Pharmacokinetics of Tamoxifen and Its Major Metabolites and the Effect of the African Ancestry Specific CYP2D6*17 Variant on the Formation of the Active Metabolite, Endoxifen
Abstract
:1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. CYP2D6 Genotype
2.3. Measurement of Plasma Tamoxifen and Metabolite Concentrations
2.4. Bioanalysis of Tamoxifen and Metabolites
2.5. LC-MS/MS Conditions
2.6. Pharmacokinetic Analysis
2.7. CYP2D6*17 Activity Score and Calibration Curve
3. Statistical Analysis
4. Results
4.1. Baseline Characteristics
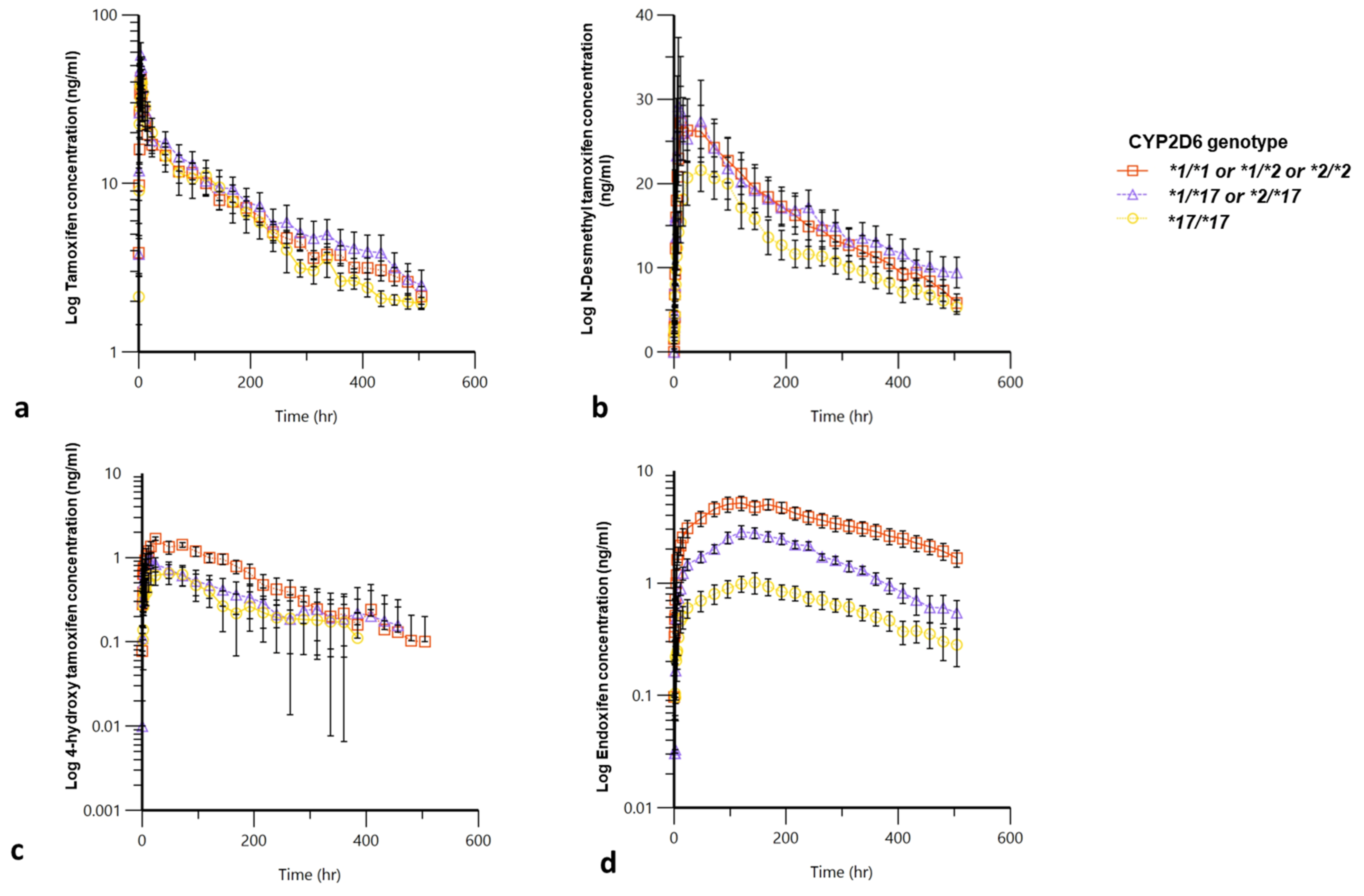
4.2. Pharmacokinetic Analysis
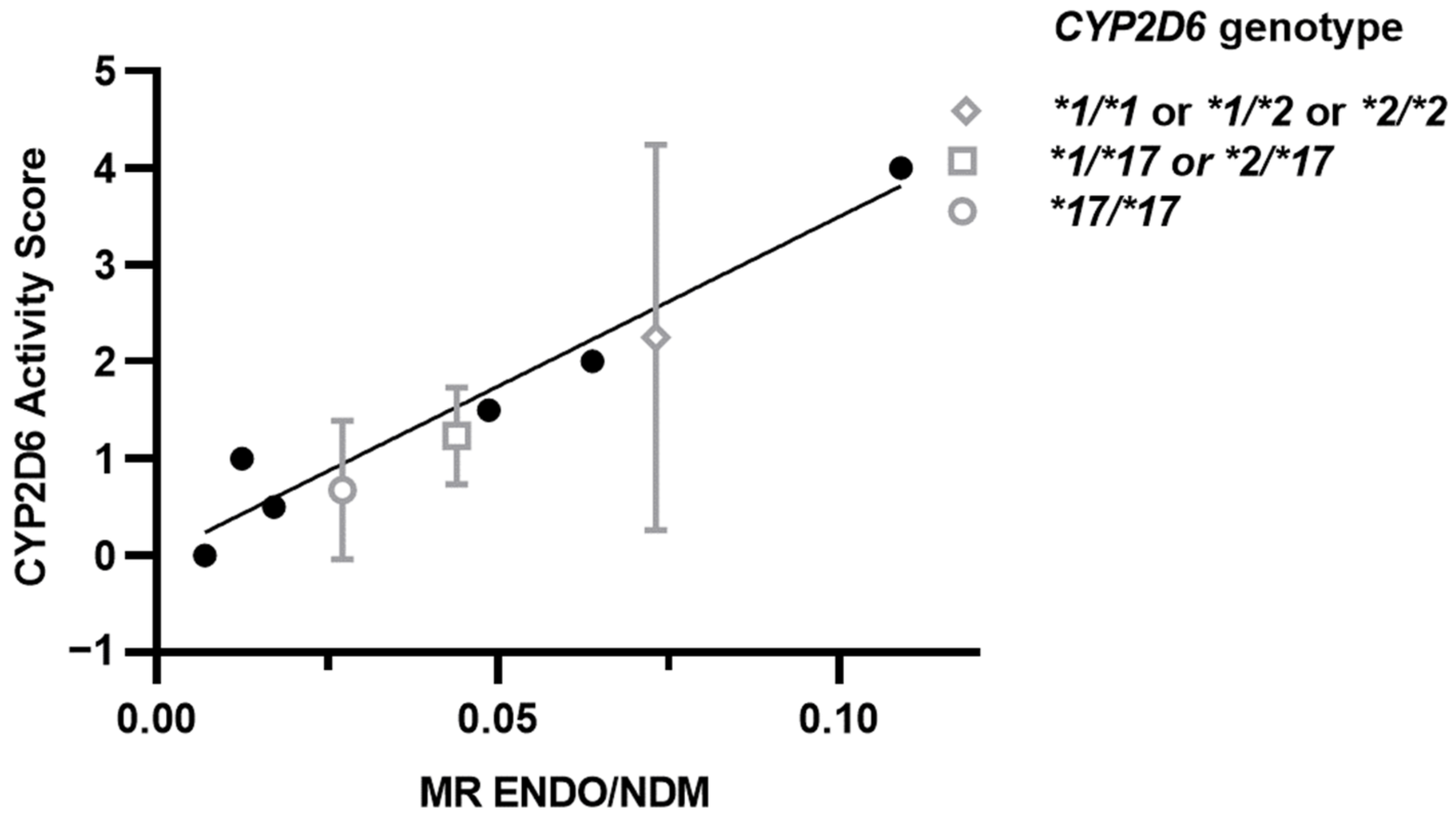
4.3. Activity Score for CYP2D6*17
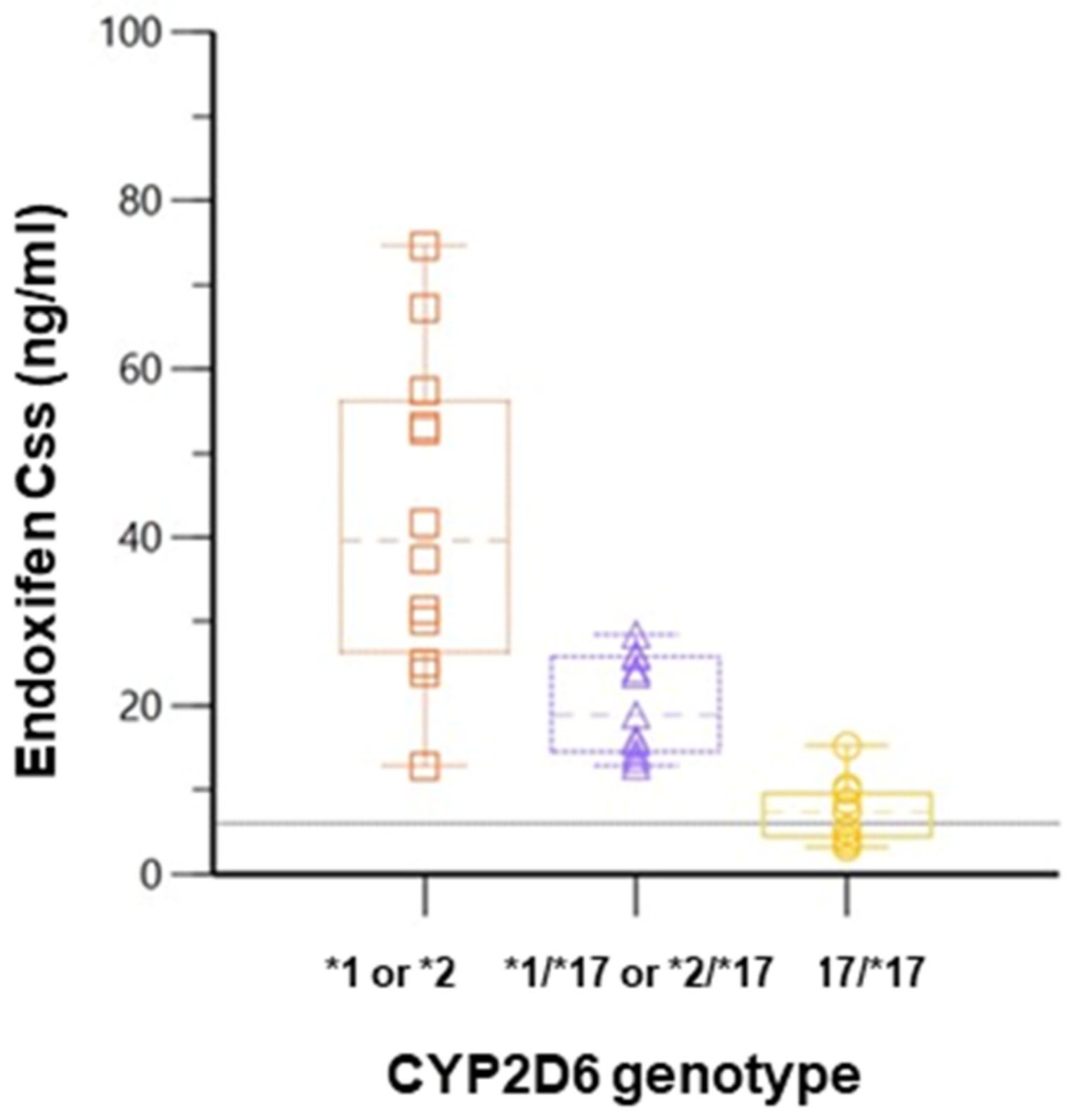
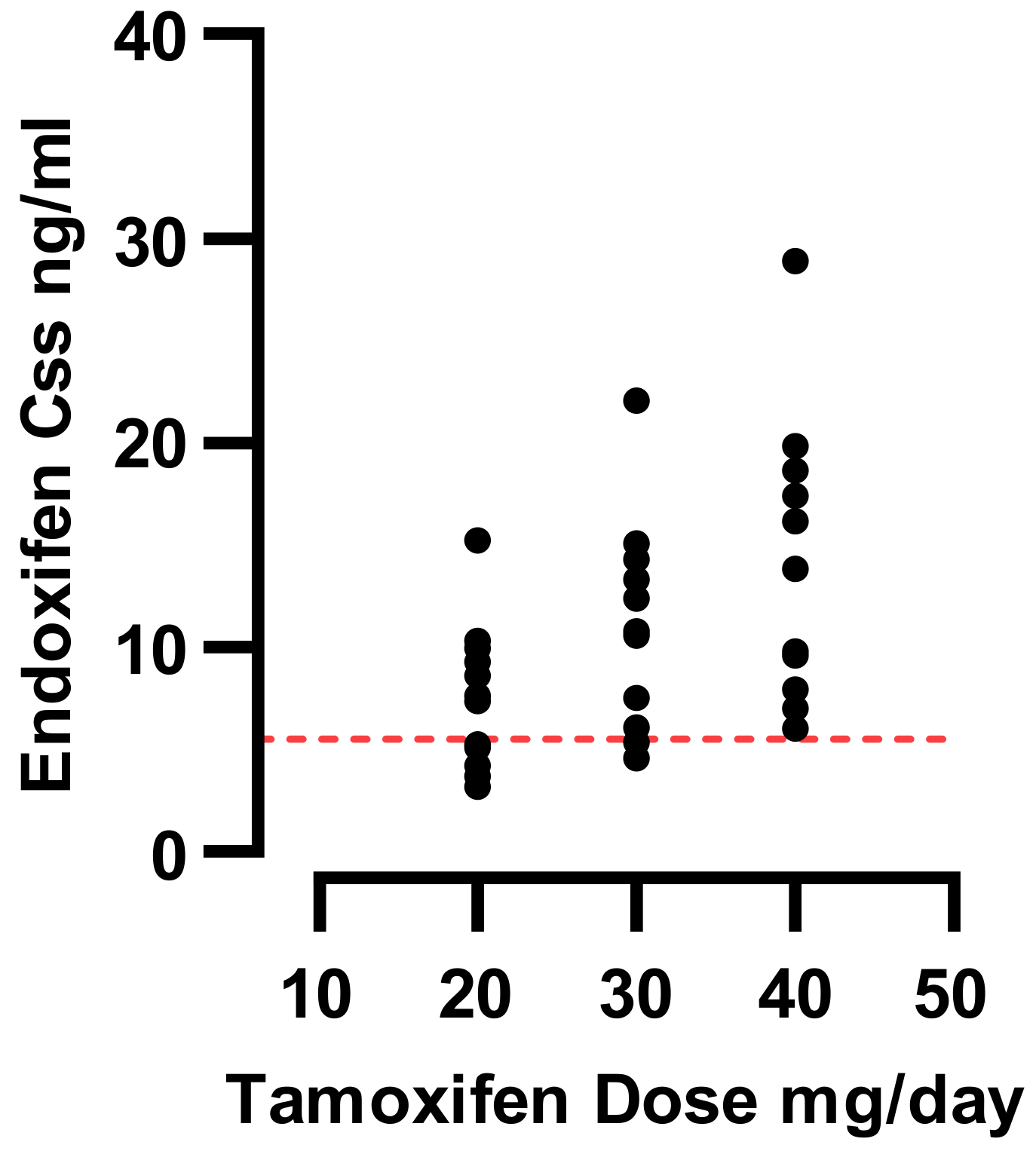
4.4. Dose Escalation and Predicted Endoxifen Css
5. Discussion
Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quirke, V.M. Tamoxifen from Failed Contraceptive Pill to Best-Selling Breast Cancer Medicine: A Case-Study in Pharmaceutical Innovation. Front. Pharm. 2017, 8, 620. [Google Scholar] [CrossRef] [Green Version]
- Gray, R.G.; Rea, D.; Handley, K.; Bowden, S.J.; Perry, P.; Earl, H.M.; Poole, C.J.; Bates, T.; Chetiyawardana, S.; Dewar, J.A.; et al. ATTom: Long-Term Effects of Continuing Adjuvant Tamoxifen to 10 Years versus Stopping at 5 Years in 6,953 Women with Early Breast Cancer. J. Clin. Oncol. 2013, 31, 5. [Google Scholar] [CrossRef]
- Tamoxifen Drug Label. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2005/17970s053lbl.pdf (accessed on 28 July 2022).
- Effects of Chemotherapy and Hormonal Therapy for Early Breast Cancer on Recurrence and 15-Year Survival: An Overview of the Randomised Trials. Lancet 2005, 365, 1687–1717. [CrossRef]
- Kiyotani, K.; Mushiroda, T.; Sasa, M.; Bando, Y.; Sumitomo, I.; Hosono, N.; Kubo, M.; Nakamura, Y.; Zembutsu, H. Impact of CYP2D6*10 on Recurrence-Free Survival in Breast Cancer Patients Receiving Adjuvant Tamoxifen Therapy. Cancer Sci. 2008, 99, 995–999. [Google Scholar] [CrossRef]
- Serrano, D.; Lazzeroni, M.; Zambon, C.F.; MacIs, D.; Maisonneuve, P.; Johansson, H.; Guerrieri-Gonzaga, A.; Plebani, M.; Basso, D.; Gjerde, J.; et al. Efficacy of Tamoxifen Based on Cytochrome P450 2D6, CYP2C19 and SULT1A1 Genotype in the Italian Tamoxifen Prevention Trial. Pharm. J. 2011, 11, 100–107. [Google Scholar] [CrossRef] [Green Version]
- Hansten, P.D. The Underrated Risks of Tamoxifen Drug Interactions. Eur. J. Drug Metab. Pharm. 2018, 43, 495–508. [Google Scholar] [CrossRef] [Green Version]
- McCowan, C.; Wang, S.; Thompson, A.M.; Makubate, B.; Petrie, D.J. The Value of High Adherence to Tamoxifen in Women with Breast Cancer: A Community-Based Cohort Study. Br. J. Cancer 2013, 109, 1172–1180. [Google Scholar] [CrossRef] [Green Version]
- Wood, A.J.J.; Osborne, C.K. Tamoxifen in the Treatment of Breast Cancer. N. Engl. J. Med. 1998, 339, 1609–1618. [Google Scholar] [CrossRef]
- Snozek, C.L.H.; O’Kane, D.J.; Algeciras-Schimnich, A.; Tu, D.; Moore, M.; Zalcberg, J.; Kennecke, H.; Shapiro, J.; Koski, S.; Pavlakis, N.; et al. Pharmacogenetics of Solid Tumors: Directed Therapy in Breast, Lung, and Colorectal Cancer: A Paper from the 2008 William Beaumont Hospital Symposium on Molecular Pathology. J. Mol. Diagn. 2009, 11, 381–389. [Google Scholar] [CrossRef] [Green Version]
- Coller, J.K.; Krebsfaenger, N.; Klein, K.; Endrizzi, K.; Wolbold, R.; Lang, T.; Nüssler, A.; Neuhaus, P.; Zanger, U.M.; Eichelbaum, M.; et al. The Influence of CYP2B6, CYP2C9 and CYP2D6 Genotypes on the Formation of the Potent Antioestrogen Z-4-Hydroxy-Tamoxifen in Human Liver. Br. J. Clin. Pharm. 2002, 54, 157–167. [Google Scholar] [CrossRef]
- Thorén, L.; Lindh, J.D.; Ackehed, G.; Kringen, M.K.; Hall, P.; Bergh, J.; Molden, E.; Margolin, S.; Eliasson, E. Impairment of Endoxifen Formation in Tamoxifen-Treated Premenopausal Breast Cancer Patients Carrying Reduced-Function CYP2D6 Alleles. Br. J. Clin. Pharm. 2021, 87, 1243–1252. [Google Scholar] [CrossRef]
- Puszkiel, A.; Arellano, C.; Vachoux, C.; Evrard, A.; le Morvan, V.; Boyer, J.C.; Robert, J.; Delmas, C.; Dalenc, F.; Debled, M.; et al. Factors Affecting Tamoxifen Metabolism in Patients With Breast Cancer: Preliminary Results of the French PHACS Study. Clin. Pharm. Ther. 2019, 106, 585–595. [Google Scholar] [CrossRef]
- Madlensky, L.; Natarajan, L.; Tchu, S.; Pu, M.; Mortimer, J.; Flatt, S.W.; Nikoloff, D.M.; Hillman, G.; Fontecha, M.R.; Lawrence, H.J.; et al. Tamoxifen Metabolite Concentrations, CYP2D6 Genotype, and Breast Cancer Outcomes. Clin. Pharm. Ther. 2011, 89, 718–725. [Google Scholar] [CrossRef]
- Borges, S.; Desta, Z.; Li, L.; Skaar, T.C.; Ward, B.A.; Nguyen, A.; Jin, Y.; Storniolo, A.M.; Nikoloff, D.M.; Wu, L.; et al. Quantitative Effect of CYP2D6 Genotype and Inhibitors on Tamoxifen Metabolism: Implication for Optimization of Breast Cancer Treatment. Clin. Pharm. Ther. 2006, 80, 61–74. [Google Scholar] [CrossRef]
- Jung, J.A.; Lim, H.S. Association between CYP2D6 Genotypes and the Clinical Outcomes of Adjuvant Tamoxifen for Breast Cancer: A Meta-Analysis. Pharmacogenomics 2013, 15, 49–60. [Google Scholar] [CrossRef]
- Helland, T.; Henne, N.; Bifulco, E.; Naume, B.; Borgen, E.; Kristensen, V.N.; Kvaløy, J.T.; Lash, T.L.; Alnæs, G.I.G.; van Schaik, R.H.; et al. Serum Concentrations of Active Tamoxifen Metabolites Predict Long-Term Survival in Adjuvantly Treated Breast Cancer Patients. Breast Cancer Res. 2017, 19, 1–13. [Google Scholar] [CrossRef]
- Saladores, P.; Mürdter, T.; Eccles, D.; Chowbay, B.; Zgheib, N.K.; Winter, S.; Ganchev, B.; Eccles, B.; Gerty, S.; Tfayli, A.; et al. Tamoxifen Metabolism Predicts Drug Concentrations and Outcome in Premenopausal Patients with Early Breast Cancer. Pharm. J. 2015, 15, 84–94. [Google Scholar] [CrossRef] [Green Version]
- Brauch, H.; Mürdter, T.E.; Eichelbaum, M.; Schwab, M. Pharmacogenomics of Tamoxifen Therapy. Clin. Chem. 2009, 55, 1770–1782. [Google Scholar] [CrossRef] [Green Version]
- Masimirembwa, C.; Persson, I.; Bertilsson, L.; Hasler, J.; Ingelman-Sundberg, M. A Novel Mutant Variant of the CYP2D6 Gene (CYP2D6*17) Common in a Black African Population: Association with Diminished Debrisoquine Hydroxylase Activity. Br. J. Clin. Pharm. 1996, 42, 713–719. [Google Scholar] [CrossRef] [Green Version]
- Yokota, H.; Tamura, S.; Furuya, H.; Kimura, S.; Watanabe, M.; Kanazawa, I.; Kondo, I.; Gonzalez, F.J. Evidence for a New Variant CYP2D6 Allele CYP2D6J in a Japanese Population Associated with Lower in Vivo Rates of Sparteine Metabolism. Pharmacogenetics 1993, 3, 256–263. [Google Scholar] [CrossRef]
- Lim, H.-S.; Ju Lee, H.; Seok Lee, K.; Sook Lee, E.; Jang, I.-J.; Ro, J. Clinical Implications of CYP2D6 Genotypes Predictive of Tamoxifen Pharmacokinetics in Metastatic Breast Cancer. J. Clin. Oncol. 2007, 25, 3837–3845. [Google Scholar] [CrossRef] [PubMed]
- Kiyotani, K.; Mushiroda, T.; Imamura, C.K.; Hosono, N.; Tsunoda, T.; Kubo, M.; Tanigawara, Y.; Flockhart, D.A.; Desta, Z.; Skaar, T.C.; et al. Significant Effect of Polymorphisms in CYP2D6 and ABCC2 on Clinical Outcomes of Adjuvant Tamoxifen Therapy for Breast Cancer Patients. J. Clin. Oncol. 2010, 28, 1287–1293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, H.S.; Choi, J.Y.; Lee, M.J.; Park, S.; Yeo, C.W.; Lee, S.S.; Shin, J.G.; Park, B.W. Association between Genetic Polymorphisms of CYP2D6 and Outcomes in Breast Cancer Patients with Tamoxifen Treatment. J. Korean Med. Sci. 2011, 26, 1007–1013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toyama, T.; Yamashita, H.; Sugiura, H.; Kondo, N.; Iwase, H.; Fujii, Y. No Association Between CYP2D6*10 Genotype and Survival of Node-Negative Japanese Breast Cancer Patients Receiving Adjuvant Tamoxifen Treatment. Jpn J. Clin. Oncol. 2009, 39, 651–656. [Google Scholar] [CrossRef]
- Bradford, L.D. CYP2D6 Allele Frequency in European Caucasians, Asians, Africans and Their Descendants. Pharmacogenomics 2002, 3, 229–243. [Google Scholar] [CrossRef]
- Matimba, A.; Oluka, M.N.; Ebeshi, B.U.; Sayi, J.; Bolaji, O.O.; Guantai, A.N.; Masimirembwa, C.M. Establishment of a Biobank and Pharmacogenetics Database of African Populations. Eur. J. Hum. Genet. 2008, 16, 780–783. [Google Scholar] [CrossRef] [Green Version]
- Dodgen, T.M.; Hochfeld, W.E.; Fickl, H.; Asfaha, S.M.; Durandt, C.; Rheeder, P.; Drögemöller, B.I.; Wright, G.E.B.; Warnich, L.; Labuschagne, C.D.; et al. Introduction of the AmpliChip CYP450 Test to a South African Cohort: A Platform Comparative Prospective Cohort Study. BMC Med. Genet. 2013, 14, 1–15. [Google Scholar] [CrossRef]
- Rajman, I.; Knapp, L.; Morgan, T.; Masimirembwa, C. African Genetic Diversity: Implications for Cytochrome P450-Mediated Drug Metabolism and Drug Development. EBioMedicine 2017, 17, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Matimba, A.; Del-Favero, J.; van Broeckhoven, C.; Masimirembwa, C. Novel Variants of Major Drug-Metabolising Enzyme Genes in Diverse African Populations and Their Predicted Functional Effects. Hum. Genom. 2009, 3, 169–190. [Google Scholar] [CrossRef] [Green Version]
- Caudle, K.E.; Dunnenberger, H.M.; Freimuth, R.R.; Peterson, J.F.; Burlison, J.D.; Whirl-Carrillo, M.; Scott, S.A.; Rehm, H.L.; Williams, M.S.; Klein, T.E.; et al. Standardizing Terms for Clinical Pharmacogenetic Test Results: Consensus Terms from the Clinical Pharmacogenetics Implementation Consortium (CPIC). Genet. Med. 2017, 19, 215–223. [Google Scholar] [CrossRef]
- Goetz, M.P.; Sangkuhl, K.; Guchelaar, H.-J.; Schwab, M.; Province, M.; Whirl-Carrillo, M.; Symmans, W.F.; McLeod, H.L.; Ratain, M.J.; Zembutsu, H.; et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 and Tamoxifen Therapy. Clin. Pharm. Ther. 2018, 103, 770–777. [Google Scholar] [CrossRef] [Green Version]
- Craig Jordan, V. The Role of Tamoxifen in the Treatment and Prevention of Breast Cancer. Curr. Probl. Cancer 1992, 16, 134–176. [Google Scholar] [CrossRef]
- De Vries Schultink, A.H.M.; Zwart, W.; Linn, S.C.; Beijnen, J.H.; Huitema, A.D.R. Effects of Pharmacogenetics on the Pharmacokinetics and Pharmacodynamics of Tamoxifen. Clin. Pharm. 2015, 54, 797–810. [Google Scholar] [CrossRef] [Green Version]
- Sanchez-Spitman, A.B.; Swen, J.J.; Dezentje, V.O.; Moes, D.J.A.R.; Gelderblom, H.; Guchelaar, H.J. Clinical Pharmacokinetics and Pharmacogenetics of Tamoxifen and Endoxifen. Expert Rev. Clin. Pharmacol. 2019, 12, 523–536. [Google Scholar] [CrossRef]
- Desta, Z.; Ward, B.A.; Soukhova, N.V.; Flockhart, D.A. Comprehensive Evaluation of Tamoxifen Sequential Biotransformation by the Human Cytochrome P450 System in Vitro: Prominent Roles for CYP3A and CYP2D6. J. Pharmacol. Exp. Ther. 2004, 310. [Google Scholar] [CrossRef]
- Hertz, D.L.; McLeod, H.L.; Irvin, W.J., Jr. Tamoxifen and CYP2D6: A Contradiction of Data. Oncologist 2012, 17, 620. [Google Scholar] [CrossRef] [Green Version]
- Mürdter, T.E.; Schroth, W.; Bacchus-Gerybadze, L.; Winter, S.; Heinkele, G.; Simon, W.; Fasching, P.A.; Fehm, T.; Eichelbaum, M.; Schwab, M.; et al. Activity Levels of Tamoxifen Metabolites at the Estrogen Receptor and the Impact of Genetic Polymorphisms of Phase I and II Enzymes on Their Concentration Levels in Plasma. Clin. Pharm. Ther. 2011, 89, 708–717. [Google Scholar] [CrossRef]
- Lim, J.S.L.; Chen, X.A.; Singh, O.; Yap, Y.S.; Ng, R.C.H.; Wong, N.S.; Wong, M.; Lee, E.J.D.; Chowbay, B. Impact of CYP2D6, CYP3A5, CYP2C9 and CYP2C19 Polymorphisms on Tamoxifen Pharmacokinetics in Asian Breast Cancer Patients. Br. J. Clin. Pharm. 2011, 71, 737–750. [Google Scholar] [CrossRef] [Green Version]
- Schroth, W.; Antoniadou, L.; Fritz, P.; Schwab, M.; Muerdter, T.; Zanger, U.M.; Simon, W.; Eichelbaum, M.; Brauch, H. Breast Cancer Treatment Outcome With Adjuvant Tamoxifen Relative to Patient CYP2D6 and CYP2C19 Genotypes. J. Clin. Oncol. 2007, 25, 5187–5193. [Google Scholar] [CrossRef]
- Marcath, L.A.; Deal, A.M.; van Wieren, E.; Danko, W.; Walko, C.M.; Ibrahim, J.G.; Weck, K.E.; Jones, D.R.; Desta, Z.; McLeod, H.L.; et al. Comprehensive Assessment of Cytochromes P450 and Transporter Genetics with Endoxifen Concentration during Tamoxifen Treatment. Pharm. Genom. 2017, 27, 402. [Google Scholar] [CrossRef]
- Khan, B.A.; Robinson, R.; Fohner, A.E.; Muzquiz, L.A.I.; Schilling, B.D.; Beans, J.A.; Olnes, M.J.; Trawicki, L.; Frydenlund, H.; Laukes, C.; et al. Cytochrome P450 Genetic Variation Associated with Tamoxifen Biotransformation in American Indian and Alaska Native People. Clin. Transl. Sci. 2018, 11, 312–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, S.F. Polymorphism of Human Cytochrome P450 2D6 and Its Clinical Significance: Part II. Clin. Pharmacokinet. 2009, 48, 761–804. [Google Scholar] [CrossRef]
- Adam, H.K.; Patterson, J.S.; Kemp, J.V. Studies on the Metabolism and Pharmacokinetics of Tamoxifen in Normal Volunteers. Cancer Treat. Rep. 1980, 64, 761–764. [Google Scholar] [PubMed]
- Fromson, J.M.; Pearson, S.; Bramah, S. The Metabolism of Tamoxifen (I.C.I. 46,474). II. In Female Patients. Xenobiotica 1973, 3, 711–714. [Google Scholar] [CrossRef] [PubMed]
- Accessdata.Fda.Gov. Drug Approval Package: Nolvadex (Tamoxifen Citrate) NDA #21-109. 2019. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2002/21109_Nolvadex_prntlbl.pdf (accessed on 22 April 2022).
- Etienne, M.C.; Milano, G.; Fischel, J.L.; Frenay, M.; François, E.; Formento, J.L.; Gioanni, J.; Namer, M. Tamoxifen Metabolism: Pharmacokinetic and in Vitro Study. Br. J. Cancer 1989, 60, 30–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuchs, W.S.; Leary, W.P.; van der Meer, M.J.; Gay, S.; Witschital, K.; von Nieciecki, A. Pharmacokinetics and Bioavailability of Tamoxifen in Postmenopausal Healthy Women. Arzneimittelforschung 1996, 46, 418–422. [Google Scholar]
- Teft, W.A.; Gong, I.Y.; Dingle, B.; Potvin, K.; Younus, J.; Vandenberg, T.A.; Brackstone, M.; Perera, F.E.; Choi, Y.H.; Zou, G.; et al. CYP3A4 and Seasonal Variation in Vitamin D Status in Addition to CYP2D6 Contribute to Therapeutic Endoxifen Level during Tamoxifen Therapy. Breast Cancer Res. Treat. 2013, 139, 95–105. [Google Scholar] [CrossRef]
- Schroth, W.; Winter, S.; Mürdter, T.; Schaeffeler, E.; Eccles, D.; Eccles, B.; Chowbay, B.; Khor, C.C.; Tfayli, A.; Zgheib, N.K.; et al. Improved Prediction of Endoxifen Metabolism by Cyp2d6 Genotype in Breast Cancer Patients Treated with Tamoxifen. Front. Pharm. 2017, 8, 582. [Google Scholar] [CrossRef] [Green Version]
- Braal, C.L.; Westenberg, J.D.; Buijs, S.M.; Abrams, S.; Mulder, T.A.M.; van Schaik, R.H.N.; Koolen, S.L.W.; Jager, A.; Mathijssen, R.H.J. Factors Affecting Inter-Individual Variability in Endoxifen Concentrations in Patients with Breast Cancer: Results from the Prospective TOTAM Trial. Breast Cancer Res. Treat. 2022, 195, 65–74. [Google Scholar] [CrossRef]
- Boucenna, A.; Boudaoud, K.; Hireche, A.; Rezgoune, M.L.; Abadi, N.; Filali, T.; Satta, D. Influence of CYP2D6, CYP2C19 and CYP3A5 Polymorphisms on Plasma Levels of Tamoxifen Metabolites in Algerian Women with ER+ Breast Cancer. Egypt. J. Med. Hum. Genet. 2022, 23, 1–11. [Google Scholar] [CrossRef]
- Goetz, M.P.; Knox, S.K.; Suman, V.J.; Rae, J.M.; Safgren, S.L.; Ames, M.M.; Visscher, D.W.; Reynolds, C.; Couch, F.J.; Lingle, W.L.; et al. The Impact of Cytochrome P450 2D6 Metabolism in Women Receiving Adjuvant Tamoxifen. Breast Cancer Res. Treat. 2007, 101, 113–121. [Google Scholar] [CrossRef]
- Schroth, W.; Goetz, M.P.; Hamann, U.; Fasching, P.A.; Schmidt, M.; Winter, S.; Fritz, P.; Simon, W.; Suman, V.J.; Ames, M.M.; et al. Association Between CYP2D6 Polymorphisms and Outcomes Among Women With Early Stage Breast Cancer Treated With Tamoxifen. JAMA 2009, 302, 1429. [Google Scholar] [CrossRef] [Green Version]
- Goetz, M.P.; Rae, J.M.; Suman, V.J.; Safgren, S.L.; Ames, M.M.; Visscher, D.W.; Reynolds, C.; Couch, F.J.; Lingle, W.L.; Flockhart, D.A.; et al. Pharmacogenetics of Tamoxifen Biotransformation Is Associated with Clinical Outcomes of Efficacy and Hot Flashes. J. Clin. Oncol. 2005, 23, 9312–9318. [Google Scholar] [CrossRef]
- Kiyotani, K.; Mushiroda, T.; Imamura, C.K.; Tanigawara, Y.; Hosono, N.; Kubo, M.; Sasa, M.; Nakamura, Y.; Zembutsu, H. Dose-Adjustment Study of Tamoxifen Based on CYP2D6 Genotypes in Japanese Breast Cancer Patients. Breast Cancer Res. Treat. 2012, 131, 137–145. [Google Scholar] [CrossRef]
- Martinez de Dueñas, E.; Ochoa Aranda, E.; Blancas Lopez-Barajas, I.; Ferrer Magdalena, T.; Bandrés Moya, F.; Chicharro García, L.M.; Gómez Capilla, J.A.; Zafra Ceres, M.; de Haro, T.; Romero Llorens, R.; et al. Adjusting the Dose of Tamoxifen in Patients with Early Breast Cancer and CYP2D6 Poor Metabolizer Phenotype. Breast 2014, 23, 400–406. [Google Scholar] [CrossRef]
- Hertz, D.L.; Deal, A.; Ibrahim, J.G.; Walko, C.M.; Weck, K.E.; Anderson, S.; Magrinat, G.; Olajide, O.; Moore, S.; Raab, R.; et al. Tamoxifen Dose Escalation in Patients With Diminished CYP2D6 Activity Normalizes Endoxifen Concentrations Without Increasing Toxicity. Oncologist 2016, 21, 795–803. [Google Scholar] [CrossRef] [Green Version]
- Khalaj, Z.; Baratieh, Z.; Nikpour, P.; Schwab, M.; Schaeffeler, E.; Mokarian, F.; Khanahmad, H.; Salehi, R.; Mürdter, T.E.; Salehi, M. Clinical Trial: CYP2D6 Related Dose Escalation of Tamoxifen in Breast Cancer Patients with Iranian Ethnic Background Resulted in Increased Concentrations of Tamoxifen and Its Metabolites. Front. Pharm. 2019, 10, 530. [Google Scholar] [CrossRef] [Green Version]
- Fox, P.; Balleine, R.L.; Lee, C.; Gao, B.; Balakrishnar, B.; Menzies, A.M.; Yeap, S.H.; Ali, S.S.; Gebski, V.; Provan, P.; et al. Dose Escalation of Tamoxifen in Patients with Low Endoxifen Level: Evidence for Therapeutic Drug Monitoring-The TADE Study. Clin. Cancer Res. 2016, 22, 3164–3171. [Google Scholar] [CrossRef] [Green Version]
- Puszkiel, A.; Arellano, C.; Vachoux, C.; Evrard, A.; le Morvan, V.; Boyer, J.C.; Robert, J.; Delmas, C.; Dalenc, F.; Debled, M.; et al. Model-Based Quantification of Impact of Genetic Polymorphisms and Co-Medications on Pharmacokinetics of Tamoxifen and Six Metabolites in Breast Cancer. Clin. Pharm. Ther. 2021, 109, 1244–1255. [Google Scholar] [CrossRef]
- Braal, C.L.; Jager, A.; de Hoop, E.O.; Westenberg, J.D.; Lommen, K.M.W.T.; de Bruijn, P.; Vastbinder, M.B.; van Rossum-Schornagel, Q.C.; Thijs-Visser, M.F.; van Alphen, R.J.; et al. Therapeutic Drug Monitoring of Endoxifen for Tamoxifen Precision Dosing: Feasible in Patients with Hormone-Sensitive Breast Cancer. Clin. Pharm. 2022, 61, 527–537. [Google Scholar] [CrossRef]
- De Vries Schultink, A.H.M.; Huitema, A.D.R.; Beijnen, J.H. Therapeutic Drug Monitoring of Endoxifen as an Alternative for CYP2D6 Genotyping in Individualizing Tamoxifen Therapy. Breast 2018, 42, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Dezentjé, V.O.; Opdam, F.L.; Gelderblom, H.; Hartigh den, J.; van der Straaten, T.; Vree, R.; Maartense, E.; Smorenburg, C.H.; Putter, H.; Dieudonné, A.S.; et al. CYP2D6 Genotype- and Endoxifen-Guided Tamoxifen Dose Escalation Increases Endoxifen Serum Concentrations without Increasing Side Effects. Breast Cancer Res. Treat. 2015, 153. [Google Scholar] [CrossRef] [PubMed]
- Binkhorst, L.; Bannink, M.; de Bruijn, P.; Ruit, J.; Droogendijk, H.; van Alphen, R.J.; den Boer, T.D.; Lam, M.H.; Jager, A.; van Gelder, T.; et al. Augmentation of Endoxifen Exposure in Tamoxifen-Treated Women Following SSRI Switch. Clin. Pharm. 2016, 55, 249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Binkhorst, L.; van Gelder, T.; Loos, W.J.; de Jongh, F.E.; Hamberg, P.; Moghaddam-Helmantel, I.M.G.; de Jonge, E.; Jager, A.; Seynaeve, C.; van Schaik, R.H.N.; et al. Effects of CYP Induction by Rifampicin on Tamoxifen Exposure. Clin. Pharm. Ther. 2012, 92, 62–67. [Google Scholar] [CrossRef]
- Buck, S.A.J.; Braal, C.L.; Hofman, M.M.; Oomen-de Hoop, E.; de Bruijn, P.; Ghobadi Moghaddam-Helmantel, I.M.; Hussaarts, K.G.A.M.; Vastbinder, M.B.; van Rossum-Schornagel, Q.C.; van Schaik, R.H.N.; et al. Influence of Probenecid on Endoxifen Systemic Exposure in Breast Cancer Patients on Adjuvant Tamoxifen Treatment. Ther. Adv. Med. Oncol. 2022, 14, 17588359221081075. [Google Scholar] [CrossRef]
- Becker, S.L. The Role of Pharmacological Enhancement in Protease Inhibitor-Based Highly Active Antiretroviral Therapy. Expert Opin. Investig. Drugs 2003, 12, 401–412. [Google Scholar] [CrossRef]
- Muroi, Y.; Saito, T.; Takahashi, M.; Sakuyama, K.; Niinuma, Y.; Ito, M.; Tsukada, C.; Ohta, K.; Endo, Y.; Oda, A.; et al. Functional Characterization of Wild-Type and 49 CYP2D6 Allelic Variants for N-Desmethyltamoxifen 4-Hydroxylation Activity. Drug Metab. Pharm. 2014, 29, 360–366. [Google Scholar] [CrossRef] [Green Version]
- Abdullah-Koolmees, H.; van Keulen, A.M.; Nijenhuis, M.; Deneer, V.H.M. Pharmacogenetics Guidelines: Overview and Comparison of the DPWG, CPIC, CPNDS, and RNPGx Guidelines. Front. Pharm. 2021, 11, 595219. [Google Scholar] [CrossRef]
- Caudle, K.E.; Sangkuhl, K.; Whirl-Carrillo, M.; Swen, J.J.; Haidar, C.E.; Klein, T.E.; Gammal, R.S.; Relling, M.V.; Scott, S.A.; Hertz, D.L.; et al. Standardizing CYP2D6 Genotype to Phenotype Translation: Consensus Recommendations from the Clinical Pharmacogenetics Implementation Consortium and Dutch Pharmacogenetics Working Group. Clin. Transl. Sci. 2020, 13, 116–124. [Google Scholar] [CrossRef] [Green Version]
- Wennerholm, A.; Dandara, C.; Sayi, J.; Svensson, J.O.; Abdi, Y.A.; Ingelman-Sundberg, M.; Bertilsson, L.; Hasler, J.; Gustafsson, L.L. The African-Specific CYP2D617 Allele Encodes an Enzyme with Changed Substrate Specificity. Clin. Pharm. Ther. 2002, 71, 77–88. [Google Scholar] [CrossRef]
- Molden, E.; Jukić, M.M. CYP2D6 Reduced Function Variants and Genotype/Phenotype Translations of CYP2D6 Intermediate Metabolizers: Implications for Personalized Drug Dosing in Psychiatry. Front. Pharm. 2021, 12, 761. [Google Scholar] [CrossRef]
- Van der Lee, M.; Guchelaar, H.J.; Swen, J.J. Substrate Specificity of CYP2D6 Genetic Variants. Pharmacogenomics 2021, 22, 1081–1089. [Google Scholar] [CrossRef]
- Eggemann, H.; Brucker, C.; Schrauder, M.; Thill, M.; Flock, F.; Reinisch, M.; Costa, S.D.; Ignatov, A. Survival Benefit of Tamoxifen in Male Breast Cancer: Prospective Cohort Analysis. Br. J. Cancer 2020, 123, 33–37. [Google Scholar] [CrossRef]
- Lenehan, J.G.; Teft, W.A.; Kim, R.B. Comparison of Endoxifen Levels between Male and Female Breast Cancer Patients Treated with Tamoxifen. J. Clin. Oncol. 2016, 34, 578. [Google Scholar] [CrossRef]

| Participant Baseline Characteristics | ||
|---|---|---|
| N 1 | 42 | |
| Sex | Female (N, [%]) | 3 [7] |
| Male (N, [%]) | 39 [93] | |
| Race | Black | |
| Age: years (median, [range]) | 23.4 [19.1–30.2] | |
| Weight: kg (median, [range]) | 65.0 [53–89] | |
| Height: cm (median, [range]) | 173.0 [155–192] | |
| BMI: kg/m2 (median,] [range]) | 22.5 [19.2−26.7] | |
| CYP2D6*1/*1, *1/*2 or *2/*2 | CYP2D6*1/*17 or *2/*17 | CYP2D6*17/*17 | p Value | |
|---|---|---|---|---|
| Tamoxifen | ||||
| Cmax (ng/mL) | 51.88 (18.25) | 62.96 (25.68) | 54.23 (14.13) | 0.3803 |
| Tmax (h) | 4.154 (1.97) | 3.94 (1.27) | 4.67 (2.22) | 0.0503 |
| AUC0-last (h·ng/mL) | 3650.75 (1203.75) | 4246.94 (2068.27) | 3520.99 (1874.01) | 0.5116 |
| AUC0-∞ (h·ng/mL) | 4560.56 (2030.04) | 4853.29 (2285.58) | 4673.49 (2036.21) | 0.9345 |
| Thalf (h) | 152.81 (44.15) | 160.90 (34.58) | 165.27 (60.73) | 0.7834 |
| V/f (L) | 1530.42 (833.69) | 1166.25 (585.18) | 1344.75 (790.65) | 0.4404 |
| CL (L/h) | 4.88 (1.38) | 4.84 (1.90) | 4.97 (1.84) | 0.9793 |
| N-desmethyl tamoxifen | ||||
| Cmax (ng/mL) | 33.98 (16.01) | 39.66 (20.33) | 31.37 (9.447) | 0.3791 |
| Tmax (h) | 39 (27.09) | 25.25 (19.15) | 49.78 (31.44) | 0.0593 |
| AUC0-last (h·ng/mL) | 8542.90 (2863.16) | 7742.71 (2072.57) | 7232.27 (1387.74) | 0.2918 |
| AUC0-∞ (h·ng/mL) | 10,680.76 (4546.64) | 9944.45 (2567.0) | 9372.26 (2088.38) | 0.5693 |
| Thalf (h) | 262.00 (114.97) | 297.06 (179.08 | 256.24 (125.26) | 0.7165 |
| V/f (L) | 666.231 (299.65) | 578.21 (353.64) | 603.4 (240.53) | 0.7306 |
| CL (L/h) | 2.30 (1.04) | 1.79 (0.4) | 2.39 (0.55) | 0.0701 |
| 4-Hydroxy-tamoxifen | ||||
| Cmax (ng/mL) | 1.518 (0.57) | 1.06 (0.41) | 0.724 (0.360 | 0.0002 * |
| Tmax (h) | 29.33 (14.89) | 24 (16.49) | 44.8 (28.06) | 0.0340 * |
| AUC0-last (h·ng/mL) | 245.33 (142) | 218.72 (153.63) | 132.318 (121.7) | 0.0950 |
| AUC0-∞ (h·ng/mL) | 321.067 (129.19) | 299.35 (168.81) | 245.27 (170.76) | 0.4305 |
| Thalf (h) | 98.57 (79.17) | 122.99 (50.12) | 103.14 (65.24) | 0.6036 |
| V/f (L) | 4229.37 (2072.66) | 4629.26 (1752.04) | 30,269.62 (7873.91) | <0.001 * |
| CL (L/h) | 103.64 (32.79) | 128.48 (69.80) | 288.16 (257.62) | 0.070 |
| Endoxifen | ||||
| Cmax (ng/mL) | 5.26 (2.14) | 2.95 (1.0) | 1.034 (0.50) | <0.001 * |
| Tmax (h) | 124.8 (40.8) | 132 (18.14) | 144 (26.83) | 0.2517 |
| AUC0-last (h·ng/mL) | 1857.62 (854.39) | 808.42 (180.82) | 355.51 (132.36) | <0.001 * |
| AUC0-∞ (h·ng/mL) | 2625.5 (1167.68) | 930.69 (212.41) | 452.01 (196.94) | <0.001 * |
| Thalf (h) | 246.05 (102.01) | 171.87 (35.49) | 243.71 (99.46) | 0.0508 |
| V/f (L) | 3324.79 (1825) | 3940.09 (2330.34) | 11,931.32 (4261.43) | <0.001 * |
| CL (L/h) | 12.57 (9.99) | 20.35 (6.2) | 38.6 (17.63) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanji, C.R.; Nyabadza, G.; Nhachi, C.; Masimirembwa, C. Pharmacokinetics of Tamoxifen and Its Major Metabolites and the Effect of the African Ancestry Specific CYP2D6*17 Variant on the Formation of the Active Metabolite, Endoxifen. J. Pers. Med. 2023, 13, 272. https://doi.org/10.3390/jpm13020272
Kanji CR, Nyabadza G, Nhachi C, Masimirembwa C. Pharmacokinetics of Tamoxifen and Its Major Metabolites and the Effect of the African Ancestry Specific CYP2D6*17 Variant on the Formation of the Active Metabolite, Endoxifen. Journal of Personalized Medicine. 2023; 13(2):272. https://doi.org/10.3390/jpm13020272
Chicago/Turabian StyleKanji, Comfort Ropafadzo, Georginah Nyabadza, Charles Nhachi, and Collen Masimirembwa. 2023. "Pharmacokinetics of Tamoxifen and Its Major Metabolites and the Effect of the African Ancestry Specific CYP2D6*17 Variant on the Formation of the Active Metabolite, Endoxifen" Journal of Personalized Medicine 13, no. 2: 272. https://doi.org/10.3390/jpm13020272
APA StyleKanji, C. R., Nyabadza, G., Nhachi, C., & Masimirembwa, C. (2023). Pharmacokinetics of Tamoxifen and Its Major Metabolites and the Effect of the African Ancestry Specific CYP2D6*17 Variant on the Formation of the Active Metabolite, Endoxifen. Journal of Personalized Medicine, 13(2), 272. https://doi.org/10.3390/jpm13020272







