Task-Based and Resting-State Functional MRI in Observing Eloquent Cerebral Areas Personalized for Epilepsy and Surgical Oncology Patients: A Review of the Current Evidence
Abstract
:1. Introduction
2. The BOLD Effect
- Increased local cerebral blood volume (rCBV);
- Increased local cerebral blood flow (rCBF);
- Relative rise in oxyhemoglobin levels in capillaries and venous blood.
3. Techniques for the Acquisition and Processing of BOLD Images
4. Types of fMRI
4.1. Task-Based Methods
4.2. Resting-State Method
5. Clinical Applications
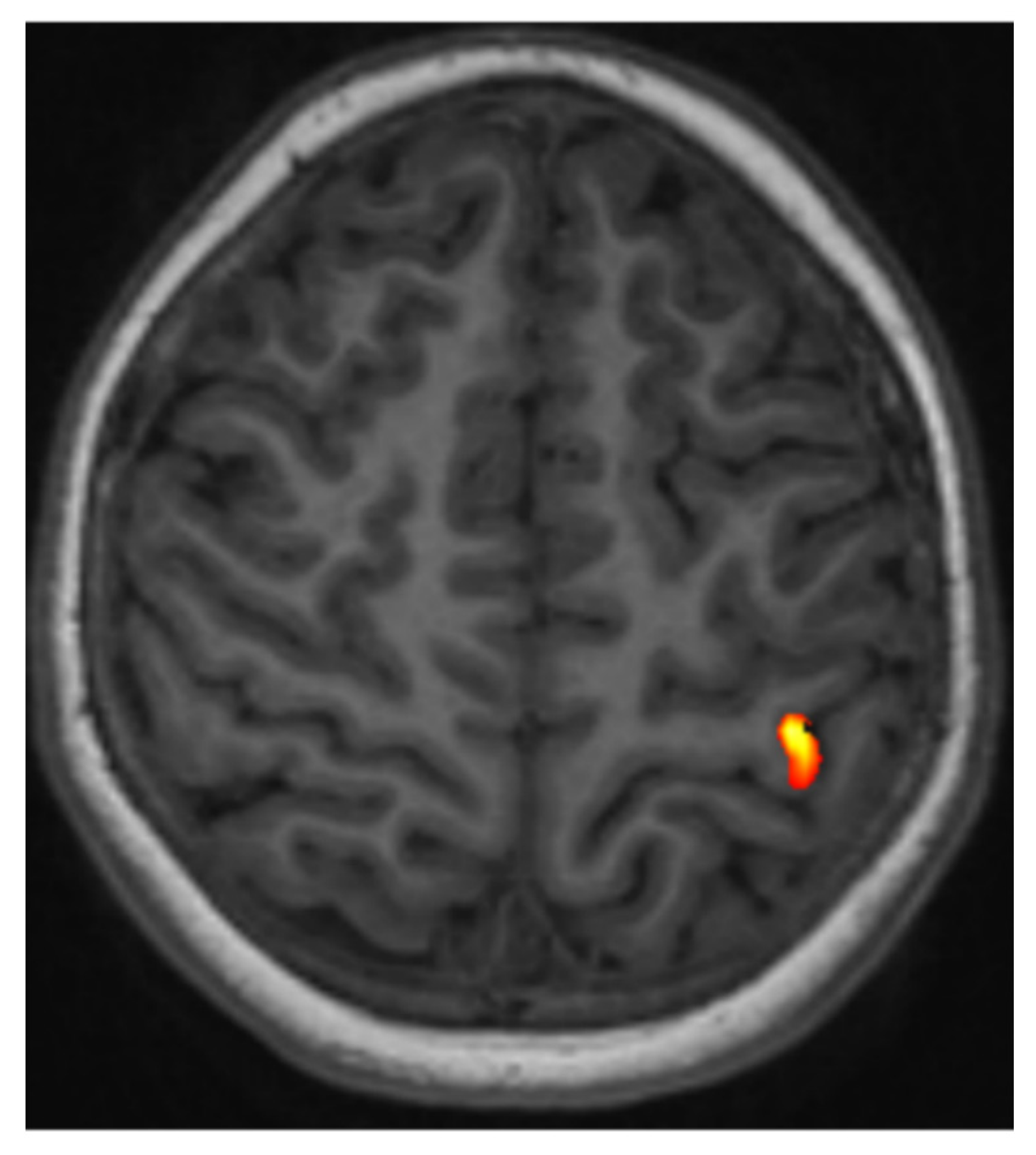
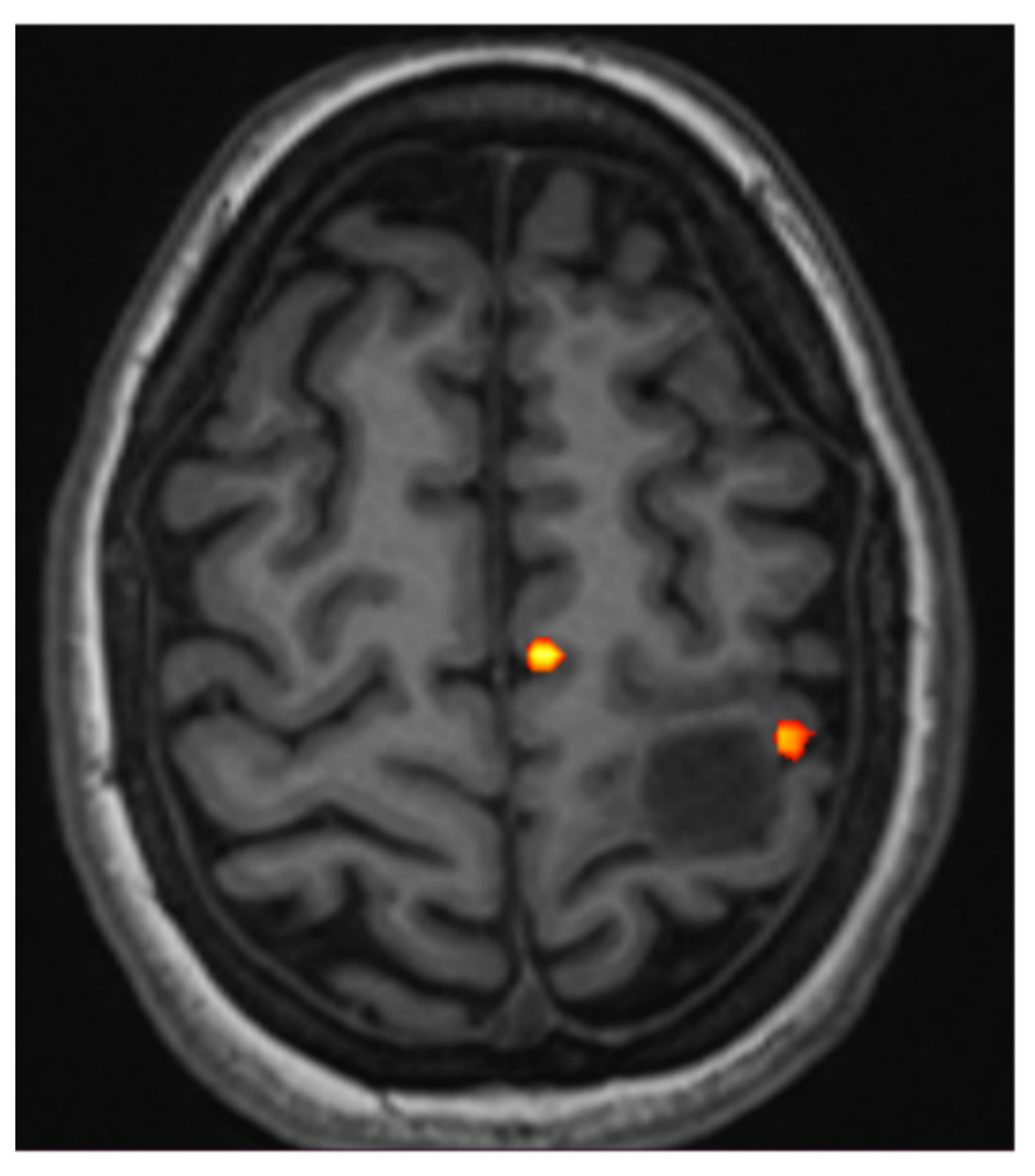
5.1. fMRI of Motor and Somatosensory Functions
- When the anatomy is effaced or partially effaced, and morphological Rolandic landmarks cannot be identified due to tumor growth;
- When a tumor lies in proximity to the identifiable motor hand area.
5.2. fMRI of Language Functions
- Patients with tumor-related linguistic impairments, including right hemisphere tumors, in whom nonstandard organization of relevant cortical representations of the language must be presumed;
- Patients with no language deficit but with left hemisphere tumors that are anatomically near the inferior frontal gyrus (Broca’s area), superior temporal gyrus (Wernicke’s area), the anterior insula (Dronkers’ area), and the supramarginal or angular gyri (Geschwind area);
- Left-handed patients, including those with right hemispheric tumors.
5.3. fMRI of Visual Functions
6. Limitations of Task-Based fMRI
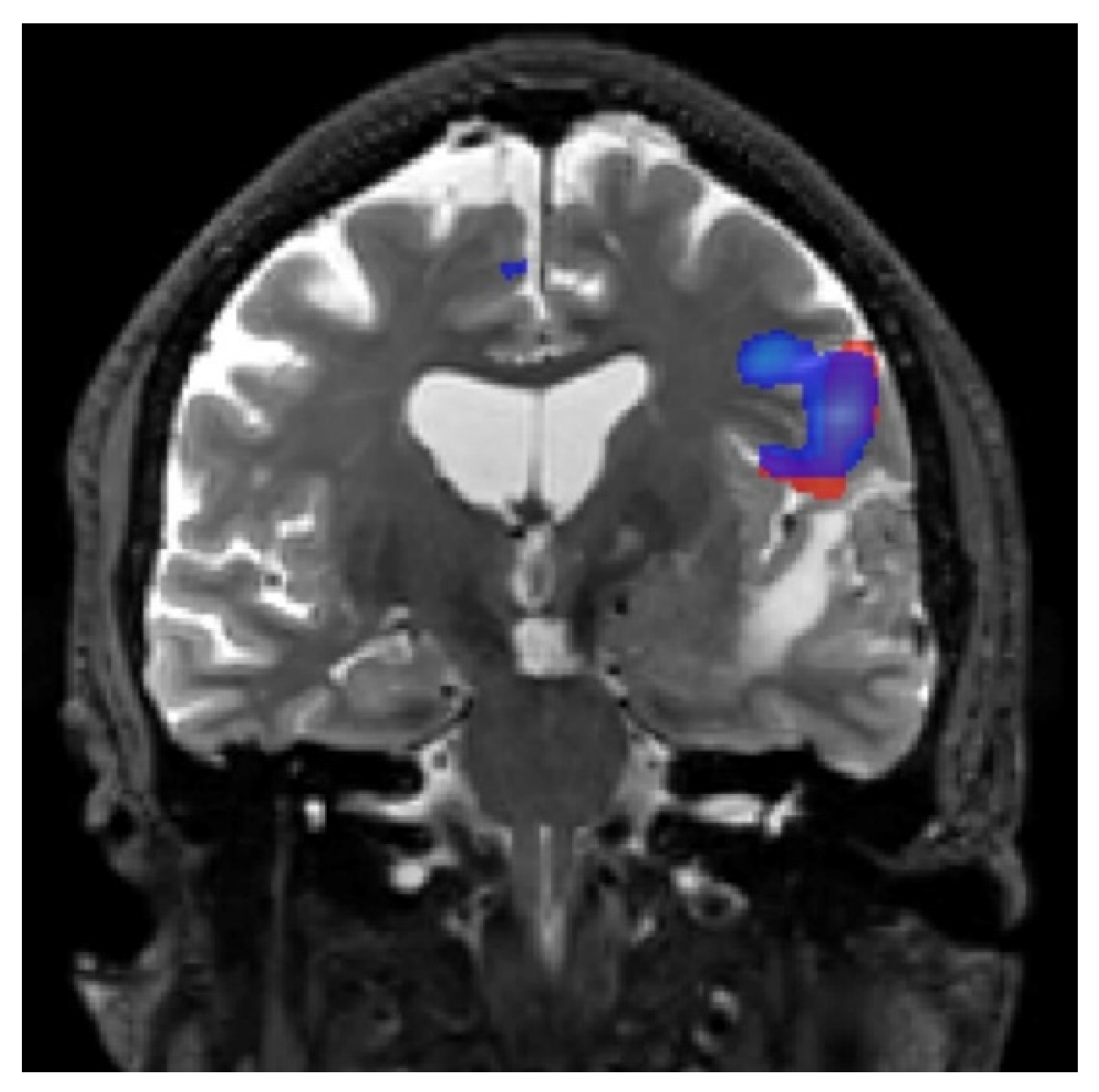
7. Resting-State fMRI Applications
8. Up-to-Date Research Endeavors for Task-Based fMRI in Epilepsy and Oncology Patients
9. Up-to-Date Research Endeavors for Resting-State fMRI in Epilepsy and Oncology Patients
10. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| fMRI | Functional magnetic resonance imaging |
| BOLD | Blood oxygen level-dependent functional magnetic resonance imaging |
| rCBV | Cerebral blood volume |
| rCBF | Cerebral blood flow |
| EPI | Echo-planar-imaging |
| GRE | Gradient echo |
| SE | Spin-echo |
| SNR | Signal-to-noise ratio |
| ROIs | Regions-of-interest |
| DES | Direct electrocortical stimulation |
| SMA | Supplementary motor area |
| FFMap | Functional field map |
References
- Barras, C.D.; Asadi, H.; Baldeweg, T.; Mancini, L.; Yousry, T.A.; Bisdas, S. Functional magnetic resonance imaging in clinical practice: State of the art and science. Aust. Fam. Physician 2016, 45, 798–803. [Google Scholar]
- Shah, L.M.; Anderson, J.S.; Lee, J.N.; Wiggins, I.I.I.R. Functional magnetic resonance imaging. InSeminars Roentgenol. 2010, 45, 147–156. [Google Scholar] [CrossRef]
- Lee, M.H.; Smyser, C.D.; Shimony, J.S. Resting-state fMRI: A review of methods and clinical applications. AJNR Am. J. Neuroradiol. 2013, 34, 1866–1872. [Google Scholar] [CrossRef] [Green Version]
- Stippich, C. Clinical functional MRI. In Presurgical Functional Neuroimaging: Presurgical Functional Neuroimaging; Springer: Berlin/Heidelberg, Germany, 2022. [Google Scholar] [CrossRef]
- Buxton, R.B.; Uludağ, K.; Dubowitz, D.J.; Liu, T.T. Modeling the hemodynamic response to brain activation. Neuroimage 2004, 23, S220–S233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stippich, C.; Heiland, S.; Tronnier, V.; Mohr, A.; Sartor, K. Functional magnetic resonance imaging: Physiological background, technical aspects and prerequisites for clinical use. RoFo Fortschr. Auf Dem Geb. Der Rontgenstrahlen Der Nukl. 2002, 174, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Stippich, C.; Ochmann, H.; Sartor, K. Somatotopic mapping of the human primary sensorimotor cortex during motor imagery and motor execution by functional magnetic resonance imaging. Neurosci. Lett. 2002, 331, 50–54. [Google Scholar] [CrossRef]
- Hulvershorn, J.; Bloy, L.; Gualtieri, E.E.; Leigh, J.S.; Elliott, M.A. Spatial sensitivity and temporal response of spin echo and gradient echo bold contrast at 3 T using peak hemodynamic activation time. Neuroimage 2005, 24, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Hulvershorn, J.; Bloy, L.; Gualtieri, E.E.; Redmann, C.P.; Leigh, J.S.; Elliott, M.A. Temporal resolving power of spin echo and gradient echo fMRI at 3T with apparent diffusion coefficient compartmentalization. Hum. Brain Mapp. 2005, 25, 247–258. [Google Scholar] [CrossRef]
- Filippi, M. fMRI Techniques and Protocols; Filippi, M., Ed.; Humana Press: Milan, Italy, 2016; Volume 830. [Google Scholar]
- Boxerman, J.L.; Bandettini, P.A.; Kwong, K.K.; Baker, J.R.; Davis, T.L.; Rosen, B.R.; Weisskoff, R.M. The intravascular contribution to fMRI signal change: Monte Carlo modeling and diffusion-weighted studies in vivo. Magn. Reson. Med. 1995, 34, 4–10. [Google Scholar] [CrossRef]
- Lindquist, M.A.; Geuter, S.; Wager, T.D.; Caffo, B.S. Modular preprocessing pipelines can reintroduce artifacts into fMRI data. Hum. Brain Mapp. 2019, 40, 2358–2376. [Google Scholar] [CrossRef] [Green Version]
- Chen, N.-K.; Dickey, C.C.; Yoo, S.-S.; Guttmann, C.R.G.; Panych, L.P. Selection of voxel size and slice orientation for fMRI in the presence of susceptibility field gradients: Application to imaging of the amygdala. Neuroimage 2003, 19, 817–825. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.C.; Jack, C.R.; Grimm, R.C.; Rossman, P.J.; Felmlee, J.P.; Ehman, R.L.; Riederer, S.J. Real-time adaptive motion correction in functional MRI. Magn. Reson. Med. 1996, 36, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Dale, A.M.; Buckner, R.L. Selective averaging of rapidly presented individual trials using fMRI. Hum. Brain Mapp. 1997, 5, 329–340. [Google Scholar] [CrossRef]
- Bandettini, P.A. MRI Studies of Brain Activation: Dynamic Characteristics in Functional MRI of the Brain; Society of Magnetic Resonance in Medicine: Berkeley, CA, USA, 1993. [Google Scholar]
- Donaldson, D.I. Parsing brain activity with fMRI and mixed designs: What kind of a state is neuroimaging in? Trends Neurosci. 2004, 27, 442–444. [Google Scholar] [CrossRef]
- Maccotta, L.; Zacks, J.M.; Buckner, R.L. Rapid self-paced event-related functional MRI: Feasibility and implications of stimulus- versus response-locked timing. Neuroimage 2001, 14, 1105–1121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ollinger, J.M.; Shulman, G.L.; Corbetta, M. Separating processes within a trial in event-related functional MRI I. Methods Neuroimage 2001, 13, 210–217. [Google Scholar] [CrossRef]
- Yarkoni, T.; Speer, N.K.; Balota, D.A.; McAvoy, M.P.; Zacks, J.M. Pictures of a thousand words: Investigating the neural mechanisms of reading with extremely rapid event-related fMRI. Neuroimage 2008, 42, 973–987. [Google Scholar] [CrossRef] [Green Version]
- Buckner, R.L.; Bandettini, P.A.; O’Craven, K.M.; Savoy, R.L.; Petersen, S.E.; Raichle, M.E.; Rosen, B.R. Detection of cortical activation during averaged single trials of a cognitive task using functional magnetic resonance imaging. Proc. Natl. Acad. Sci. USA 1996, 93, 14878–14883. [Google Scholar] [CrossRef] [Green Version]
- Taylor, S.F.; Stern, E.R.; Gehring, W.J. Neural systems for error monitoring: Recent findings and theoretical perspectives: Recent findings and theoretical perspectives. Neuroscientist 2007, 13, 160–172. [Google Scholar] [CrossRef]
- Donaldson, D.I.; Petersen, S.E.; Ollinger, J.M.; Buckner, R.L. Dissociating state and item components of recognition memory using fMRI. Neuroimage 2001, 13, 129–142. [Google Scholar] [CrossRef] [Green Version]
- Dosenbach, N.U.; Visscher, K.M.; Palmer, E.D.; Miezin, F.M.; Wenger, K.K.; Kang, H.C.; Burgund, E.D.; Grimes, A.L.; Schlaggar, B.L.; Petersen, S.E. A core system for the implementation of task sets. Neuron 2006, 50, 799–812. [Google Scholar] [CrossRef] [Green Version]
- Fox, M.D.; Snyder, A.Z.; Barch, D.M.; Gusnard, D.A.; Raichle, M.E. Transient BOLD responses at block transitions. Neuroimage 2005, 28, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Konishi, S.; Donaldson, D.I.; Buckner, R.L. Transient activation during block transition. Neuroimage 2001, 13, 364–374. [Google Scholar] [CrossRef] [Green Version]
- Meltzer, J.A.; Negishi, M.; Constable, R.T. Biphasic hemodynamic responses influence deactivation and may mask activation in block-design fMRI paradigms. Hum. Brain Mapp. 2008, 29, 385–399. [Google Scholar] [CrossRef] [Green Version]
- Miezin, F.M.; Maccotta, L.; Ollinger, J.M.; Petersen, S.E.; Buckner, R.L. Characterizing the hemodynamic response: Effects of presentation rate, sampling procedure, and the possibility of ordering brain activity based on relative timing. Neuroimage 2000, 11, 735–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petersen, S.E.; Dubis, J.W. The mixed block/event-related design. Neuroimage 2012, 62, 1177–1184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, S.M. Introduction to Resting State fMRI Functional Connectivity; Oxford University Press: London, UK, 2017. [Google Scholar]
- Biswal, B.; Yetkin, F.Z.; Haughton, V.M.; Hyde, J.S. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn. Reson Med. 1995, 34, 537–541. [Google Scholar] [CrossRef]
- Raichle, M.E.; MacLeod, A.M.; Snyder, A.Z.; Powers, W.J.; Gusnard, D.A.; Shulman, G.L. A default mode of brain function. Proc. Natl. Acad. Sci. USA 2001, 98, 676–682. [Google Scholar] [CrossRef] [Green Version]
- Fox, M.D.; Corbetta, M.; Snyder, A.Z.; Vincent, J.L.; Raichle, M.E. Spontaneous neuronal activity distinguishes human dorsal and ventral attention systems. Proc. Natl. Acad. Sci. USA 2006, 103, 10046–10051. [Google Scholar] [CrossRef] [Green Version]
- Vincent, J.L.; Kahn, I.; Snyder, A.Z.; Raichle, M.E.; Buckner, R.L. Evidence for a frontoparietal control system revealed by intrinsic functional connectivity. J. Neurophysiol. 2008, 100, 3328–3342. [Google Scholar] [CrossRef] [Green Version]
- Voss, J.; Meier, T.B.; Freidel, R.; Kundu, B.; Nair, V.A.; Holdsworth, R.; Kuo, J.S.; Prabhakaran, V. The role of secondary motor and language cortices in morbidity and mortality: A retrospective functional MRI study of surgical planning for patients with intracranial tumors. Neurosurg. Focus 2013, 34, E7. [Google Scholar] [CrossRef] [Green Version]
- Krasnow, B.; Tamm, L.; Greicius, M.; Yang, T.; Glover, G.; Reiss, A.; Menon, V. Comparison of fMRI activation at 3 and 1.5 T during perceptual, cognitive, and affective processing. Neuroimage 2003, 18, 813–826. [Google Scholar] [CrossRef] [PubMed]
- García-Eulate, R.; García-García, D.; Dominguez, P.D.; Noguera, J.J.; De Luis, E.; Rodriguez-Oroz, M.C.; Zubieta, J.L. Functional bold MRI: Advantages of the 3 T vs. the 1.5 T. Clin. Imaging 2011, 35, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Holodny, A.I.; Schulder, M.; Liu, W.C.; Wolko, J.; Maldjian, J.A.; Kalnin, A.J. The effect of brain tumors on BOLD functional MR imaging activation in the adjacent motor cortex: Implications for image-guided neurosurgery. AJNR Am. J. Neuroradiol. 2000, 21, 1415–1422. [Google Scholar] [PubMed]
- Pillai, J.J.; Zacà, D. Comparison of BOLD cerebrovascular reactivity mapping and DSC MR perfusion imaging for prediction of neurovascular uncoupling potential in brain tumors. Technol. Cancer Res. Treat 2012, 11, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Zacà, D.; Jovicich, J.; Nadar, S.R.; Voyvodic, J.T.; Pillai, J.J. Cerebrovascular reactivity mapping in patients with low grade gliomas undergoing presurgical sensorimotor mapping with BOLD fMRI: BOLD CVR mapping in low grade gliomas. J. Magn. Reson Imaging 2014, 40, 383–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baudendistel, K.; Schad, L.R.; Wenz, F.; Essig, M.; Schröder, J.; Jahn, T.; Knopp, M.V.; Lorenz, W.J. Monitoring of task performance during functional magnetic resonance imaging of sensorimotor cortex at 1.5 T. Magn. Reson. Imaging 1996, 14, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Ogg, R.J.; Laningham, F.H.; Clarke, D.; Einhaus, S.; Zou, P.; Tobias, M.E.; Boop, F.A. Passive range of motion functional magnetic resonance imaging localizing sensorimotor cortex in sedated children: Clinical article. J. Neurosurg. Pediatr. 2009, 4, 317–322. [Google Scholar] [CrossRef]
- Lee, C.C.; Jack, C.R., Jr.; Riederer, S.J. Mapping of the central sulcus with functional MR: Active versus passive activation tasks. AJNR Am. J. Neuroradiol. 1998, 19, 847–852. [Google Scholar] [PubMed]
- Roland, P.E. Brain activation. In Motor Functions; Language; Wiley: New York, NY, USA, 1999; pp. 269–290. [Google Scholar]
- Cunnington, R.; Windischberger, C.; Deecke, L.; Moser, E. The preparation and execution of self-initiated and externally-triggered movement: A study of event-related fMRI. Neuroimage 2002, 15, 373–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, C.C.; Ward, H.A.; Sharbrough, F.W.; Meyer, F.B.; Marsh, W.R.; Raffel, C.; So, E.L.; Cascino, G.D.; Shin, C.; Xu, Y.; et al. Assessment of functional MR imaging in neurosurgical planning. AJNR Am. J. Neuroradiol. 1999, 20, 1511–1519. [Google Scholar]
- Bizzi, A.; Blasi, V.; Falini, A.; Ferroli, P.; Cadioli, M.; Danesi, U.; Aquino, D.; Marras, C.; Caldiroli, D.; Broggi, G. Presurgical functional MR imaging of language and motor functions: Validation with intraoperative electrocortical mapping. Radiology 2008, 248, 579–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartos, R.; Jech, R.; Vymazal, J.; Petrovický, P.; Vachata, P.; Hejčl, A.; Zolal, A.; Sames, M. Validity of primary motor area localization with fMRI versus electric cortical stimulation: A comparative study. Acta Neurochir. 2009, 151, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- Meier, M.P.; Ilmberger, J.; Fesl, G.; Ruge, M.I. Validation of functional motor and language MRI with direct cortical stimulation. Acta Neurochir. 2013, 155, 675–683. [Google Scholar] [CrossRef]
- Håberg, A.; Kvistad, K.A.; Unsgård, G.; Haraldseth, O. Preoperative blood oxygen level-dependent functional magnetic resonance imaging in patients with primary brain tumors: Clinical application and outcome. Neurosurgery 2004, 54, 902–914; discussion 914–915. [Google Scholar] [CrossRef]
- Krishnan, R.; Raabe, A.; Hattingen, E.; Szelényi, A.; Yahya, H.; Hermann, E.; Zimmermann, M.; Seifert, V. Functional magnetic resonance imaging-integrated neuronavigation: Correlation between lesion-to-motor cortex distance and outcome. Neurosurgery 2004, 55, 904–914; discussion 914–915. [Google Scholar] [CrossRef] [PubMed]
- Lehéricy, S.; Duffau, H.; Cornu, P.; Capelle, L.; Pidoux, B.; Carpentier, A.; Auliac, S.; Clemenceau, S.; Sichez, J.-P.; Bitar, A.; et al. Correspondence between functional magnetic resonance imaging somatotopy and individual brain anatomy of the central region: Comparison with intraoperative stimulation in patients with brain tumors. J. Neurosurg. 2000, 92, 589–598. [Google Scholar] [CrossRef] [Green Version]
- Stippich, C.; Hofmann, R.; Kapfer, D.; Hempel, E.; Heiland, S.; Jansen, O.; Sartor, K. Somatotopic mapping of the human primary somatosensory cortex by fully automated tactile stimulation using functional magnetic resonance imaging. Neurosci. Lett. 1999, 277, 25–28. [Google Scholar] [CrossRef]
- Stippich, C.; Romanowski, A.; Nennig, E.; Kress, B.; Sartor, K. Time-efficient localization of the human secondary somatosensory cortex by functional magnetic resonance imaging. Neurosci. Lett. 2005, 381, 264–268. [Google Scholar] [CrossRef]
- Deblaere, K.; Backes, W.; Hofman, P.; Vandemaele, P.; Vonck, K.; Boon, P.; Troost, J.; Vermeulen, J.; Wilmink, J.; Achten, E.; et al. Developing a comprehensive presurgical functional MRI protocol for patients with intractable temporal lobe epilepsy: A pilot study. Neuroradiology 2002, 44, 667–673. [Google Scholar] [CrossRef]
- Ojemann, G.A.; Ojemann, J.; Ramsey, N.F. Relation between functional magnetic resonance imaging (fMRI) and single neuron, local field potential (LFP) and electrocorticography (ECoG) activity in human cortex. Front. Hum. Neurosci. 2013, 7, 34. [Google Scholar] [CrossRef] [Green Version]
- Binder, J.R.; Frost, J.A.; Hammeke, T.A.; Cox, R.W.; Rao, S.M.; Prieto, T. Human brain language areas identified by functional magnetic resonance imaging. J. Neurosci. 1997, 17, 353–362. [Google Scholar] [CrossRef] [Green Version]
- Black, D.; Vachha, B.; Mian, A.; Faro, S.; Maheshwari, M.; Sair, H.; Petrella, J.; Pillai, J.; Welker, K. American society of functional neuroradiology–recommended fMRI paradigm algorithms for presurgical language assessment. AJNR Am. J. Neuroradiol. 2017, 38, E65–E73. [Google Scholar] [CrossRef] [Green Version]
- Bargalló, N.; Cano-López, I.; Rosazza, C.; Vernooij, M.W.; Smits, M.; Vitali, P.; Alvarez-Linera, J.; Urbach, H.; Mancini, L.; Ramos, A.; et al. Clinical practice of language fMRI in epilepsy centers: A European survey and conclusions by the ESNR Epilepsy Working Group. Neuroradiology 2020, 62, 549–562. [Google Scholar] [CrossRef] [Green Version]
- Zacà, D.; Jarso, S.; Pillai, J.J. Role of semantic paradigms for optimization of language mapping in clinical FMRI studies. AJNR Am. J. Neuroradiol. 2013, 34, 1966–1971. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morris, G.L., 3rd; Mueller, W.M.; Yetkin, F.Z.; Haughton, V.M.; Hammeke, T.A.; Swanson, S.; Rao, S.M.; Jesmanowicz, A.; Estkowski, L.D.; Bandettini, P.A.; et al. Functional magnetic resonance imaging in partial epilepsy. Epilepsia 1994, 35, 1194–1198. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, C.F.A.; Dhingra, I.; Li, A.X.; Blumenfeld, H.; Alkawadri, R.; Bickel, S.; Helmstaedter, C.; Meletti, S.; Bronen, R.A.; Warfield, S.K.; et al. Presurgical language fMRI: Technical practices in epilepsy surgical planning. Hum. Brain Mapp. 2018, 39, 4032–4042. [Google Scholar] [CrossRef] [Green Version]
- Hamberger, M.J.; Cole, J. Language organization and reorganization in epilepsy. Neuropsychol. Rev. 2011, 21, 240–251. [Google Scholar] [CrossRef]
- Sharan, A.; Ooi, Y.C.; Langfitt, J.; Sperling, M.R. Intracarotid amobarbital procedure for epilepsy surgery. Epilepsy. Behav. 2011, 20, 209–213. [Google Scholar] [CrossRef]
- Spreer, J.; Quiske, A.; Altenmüller, D.M.; Arnold, S.; Schulze-Bonhage, A.; Steinhoff, B.J.; Schumacher, M. Unsuspected atypical hemispheric dominance for language as determined by fMRI. Epilepsia 2011, 42, 957–959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hertz-Pannier, L.; Gaillard, W.D.; Mott, S.H.; Cuenod, C.A.; Bookheimer, S.Y.; Weinstein, S.; Conry, J.; Papero, P.H.; Schiff, S.J.; Bihan, D.L.; et al. Noninvasive assessment of language dominance in children and adolescents with functional MRI: A preliminary study. Neurology 1997, 48, 1003–1012. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, S.R.; Kiriakopoulos, E.; Mikulis, D.; Drake, J.M.; Hoffman, H.J.; Humphreys, R.; Hwang, P.; Otsubo, H.; Holowka, S.; Logan, W.; et al. Combined utility of functional MRI, cortical mapping, and frameless stereotaxy in the resection of lesions in eloquent areas of brain in children. Pediatr. Neurosurg. 1997, 26, 68–82. [Google Scholar] [CrossRef]
- Logan, W.J. Functional magnetic resonance imaging in children. Semin Pediatr. Neurol. 1999, 6, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Gaillard, W.D.; Hertz-Pannier, L.; Mott, S.H.; Barnett, A.S.; LeBihan, D.; Theodore, W.H. Functional anatomy of cognitive development: fMRI of verbal fluency in children and adults. Neurology 2000, 54, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Rausch, R.; Silfvenious, H. Intra-arterial amobarbital procedures. In Surgical Treatment of the Epilepsies; Engel, J.J., Ed.; Raven Press: New York, NY, USA, 1993; pp. 341–357. [Google Scholar]
- Binder, J.; Swanson, S.J.; Hammeke, T.A.; Morris, G.L.; Mueller, W.M.; Fischer, M.; Benbadis, S.; Frost, J.; Rao, S.; Haughton, V.M. Determination of language dominance using functional MRI: A comparison with the Wada test. Neurology 1996, 46, 978–984. [Google Scholar] [CrossRef]
- Bahn, M.M.; Lin, W.; Silbergeld, D.L.; Miller, J.W.; Kuppusamy, K.; Cook, R.J.; Hammer, G.; Wetzel, R.; Cross, D. Localization of language cortices by functional MR imaging compared with intracarotid amobarbital hemispheric sedation. AJR Am. J. Roentgenol. 1997, 169, 575–579. [Google Scholar] [CrossRef]
- Lehericy, S.; Cohen, L.; Bazin, B.; Samson, S.; Giacomini, E.; Rougetet, R.; Hertz-Pannier, L.; Le Bihan, D.; Marsault, C.; Baulac, M. Functional MR evaluation of temporal and frontal language dominance compared with the Wada test. Neurology 2000, 54, 1625–1633. [Google Scholar] [CrossRef]
- Dym, R.J.; Burns, J.; Freeman, K.; Lipton, M.L. Is functional MR imaging assessment of hemispheric language dominance as good as the Wada test?: A meta-analysis. Radiology 2011, 261, 446–455. [Google Scholar] [CrossRef] [Green Version]
- Hirsch, J.; Ruge, M.I.; Kim, K.H.; Correa, D.D.; Victor, J.D.; Relkin, N.R.; Labar, D.R.; Krol, G.; Bilsky, M.H.; Souweidane, M.M.; et al. An integrated functional magnetic resonance imaging procedure for preoperative mapping of cortical areas associated with tactile, motor, language, and visual functions. Neurosurgery 2000, 47, 711–722. [Google Scholar]
- Giussani, C.; Roux, F.-E.; Ojemann, J.; Sganzerla, E.P.; Pirillo, D.; Papagno, C. Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies. Neurosurgery 2010, 66, 113–120. [Google Scholar] [CrossRef]
- Kuchcinski, G.; Mellerio, C.; Pallud, J.; Dezamis, E.; Turc, G.; Rigaux-Viode, O.; Malherbe, C.; Roca, P.; Leclerc, X.; Varlet, P.; et al. Three-tesla functional MR language mapping: Comparison with direct cortical stimulation in gliomas. Neurology 2015, 84, 560–568. [Google Scholar] [CrossRef]
- Morrison, M.A.; Tam, F.; Garavaglia, M.M.; Hare, G.M.T.; Cusimano, M.D.; Schweizer, T.A.; Das, S.; Graham, S.J. Sources of variation influencing concordance between functional MRI and direct cortical stimulation in brain tumor surgery. Front. Neurosci. 2016, 10, 461. [Google Scholar] [CrossRef] [Green Version]
- Castellano, A.; Cirillo, S.; Bello, L.; Riva, M.; Falini, A. Functional MRI for surgery of gliomas. Curr. Treat Options Neurol. 2017, 19, 34. [Google Scholar] [CrossRef] [PubMed]
- DeYoe, E.A.; Raut, R.V. Visual mapping using blood oxygen level dependent functional magnetic resonance imaging. Neuroimaging Clin. N Am. 2014, 24, 573–584. [Google Scholar] [CrossRef] [Green Version]
- Kapsalakis, I.Z.; Kapsalaki, E.Z.; Gotsis, E.D.; Verganelakis, D.; Toulas, P.; Hadjigeorgiou, G.; Chung, I.; Fezoulidis, I.; Papadimitriou, A.; Robinson, J.S.; et al. Preoperative evaluation with FMRI of patients with intracranial gliomas. Radiol Res Pract. 2012, 2012, 727810. [Google Scholar] [CrossRef] [PubMed]
- Patten, M.L.; Welchman, A.E. fMRI activity in posterior parietal cortex relates to the perceptual use of binocular disparity for both signal-in-noise and feature difference tasks. PLoS ONE 2015, 10, e0140696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopes-Ferreira, D.; Neves, H.; Queiros, A.; Faria-Ribeiro, M.; Peixoto-de-Matos, S.C.; González-Méijome, J.M. Ocular dominance and visual function testing. Biomed Res. Int. 2013, 2013, 238943. [Google Scholar] [CrossRef] [Green Version]
- Omisade, A.; O’Grady, C.B.; Schmidt, M.H.; Fisk, J.D. Visual and auditory fMRI paradigms for presurgical language mapping: Convergent validity and relationship to individual variables. Neurol. Res. Int. 2019, 2019, 6728120. [Google Scholar] [CrossRef]
- Shimony, J.S.; Zhang, D.; Johnston, J.M.; Fox, M.D.; Roy, A.; Leuthardt, E.C. Resting-state spontaneous fluctuations in brain activity: A new paradigm for presurgical planning using fMRI. Acad. Radiol. 2009, 16, 578–583. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Buckner, R.L.; Talukdar, T.; Tanaka, N.; Madsen, J.R.; Stufflebeam, S.M. Task-free presurgical mapping using functional magnetic resonance imaging intrinsic activity: Laboratory investigation. J. Neurosurg. 2009, 111, 746–754. [Google Scholar] [CrossRef] [Green Version]
- Kokkonen, S.-M.; Nikkinen, J.; Remes, J.; Kantola, J.; Starck, T.; Haapea, M.; Tuominen, J.; Tervonen, O.; Kiviniemi, V. Preoperative localization of the sensorimotor area using independent component analysis of resting-state fMRI. Magn. Reson. Imaging 2009, 27, 733–740. [Google Scholar] [CrossRef]
- Zhang, Z.; Liao, W.; Zuo, X.-N.; Wang, Z.; Yuan, C.; Jiao, Q.; Chen, H.; Biswal, B.B.; Lu, G.; Liu, Y. Resting-state brain organization revealed by functional covariance networks. PLoS ONE 2011, 6, e28817. [Google Scholar] [CrossRef]
- Zhang, D.; Snyder, A.Z.; Fox, M.D.; Sansbury, M.W.; Shimony, J.S.; Raichle, M.E. Intrinsic functional relations between human cerebral cortex and thalamus. J. Neurophysiol. 2008, 100, 1740–1748. [Google Scholar] [CrossRef] [Green Version]
- Sanai, N.; Mirzadeh, Z.; Berger, M.S. Functional outcome after language mapping for glioma resection. N. Engl. J. Med. 2008, 358, 18–27. [Google Scholar] [CrossRef]
- Lowe, M.J.; Mock, B.J.; Sorenson, J.A. Functional connectivity in single and multislice echoplanar imaging using resting-state fluctuations. Neuroimage 1998, 7, 119–132. [Google Scholar] [CrossRef]
- Cordes, D.; Haughton, V.M.; Arfanakis, K.; Wendt, G.J.; Turski, P.A.; Moritz, C.H.; Quigley, M.A.; Meyerand, M.E. Mapping functionally related regions of brain with functional connectivity MR imaging. AJNR Am. J. Neuroradiol. 2000, 21, 1636–1644. [Google Scholar] [PubMed]
- van de Ven, V.G.; Formisano, E.; Prvulovic, D.; Roeder, C.H.; Linden, D.E.J. Functional connectivity as revealed by spatial independent component analysis of fMRI measurements during rest. Hum. Brain Mapp. 2004, 22, 165–178. [Google Scholar] [CrossRef]
- Ott, C.; Rosengarth, K.; Doenitz, C.; Hoehne, J.; Wendl, C.; Dodoo-Schittko, F.; Lang, E.; Schmidt, N.O.; Goldhacker, M. Preoperative assessment of Language Dominance through Combined Resting-State and Task-Based functional magnetic resonance imaging. J. Pers. Med. 2021, 11, 1342. [Google Scholar] [CrossRef] [PubMed]
- Massot-Tarrús, A.; White, K.P.; Mousavi, S.R.; Hayman-Abello, S.; Hayman-Abello, B.; Mirsattari, S.M. Concordance between fMRI and Wada test for memory lateralization in temporal lobe epilepsy: A meta-analysis and systematic review. Epilepsy Behav. 2020, 107, 107065. [Google Scholar] [CrossRef] [PubMed]
- Bohm, P.; McKay, J.; Lucas, J.; Sabsevitz, D.; Feyissa, A.M.; Ritaccio, T.; Grewal, S.S.; Wharen, R.E.; Gupta, V.; Tatum, W.O. Wada testing and fMRI in a polyglot evaluated for epilepsy surgery. Epileptic Disord. 2020, 22, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Meinhold, T.; Hofer, W.; Pieper, T.; Kudernatsch, M.; Staudt, M. Presurgical language fMRI in children, adolescents and young adults. Clin. Neuroradiol. 2020, 30, 691–704. [Google Scholar] [CrossRef]
- Agarwal, S.; Sair, H.I.; Pillai, J.J. The problem of neurovascular uncoupling. Neuroimaging Clin. 2021, 31, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Vakamudi, K.; Posse, S.; Jung, R.; Cushnyr, B.; Chohan, M.O. Real-time presurgical resting-state fMRI in patients with brain tumors: Quality control and comparison with task-fMRI and intraoperative mapping. Hum. Brain Mapp. 2020, 41, 797–814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azad, T.D.; Duffau, H. Limitations of functional neuroimaging for patient selection and surgical planning in glioma surgery. Neurosurg. Focus 2020, 48, E12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thakkar, I.; Arraño-Carrasco, L.; Cortes-Rivera, B.; Zunino-Pesce, R.; Mery-Muñoz, F.; Rodriguez-Fernández, M.; Smits, M.; Mendez-Orellana, C. Alternative language paradigms for functional magnetic resonance imaging as presurgical tools for inducing crossed cerebro-cerebellar language activations in brain tumor patients. Eur. Radiol. 2022, 32, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Luckett, P.; Lee, J.J.; Park, K.Y.; Dierker, D.; Daniel, A.G.S.; Seitzman, B.A.; Hacker, C.D.; Ances, B.M.; Leuthardt, E.C.; Snyder, A.Z.; et al. Mapping of the language network with deep learning. Front. Neurol. 2020, 11, 819. [Google Scholar] [CrossRef]
- Rebsamen, M.; Rummel, C.; Reyes, M.; Wiest, R.; McKinley, R. Direct cortical thickness estimation using deep learning-based anatomy segmentation and cortex parcellation. Hum. Brain Mapp. 2020, 41, 4804–4814. [Google Scholar] [CrossRef]
- Rim, B.; Sung, N.-J.; Min, S.; Hong, M. Deep learning in physiological signal data: A survey. Sensors 2020, 20, 969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crunelli, V.; Lőrincz, M.L.; McCafferty, C.; Lambert, R.C.; LeResche, N.; Di Giovanni, G.; David, F. Clinical and experimental insight into pathophysiology, comorbidity and therapy of absence seizures. Brain 2020, 143, 2341–2368. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, M.-P.; Tran, T.X.; Pompili, D.; Elisevich, K.; Soltanian-Zadeh, H. Multimodal data analysis of epileptic EEG and rs-fMRI via deep learning and edge computing. Artif. Intell. Med. 2020, 104, 101813. [Google Scholar] [CrossRef]
- Cui, W.; Wang, Y.; Ren, J.; Hubbard, C.S.; Fu, X.; Fang, S.; Wang, D.; Zhang, H.; Li, Y.; Li, L.; et al. Personalized fMRI delineates functional regions preserved within brain tumors. Ann. Neurol. 2022, 91, 353–366. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Van Dyk, K.; Cho, N.; Raymond, C.; Choi, J.; Salamon, N.; Pope, W.B.; Lai, A.; Cloughesy, T.F.; Nghiemphuet, P.L.; et al. Characterization of cognitive function in survivors of diffuse gliomas using resting-state functional MRI (rs-fMRI). Brain Imaging Behav. 2022, 16, 239–251. [Google Scholar] [CrossRef] [PubMed]
- Sighinolfi, G.; Mitolo, M.; Testa, C.; Martinoni, M.; Evangelisti, S.; Rochat, M.J.; Zoli, M.; Mazzatenta, D.; Lodi, R.; Tonon, C. What Can Resting-State fMRI Data Analysis Explain about the Functional Brain Connectivity in Glioma Patients? Tomography 2022, 8, 267–280. [Google Scholar] [CrossRef] [PubMed]
- Parkes, L.; Satterthwaite, T.D.; Bassett, D.S. Towards precise resting-state fMRI biomarkers in psychiatry: Synthesizing developments in transdiagnostic research, dimensional models of psychopathology, and normative neurodevelopment. Curr. Opin. Neurobiol. 2020, 65, 120–128. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Arfaj, H.K.; Al-Sharydah, A.M.; AlSuhaibani, S.S.; Alaqeel, S.; Yousry, T. Task-Based and Resting-State Functional MRI in Observing Eloquent Cerebral Areas Personalized for Epilepsy and Surgical Oncology Patients: A Review of the Current Evidence. J. Pers. Med. 2023, 13, 370. https://doi.org/10.3390/jpm13020370
Al-Arfaj HK, Al-Sharydah AM, AlSuhaibani SS, Alaqeel S, Yousry T. Task-Based and Resting-State Functional MRI in Observing Eloquent Cerebral Areas Personalized for Epilepsy and Surgical Oncology Patients: A Review of the Current Evidence. Journal of Personalized Medicine. 2023; 13(2):370. https://doi.org/10.3390/jpm13020370
Chicago/Turabian StyleAl-Arfaj, Hussain Khalid, Abdulaziz Mohammad Al-Sharydah, Sari Saleh AlSuhaibani, Soliman Alaqeel, and Tarek Yousry. 2023. "Task-Based and Resting-State Functional MRI in Observing Eloquent Cerebral Areas Personalized for Epilepsy and Surgical Oncology Patients: A Review of the Current Evidence" Journal of Personalized Medicine 13, no. 2: 370. https://doi.org/10.3390/jpm13020370
APA StyleAl-Arfaj, H. K., Al-Sharydah, A. M., AlSuhaibani, S. S., Alaqeel, S., & Yousry, T. (2023). Task-Based and Resting-State Functional MRI in Observing Eloquent Cerebral Areas Personalized for Epilepsy and Surgical Oncology Patients: A Review of the Current Evidence. Journal of Personalized Medicine, 13(2), 370. https://doi.org/10.3390/jpm13020370






