Orthognathic Surgery with Interdisciplinary Digital Planning in Patients with Geroderma Osteodysplasticum: A Case Report
Abstract
:1. Introduction
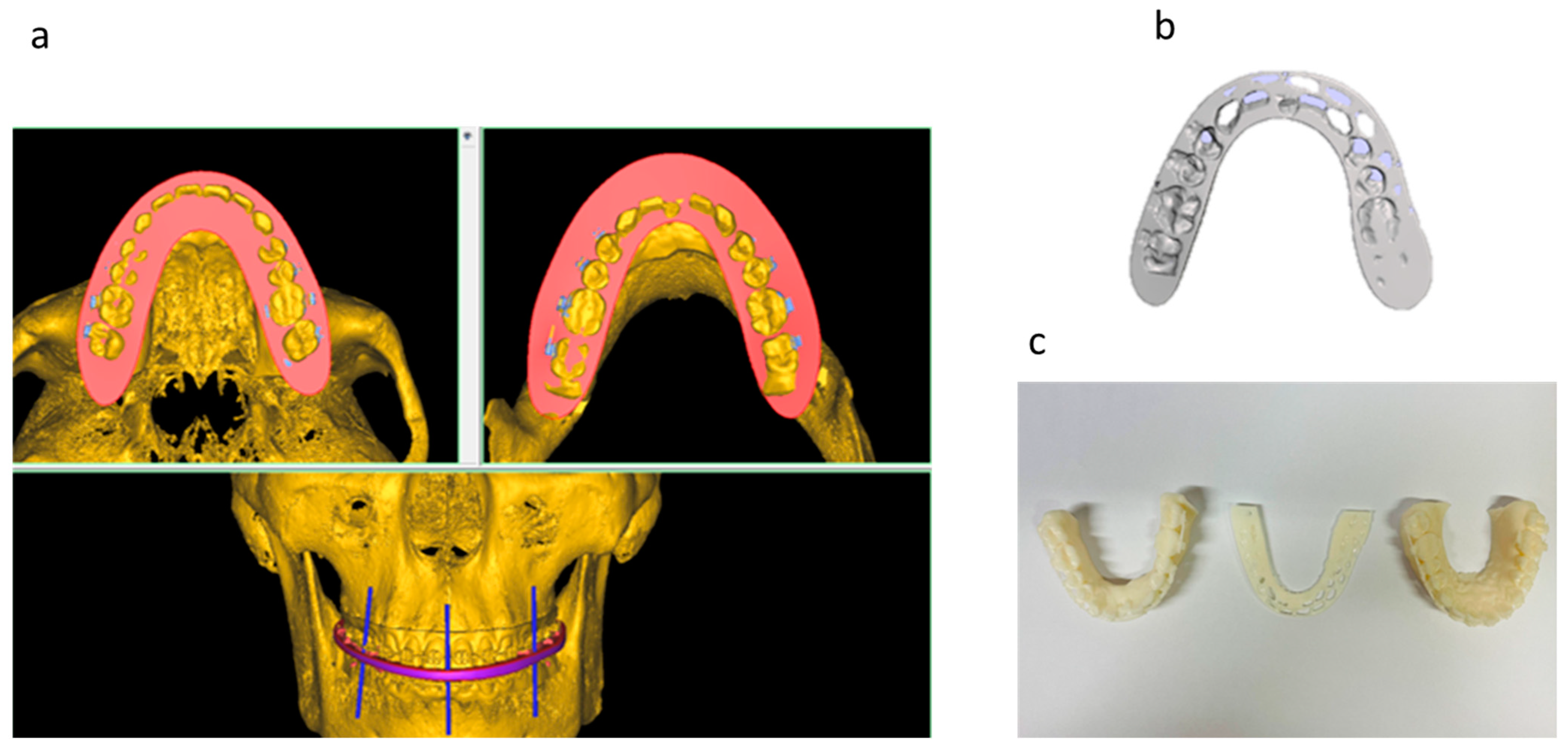
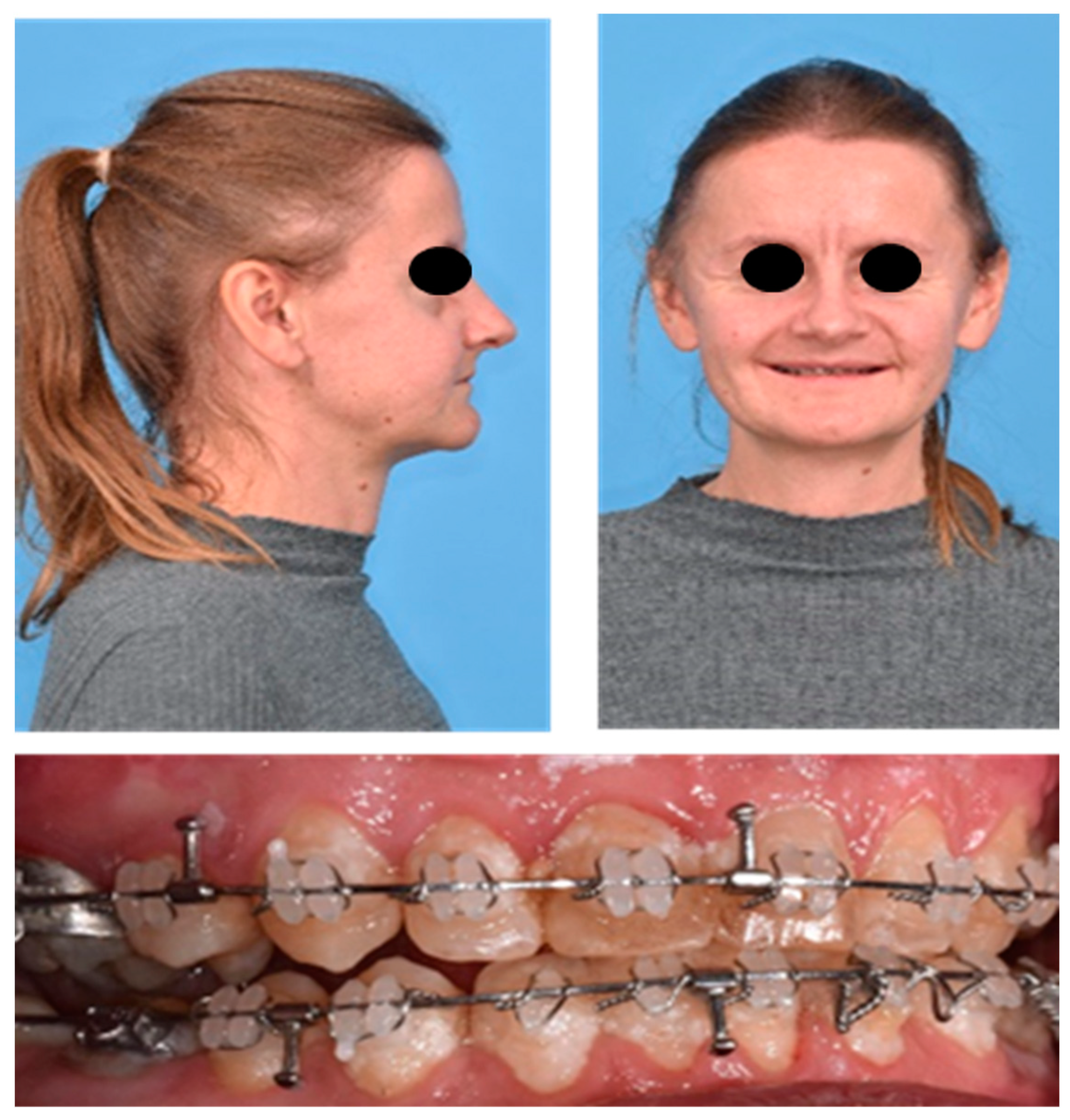
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bamatter, F.; Franceschetti, A. Gérodermie ostéodysplasique héréditaire; un nouveau biotype de la progeria [Hereditary osteodysplastic geoderma; a new biotype of progeria]. Confin. Neurol. 1949, 9, 397. [Google Scholar] [CrossRef] [PubMed]
- Hunter, A.G.; Martsolf, J.T.; Baker, C.G.; Reed, M.H. Geroderma osteodysplastica. A report of two affected families. Hum. Genet. 1978, 40, 311–324. [Google Scholar] [CrossRef] [PubMed]
- Rajab, A.; Kornak, U.; Budde, B.S.; Hoffmann, K.; Jaeken, J.; Nürnberg, P.; Mundlos, S. Geroderma osteodysplasticum hereditaria and wrinkly skin syndrome in 22 patients from Oman. Am. J. Med. Genet. 2008, 146, 965–976. [Google Scholar] [CrossRef] [PubMed]
- Hennies, H.C.; Kornak, U.; Zhang, H.; Egerer, J.; Zhang, X.; Seifert, W.; Kühnisch, J.; Budde, B.; Nätebus, M.; Brancati, F.; et al. Gerodermia osteodysplastica is caused by mutations in SCYL1BP1, a Rab-6 interacting golgin. Nat. Genet. 2008, 40, 1410–1412. [Google Scholar] [CrossRef]
- Al-Dosari, M.; Alkuraya, F.S. A novel missense mutation in SCYL1BP1 produces geroderma osteodysplastica phenotype indistinguishable from that caused by nullimorphic mutations. Am. J. Med. Genet. 2009, 149, 2093–2098. [Google Scholar] [CrossRef]
- Yildirim, Y.; Tolun, A.; Tüysüz, B. The phenotype caused by PYCR1 mutations corresponds to geroderma osteodysplasticum rather than autosomal recessive cutis laxa type 2. Am. J. Med. Genet. 2011, 155, 134–140. [Google Scholar] [CrossRef]
- Patton, M.A.; Tolmie, J.; Ruthnum, P.; Bamforth, S.; Baraitser, M.; Pembrey, M. Congenital cutis laxa with retardation of growth and development. J. Med. Genet. 1987, 24, 556–561. [Google Scholar] [CrossRef]
- Sakati, N.O.; Nyhan, W.L. Congenital cutis laxa and osteoporosis. Am. J. Dis. Child. 1960, 137, 452–454. [Google Scholar] [CrossRef]
- Kariminejad, A.; Afroozan, F.; Bozorgmehr, B.; Ghanadan, A.; Akbaroghli, S.; Khorram Khorshid, H.R.; Mojahedi, F.; Setoodeh, A.; Loh, A.; Tan, Y.X.; et al. Discriminative Features in Three Autosomal Recessive Cutis Laxa Syndromes: Cutis Laxa IIA, Cutis Laxa IIB, and Geroderma Osteoplastica. Int. J. Mol. Sci. 2017, 18, 635. [Google Scholar] [CrossRef]
- Hunter, A.G. Is geroderma osteodysplastica underdiagnosed? J. Med. Genet. 1988, 25, 854–857. [Google Scholar] [CrossRef]
- Lustmann, J.; Nahlieli, O.; Harary, D.; Casap, N.; Neder, A.; Zlotogora, J. Gerodermia osteodysplastica: Report on two patients and surgical correction of facial deformity. Am. J. Med. Genet. 1993, 47, 261–267. [Google Scholar] [CrossRef]
- Alotaibi, M.; Aldhubaiban, D.; Alasmari, A.; Alotaibi, L. A Case of Geroderma Osteodysplasticum Syndrome: Unique Clinical Findings. Glob. Med. Genet. 2021, 9, 175–178. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.; Kapoor, S.; Puri, R.; Bijarnia, S. Gerodermia Osteodysplastica. Indian J. Pediatr. 2004, 71, e77–e79. [Google Scholar]
- Takeda, R.; Takagi, M.; Shinohara, H.; Futagawa, H.; Narumi, S.; Hasegawa, T.; Nishimura, G.; Yoshihashi, H. Novel compound heterozygous mutations identified by whole exome sequencing in a Japanese patient with geroderma osteodysplastica. Eur. J. Med. Genet. 2017, 60, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Noordam, C.; Funke, S.; Knoers, N.V.; Jira, P.; Wevers, R.A.; Urban, Z.; Morava, E. Decreased bone density and treatment in patients with autosomal recessive cutis laxa. Acta Paediatr. 2009, 98, 490–494. [Google Scholar] [CrossRef]
- Rodriguez-Revenga, L.; Iranzo, P.; Badenas, C.; Puig, S.; Carrió, A.; Milà, M. A novel elastin gene mutation resulting in an autosomal dominant form of cutis laxa. Arch. Dermatol. 2004, 140, 1135–1139. [Google Scholar] [CrossRef] [PubMed]
- Fricain, M.; Charavet, C.; Raoult, A.G.; Oueiss, A.; Savoldelli, C. Condylar repositioning according to digital bite registration method for virtual orthognathic surgery planning: A series of 49 consecutive patients. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e133–e140. [Google Scholar] [CrossRef]
- Nilsson, J.; Thor, A.; Kamer, L. Development of workflow for recording virtual bite in the planning of orthognathic operations. Br. J. Oral Maxillofac. Surg. 2015, 53, 384–386. [Google Scholar] [CrossRef]
- Nilsson, J.; Richards, R.G.; Thor, A.; Kamer, L. Virtual bite registration using intraoral digital scanning, CT and CBCT: In vitro evaluation of a new method and its implication for orthognathic surgery. J. Cranio-Maxillo-Facial Surg. 2016, 44, 1194–1200. [Google Scholar] [CrossRef]
- Cao, R.K.; Li, L.S.; Cao, Y.J. Application of three-dimensional technology in orthognathic surgery: A narrative review. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 7858–7865. [Google Scholar] [CrossRef]
- Zinser, M.J.; Sailer, H.F.; Ritter, L.; Braumann, B.; Maegele, M.; Zöller, J.E. A paradigm shift in orthognathic surgery? A comparison of navigation, computer-aided designed/computer-aided manufactured splints, and “classic” intermaxillary splints to surgical transfer of virtual orthognathic planning. J. Oral Maxillofac. Surg. 2013, 71, 2151.e1–2151.e21. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Lonic, D.; Lo, L.J. 3D printing in orthognathic surgery—A literature review. J. Formos. Med. Assoc. 2018, 117, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Aboul-Hosn Centenero, S.; Hernández-Alfaro, F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results—Our experience in 16 cases. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2017, 40, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Louvrier, A.; Marty, P.; Barrabé, A.; Euvrard, E.; Chatelain, B.; Weber, E.; Meyer, C. How useful is 3D printing in maxillofacial surgery? J. Stomatol. Oral Maxillofac. Surg. 2017, 118, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Roy, T.; Steinbacher, D.M. Virtual Planning and 3D Printing in Contemporary Orthognathic Surgery. Semin. Plast. Surg. 2022, 36, 169–182. [Google Scholar] [CrossRef] [PubMed]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tolksdorf, K.; Schultze-Mosgau, S.; Jacobs, C.; Tietz, S.; Hennig, C.-L. Orthognathic Surgery with Interdisciplinary Digital Planning in Patients with Geroderma Osteodysplasticum: A Case Report. J. Pers. Med. 2023, 13, 1578. https://doi.org/10.3390/jpm13111578
Tolksdorf K, Schultze-Mosgau S, Jacobs C, Tietz S, Hennig C-L. Orthognathic Surgery with Interdisciplinary Digital Planning in Patients with Geroderma Osteodysplasticum: A Case Report. Journal of Personalized Medicine. 2023; 13(11):1578. https://doi.org/10.3390/jpm13111578
Chicago/Turabian StyleTolksdorf, Konrad, Stefan Schultze-Mosgau, Collin Jacobs, Stephanie Tietz, and Christoph-Ludwig Hennig. 2023. "Orthognathic Surgery with Interdisciplinary Digital Planning in Patients with Geroderma Osteodysplasticum: A Case Report" Journal of Personalized Medicine 13, no. 11: 1578. https://doi.org/10.3390/jpm13111578




