | 9.1% | ||
| Age (yrs) | 63 (50; 74) | 66 (53; 75) | 0.233 | |
| Sex: Male | 55.3% | 56.2% | 0.849 | |
| Ethnicity | White | 77.4% | 79.0% | 0.332 |
| Black | 4.8% | 2.9% | ||
| Asian | 9.6% | 8.7% | ||
| Chinese | 1.9% | 0.7% | ||
| Other | 5.8% | 6.2% | ||
| Unspecified | 0.5% | 2.5% | ||
| Primary CKD Pathology | ADPKD | 11.1% | 6.5% | 0.042 *c |
| Diabetic Nephropathy | 13.5% | 8.7% | ||
| Glomerulonepgritis | 18.3% | 17.0% | ||
| Acute/Chronic TIN | 2.9% | 4.3% | ||
| Obstructive/Stones/Reflux | 12.0% | 9.8% | ||
| Renovascular/HTN/ Ischaemic | 12.0% | 12.7% | ||
| Vasculitis/SLE | 6.7% | 14.1% | ||
| Myeloma | 2.4% | 0.7% | ||
| Hereditary Nephropathy | 1.4% | 0.4% | ||
| Other | 7.7% | 8.7% | ||
| Uncertain Aetiology | 12.0% | 17.0% | ||
| Cardiovascular Disease | 20.7% | 19.9% | 0.840 | |
| Diabetes Mellitus | 32.7% | 25.4% | 0.077 | |
| Davies’ Comorbidity Score | 1 (1; 2) | 1 (1; 2) | 0.718 | |
| ACEi/A2RB | ACEi | 33.4% | 22.3% | 0.560 |
| A2RB | 21.5% | 21.8% | 0.742 | |
| Both | 2.4% | 3.3% | 0.201 | |
| Aldosterone Inhibitors | 2.6% | 2.9% | 0.137 | |
| Baseline Serum Creatinine (umol/L) | 222 (141; 322) | 154 (119; 214) | <0.001 * | |
| Baseline MDRD eGFR (mL/min/1.73 m2) | 24 (15; 40) | 34 (24; 48) | <0.001 * | |
| uPCR mg/gCr | 115 (24; 287) | 25 (9; 73) | <0.001 * | |
| uL-FABP ELISA (mcg/gCr) | 7.8 (0; 31.1) | 1.9 (0; 9.4) | <0.001 * | |
| 1 Year Serum Creatinine (umol/L) | 278 (177; 438) | 149 (109; 199) | <0.001 * | |
| 1 Year MDRD eGFR (mL/min/1.73 m2) | 17 (10; 30) | 37 (25; 52) | <0.001 * | |
| Increase in Creatinine (%) | 22.6 (13.3; 41.9) | −3.5 (−12.3; 1.5) | <0.001 * | |
| Decrease in eGFR (mL/min/1.73 m2) | 5 (3; 8) | −1 (−5; 1) | <0.001 * | |
| Outcome: CKD Progression, Predictor: uL-FABP | ||||
|---|---|---|---|---|
| Unadjusted | +Age, Sex | |||
| OR (95% CI) | Sig | OR (95% CI) | Sig | |
| uL-FABP | 1.01 (1.00; 1.01) | 0.002 * | 1.01 (1.00; 1.01) | 0.002 * |
| Outcome: CKD progression, Predictor: uPCR | ||||
| Unadjusted | +Age, Sex | |||
| OR (95% CI) | Sig | OR (95% CI) | Sig | |
| uPCR | 1.00 (1.00; 1.01) | <0.001 * | 1.00 (1.00; 1.01) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitsides, N.; Mitra, V.; Saha, A.; Harris, S.; Kalra, P.A.; Mitra, S. Urinary Liver-Type Fatty Acid Binding Protein, a Biomarker for Disease Progression, Dialysis and Overall Mortality in Chronic Kidney Disease. J. Pers. Med. 2023, 13, 1481. https://doi.org/10.3390/jpm13101481
Mitsides N, Mitra V, Saha A, Harris S, Kalra PA, Mitra S. Urinary Liver-Type Fatty Acid Binding Protein, a Biomarker for Disease Progression, Dialysis and Overall Mortality in Chronic Kidney Disease. Journal of Personalized Medicine. 2023; 13(10):1481. https://doi.org/10.3390/jpm13101481
Chicago/Turabian StyleMitsides, Nicos, Vikram Mitra, Ananya Saha, Shelly Harris, Philip A. Kalra, and Sandip Mitra. 2023. "Urinary Liver-Type Fatty Acid Binding Protein, a Biomarker for Disease Progression, Dialysis and Overall Mortality in Chronic Kidney Disease" Journal of Personalized Medicine 13, no. 10: 1481. https://doi.org/10.3390/jpm13101481
APA StyleMitsides, N., Mitra, V., Saha, A., Harris, S., Kalra, P. A., & Mitra, S. (2023). Urinary Liver-Type Fatty Acid Binding Protein, a Biomarker for Disease Progression, Dialysis and Overall Mortality in Chronic Kidney Disease. Journal of Personalized Medicine, 13(10), 1481. https://doi.org/10.3390/jpm13101481






