Abstract
Coronary heart disease (CHD) is one of the main cardiovascular diseases that can cause disability and death across the globe. Although previous research explored the links between CHD and cognitive deficits, only a subset of cognitive abilities was analyzed and a small clinical sample size was used. Thus, the aim of the current study is to assess how CHD can affect the cognitive domains of episodic memory, semantic verbal fluency, fluid reasoning, and numerical ability in a large cohort of participants from the United Kingdom. Results revealed that episodic memory, semantic verbal fluency, fluid reasoning, and numerical ability are negatively affected by CHD. Prevention and intervention should be developed to preserve cognitive abilities in people with CHD, but more studies should explore specific ways of doing so.
1. Introduction
As one of the main cardiovascular diseases, coronary heart disease (CHD) is the world’s leading cause of disability and death [1]. CHD is characterized by a lot of clinical symptoms, manifested as angina, myocardial infarction (MI), and/or sudden cardiac death [2,3].
Cognitive deficits are very common among older people, which are characterized by a lower performance on a wide range of cognitive domains, such as attention, memory, and executive function, even after accounting for age and educational level [4]. Dementia is a state of disease in which cognitive deficits are severe enough to affect normal functioning [5]. According to studies, the global prevalence of dementia ranges between 5% and 7%, with the highest rate in developing countries [5]. Cognitive impairments impose significant individual, societal, and financial burdens on people, especially as the world’s population ages [6].
Regarding the associations between CHD and cognitive impairments, some previous studies found that CHD is a major risk factor of cognitive decline [7,8], whereas others found no link between cognitive impairments and CHD [9,10]. A more recent meta-analysis found a link between CHD and the risk of cognitive impairment [11]. Subgroup findings also revealed that people with CHD are at a higher risk of developing vascular dimensions, but not Alzheimer’s disease [11,12].
There are several reasons that can explain why CHD could negatively affect cognition, which may include (1) common risk factors of both CHD and cognitive impairments, such as low physical activities, (2) CABG surgery, which may affect cognitive abilities in people with CHD, and (3) inflammation associated with CHD (see [11]).
Thus, the relationship between CHD and cognitive impairments remains unclear given that the variability in these studies primarily involved small clinical samples. Therefore, there is a need for cohort-based studies, which are characterized by high generalizability. In addition, cognition is not a unitary concept but has multiple components. Previous studies focused on one or more cognitive domains in one study but ignored others. Thus, the aim of the current study is to assess how CHD can affect the cognitive domains of episodic memory, semantic verbal fluency, fluid reasoning, and numerical ability in a large cohort of participants from the United Kingdom.
2. Methods
2.1. Data
We extracted and analyzed data from Understanding Society: collected annual data from a representative sample of UK households since 1991, the UK Household Longitudinal Study (UKHLS) [13]. Participants were asked whether they have been clinically diagnosed with CHD in Wave 1 (collected between 2009 and 2010). After that, participants were asked if they had been clinically diagnosed with CHD in each wave until Wave 3. Participants completed cognitive measures at Wave 3 (collected between 2011 and 2012). We removed individuals with any missing fields of interest. Age- and sex-matched healthy controls were chosen from the people who indicated that they were not clinically diagnosed with CHD. Thus, there were 260 participants with clinically diagnosed CHD, with a mean age of 63.61 ± 16.19 (61.15% males), and 4782 participants without CHD with a mean age of 63.40 ± 9.90 (61.36% males).
2.2. Measures
2.2.1. CHD
In population-based studies, the validity of self-reported cardiovascular disease has been approved (e.g., [14]). The question “Has a doctor or other health professional ever told you that you have any of these conditions?” was used to assess CHD in retrospect at Wave 1. Following-up waves asked participants if they had recently been diagnosed with CHD.
2.2.2. Cognitive Abilities
Episodic memory was assessed with immediate and delayed word recall tasks. An animal fluency task was used to assess semantic verbal fluency [15,16,17]. The number series task is intended to assess fluid reasoning, or the ability to solve novel problems using abstract thought. Logic puzzles are commonly used to assess fluid reasoning [15]. Numerical ability tests involve solving problems that might be encountered in daily life, which was measured by a series of questions such as “In a sale, a shop is selling all items at half price. Before the sale, a sofa costs £300. How much will it cost in the sale?” Details of the procedures of these tasks can be found at: https://www.understandingsociety.ac.uk/sites/default/files/downloads/documentation/mainstage/user-guides/6614_Cognitive_Ability_measures_v1.1.pdf (accessed on 10 January 2022) and were copied below. All scores were standardized before further analysis (mean = 0, S.D. = 1).
The immediate and delayed recall tasks: “For this task, the computer reads a list of 10 words to standardise the presentation and speed of the word list. The interviewer checks if the respondent can hear the computer playing a short test message. If the voice cannot be heard, the interviewer checks again, following adjustment of the volume. If the respondent still cannot hear the computer’s voice, the interviewer reads the words at a slow steady rate of about one word every two seconds. The list of words is not repeated. No aids are allowed for the test. Interviewer: The computer will now read a set of 10 words. I would like you to remember as many as you can. We have purposely made the list long so it will be difficult for anyone to remember all the words. Most people remember just a few. Please listen carefully to the set of words, as they cannot be repeated. When it has finished, I will ask you to recall aloud as many of the words as you can, in any order. Is this clear? Now please tell me the words you can remember. Respondents give the words in any order. The interviewer codes each correct response. For the delayed word recall test, after the Number Series test (below), respondents were again asked to remember the words from the list. The interviewer codes each correct response. We used the word lists developed for the HRS, as does ELSA. The different lists were given to members of the same household based on random assignment. The lists can also be varied in subsequent waves to reduce learning.”
Animal naming task: “Interviewer: Now, I would like you to name as many animals as you can. You have one-minute, so name them as quickly as possible. We will begin when you say the first animal. If you are unsure of anything, please ask me now, as I am unable to answer questions once the minute starts. The interviewer instructions are to write down the actual words in the order in which they are produced. They are recorded in the Cognitive Ability Booklet. With respect to scoring, extinct, imaginary or magical (e.g., dodo, unicorn, dragon) animals were scored as correct, but given names (e.g., Felix, Buster) were not. The assessment was timed by CAPI. The interviewer began the 60 s countdown on the computer as soon as the respondent said the first correct word.”
Number series task: “For this test, respondents use a pencil and paper to write down the number sequences as read by the interviewer. The number series consists of several numbers with a blank number in the series. The respondent will be asked which number goes in the blank. The interviewer begins with a simple example so the respondent can see how the test works. For the example, the interviewer can tell the respondent if they give an incorrect response and inform them of the correct answer. If the respondent does not understand the instructions, or answered ‘Don’t know’ in the example, a further example is worked through. If they answer incorrectly a second time, CAPI instructs the interviewer to inform them of the correct response and explain how the sequence works. If the respondent still does not understand, or seems confused, the interviewer codes this and moves on to the next task. However, if the respondent understands the task, the interviewer moved on to the number series.”
Numerical ability test: “Interviewer: Next, I would like to ask you some questions to understand how people use numbers in everyday life. If CATI, the interviewer added: You might want to have a pencil and paper handy to help you answer the following items. The measure of numeric ability asks respondents up to five questions that are graded in complexity. Based on performance on the first three items, respondents can get additional more difficult items and a higher score, or an additional more simple item. ‘Don’t know’ was not a permitted response. There was a showcard with the text of the question. This can be seen in the fieldwork documents: https://www.understandingsociety.ac.uk/documentation/mainstage/fieldworkdocuments (accessed on 1 January 2020).”
2.2.3. Demographic Controls
Demographic controls included age, sex, monthly income, highest educational qualification, legal marital status, and residence. The way these variables were coded in the model can be found in Table 1.

Table 1.
Descriptive statistics of demographic characteristics and cognitive performance for people with and without CHD.
2.3. Analysis
A train-and-test approach was used to analyze this dataset. First, five generalized linear models were constructed based on data from people without CHD, by taking demographic controls in the model including age, sex, monthly income, highest educational qualification, legal marital status, and residence into the model as independent variables to predict outcome cognitive variables, including the delayed word recall, the immediate word recall, numeracy, and the number series scores. Then demographics from people with CHD were input into these models to estimate the expected scores of people with CHD, as if they have not been clinically diagnosed with CHD. Finally, one-sample t-tests were used to determine the differences between the expected and actual cognitive scores of people with CHD. This approach has more advantages than paired-sample t-tests, because it does not require equal same size and can control potential confounders, such as demographics.
3. Results
Descriptive statistics can be found in Table 1. The estimates (b) of the linear models trained on healthy controls can be found in Table 2. The main findings were that people with CHD are characterized by a lower immediate word recall (t(259) = −2.81, p < 0.01, Cohen’s d = −0.15, 95% C.I. = [−0.25, −0.04]), delayed word recall (t(259) = −3.31, p < 0.01, Cohen’s d = −0.17, 95% C.I. = [−0.27, −0.07]), semantic verbal fluency (t(259) = −3.82, p < 0.001, Cohen’s d = −0.23, 95% C.I. = [−0.35, −0.11]), and fluid reasoning (t(259) = −2.96, p < 0.01, Cohen’s d = −0.17, 95% C.I. = [−0.28, −0.06]), compared to what they would expect given their demographics (Figure 1).

Table 2.
The estimates (b) of linear models trained based on demographic predictors.
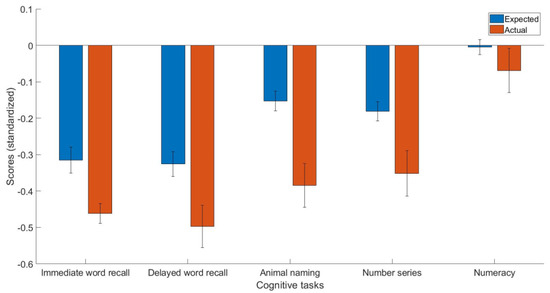
Figure 1.
The expected and actual cognitive task scores in people with CHD.
4. Discussion
Taken together, the current study’s goal is to assess how CHD can affect the cognitive domains of episodic memory, semantic verbal fluency, fluid reasoning, and numerical ability in a large cohort of participants from the United Kingdom. Results revealed that episodic memory, semantic verbal fluency, fluid reasoning, and numerical ability are negatively affected by CHD, which appears to be in line with several previous studies [7,8,11,12], but inconsistent with others that did not find such associations [9,10,12].
However, the potential underlying mechanisms that link CHD and cognitive impairments are still unclear. Previous studies have found several common risk factors for CHD and cognitive impairments among older people, including low physical activity, CHD mellitus, and hypertension [18,19,20,21,22,23]. Thus, the widely acknowledged cardiovascular risk factors may contribute to the development of cognitive impairments. In addition, studies have found that multiple comorbid cardiovascular risk factors contribute to dementia [23,24,25]. Specifically, Bleckwenn et al. (2017) found that CHD influences cognitive decline in people who have recently been diagnosed with dementia [26]. Atrial fibrillation represents one of the most common cardiac arrhythmias, with its prevalence estimated to be ranging from 0.2 to 5% in CHD patients. After coronary artery bypass graft (CABG) surgery, arrhythmia is another common symptom, occurring in approximately 20 to 40% of patients [27]. Atrial fibrillation has been identified as a significant risk factor of cognitive impairment [28,29]. Moreover, CABG surgery is also related to cognitive impairments, with around 50% of patients with cognitive impairment after 1 to 5 years post-surgery [30]. Atherosclerosis progression is closely connected to CHD and negatively affects cerebral vessels, resulting in cerebrovascular dysfunctions and cerebral blood flow impairments [31,32], which may, then, contribute to vascular dementia. Inflammation associated with CHD may also play a role in the cognitive impairment of people with CHD [33,34].
There are some limitations to our study, as well. First, cross-sectional studies cannot establish a causal relationship. A longitudinal approach should be used in future studies to determine the temporal order of CHD diagnosis and cognitive impairments. Second, cardiovascular risk factors, treatment, and medication were not controlled in our study, given that they might have had an influence on the results. Future studies should ascertain information collection about treatment and medication. Third, we did not control for mental health comorbidities, which may have an effect on cognition. Future studies should try to do so. Finally, our study only included people with CHD from the United Kingdom, making it difficult to make assumptions about different countries. Future studies on how CHD can affect cognitive abilities in other countries should be conducted.
In conclusion, we looked at how CHD can affect the cognitive domains of episodic memory, semantic verbal fluency, fluid reasoning, and numerical ability in a large cohort of participants from the United Kingdom. Results revealed that episodic memory, semantic verbal fluency, fluid reasoning, and numerical ability are negatively affected by CHD. However, we were unable to rule out the effect of confounders, such as cardiovascular factors, treatment, and medication. Prevention and intervention should be developed to preserve cognitive abilities in people with CHD, but more studies should explore specific ways of doing so.
Author Contributions
W.K.: conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, writing—original draft, and writing—review and editing. A.M.: writing—original draft and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethics approval was received from the University of Essex-Ethics Committee (Approval Code: ETH1920-0123).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.understandingsociety.ac.uk (accessed on 7 February 2022).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ang, C.S.; Chan, K.M. A review of coronary artery disease research in Malaysia. Med. J. Malays. 2016, 71 (Suppl. S1), 46. [Google Scholar]
- Álvarez-Álvarez, M.M.; Zanetti, D.; Carreras-Torres, R.; Moral, P.; Athanasiadis, G. A survey of sub-Saharan gene flow into the Mediterranean at risk loci for coronary artery disease. Eur. J. Hum. Genet. 2017, 25, 472–476. [Google Scholar] [CrossRef]
- Libby, P.; Theroux, P. Pathophysiology of coronary artery disease. Circulation 2015, 111, 3481–3488. [Google Scholar] [CrossRef]
- Eshkoor, S.A.; Hamid, T.A.; Mun, C.Y.; Ng, C.K. Mild cognitive impairment and its management in older people. Clin. Interv. Aging 2015, 10, 687–693. [Google Scholar] [CrossRef] [PubMed]
- de Souza-Talarico, J.N.; de Carvalho, A.P.; Brucki, S.M.; Nitrini, R.; Ferretti-Rebustini, R.E. Dementia and cognitive impairment prevalence and associated factors in indigenous populations: A systematic review. Alzheimer Dis. Assoc. Disord. 2016, 30, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Dye, L.; Boyle, N.B.; Champ, C.; Lawton, C. The relationship between obesity and cognitive health and decline. Proc. Nutr. Soc. 2017, 76, 443–454. [Google Scholar] [CrossRef]
- Gondim, A.S.; Coelho Filho, J.M.; Cavalcanti, A.A.; Roriz Filho, J.S.; Nogueira, C.B.; Peixoto Junior, A.A.; Lima, J.W.O. Prevalence of functional cognitive impairment and associated factors in Brazilian community-dwelling older adults. Dement. Neuropsychol. 2017, 11, 32–39. [Google Scholar] [CrossRef]
- Mahon, S.; Parmar, P.; Barker-Collo, S.; Krishnamurthi, R.; Jones, K.; Theadom, A.; Feigin, V. Determinants, prevalence, and trajectory of long-term post-stroke cognitive impairment: Results from a 4-year follow-up of the ARCOS-IV Study. Neuroepidemiology 2017, 49, 129–134. [Google Scholar] [CrossRef]
- Xing, Y.L.; Chen, M.A.; Sun, Y.; Neradilek, M.B.; Wu, X.T.; Zhang, D.; Zhao, X.Q. Atherosclerosis, its risk factors, and cognitive impairment in older adults. J. Geriatr. Cardiol. 2020, 17, 434–440. [Google Scholar]
- Yang, Z.; Edwards, D.; Burgess, S.; Brayne, C.; Mant, J. Association of prior atherosclerotic cardiovascular disease with dementia after stroke: A Retrospective Cohort Study. J. Alzheimer’s Dis. 2020, 77, 1157–1167. [Google Scholar] [CrossRef]
- Liang, X.; Huang, Y.; Han, X. Associations between coronary heart disease and risk of cognitive impairment: A meta-analysis. Brain Behav. 2021, 11, e02108. [Google Scholar] [CrossRef]
- Li, J.; Wu, Y.; Zhang, D.; Nie, J. Associations between heart failure and risk of dementia: A PRISMA-compliant meta-analysis. Medicine 2020, 99, e18492. [Google Scholar] [CrossRef]
- University of Essex, Institute for Social and Economic Research. Understanding Society: Waves 1–12, 2009–2021 and Harmonised BHPS: Waves 1–18, 1991–2009. [Data Collection], 17th ed.; UK Data Service, 2022; SN: 6614. [Google Scholar]
- Barr, E.L.; Tonkin, A.M.; Welborn, T.A.; Shaw, J.E. Validity of self-reported cardiovascular disease events in comparison to medical record adjudication and a statewide hospital morbidity database: The AusDiab study. Intern. Med. J. 2009, 39, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Fisher, G.G.; McArdle, J.J.; McCammon, R.J.; Sonnega, A.; Weir, D. New Measures of Fluid Intelligence in the HRS; Institute for Social Research, University of Michigan: Ann Arbor, MI, USA, 2013. [Google Scholar]
- Henry, J.D.; Crawford, J.R.; Phillips, L.H. Verbal fluency performance in dementia of the Alzheimer’s type: A meta-analysis. Neuropsychologia 2004, 42, 1212–1222. [Google Scholar] [CrossRef] [PubMed]
- Rosen, W.G. Verbal fluency in aging and dementia. J. Clin. Exp. Neuropsychol. 1980, 2, 135–146. [Google Scholar] [CrossRef]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [PubMed]
- Escobar, E. Hypertension and coronary heart disease. J. Hum. Hypertens. 2002, 16 (Suppl. S1), S61–S63. [Google Scholar] [CrossRef]
- Naito, R.; Miyauchi, K. Coronary artery disease and type 2 diabetes mellitus. Int. Heart J. 2017, 58, 475–480. [Google Scholar] [CrossRef]
- Santisteban, M.M.; Iadecola, C. Hypertension, dietary salt and cognitive impairment. J. Cereb. Blood Flow Metab. 2018, 38, 2112–2128. [Google Scholar] [CrossRef]
- Yuan, X.Y.; Wang, X.G. Mild cognitive impairment in type 2 diabetes mellitus and related risk factors: A review. Rev. Neurosci. 2017, 28, 715–723. [Google Scholar] [CrossRef]
- Santisteban, M.M.; Iadecola, C.; Carnevale, D. Hypertension, Neurovascular Dysfunction, and Cognitive Impairment. Hypertension 2023, 80, 22–34. [Google Scholar] [CrossRef]
- Wang, Z.T.; Fu, Y.; Zhang, Y.R.; Chen, S.D.; Huang, S.Y.; Yang, L.; Li, H.Q.; Ou, Y.N.; Feng, J.F.; Dong, Q.; et al. Modified dementia risk score as a tool for the prediction of dementia: A prospective cohort study of 239745 participants. Transl. Psychiatry 2022, 12, 509. [Google Scholar] [CrossRef]
- Whitmer, R.A.; Sidney, S.; Selby, J.; Johnston, S.C.; Yaffe, K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 2005, 64, 277–281. [Google Scholar] [CrossRef]
- Bleckwenn, M.; Kleineidam, L.; Wagner, M.; Jessen, F.; Weyerer, S.; Werle, J.; Wiese, B.; Lühmann, D.; Posselt, T.; König, H.-H.; et al. Impact of coronary heart disease on cognitive decline in Alzheimer’s disease: A prospective longitudinal cohort study in primary care. Br. J. Gen. Pract. 2017, 67, e111–e117. [Google Scholar] [CrossRef]
- Michniewicz, E.; Mlodawska, E.; Lopatowska, P.; Tomaszuk-Kazberuk, A.; Malyszko, J. Patients with atrial fibrillation and coronary artery disease-Double trouble. Adv. Med. Sci. 2018, 63, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Zuo, W.; Wu, J. The interaction and pathogenesis between cognitive impairment and common cardiovascular diseases in the elderly. Ther. Adv. Chronic Dis. 2022, 13, 20406223211063020. [Google Scholar] [CrossRef] [PubMed]
- Sepehri Shamloo, A.; Dagres, N.; Müssigbrodt, A.; Stauber, A.; Kircher, S.; Richter, S.; Dinov, B.; Bertagnolli, L.; Husser-Bollmann, D.; Bollmann, A.; et al. Atrial fibrillation and cognitive impairment: New insights and future directions. Heart Lung Circ. 2020, 29, 69–85. [Google Scholar] [CrossRef] [PubMed]
- Greaves, D.; Psaltis, P.J.; Ross, T.J.; Davis, D.; Smith, A.E.; Boord, M.S.; Keage, H.A.D. Cognitive outcomes following coronary artery bypass grafting: A systematic review and meta-analysis of 91,829 patients. Int. J. Cardiol. 2019, 289, 43–49. [Google Scholar] [CrossRef]
- Lecordier, S.; Manrique-Castano, D.; El Moghrabi, Y.; ElAli, A. Neurovascular Alterations in Vascular Dementia: Emphasis on Risk Factors. Front. Aging Neurosci. 2021, 13, 727590. [Google Scholar] [CrossRef]
- Shabir, O.; Berwick, J.; Francis, S.E. Neurovascular dysfunction in vascular dementia, Alzheimer’s and atherosclerosis. BMC Neurosci. 2018, 19, 62. [Google Scholar] [CrossRef]
- Abete, P.; Della-Morte, D.; Gargiulo, G.; Basile, C.; Langellotto, A.; Galizia, G.; Testa, G.; Canonico, V.; Bonaduce, D.; Cacciatore, F. Cognitive impairment and cardiovascular diseases in the elderly. A heart-brain continuum hypothesis. Ageing Res. Rev. 2014, 18, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Corona, A.W.; Fenn, A.M.; Godbout, J.P. Cognitive and behavioral consequences of impaired immunoregulation in aging. J. Neuroimmune Pharmacol. 2012, 7, 7–23. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).