Correlation between Degenerative Thoracolumbar Kyphosis and Lumbar Posterior Muscle
Abstract
:1. Introduction
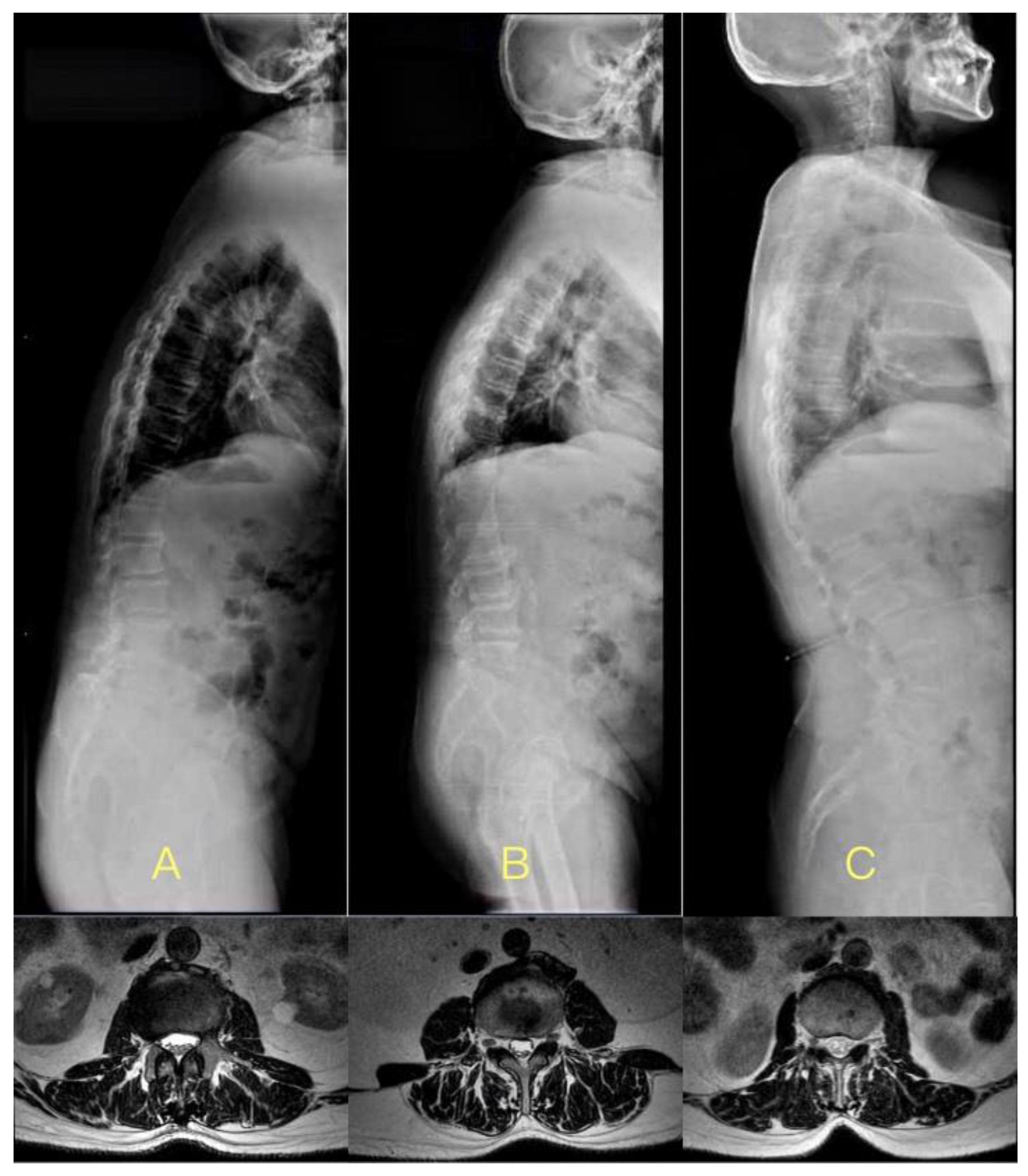
2. Materials and Methods
2.1. Participants
2.2. BMI
2.3. MRI
2.4. Parameters Measurement
2.5. Subgroup Analysis
2.6. Statistical Analysis
3. Results
3.1. LCIV in DTLK and Control Groups
3.2. The Influencing Factor of LCIV
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, W.J.; Kang, J.W.; Kang, S.I.; Sung, H.I.; Park, K.Y.; Park, J.G.; Kwon, W.C.; Choy, W.S. Factors affecting clinical results after corrective osteotomy for lumbar degenerative kyphosis. Asian Spine J. 2010, 4, 7–14. [Google Scholar] [CrossRef]
- Lewis, S.J.; Keshen, S.G.; Kato, S.; Dear, T.E.; Gazendam, A.M. Risk Factors for Postoperative Coronal Balance in Adult Spinal Deformity Surgery. Global Spine J. 2018, 8, 690–697. [Google Scholar] [CrossRef]
- Wang, C.; Chang, H.; Gao, X.; Xu, J.; Meng, X. Risk factors of degenerative lumbar scoliosis in patients with lumbar spinal canal stenosis. Medicine 2019, 98, e17177. [Google Scholar] [CrossRef]
- Cooper, R.G.; Forbes, W.S.C.; Jayson, M.I.V. Radiographic demonstration of paraspinal muscle wasting in patients with chronic low back pain. Br. J. Rheumatol. 1992, 31, 389–394. [Google Scholar] [CrossRef]
- Hicks, G.E.; Simonsick, E.M.; Harris, T.B.; Newman, A.B.; Weiner, D.K.; Nevitt, M.A.; Tylavsky, F.A. Cross-sectional associations between trunk muscle composition, back pain, and physical function in the health, aging and body composition study. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 882–887. [Google Scholar] [CrossRef]
- Yagi, M.; Hosogane, N.; Watanabe, K.; Asazuma, T.; Matsumoto, M. The paravertebral muscle and psoas for the maintenance of global spinal alignment in patient with degenerative lumbar scoliosis. Spine J. 2016, 16, 451–458. [Google Scholar] [CrossRef]
- Banno, T.; Yamato, Y.; Hasegawa, T.; Kobayashi, S.; Togawa, D.; Oe, S.; Mihara, Y.; Kurosu, K.; Yamamoto, N.; Matsuyama, Y. Assessment of the Cross-Sectional Areas of the Psoas Major and Multifidus Muscles in Patients with Adult Spinal Deformity. Clin. Spine Surg. 2017, 30, E968–E973. [Google Scholar] [CrossRef]
- Kalichman, L.; Hodges, P.; Li, L.; Guermazi, A.; Hunter, D.J. Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur. Spine J. 2010, 19, 1136–1144. [Google Scholar] [CrossRef]
- Moal, B.; Bronsard, N.; Raya, J.G.; Vital, J.M.; Schwab, F.; Skalli, W.; Lafage, V. Volume and fat infiltration of spino-pelvic musculature in adults with spinal deformity. World J. Orthop. 2015, 6, 727–737. [Google Scholar] [CrossRef]
- Jun, H.S.; Kim, J.H.; Ahn, J.H.; Chang, I.B.; Song, J.H.; Kim, T.H.; Park, M.S.; Chan Kim, Y.; Kim, S.W.; Oh, J.K.; et al. The Effect of Lumbar Spinal Muscle on Spinal Sagittal Alignment: Evaluating Muscle Quantity and Quality. Neurosurgery 2016, 79, 847–855. [Google Scholar] [CrossRef]
- Banno, T.; Arima, H.; Hasegawa, T.; Yamato, Y.; Togawa, D.; Yoshida, G.; Yasuda, T.; Oe, S.; Mihara, Y.; Ushirozako, H.; et al. The Effect of Paravertebral Muscle on the Maintenance of Upright Posture in Patients with Adult Spinal Deformity. Spine Deform. 2019, 7, 125–131. [Google Scholar] [CrossRef]
- Takayama, K.; Kita, T.; Nakamura, H.; Kanematsu, F.; Yasunami, T.; Sakanaka, H.; Yamano, Y. New Predictive Index for Lumbar Paraspinal Muscle Degeneration Associated with Aging. Spine (Phila Pa 1976) 2016, 41, E84–E90. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Landi, F.; Schneider, S.M.; Zúñiga, C.; Arai, H.; Boirie, Y.; Chen, L.-K.; Fielding, R.A.; Martin, F.C.; Michel, J.-P.; et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Age Ageing 2014, 43, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Shafaq, N.; Suzuki, A.; Matsumura, A.; Terai, H.; Toyoda, H.; Yasuda, H.; Ibrahim, M.; Nakamura, H. Asymmetric degeneration of paravertebral muscles in patients with degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2012, 37, 1398–1406. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Meier, M.; Grob, D.; Müntener, M. Paraspinal muscle fibre type alterations associated with scoliosis: An old problem revisited with new evidence. Eur. Spine J. 1998, 7, 289–293. [Google Scholar] [CrossRef]
- Masaki, M.; Aoyama, T.; Murakami, T.; Yanase, K.; Ji, X.; Tateuchi, H.; Ichihashi, N. Association of low back pain with muscle stiffness and muscle mass of the lumbar back muscles, and sagittal spinal alignment in young and middle-aged medical workers. Clin. Biomech. 2017, 49, 128–133. [Google Scholar] [CrossRef]
- Hiyama, A.; Katoh, H.; Sakai, D.; Tanaka, M.; Sato, M.; Watanabe, M. The correlation analysis between sagittal alignment and cross-sectional area of paraspinal muscle in patients with lumbar spinal stenosis and degenerative spondylolisthesis. BMC Musculoskelet. Disord. 2019, 20, 352. [Google Scholar] [CrossRef]
- Hongo, M.; Miyakoshi, N.; Shimada, Y.; Sinaki, M. Association of spinal curve deformity and back extensor strength in elderly women with osteoporosis in Japan and the United States. Osteoporos. Int. 2012, 23, 1029–1034. [Google Scholar] [CrossRef]
- Diebo, B.G.; Varghese, J.J.; Lafage, R.; Schwab, F.J.; Lafage, V. Sagittal alignment of the spine: What do you need to know? Clin. Neurol. Neurosurg. 2015, 139, 295–301. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Aunoble, S.; Philippe, L.; Nicolas, P. Pelvic parameters: Origin and significance. Eur. Spine J. 2011, 20 (Suppl. S5), 564–571. [Google Scholar] [CrossRef]
- Danneels, L.A.; Vanderstraeten, G.G.; Cambier, D.C.; Witvrouw, E.E.; De Cuyper, H.J. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur. Spine J. 2000, 9, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Solovieva, S.; Husgafvel-Pursiainen, K.; Telama, R.; Yang, X.; Viikari, J.; Raitakari, O.T.; Viikari-Juntura, E. The role of obesity and physical activity in non-specific and radiating low back pain: The Young Finns study. Semin. Arthritis Rheum. 2013, 42, 640–650. [Google Scholar] [CrossRef] [PubMed]
- Yukawa, Y.; Kato, F.; Suda, K.; Yamagata, M.; Ueta, T.; Yoshida, M. Normative data for parameters of sagittal spinal alignment in healthy subjects: An analysis of gender specific differences and changes with aging in 626 asymptomatic individuals. Eur. Spine J. 2018, 27, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.B.; Kim, Y.J.; Ahn, Y.J.; Kang, G.B.; Yang, J.H.; Lim, H.; Lee, S.W. A comparative analysis of sagittal spinopelvic alignment between young and old men without localized disc degeneration. Eur. Spine J. 2014, 23, 1400–1406. [Google Scholar] [CrossRef]
- Chamney, P.W.; Wabel, P.; Moissl, U.M.; Müller, M.J.; Bosy-Westphal, A.; Korth, O.; Fuller, N.J. A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am. J. Clin. Nutr. 2007, 85, 80–89. [Google Scholar] [CrossRef]
- Crawford, R.; Filli, L.; Elliott, J.; Nanz, D.; Fischer, M.; Marcon, M.; Ulbrich, E. Age- and Level-Dependence of Fatty Infiltration in Lumbar Paravertebral Muscles of Healthy Volunteers. AJNR Am. J. Neuroradiol. 2016, 37, 742–748. [Google Scholar] [CrossRef]
- Berven, S.; Wadhwa, R. Sagittal Alignment of the Lumbar Spine. Neurosurg. Clin. N. Am. 2018, 29, 331–339. [Google Scholar] [CrossRef]
- Zhou, S.; Li, W.; Su, T.; Du, C.; Wang, W.; Xu, F.; Sun, Z.; Li, W. Does lumbar lordosis minus thoracic kyphosis predict the clinical outcome of patients with adult degenerative scoliosis? J. Orthop. Surg. Res. 2019, 14, 290. [Google Scholar] [CrossRef]


| DTLK Group | Control Group | p | |
|---|---|---|---|
| Case | 126 | 87 | |
| Gender | 0.829 | ||
| Male | 35 | 23 | |
| Female | 91 | 64 | |
| Age, years | 68.0 ± 8.1 | 68.4 ± 8.3 | 0.711 |
| BMI, kg/m2 | 26.1 ± 3.6 | 26.3 ± 3.4 | 0.745 |
| N: 18.5–24.9 | 52 | 35 | |
| OW: 25–29.9 | 50 | 39 | |
| OB: ≥30 | 24 | 13 | |
| TLK, ° | 25.8 ± 10.1 | 6.7 ± 5.4 | <0.001 |
| LL, ° | 36.6 ± 19.1 | 43.9 ± 11.3 | 0.001 |
| LCIV, mm | DTLK Group | Control Group | p |
|---|---|---|---|
| T12-L1 | 4.4 ± 5.4 | 9.8 ± 4.4 | <0.001 |
| L1-L2 | 5.4 ± 5.7 | 10.0 ± 4.4 | <0.001 |
| L2-L3 | 6.7 ± 5.9 | 9.8 ± 4.4 | <0.001 |
| L3-L4 | 9.2 ± 6.2 | 10.0 ± 4.4 | 0.361 |
| L4-L5 | 13.7 ± 5.6 | 12.6 ± 5.2 | 0.202 |
| mLCIV | 7.9 ± 5.1 | 10.4 ± 3.9 | <0.001 |
| LCIV, mm | DTLK Group | Control Group | ||||
|---|---|---|---|---|---|---|
| Male | Female | p | Male | Female | p | |
| T12-L1 | 2.4 ± 6.5 | 5.1 ± 4.9 | 0.044 | 11.0 ± 4.5 | 9.5 ± 4.3 | 0.198 |
| L1-L2 | 4.1 ± 7.1 | 5.8 ± 5.1 | 0.241 | 12.1 ± 4.5 | 9.3 ± 4.2 | 0.015 |
| L2-L3 | 7.4 ± 7.3 | 6.4 ± 5.4 | 0.527 | 12.3 ± 4.2 | 9.0 ± 4.1 | 0.003 |
| L3-L4 | 10.1 ± 9.2 | 8.9 ± 4.9 | 0.575 | 12.1 ± 4.6 | 9.3 ± 4.1 | 0.014 |
| L4-L5 | 15.2 ± 8.0 | 13.2 ± 4.6 | 0.265 | 14.9 ± 4.2 | 11.9 ± 5.4 | 0.028 |
| mLCIV | 7.8 ± 7.0 | 7.9 ± 4.3 | 0.979 | 12.5 ± 3.7 | 9.8 ± 3.8 | 0.008 |
| LCIV, mm | DTLK Group | Control Group | ||||
|---|---|---|---|---|---|---|
| N | OW | OB | N | OW | OB | |
| T12-L1 | 2.7 ± 4.1 bb | 4.1 ± 6.2 c | 7.7 ± 4.2 | 7.9 ± 4.7 a,bb | 10.4 ± 3.7 c | 13.2 ± 2.8 |
| L1-L2 | 3.4 ± 4.3 bb | 5.6 ± 6.5 | 8.2 ± 4.8 | 8.2 ± 4.9 a,bb | 10.6 ± 3.3 | 12.8 ± 3.9 |
| L2-L3 | 5.1 ± 5.2 b | 7.0 ± 6.6 | 8.7 ± 5.2 | 8.0 ± 4.3 a,bb | 10.6 ± 3.8 | 12.3 ± 4.3 |
| L3-L4 | 8.8 ± 5.4 | 9.3 ± 7.4 | 9.8 ± 5.0 | 8.2 ± 4.0 a,bb | 10.8 ± 4.2 | 12.3 ± 4.6 |
| L4-L5 | 12.8 ± 5.5 | 14.0 ± 6.5 | 14.5 ± 4.0 | 10.8 ± 5.5 bb | 14.1 ± 4.5 | 13.0 ± 5.2 |
| mLCIV | 6.6 ± 4.2 b | 8.0 ± 6.0 | 9.8 ± 4.0 | 8.6 ± 3.9 aa,bb | 11.3 ± 3.3 | 12.7 ± 3.6 |
| Coefficient | Unstandardized | Standardized | t | p Value | ||
|---|---|---|---|---|---|---|
| B | SE | Beta | ||||
| DTLK group | Constant | 13.749 | 1.027 | 13.386 | <0.001 | |
| TLK | −0.183 | 0.036 | −0.480 | −5.131 | <0.001 | |
| Control group | Constant | 1.016 | 3.161 | 0.321 | 0.749 | |
| BMI | 0.356 | 0.120 | 0.328 | 2.970 | 0.004 | |
| All cases | Constant | 5.407 | 2.149 | 2.516 | 0.013 | |
| TLK | 0.246 | 0.080 | 0.215 | 3.062 | 0.003 | |
| BMI | −0.127 | 0.022 | −0.413 | −5.872 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, C.; Xu, S.; Liang, Y.; Zheng, B.; Zhu, Z.; Liu, H. Correlation between Degenerative Thoracolumbar Kyphosis and Lumbar Posterior Muscle. J. Pers. Med. 2023, 13, 1503. https://doi.org/10.3390/jpm13101503
Guo C, Xu S, Liang Y, Zheng B, Zhu Z, Liu H. Correlation between Degenerative Thoracolumbar Kyphosis and Lumbar Posterior Muscle. Journal of Personalized Medicine. 2023; 13(10):1503. https://doi.org/10.3390/jpm13101503
Chicago/Turabian StyleGuo, Chen, Shuai Xu, Yan Liang, Bin Zheng, Zhenqi Zhu, and Haiying Liu. 2023. "Correlation between Degenerative Thoracolumbar Kyphosis and Lumbar Posterior Muscle" Journal of Personalized Medicine 13, no. 10: 1503. https://doi.org/10.3390/jpm13101503
APA StyleGuo, C., Xu, S., Liang, Y., Zheng, B., Zhu, Z., & Liu, H. (2023). Correlation between Degenerative Thoracolumbar Kyphosis and Lumbar Posterior Muscle. Journal of Personalized Medicine, 13(10), 1503. https://doi.org/10.3390/jpm13101503




