Improving Strength and Fatigue Resistance in Post-Polio Syndrome Individuals with REAC Neurobiological Treatments
Abstract
:1. Introduction
2. Materials and Methods
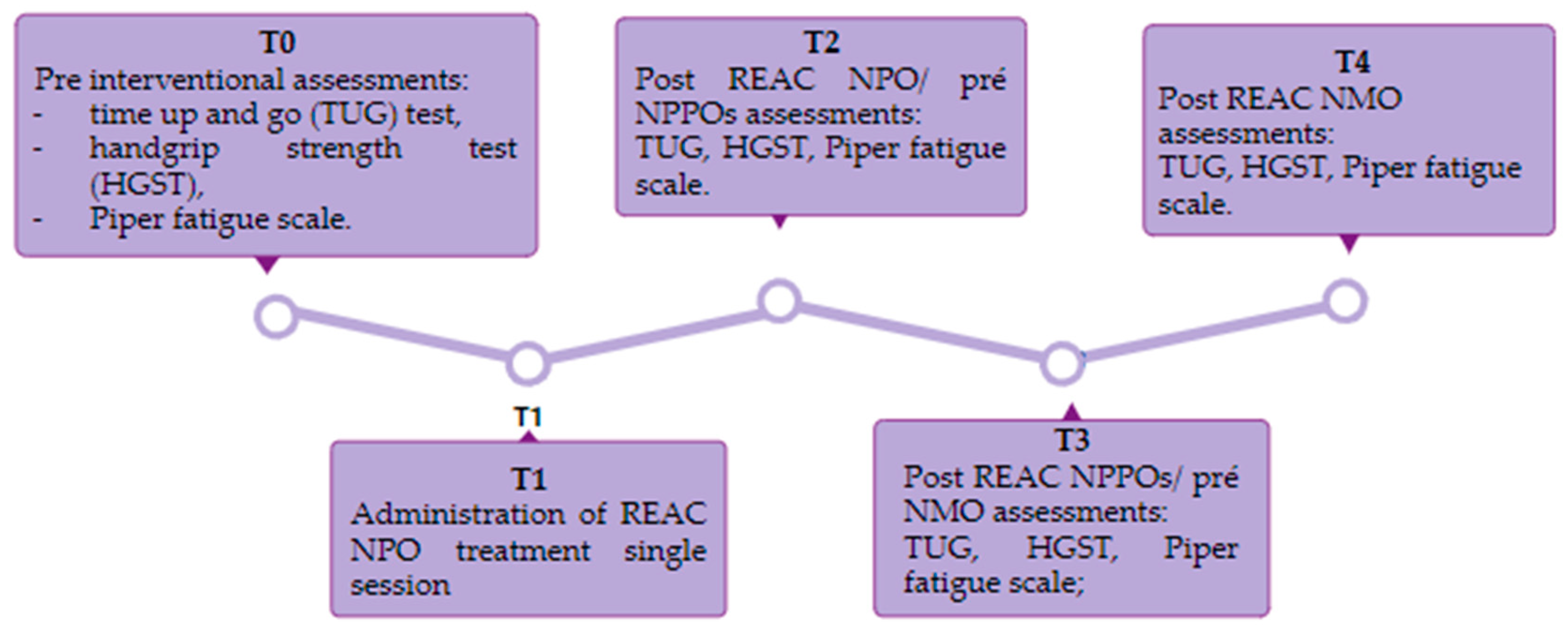
2.1. Study Design
2.2. Sample Size Determination and Power Analysis
2.3. Inclusion and Exclusion Criteria
2.4. Research Locations
2.5. Population
2.6. Procedures and Duration of the Study
2.7. Muscle Strength and Fatigue Testing
2.7.1. Time Up and Go
2.7.2. Handgrip Strength Test (HGST)
2.7.3. Revised Piper Fatigue Scale (RPFS)
2.8. Radio Electric Asymmetric Conveyer (REAC) Technology and Neuro Psycho Physical Optimization Treatments
2.8.1. REAC Technology
2.8.2. Neuro Postural Optimization (NPO)
2.8.3. Neuro Psycho Physical Optimization and Neuro Psycho Physical Optimization Cervical Brachial
2.8.4. Neuromuscular Optimization (NMO)
2.9. Study Replicability
2.10. Statistical Analysis
3. Results
3.1. Time Up and Go
3.2. Handgrip Strength Test
3.3. Fatigue
| Revised Piper Fatigue Scale—General Fatigue (p-Values) | ||||
|---|---|---|---|---|
| T0 | T2 | T3 | T4 | |
| T0 | - | |||
| T2 | <0.01 * | - | ||
| T3 | <0.01 * | >0.05 | - | |
| T4 | <0.01 * | >0.08 | <0.10 | - |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sáinz, M.; Pelayo, R.; Laxe, S.; Castaño, B.; Capdevilla, E.; Portell, E. Describing post-polio syndrome. Neurologia 2022, 37, 346–354. Available online: https://www.ncbi.nlm.nih.gov/pubmed/35672121 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Farbu, E.; Gilhus, N.E.; Barnes, M.P.; Borg, K.; De Visser, M.; Driessen, A.; Howard, R.; Nollet, F.; Opara, J.; Stalberg, E. EFNS guideline on diagnosis and management of post-polio syndrome. Report of an EFNS task force. Eur. J. Neurol. 2006, 13, 795–801. Available online: https://www.ncbi.nlm.nih.gov/pubmed/16879288 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Gawne, A.C.; Halstead, L.S. Post-polio syndrome: Historical perspective, epidemiology and clinical presentation. NeuroRehabilitation 1997, 8, 73–81. Available online: https://www.ncbi.nlm.nih.gov/pubmed/24525978 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Ragonese, P.; Fierro, B.; Salemi, G.; Randisi, G.; Buffa, D.; D’Amelio, M.; Aloisio, A.; Savettieri, G. Prevalence and risk factors of post-polio syndrome in a cohort of polio survivors. J. Neurol. Sci. 2005, 236, 31–35. Available online: https://www.ncbi.nlm.nih.gov/pubmed/16014307 (accessed on 1 July 2023). [CrossRef]
- Ramlow, J.; Alexander, M.; LaPorte, R.; Kaufmann, C.; Kuller, L. Epidemiology of the post-polio syndrome. Am. J. Epidemiology 1992, 136, 769–786. Available online: https://www.ncbi.nlm.nih.gov/pubmed/1442743 (accessed on 1 July 2023). [CrossRef]
- Trojan, D.A.; Cashman, N.R. Post-poliomyelitis syndrome. Muscle Nerve 2005, 31, 6–19. Available online: https://www.ncbi.nlm.nih.gov/pubmed/15599928 (accessed on 1 July 2023). [CrossRef]
- Gonzalez, H.; Olsson, T.; Borg, K. Management of postpolio syndrome. Lancet Neurol. 2010, 9, 634–642. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20494327 (accessed on 1 July 2023). [CrossRef]
- Halstead, L.S.; Rossi, C.D. New Problems in old polio patients: Results of a survey of 539 polio survivors. Orthopedics 1985, 8, 845–850. Available online: https://www.ncbi.nlm.nih.gov/pubmed/3867865 (accessed on 1 July 2023). [CrossRef]
- Conde, M.T.R.P.; Oliveira, A.S.B.; Quadros, A.A.J.; Moreira, G.A.; Silva, H.C.A.; Pereira, R.D.B.; e Silva, T.M.; Tufik, S.; Waldman, E.A. Post-polio syndrome: Epidemiologic and prognostic aspects in Brazil. Acta Neurol. Scand. 2009, 120, 191–197. Available online: https://www.ncbi.nlm.nih.gov/pubmed/19133864 (accessed on 1 July 2023). [CrossRef]
- Dalakas, M.C. The post-polio syndrome as an evolved clinical entity. Definition and clinical description. Ann. N. Y. Acad. Sci. 1995, 753, 68–80. Available online: https://www.ncbi.nlm.nih.gov/pubmed/7611661 (accessed on 1 July 2023). [CrossRef]
- Motta, M.P.; Quadros, A.A.J.; Conti, M.d.S.B.; Oliveira, A.S.B. Post-polio syndrome. Braz. J. Biol. Sci. 2018, 5, 631–639. [Google Scholar] [CrossRef]
- Thomas, C.K.; Zijdewind, I. Fatigue of muscles weakened by death of motoneurons. Muscle Nerve 2006, 33, 21–41. Available online: https://www.ncbi.nlm.nih.gov/pubmed/16025525 (accessed on 1 July 2023). [CrossRef]
- Oliveira, A.S.B.; Quadros, A.A.J.; Silva, H.C.A.; Conde, M.T.R.P.; Silva, T.M.; Fontes, S.V.; Gabbai, A.A.; Steiner, A.L.; Viana, C.F.; Barros, D.R.; et al. Síndrome Pós-Poliomielite (SPP)-Orientações Para Profissionais de Saúde; Governo Do Estado De São Paulo: São Paulo, Brazil, 2008; p. 126. [Google Scholar]
- World Medical Association. World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. Available online: https://www.ncbi.nlm.nih.gov/pubmed/24141714 (accessed on 1 July 2023). [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. Available online: https://www.ncbi.nlm.nih.gov/pubmed/17695343 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval. Health Prof. 2021, 18, 17. Available online: https://www.ncbi.nlm.nih.gov/pubmed/34325496 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Ortega-Bastidas, P.; Gómez, B.; Aqueveque, P.; Luarte-Martínez, S.; Cano-De-La-Cuerda, R. Instrumented timed up and go test (itug)—More than assessing time to predict falls: A systematic review. Sensors 2023, 23, 3426. Available online: https://www.ncbi.nlm.nih.gov/pubmed/37050485 (accessed on 1 July 2023). [CrossRef]
- Coelho-Junior, H.J.; Rodrigues, B.; Gonçalves, I.d.O.; Asano, R.Y.; Uchida, M.C.; Marzetti, E. The physical capabilities underlying timed “up and go” test are time-dependent in community-dwelling older women. Exp. Gerontol. 2018, 104, 138–146. Available online: https://www.ncbi.nlm.nih.gov/pubmed/29410234 (accessed on 1 July 2023). [CrossRef]
- Kristensen, M.T. Factors influencing performances and indicating risk of falls using the true Timed Up and Go test time of patients with hip fracture upon acute hospital discharge. Physiother. Res. Int. 2020, 25, 1841. Available online: https://www.ncbi.nlm.nih.gov/pubmed/32363803 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Alfieri, F.M.; Carreres, M.A.; Figuera, R.G.; Battistella, L.R. Comparison of time taken to complete the timed up and go test (TUG) between elderly adults with and without falls. Rev. Esp. Geriatr. Gerontol. 2010, 45, 174–175. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20398963 (accessed on 1 July 2023). [CrossRef]
- Freter, S.H.; Fruchter, N. Relationship between timed ‘up and go’ and gait time in an elderly orthopaedic rehabilitation population. Clin. Rehabil. 2000, 14, 96–101. Available online: https://www.ncbi.nlm.nih.gov/pubmed/10688350 (accessed on 1 July 2023). [CrossRef]
- Kelley, C.; Bennett, D.; Cooper, N.; Burgoyne, W. Comparison of grip strengths of people with post-polio syndrome, without known upper extremity weakness, to published grip strengths of normals. J. Neurol. Phys. Ther. 2004, 28, 182–183. Available online: https://journals.lww.com/jnpt/Fulltext/2004/12000/COMPARISON_OF_GRIP_STRENGTHS_OF_PEOPLE_WITH.45.aspx (accessed on 1 July 2023). [CrossRef]
- Lee, S.Y. Handgrip Strength: An Irreplaceable Indicator of Muscle Function. Ann. Rehabil. Med. 2021, 45, 167–169. Available online: https://www.ncbi.nlm.nih.gov/pubmed/34233405 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Piper, B.F. Piper fatigue scale available for clinical testing. Oncol. Nurs. Forum 1990, 17, 661–662. Available online: https://www.ncbi.nlm.nih.gov/pubmed/2251183 (accessed on 1 July 2023).
- Piper, B.F.; Dibble, S.L.; Dodd, M.J.; Weiss, M.C.; Slaughter, R.E.; Paul, S.M. The revised Piper Fatigue Scale: Psychometric evaluation in women with breast cancer. Oncol. Nurs. Forum 1998, 25, 677–684. [Google Scholar]
- Rinaldi, S.; Mura, M.; Castagna, A.; Fontani, V. Long-lasting changes in brain activation induced by a single REAC technology pulse in Wi-Fi bands. Randomized double-blind fMRI qualitative study. Sci. Rep. 2014, 4, srep05668. Available online: https://www.ncbi.nlm.nih.gov/pubmed/25011544 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Rinaldi, S.; Fontani, V.; Castagna, A.; Lotti, M.; Ventura, C.; Maioli, M.; Santaniello, S.; Pigliaru, G.; Carta, A.; Gualini, S. Regenerative treatment using a radioelectric asymmetric conveyor as a novel tool in antiaging medicine: An in vitro beta-galactosidase study. Clin. Interv. Aging 2012, 7, 191–194. Available online: https://www.ncbi.nlm.nih.gov/pubmed/22807628 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Rinaldi, A.; Martins, M.C.M.; Oliveira, A.C.D.A.M.; Rinaldi, S.; Fontani, V. Improving functional abilities in children and adolescents with autism spectrum disorder using non-invasive reac neuro psycho physical optimization treatments: A pedi-cat study. J. Pers. Med. 2023, 13, 792. Available online: https://www.ncbi.nlm.nih.gov/pubmed/37240963 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Rinaldi, C.; Landre, C.B.; Volpe, M.I.; Gonçalves, R.G.; Nunes, L.d.S.; Darienso, D.; Cruz, A.V.; Oliveira, J.D.; Rinaldi, S.; Fontani, V.; et al. Improving functional capacity and quality of life in parkinson’s disease patients through reac neuromodulation treatments for mood and behavioral disorders. J. Pers. Med. 2023, 13, 937. Available online: https://www.ncbi.nlm.nih.gov/pubmed/37373926 (accessed on 1 July 2023). [CrossRef]
- Machado, V.G.; Brun, A.B.S.; Manffra, E.F. Effects of the radio electric asymmetric conveyer (REAC) on motor disorders: An integrative review. Front. Med. Technol. 2023, 5, 1122245. Available online: https://www.ncbi.nlm.nih.gov/pubmed/36923595 (accessed on 1 July 2023). [CrossRef]
- Fontani, V.; Rinaldi, A.; Rinaldi, C.; Araldi, L.; Azzarà, A.; Carta, A.M.; Casale, N.; Castagna, A.; Del Medico, M.; Di Stasio, M.; et al. Long-lasting efficacy of radio electric asymmetric conveyer neuromodulation treatment on functional dysmetria, an adaptive motor behavior. Cureus 2022, 14, e25768. Available online: https://www.ncbi.nlm.nih.gov/pubmed/35706441 (accessed on 1 July 2023). [CrossRef]
- Rinaldi, A.; Rinaldi, C.; Pereira, J.A.C.; Margotti, M.L.; Bittencourt, M.N.; Barcessat, A.R.P.; Fontani, V.; Rinaldi, S. Radio electric asymmetric conveyer neuromodulation in depression, anxiety, and stress. Neuropsychiatr. Dis. Treat. 2019, 15, 469–480. Available online: https://www.ncbi.nlm.nih.gov/pubmed/30858704 (accessed on 1 July 2023). [CrossRef]
- Flansbjer, U.-B.; Lexell, J.; Brogårdh, C. Predictors of changes in gait performance over four years in persons with late effects of polio. NeuroRehabilitation 2017, 41, 403–411. Available online: https://www.ncbi.nlm.nih.gov/pubmed/28946571 (accessed on 1 July 2023). [CrossRef]
- Lehmann, K.; Sunnerhagen, K.S.; Willen, C. Postural control in persons with late effects of polio. Acta Neurol. Scand. 2006, 113, 55–61. Available online: https://www.ncbi.nlm.nih.gov/pubmed/16367900 (accessed on 1 July 2023). [CrossRef]
- Vreede, K.; Henriksson, J.; Borg, K.; Henriksson, M. Gait characteristics and influence of fatigue during the 6-minute walk test in patients with post-polio syndrome. J. Rehabilitation Med. 2013, 45, 924–928. Available online: https://www.ncbi.nlm.nih.gov/pubmed/23999579 (accessed on 1 July 2023). [CrossRef]
- Bickerstaffe, A.; Beelen, A.; Nollet, F. Circumstances and consequences of falls in polio survivors. J. Rehabil. Med. 2010, 42, 908–915. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21031286 (accessed on 1 July 2023). [CrossRef]
- Nam, K.Y.; Lee, S.; Yang, E.J.; Kim, K.; Jung, S.H.; Jang, S.-N.; Han, S.J.; Kim, W.-H.; Lim, J.-Y. Falls in Korean polio survivors: Incidence, consequences, and risk factors. J. Korean Med. Sci. 2016, 31, 301–309. Available online: https://www.ncbi.nlm.nih.gov/pubmed/26839487 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Tiffreau, V.; Rapin, A.; Serafi, R.; Percebois-Macadré, L.; Supper, C.; Jolly, D.; Boyer, F.-C. Post-polio syndrome and rehabilitation. Ann. Phys. Rehabil. Med. 2010, 53, 42–50. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20044320 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Rijk, J.M.; Roos, P.R.; Deckx, L.; Akker, M.v.D.; Buntinx, F. Prognostic value of handgrip strength in people aged 60 years and older: A systematic review and meta-analysis. Geriatr. Gerontol. Int. 2016, 16, 5–20. Available online: https://www.ncbi.nlm.nih.gov/pubmed/26016893 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Stålberg, E.; Grimby, G. Dynamic electromyography and muscle biopsy changes in a 4-year follow-up: Study of patients with a history of polio. Muscle Nerve 1995, 18, 699–707. Available online: https://www.ncbi.nlm.nih.gov/pubmed/7783759 (accessed on 1 July 2023). [CrossRef]
- Dalakas, M.C.; Elder, G.; Hallett, M.; Ravits, J.; Baker, M.; Papadopoulos, N.; Albrecht, P.; Sever, J. A Long-term follow-up study of patients with post-poliomyelitis neuromuscular symptoms. N. Engl. J. Med. 1986, 314, 959–963. Available online: https://www.ncbi.nlm.nih.gov/pubmed/3007983 (accessed on 1 July 2023). [CrossRef]
- Xue, Q.-L.; Walston, J.D.; Fried, L.P.; Beamer, B.A. Prediction of risk of falling, physical disability, and frailty by rate of decline in grip strength: The women’s health and aging study. Arch. Intern. Med. 2011, 171, 1119–1121. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21709116 (accessed on 1 July 2023). [CrossRef]
- Hirsch, C.H.; Bůžková, P.; Robbins, J.A.; Patel, K.V.; Newman, A.B. Predicting late-life disability and death by the rate of decline in physical performance measures. Age Ageing 2011, 41, 155–161. Available online: https://www.ncbi.nlm.nih.gov/pubmed/22156556 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Onder, G.; Penninx, B.W.J.H.; Ferrucci, L.; Fried, L.P.; Guralnik, J.M.; Pahor, M. Measures of physical performance and risk for progressive and catastrophic disability: Results from the women’s health and aging study. J. Gerontol. Ser. A 2005, 60, 74–79. Available online: https://www.ncbi.nlm.nih.gov/pubmed/15741286 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Bruno, R.L.; Frick, N.M. The psychology of polio as prelude to post-polio sequelae: Behavior modification and psychotherapy. Orthopedics 1991, 14, 1185–1193. Available online: https://www.ncbi.nlm.nih.gov/pubmed/1758786 (accessed on 1 July 2023). [CrossRef]
- Östlund, G.; Wahlin, Å.; Sunnerhagen, K.; Borg, K. Post polio syndrome: Fatigued patients a specific subgroup? J. Rehabil. Med. 2011, 43, 39–45. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21174052 (accessed on 1 July 2023). [CrossRef] [PubMed]
- Krasovsky, T. Cognition, emotion, and movement in the context of rehabilitation. Int. J. Environ. Res. Public Health 2022, 19, 14532. Available online: https://www.ncbi.nlm.nih.gov/pubmed/36361412 (accessed on 1 July 2023). [CrossRef]




| Revised Piper Fatigue Scale—Fatigue | ||||
|---|---|---|---|---|
| Conditions (Mean ± SD) | Behavioral Dimension | Affective Dimension | Sensory Dimension | Fatigue |
| T0 | 6.29 ± 1.76 | 4.95 ± 2.70 | 4.33 ± 2.56 | 5.00 ± 2.08 |
| T2 | 3.66 ± 2.37 | 2.86 ± 2.20 | 2.34 ± 1.76 | 2.82 ± 1.93 |
| T3 | 3.53 ± 2.95 | 2.97 ± 3.21 | 2.68 ± 2.02 | 2.98 ± 2.35 |
| T4 | 1.75 ± 1.97 | 1.70 ± 2.29 | 1.47 ± 1.67 | 1.60 ± 1.80 |
| Revised Piper Fatigue Scale—Behavioral Dimension (p-Values) | ||||
|---|---|---|---|---|
| Moments | T0 | T2 | T3 | T4 |
| T0 | - | |||
| T2 | <0.01 * | - | ||
| T3 | <0.01 * | >0.05 | - | |
| T4 | <0.01 * | 0.01 * | <0.07 | - |
| Revised Piper Fatigue Scale—Affective Dimension (p-Values) | ||||
|---|---|---|---|---|
| Moments | T0 | T2 | T3 | T4 |
| T0 | - | |||
| T2 | <0.01 * | - | ||
| T3 | <0.05 * | >0.05 | - | |
| T4 | <0.01 * | >0.05 | >0.05 | - |
| Revised Piper Fatigue Scale—Sensory Dimension (p-Values) | ||||
|---|---|---|---|---|
| Moments | T0 | T2 | T3 | T4 |
| T0 | - | |||
| T2 | <0.01 * | - | ||
| T3 | 0.01 * | >0.05 | - | |
| T4 | <0.01 * | >0.05 | >0.05 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira Motta, M.; Oliveira, A.S.B.; André Nogueira, J.A.; Vieira de Souza Moscardi, A.A.; Munhoz Teixeira, C.; Manchim Favaro, V.; Simcsik, A.O.; Conde, S.; Patrizi, M.C.; Rinaldi, C.; et al. Improving Strength and Fatigue Resistance in Post-Polio Syndrome Individuals with REAC Neurobiological Treatments. J. Pers. Med. 2023, 13, 1536. https://doi.org/10.3390/jpm13111536
Pereira Motta M, Oliveira ASB, André Nogueira JA, Vieira de Souza Moscardi AA, Munhoz Teixeira C, Manchim Favaro V, Simcsik AO, Conde S, Patrizi MC, Rinaldi C, et al. Improving Strength and Fatigue Resistance in Post-Polio Syndrome Individuals with REAC Neurobiological Treatments. Journal of Personalized Medicine. 2023; 13(11):1536. https://doi.org/10.3390/jpm13111536
Chicago/Turabian StylePereira Motta, Monalisa, Acary Souza Bulle Oliveira, Jeyce Adrielly André Nogueira, Alcione Aparecida Vieira de Souza Moscardi, Claudete Munhoz Teixeira, Vanessa Manchim Favaro, Amanda Orasmo Simcsik, Salete Conde, Maria Clara Patrizi, Chiara Rinaldi, and et al. 2023. "Improving Strength and Fatigue Resistance in Post-Polio Syndrome Individuals with REAC Neurobiological Treatments" Journal of Personalized Medicine 13, no. 11: 1536. https://doi.org/10.3390/jpm13111536
APA StylePereira Motta, M., Oliveira, A. S. B., André Nogueira, J. A., Vieira de Souza Moscardi, A. A., Munhoz Teixeira, C., Manchim Favaro, V., Simcsik, A. O., Conde, S., Patrizi, M. C., Rinaldi, C., Fontani, V., & Rinaldi, S. (2023). Improving Strength and Fatigue Resistance in Post-Polio Syndrome Individuals with REAC Neurobiological Treatments. Journal of Personalized Medicine, 13(11), 1536. https://doi.org/10.3390/jpm13111536









