Enhanced Recovery after Surgery Rehabilitation Protocol in the Perioperative Period of Orthopedics: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Literature Search
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
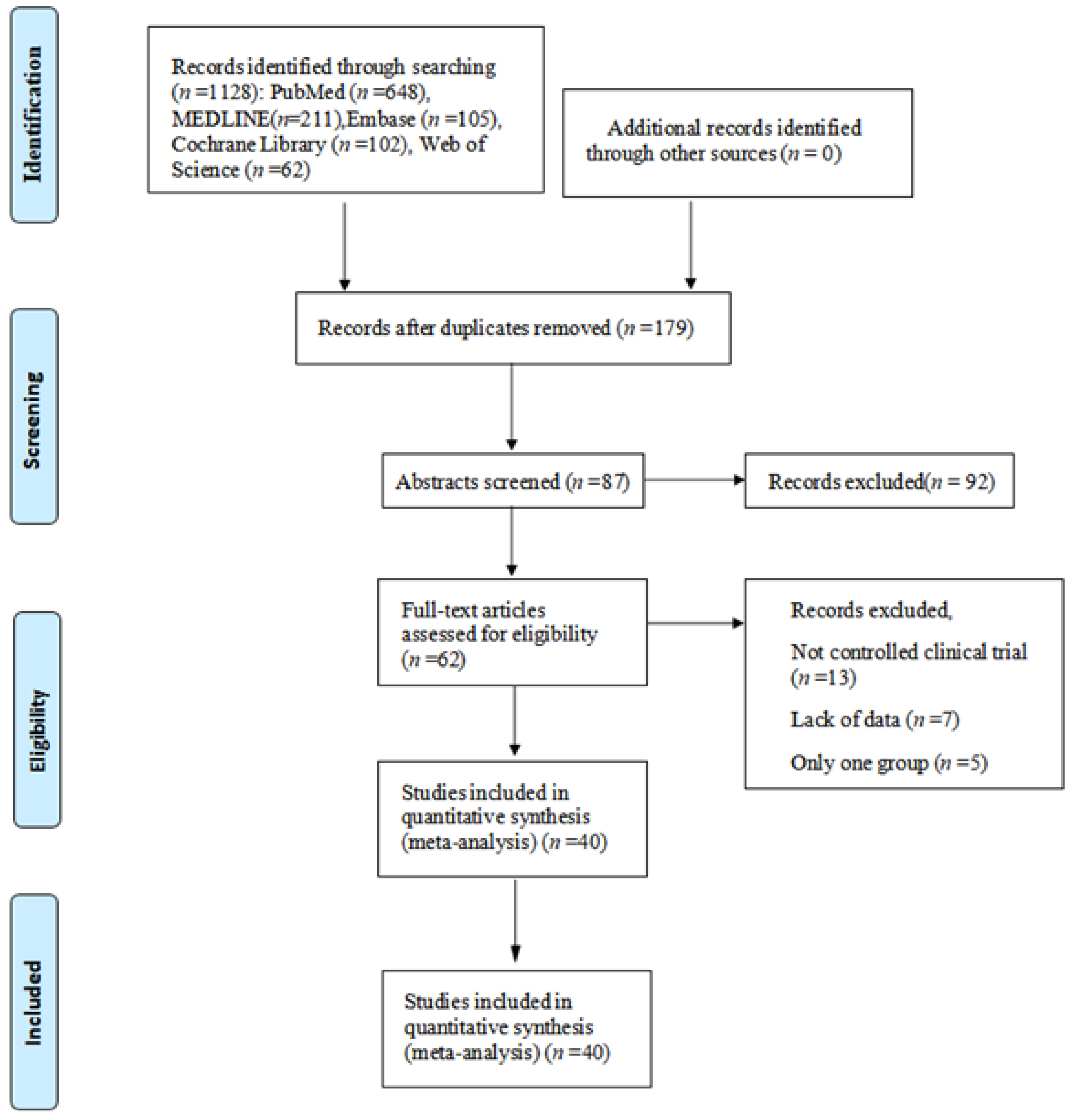
3.1. Identification of Included Studies
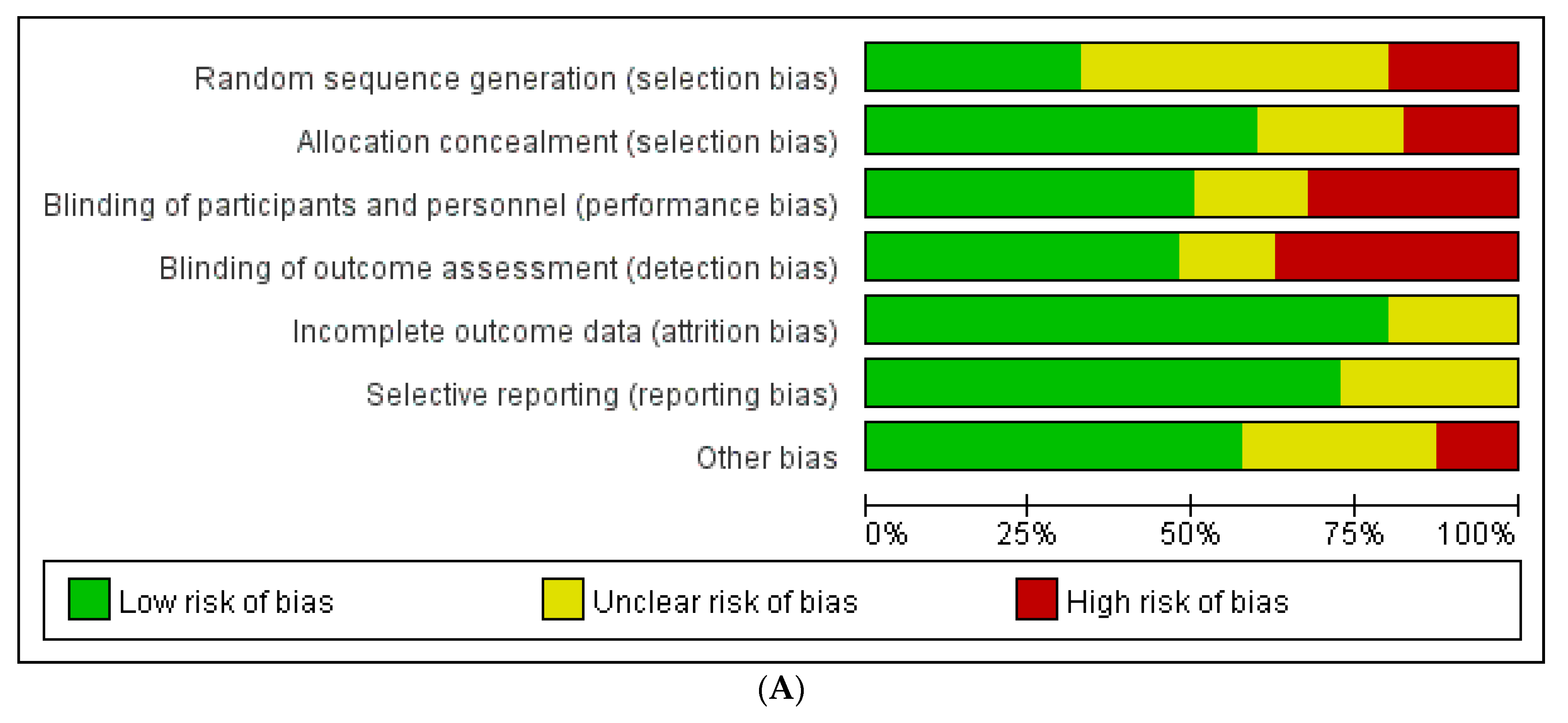
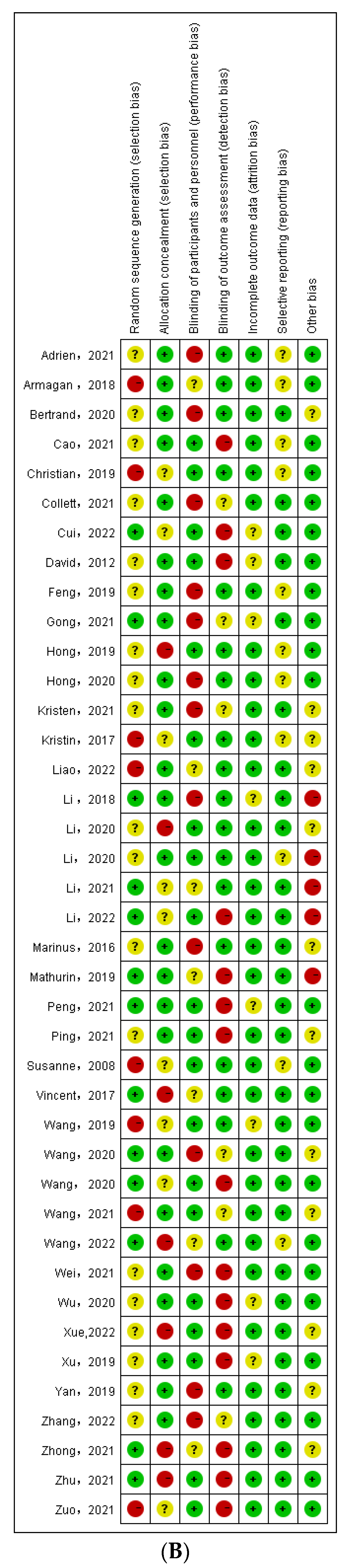
3.2. Quality Assessment of Included Studies
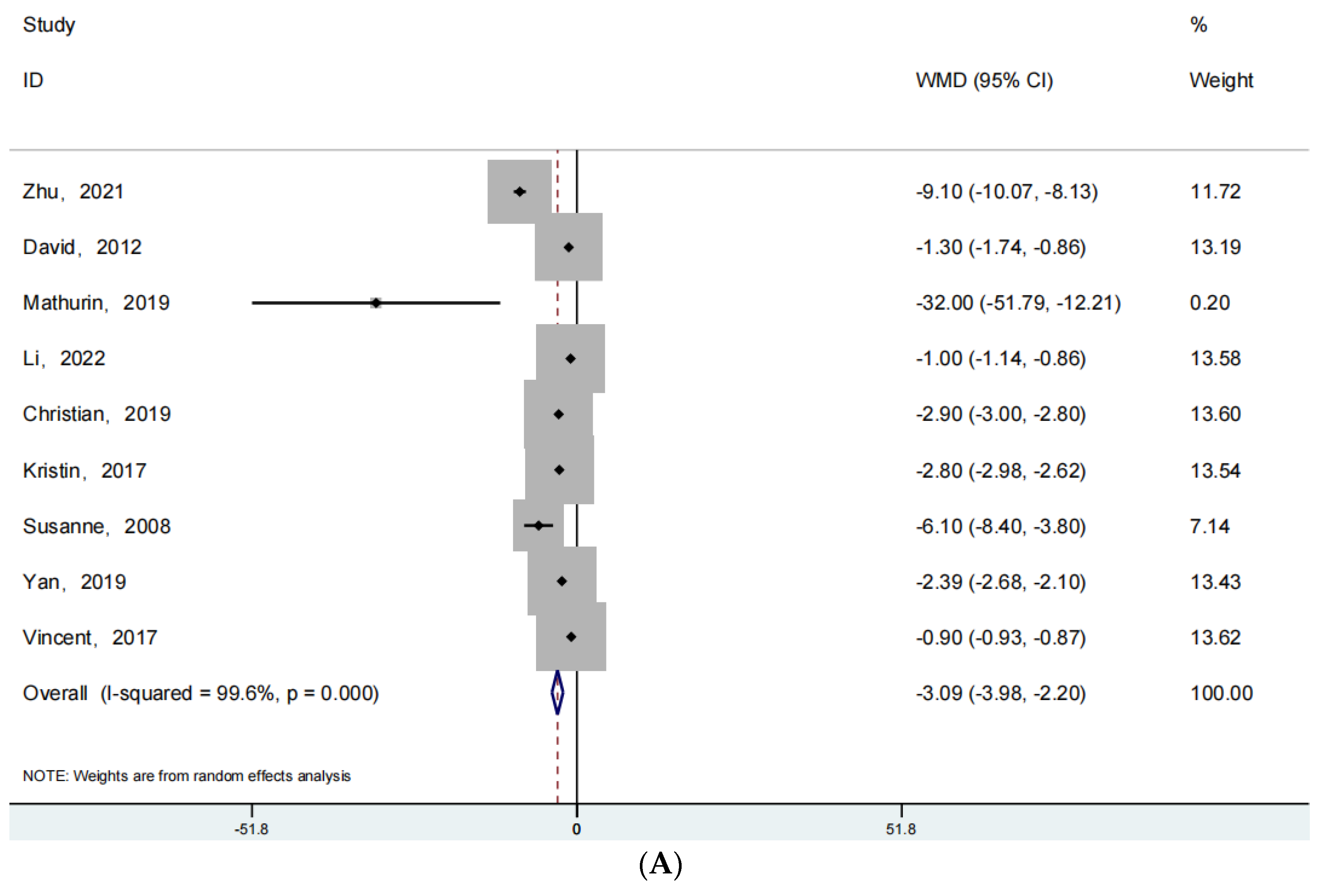
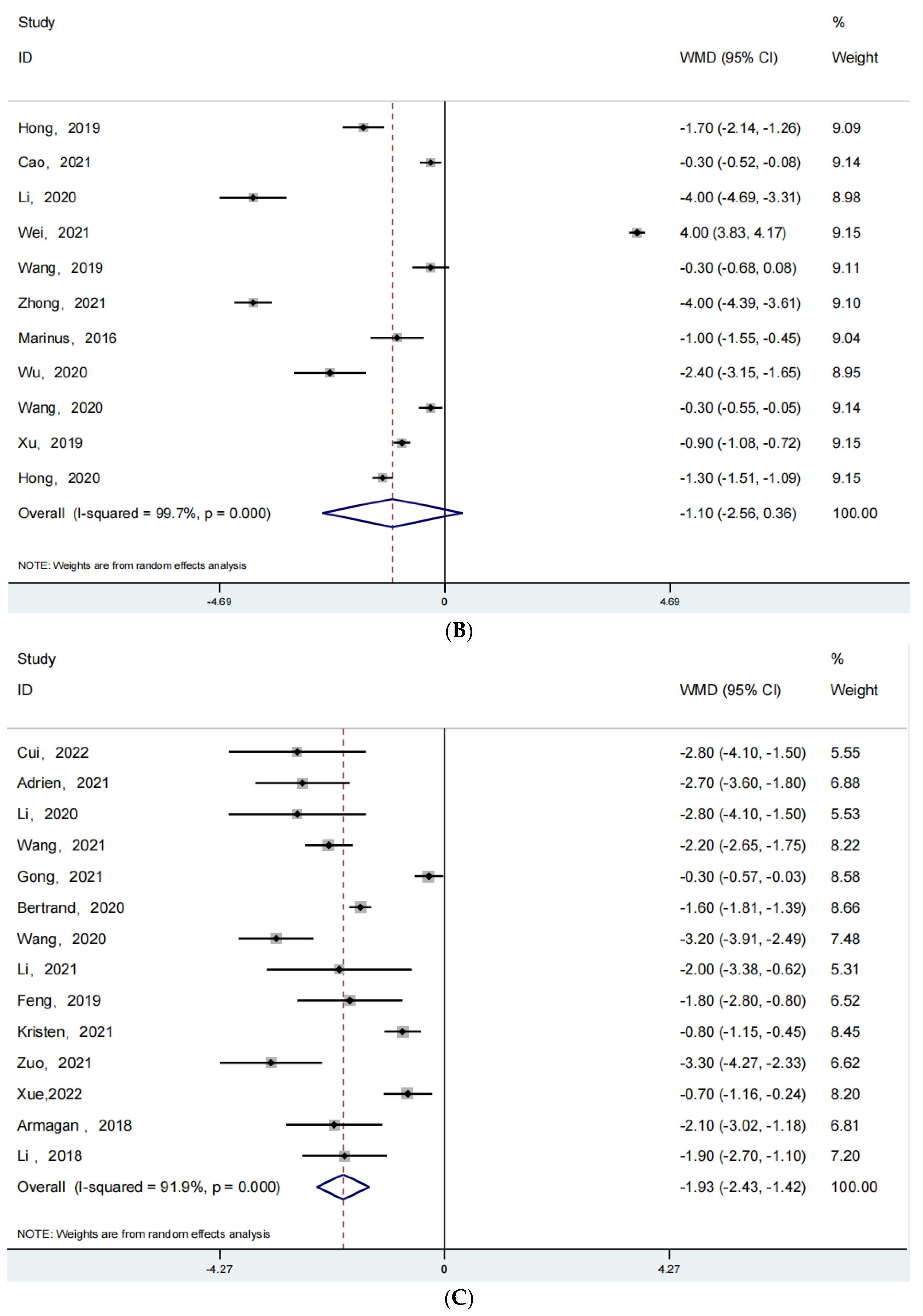
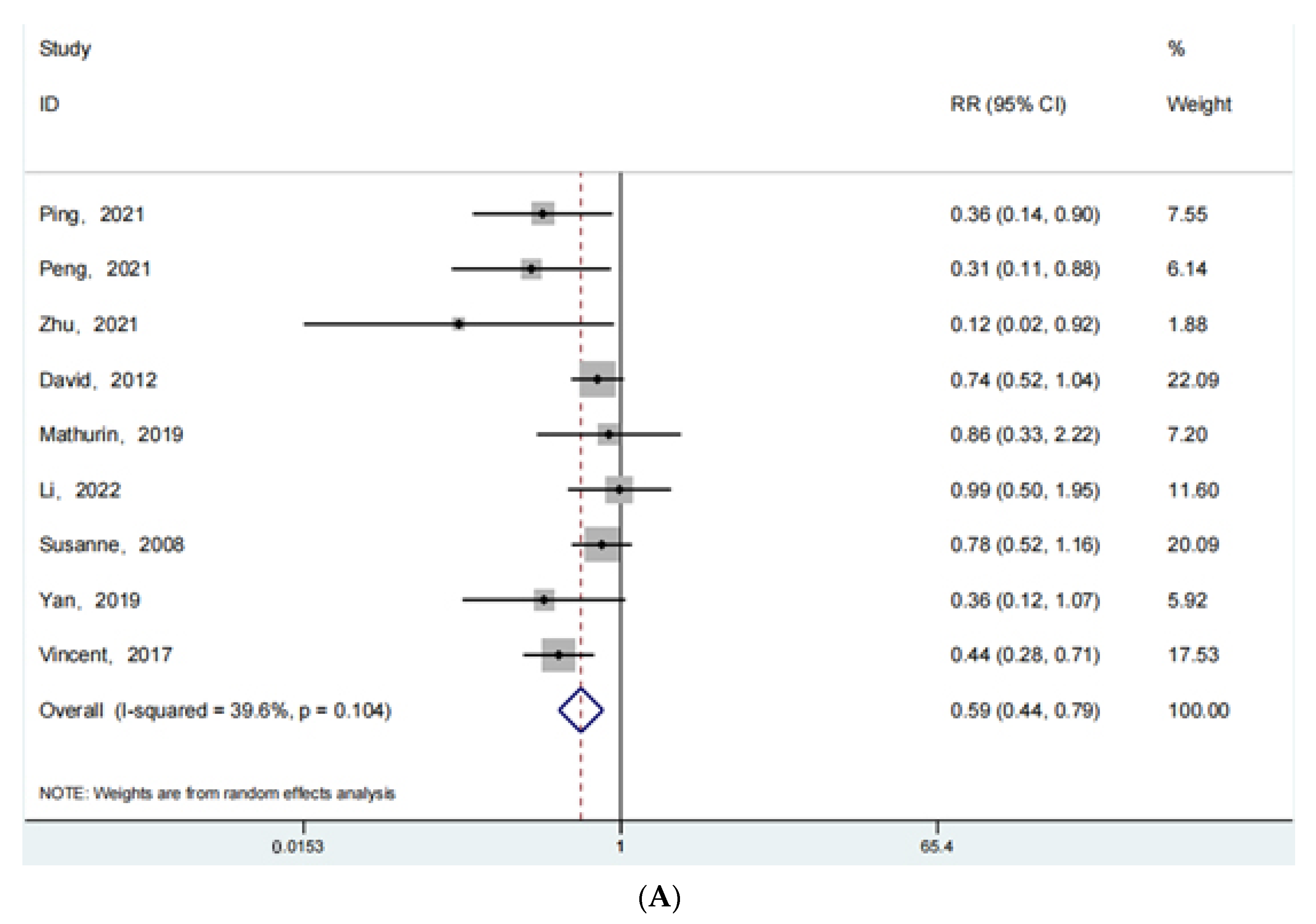
3.3. Length of Hospitalization
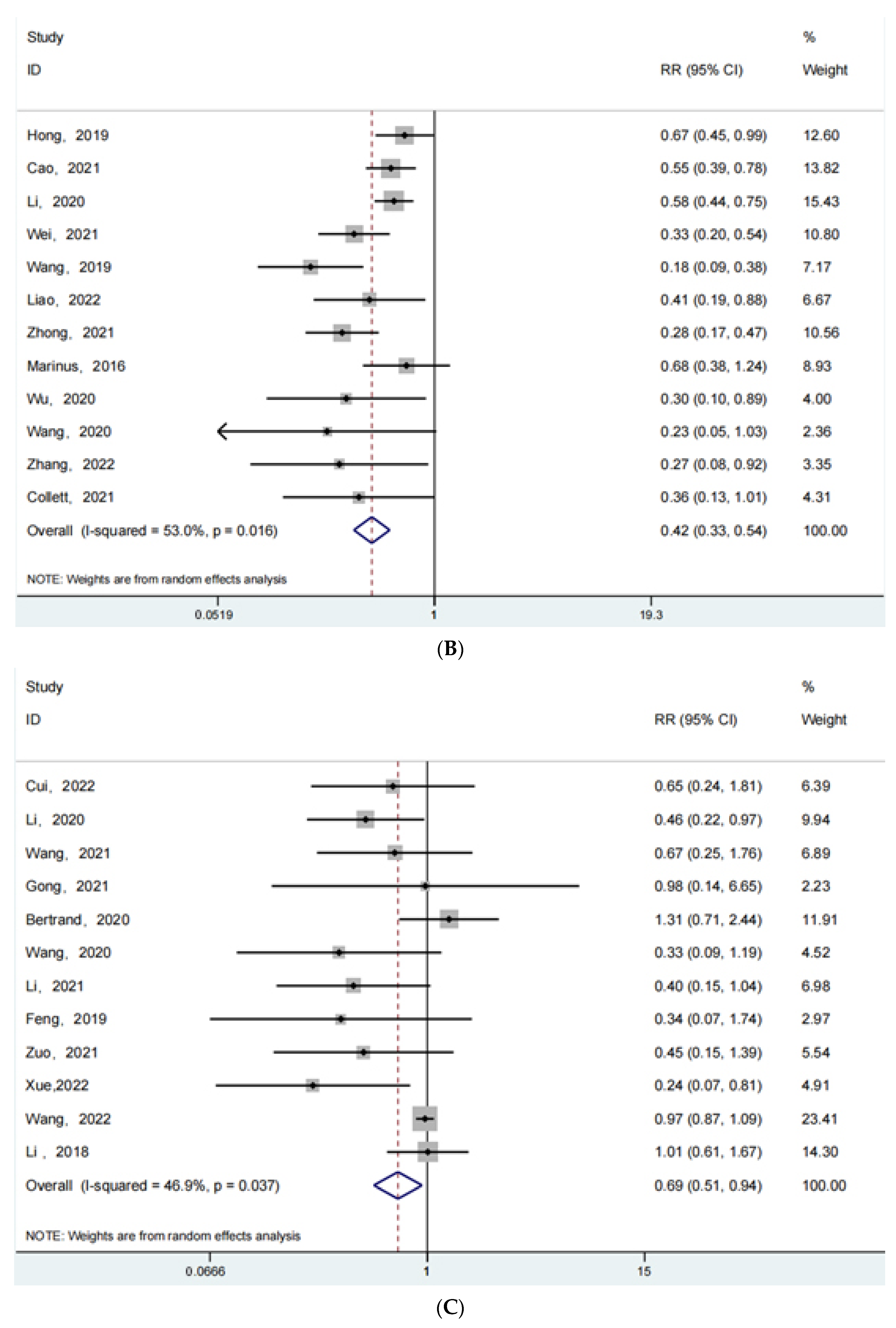
3.4. Complications
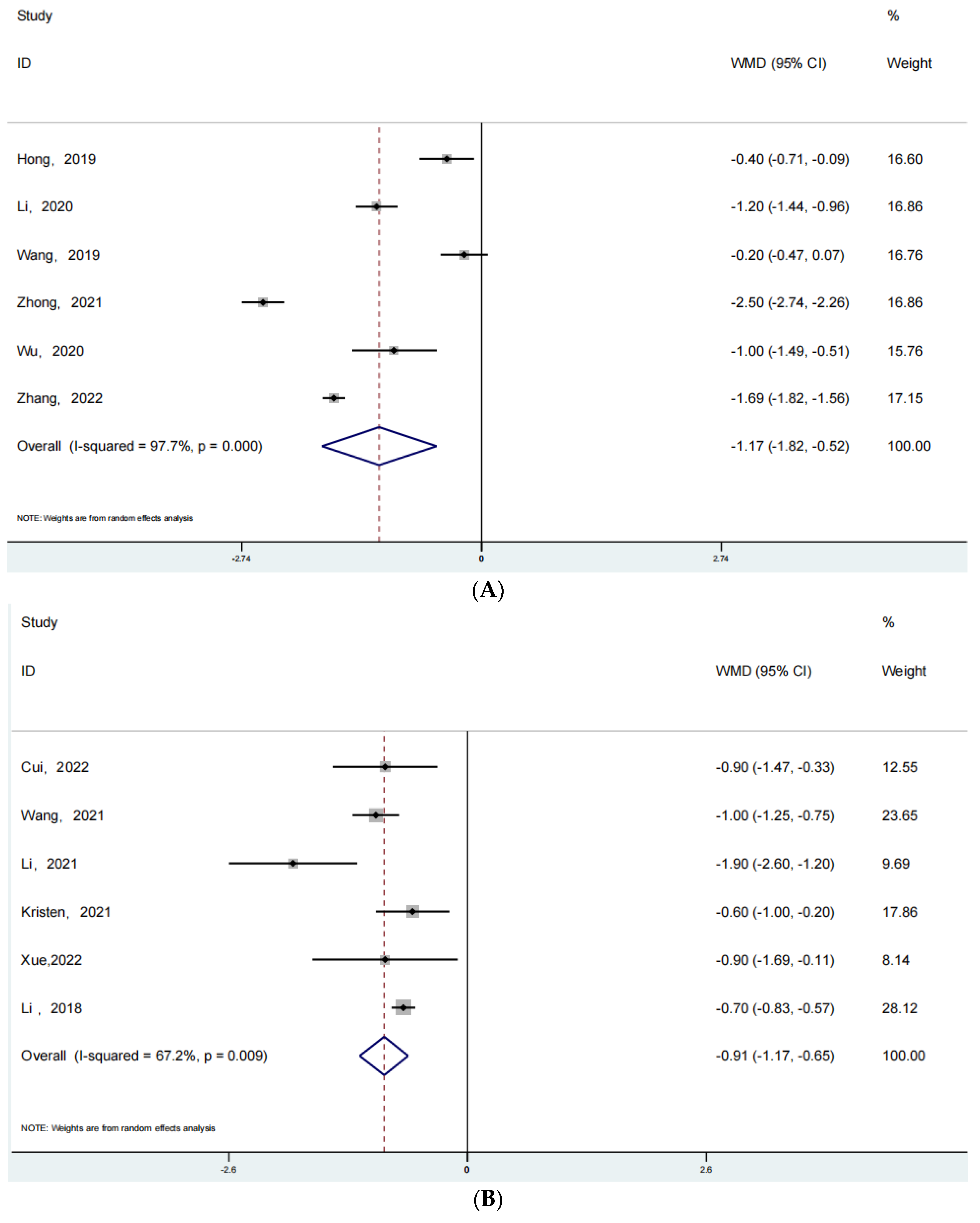
3.5. Visual Analogue Scale (VAS)
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ljungqvist, O. ERAS—Enhanced recovery after surgery: Moving evidence-based perioperative care to practice. J. Parenter. Enter. Nutr. 2014, 38, 559–566. [Google Scholar] [CrossRef]
- Wainwright, T.W.; Gill, M.; McDonald, D.A.; Middleton, R.G.; Reed, M.; Sahota, O.; Yates, P.; Ljungqvist, O. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2019, 91, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Rollins, K.E.; Lobo, D.N.; Joshi, G.P. Enhanced recovery after surgery: Current status and future progress. Best Pract. Res. Clin. Anaesthesiol. 2020, 35, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Soffin, E.M.; Wetmore, D.S.; Barber, L.A.; Vaishnav, A.S.; Beckman, J.D.; Albert, T.J.; Gang, C.H.; Qureshi, S.A. An enhanced recovery after surgery pathway: Association with rapid discharge and minimal complications after anterior cervical spine surgery. Neurosurg. Focus 2019, 46, E9. [Google Scholar] [CrossRef]
- Wainwright, T.W. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2020, 91, 363. [Google Scholar] [CrossRef] [PubMed]
- Debono, B.; Wainwright, T.W.; Wang, M.Y.; Sigmundsson, F.G.; Yang, M.M.; Smid-Nanninga, H.; Bonnal, A.; Le Huec, J.-C.; Fawcett, W.J.; Ljungqvist, O.; et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J. 2021, 21, 729–752. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, J.; He, K.; Zhang, Y.; Zhang, Y. Optimized clinical practice for superaged patients with hip fracture: Significance of damage control and enhanced recovery program. Burn. Trauma 2019, 7, s41038-019-0159-y. [Google Scholar] [CrossRef]
- Chen, K.K.; Chan, J.J.; Zubizarreta, N.J.; Poeran, J.; Chen, D.D.; Moucha, C.S. Enhanced recovery after surgery protocols in lower extremity joint arthroplasty: Using observational data to identify the optimal combination of components. J. Arthroplast. 2021, 36, 2722–2728. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J. Clin. Epidemiol. 2021, 134, 178–189. [Google Scholar] [CrossRef]
- Kotz, D.; West, R. Key concepts in clinical epidemiology: Addressing and reporting sources of bias in randomized controlled trials. J. Clin. Epidemiol. 2021, 143, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Barili, F.; Parolari, A.; Kappetein, P.A.; Freemantle, N. Statistical Primer: Heterogeneity, random- or fixed-effects model analyses?†. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 317–321. [Google Scholar] [CrossRef]
- Ping, H.; Ling, X.; Xue, Y.; Dong, F. Effect of ERAS combined with comfortable nursing on quality of life and complications in femoral neck fractures of the aged people. Evid.-Based Complement. Altern. Med. 2021, 2021, 8753076. [Google Scholar] [CrossRef] [PubMed]
- Peng, N.; Li, J. Application effect of case management mode combined with ERAS in elderly patients with hip fracture. Evid.-Based Complement. Altern. Med. 2021, 2021, 1175020. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Yan, Y.; Sun, Y.; Fan, Z.; Fang, N.; Zhang, Y.; Yin, M.; Wan, H.; Mo, W.; Lu, W.; et al. Implementation of ENHANCED RECOVERY AFTER SURGERY (ERAS) protocol for elderly patients receiving surgery for intertrochanteric fracture: A propensity score-matched analysis. J. Orthop. Surg. Res. 2021, 16, 469. [Google Scholar] [CrossRef] [PubMed]
- Macfie, D.; Zadeh, R.A.; Andrews, M.; Crowson, J.; Macfie, J. Perioperative multimodal optimisation in patients undergoing surgery for fractured neck of femur. Surgeon 2012, 10, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Gomez, M.; Marc, C.; Talha, A.; Ruiz, N.; Noublanche, S.; Gillibert, A.; Bergman, S.; Rony, L.; Maynard, V.; Hubert, L.; et al. Fast track care for pertrochanteric hip fractures: How does it impact length of stay and complications? Orthop. Traumatol. Surg. Res. 2019, 105, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Sun, Z.-J.; Zhou, Y.; Sun, W.-T.; Wang, P.-C.; Cai, X.-Y.; Liang, J.-B.; Dong, J.-M.; Zhou, D.-P.; Yu, K.; et al. Perioperative protocol of ankle fracture and distal radius fracture based on enhanced recovery after surgery program: A multicenter prospective clinical controlled study. Pain Res. Manag. 2022, 2022, 3458056. [Google Scholar] [CrossRef] [PubMed]
- Pollmann, C.T.; Røtterud, J.H.; Gjertsen, J.E.; Dahl, F.A.; Lenvik, O.; Årøen, A. Fast track hip fracture care and mortality—An observa-tional study of 2230 patients. BMC Musculoskelet. Disord. 2019, 20, 248. [Google Scholar] [CrossRef] [PubMed]
- Haugan, K.; Johnsen, L.G.; Basso, T.; Foss, O.A. Mortality and readmission following hip fracture surgery: A retrospective study comparing conventional and fast-track care. BMJ Open 2017, 7, e015574. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.J.; Borgbjerg, F.M.; Schousboe, B.; Pedersen, B.D.; Jørgensen, H.L.; Duus, B.R.; Lauritzen, J.B.; Hip Fracture Group of Bispebjerg Hospital. A Comprehensive Hip Fracture Program Reduces Complication Rates and Mortality. J. Am. Geriatr. Soc. 2008, 56, 1831–1838. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Liu, J.; Chen, H.; Ding, W.; Chen, J.; Zhao, B.; Yin, X. Enhanced recovery after surgery (ERAS) in elective intertrochanteric fracture patients result in reduced length of hospital stay (LOS) without compromising functional outcome. J. Orthop. Surg. Res. 2019, 14, 209. [Google Scholar] [CrossRef] [PubMed]
- Liu, V.X.; Rosas, E.; Hwang, J.; Cain, E.; Foss-Durant, A.; Clopp, M.; Huang, M.; Lee, D.C.; Mustille, A.; Kipnis, P.; et al. Enhanced Recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017, 152, e171032. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Jian, X.; Shangguan, Y.; Qing, J.; Chen, L. Effects of enhanced recovery after surgery in total knee arthroplasty for patients older than 65 years. Orthop. Surg. 2019, 11, 229–235. [Google Scholar] [CrossRef]
- Cao, G.; Xiang, S.; Yang, M.; Quan, S.; Yao, J.; Cai, L.; Feng, W.; Yang, X.; Xu, H.; Huang, Z.; et al. Risk factors of opioid use associated with an enhanced-recovery programme after total knee arthroplasty. BMC Musculoskelet. Disord. 2021, 22, 1046. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Rai, S.; Ze, R.; Tang, X.; Liu, R.; Hong, P. Enhanced recovery care versus traditional non-ERAS care following osteotomies in developmental dysplasia of the hip in children: A retrospective case-cohort study. BMC Musculoskelet. Disord. 2020, 21, 234–237. [Google Scholar] [CrossRef]
- Wei, B.; Tang, C.; Li, X.; Lin, R.; Han, L.; Zheng, S.; Xu, Y.; Yao, Q.; Wang, L. Enhanced recovery after surgery protocols in total knee arthroplasty via midvastus approach: A randomized controlled trial. BMC Musculoskelet. Disord. 2021, 22, 856. [Google Scholar] [CrossRef]
- Wang, H.-Y.; Wang, L.; Luo, Z.-Y.; Wang, D.; Tang, X.; Zhou, Z.; Pei, F.-X. Intravenous and subsequent long-term oral tranexamic acid in enhanced-recovery primary total knee arthroplasty without the application of a tourniquet: A randomized placebo-controlled trial. BMC Musculoskelet. Disord. 2019, 20, 478. [Google Scholar] [CrossRef]
- Liao, X.; Xu, X. The effect of cold therapy combined with ERAS in the postoperative care of patients undergoing total knee arthroplasty. Am. J. Transl. Res. 2022, 14, 3154–3163. [Google Scholar]
- Zhong, M.; Liu, D.; Tang, H.; Zheng, Y.; Bai, Y.; Liang, Q.; Yang, X. Impacts of the perioperative fast track surgery concept on the physical and psychological rehabilitation of total hip arthroplasty: A prospective cohort study of 348 patients. Medicine 2021, 100, e26869. [Google Scholar] [CrossRef]
- Stowers, M.D.J.; Manuopangai, L.; Hill, A.G.; Gray, J.R.; Coleman, B.; Munro, J.T. Enhanced recovery after surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J. Surg. 2016, 86, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Xue, H.; Zhang, W.; Wu, Y.; Yang, Y.; Ji, H. Application of enhanced recovery after surgery in total knee arthroplasty in patients with haemophilia A: A pilot study. Nurs. Open 2020, 8, 80–86. [Google Scholar] [CrossRef]
- Wang, H.-Y.; Yuan, M.-C.; Pei, F.-X.; Zhou, Z.-K.; Liao, R. Finding the optimal control level of intraoperative blood pressure in no tourniquet primary total knee arthroplasty combine with tranexamic acid: A retrospective cohort study which supports the enhanced recovery strategy. J. Orthop. Surg. Res. 2020, 15, 350. [Google Scholar] [CrossRef]
- Xu, H.; Xie, J.; Lei, Y.; Huang, Q.; Huang, Z.; Pei, F. Closed suction drainage following routine primary total joint arthroplasty is associated with a higher transfusion rate and longer postoperative length of stay: A retrospective cohort study. J. Orthop. Surg. Res. 2019, 14, 163. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Liu, H.; Li, H.; He, S.; Xiao, L.; Qin, T.; Xu, W.L. Effect of early electroacupuncture combined with enhanced recovery after surgery (ERAS) on pain perception and dysfunction in patients after total knee arthroplasty (TKA). BioMed Res. Int. 2022, 2022, 6560816. [Google Scholar] [CrossRef]
- Collett, G.; Insley, A.P.; Michaelis, S.; Shaji, S.; Feierstein, B.; Martell, J.R., Jr. Reduction of opioid use with enhanced recovery program for total knee arthroplasty. Fed. Pract. 2021, 38, 212–219. [Google Scholar] [PubMed]
- Xu, H.; Yang, J.; Xie, J.; Huang, Z.; Huang, Q.; Cao, G.; Pei, F. Tourniquet use in routine primary total knee arthroplasty is associated with a higher transfusion rate and longer postoperative length of stay: A real-world study. BMC Musculoskelet. Disord. 2020, 21, 620. [Google Scholar] [CrossRef] [PubMed]
- Cui, P.; Wang, P.; Kong, C.; Li, X.Y.; Wang, S.K.; Wang, J.L.; Liu, X.; Lu, S.B. Patients older than 75 years undergoing polysegmental lumbar fusion surgery can also benefit from enhanced recovery after surgery program. Clin. Interv. Aging 2022, ume 17, 245–252. [Google Scholar] [CrossRef]
- Lampilas, A.; Bouyer, B.; Ferrero, E.; Khalifé, M.; Bergeot, A.; Guigui, P.; Lonjon, G. Evaluation of enhanced recovery after spine surgery: Specificities in an academic public hospital. Orthop. Traumatol. Surg. Res. 2021, 107, 103027. [Google Scholar] [CrossRef]
- Li, Z.-E.; Lu, S.-B.; Kong, C.; Sun, W.-Z.; Wang, P.; Zhang, S.-T. Impact of compliance with an enhanced recovery after surgery program on the outcomes among elderly patients undergoing lumbar fusion surgery. Clin. Interv. Aging 2020, ume 15, 2423–2430. [Google Scholar] [CrossRef]
- Duojun, W.; Hui, Z.; Zaijun, L.; Yuxiang, G.; Haihong, C. Enhanced recovery after surgery pathway reduces the length of hospital stay without additional complications in lumbar disc herniation treated by percutaneous endoscopic transforaminal discectomy. J. Orthop. Surg. Res. 2021, 16, 461. [Google Scholar] [CrossRef]
- Gong, J.; Luo, L.; Liu, H.; Li, C.; Tang, Y.; Zhou, Y. How much benefit can patients acquire from enhanced recovery after surgery protocols with percutaneous endoscopic lumbar interbody fusion? Int. J. Gen. Med. 2021, 14, 3125–3132. [Google Scholar] [CrossRef]
- Debono, B.; Sabatier, P.; Boniface, G.; Bousquet, P.; Lescure, J.P.; Garnaud, V.; Hamel, O.; Lonjon, G. Implementation of enhanced re-covery after surgery (ERAS) protocol for anterior cervical discectomy and fusion: A propensity score-matched analysis. Eur Spine J. 2021, 30, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Wang, Q.; Kong, C.; Teng, Z.; Li, Z.; Zhang, S.; Sun, W.; Feng, M.; Lu, S. Enhanced recovery after surgery (ERAS) program for elderly patients with short-level lumbar fusion. J. Orthop. Surg. Res. 2020, 15, 299. [Google Scholar] [CrossRef]
- Li, Z.-E.; Lu, S.-B.; Kong, C.; Sun, W.-Z.; Wang, P.; Zhang, S.-T. Comparative short-term outcomes of enhanced recovery after surgery (ERAS) program and non-ERAS traditional care in elderly patients undergoing lumbar arthrodesis: A retrospective study. BMC Musculoskelet. Disord. 2021, 22, 283. [Google Scholar] [CrossRef]
- Feng, C.; Zhang, Y.; Chong, F.; Yang, M.; Liu, C.; Liu, L.; Huang, C.; Huang, C.; Feng, X.; Wang, X.; et al. Establishment and implementation of an enhanced recovery after surgery (ERAS) pathway tailored for minimally invasive transforaminal lumbar interbody fusion surgery. World Neurosurg. 2019, 129, e317–e323. [Google Scholar] [CrossRef] [PubMed]
- Rao, K.E.; Krodel, D.; Toaz, E.E.; Fanelli, J.; Hajduk, J.; Kato, K.; Rychlik, K.; King, E.; Sarwark, J.; Grayhack, J.; et al. Introduction of an enhanced recovery pathway results in decreased length of stay in patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion: A description of implementation strategies and retrospective before-and-after study of outcomes. J. Clin. Anesthesia 2021, 75, 110493. [Google Scholar] [CrossRef]
- Zuo, X.; Wang, L.; He, L.; Li, P.; Zhou, D.; Yang, Y. Enhanced recovery after surgery protocol accelerates recovery of lumbar disc herniation among elderly patients undergoing discectomy via promoting gastrointestinal function. Pain Res. Manag. 2021, 2021, 3573460. [Google Scholar] [CrossRef]
- Leng, X.; Zhang, Y.; Wang, G.; Liu, L.; Fu, J.; Yang, M.; Chen, Y.; Yuan, J.; Li, C.; Zhou, Y.; et al. An enhanced recovery after surgery pathway: LOS reduction, rapid discharge and minimal complications after anterior cervical spine surgery. BMC Musculoskelet. Disord. 2022, 23, 252. [Google Scholar] [CrossRef]
- Wang, S.; Wang, P.; Li, X.; Sun, W.; Kong, C.; Lu, S. Enhanced recovery after surgery pathway: Association with lower incidence of wound complications and severe hypoalbuminemia in patients undergoing posterior lumbar fusion surgery. J. Orthop. Surg. Res. 2022, 17, 178. [Google Scholar] [CrossRef] [PubMed]
- Dagal, A.; Bellabarba, C.; Bransford, R.; Zhang, F.; Chesnut, R.M.; O’Keefe, G.E.; Wright, D.R.; Dellit, T.H.; Painter, I.; Souter, M.J. Enhanced perioperative care for major spine surgery. Spine 2019, 44, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, H.; Xv, Z.K.; Wang, J.; Yu, Q.F.; Chen, G.; Li, F.C.; Ren, Y.; Chen, Q.X. Enhanced recovery care versus traditional care following laminoplasty: A retrospective case-cohort study. Medicine 2018, 97, e13195. [Google Scholar] [CrossRef] [PubMed]
- Sibia, U.S.; MacDonald, J.H.; King, P.J. Predictors of hospital length of stay in an enhanced recovery after surgery program for primary total hip arthroplasty. J. Arthroplast. 2016, 31, 2119–2123. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Che, J.; Sun, X.; Ren, W. Clinical application of perioperative anaesthesia management based on enhanced recovery after surgery concept to elderly patients undergoing total knee replacement. Comput. Intell. Neurosci. 2022, 2022, 8039358. [Google Scholar] [CrossRef]
- Bardgett, M.; Lally, J.; Malviya, A.; Kleim, B.; Deehan, D. Patient-reported factors influencing return to work after joint replacement. Occup. Med. 2015, 66, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Garriga, C.; Murphy, J.; Leal, J.; Price, A.; Prieto-Alhambra, D.; Carr, A.; Arden, N.; Rangan, A.; Cooper, C.; Peat, G.; et al. Impact of a national enhanced recovery after surgery programme on patient outcomes of primary total knee replacement: An interrupted time series analysis from “The National Joint Registry of England, Wales, Northern Ireland and the Isle of Man”. Osteoarthr. Cartil. 2019, 27, 1280–1293. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, M.G.; Murphy, J.; Cheng, L.; Janarthanan, R.; Judge, A.; Leal, J. Enhanced recovery following hip and knee arthroplasty: A systematic review of cost-effectiveness evidence. BMJ Open 2020, 10, e032204. [Google Scholar] [CrossRef]
- Li, Z.; Li, B.; Wang, G.; Wang, K.; Chen, J.; Liang, Y.; Tang, X.; Yang, Y. Impact of enhanced recovery nursing combined with limb training on knee joint function and neuro-logical function after total knee arthroplasty in patients with knee osteoarthritis. Am. J. Transl. Res. 2021, 13, 6864–6872. [Google Scholar]
- Kerolus, M.G.; Yerneni, K.; Witiw, C.D.; Shelton, A.; Canar, W.J.; Daily, D.; Fontes, R.B.V.; Deutsch, H.; Fessler, R.G.; Buvanendran, A.; et al. Enhanced recovery after surgery pathway for single-level minimally invasive transforaminal lumbar interbody fusion decreases length of stay and opioid consumption. Neurosurgery 2021, 88, 648–657. [Google Scholar] [CrossRef]
- YaDeau, J.T.; Soffin, E.M.; Tseng, A.; Zhong, H.; Dines, D.M.; Dines, J.S.; Gordon, M.A.; Lee, B.H.; Kumar, K.; Kahn, R.L.; et al. A comprehensive enhanced recovery pathway for rotator cuff surgery reduces pain, opioid use, and side effects. Clin. Orthop. Relat. Res. 2021, 479, 1740–1751. [Google Scholar] [CrossRef] [PubMed]
- Ljungqvist, O.; de Boer, H.D.; Balfour, A.; Fawcett, W.J.; Lobo, D.N.; Nelson, G.; Scott, M.J.; Wainwright, T.W.; Demartines, N. Opportunities and challenges for the next phase of enhanced recovery after surgery. JAMA Surg. 2021, 156, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, V.; Divatia, J.V. Enhanced recovery after surgery in liver resection: Current concepts and controversies. Korean J. Anesthesiol. 2019, 72, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.J.; Kim, Y.; Ejaz, A.; Spolverato, G.; Haut, E.R.; Hirose, K.; Wolfgang, C.L.; Choti, M.A.; Pawlik, T.M. Venous thromboembolic prophylaxis after a hepatic resection: Patterns of care among liver surgeons. HPB 2014, 16, 892–898. [Google Scholar] [CrossRef]
| Study (Ref.) | Type of Study | Number of Participants | Age (Years) (Mean ± SD) | Intervention | Quality of the Literature | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Trial | Control | Trial | Control | Trial | Control | ||||
| Ping, 2021 [11] | Retrospective | 40 | 40 | 69.2 | 68.7 | ERAS | CR | 6 | C |
| Peng, 2021 [12] | Retrospective | 51 | 51 | 76.8 | 75.9 | ERAS | CR | 6 | C |
| Zhu, 2021 [13] | Retrospective | 92 | 98 | 78.1 | 77.3 | ERAS | CR | 7 | LOS, C |
| David, 2012 [14] | Retrospective | 117 | 115 | 82.5 | 82.7 | ERAS | CR | 7 | LOS, C |
| Mathurin, 2019 [15] | Prospective | 27 | 27 | 84.5 | 85.0 | ERAS | CR | 8 | LOS, C |
| Li, 2022 [16] | Prospective | 285 | 361 | 46.9 | 50.3 | ERAS | CR | 7 | LOS, C |
| Christian, 2019 [17] | Retrospective | 1140 | 1090 | 79.6 | 79.7 | ERAS | CR | 6 | LOS, C |
| Kristin, 2017 [18] | Retrospective | 1032 | 788 | 83.1 | 83.1 | ERAS | CR | 5 | LOS |
| Susanne, 2008 [19] | Retrospective | 178 | 357 | 83.9 | 84.2 | ERAS | CR | 6 | LOS, C |
| Yan, 2019 [20] | Prospective | 50 | 50 | 77.8 | 78.3 | ERAS | CR | 7 | LOS, C |
| Vincent, 2017 [21] | Retrospective | 2514 | 2488 | 63.2 | 62.1 | ERAS | CR | 6 | LOS, C |
| Study (Ref.) | Type of Study | Number of Participants | Age (Years) (Mean ± SD) | Intervention | Quality of the Literature | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Trial | Control | Trial | Control | Trial | Control | ||||
| Hong, 2019 [22] | Prospective | 106 | 141 | 74.2 | 75.4 | ERAS | CR | 7 | LOS, C, VAS |
| Cao, 2021 [23] | Retrospective | 183 | 178 | 66.1 | 66.0 | ERAS | CR | 6 | LOS, C |
| Li, 2020 [24] | Retrospective | 86 | 82 | 4.0 | 4.2 | ERAS | CR | 6 | LOS, C, VAS |
| Wei, 2021 [25] | Retrospective | 60 | 60 | 65.8 | 65.6 | ERAS | CR | 6 | LOS, C |
| Wang, 2019 [26] | RCT | 59 | 59 | 63.0 | 64.1 | ERAS | CR | 9 | LOS, C, VAS |
| Liao, 2022 [27] | Retrospective | 40 | 40 | 64.8 | 65.3 | ERAS | CR | 8 | C |
| Zhong, 2021 [28] | Prospective | 180 | 168 | 64.0 | 65.0 | ERAS | CR | 5 | LOS, C, VAS |
| Marinus, 2016 [29] | Retrospective | 100 | 100 | 66.7 | 65.4 | ERAS | CR | 6 | LOS, C |
| Wu, 2020 [30] | RCT | 16 | 16 | 35.6 | 31.7 | ERAS | CR | 9 | LOS, C, VAS |
| Wang, 2020 [31] | Retrospective | 91 | 105 | 66.7 | 67.0 | ERAS | CR | 7 | LOS, C |
| Xu, 2019 [32] | Retrospective | 1724 | 4923 | 66.6 | 66.7 | ERAS | CR | 5 | LOS, C, VAS |
| Zhang, 2022 [33] | Retrospective | 50 | 50 | 68.0 | 70.0 | ERAS | CR | 7 | C, VAS |
| Collett, 2021 [34] | Retrospective | 100 | 196 | 67.7 | 66.7 | ERAS | CR | 8 | C |
| Hong, 2020 [35] | Prospective | 1423 | 4902 | 66.7 | 66.6 | ERAS | CR | 7 | LOS |
| Study (Ref.) | Type of Study | Number of Participants | Age (Years) (Mean ± SD) | Intervention | Quality of the Literature | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Trial | Control | Trial | Control | Trial | Control | ||||
| Cui, 2022 [36] | Prospective | 46 | 54 | 79.1 | 79.2 | ERAS | CR | 5 | LOS, C, VAS |
| Adrien, 2021 [37] | Retrospective | 44 | 44 | 55.1 | 55 | ERAS | CR | 7 | LOS |
| Li, 2020 [38] | Retrospective | 91 | 169 | 69.6 | 73.3 | ERAS | CR | 6 | LOS, C |
| Wang, 2021 [39] | Retrospective | 60 | 60 | 47.9 | 46.6 | ERAS | CR | 8 | LOS, C, VAS |
| Gong, 2021 [40] | Retrospective | 46 | 45 | 55.2 | 56.8 | ERAS | CR | 8 | LOS, C |
| Bertrand, 2020 [41] | Retrospective | 271 | 268 | 49.5 | 47.3 | ERAS | CR | 7 | LOS, C |
| Wang, 2020 [42] | Retrospective | 95 | 95 | 72.4 | 70.8 | ERAS | CR | 7 | LOS, C |
| Li, 2021 [43] | Retrospective | 60 | 67 | 73.6 | 74.3 | ERAS | CR | 6 | LOS, C, VAS |
| Feng, 2019 [44] | Retrospective | 44 | 30 | 61 | 59 | ERAS | CR | 6 | LOS, C |
| Kristen, 2021 [45] | Retrospective | 39 | 78 | 15.0 | 14.3 | ERAS | CR | 5 | LOS, VAS |
| Zuo, 2021 [46] | Retrospective | 84 | 95 | 71.3 | 71.6 | ERAS | CR | 6 | LOS, C |
| Xue, 2022 [47] | Retrospective | 70 | 73 | 53.2 | 52.1 | ERAS | CR | 6 | LOS, C, VAS |
| Wang, 2022 [48] | Retrospective | 530 | 530 | 65.0 | 64.2 | ERAS | CR | 7 | C |
| Armagan, 2018 [49] | Retrospective | 183 | 267 | 61.0 | 60.0 | ERAS | CR | 6 | LOS |
| Li, 2018 [50] | Retrospective | 114 | 110 | 58.5 | 56.9 | ERAS | CR | 7 | LOS, C, VAS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tao, J.; Yan, Z.; Bai, G.; Zhang, H.; Li, J. Enhanced Recovery after Surgery Rehabilitation Protocol in the Perioperative Period of Orthopedics: A Systematic Review. J. Pers. Med. 2023, 13, 421. https://doi.org/10.3390/jpm13030421
Tao J, Yan Z, Bai G, Zhang H, Li J. Enhanced Recovery after Surgery Rehabilitation Protocol in the Perioperative Period of Orthopedics: A Systematic Review. Journal of Personalized Medicine. 2023; 13(3):421. https://doi.org/10.3390/jpm13030421
Chicago/Turabian StyleTao, Jiasheng, Zijian Yan, Guowen Bai, Hua Zhang, and Jie Li. 2023. "Enhanced Recovery after Surgery Rehabilitation Protocol in the Perioperative Period of Orthopedics: A Systematic Review" Journal of Personalized Medicine 13, no. 3: 421. https://doi.org/10.3390/jpm13030421
APA StyleTao, J., Yan, Z., Bai, G., Zhang, H., & Li, J. (2023). Enhanced Recovery after Surgery Rehabilitation Protocol in the Perioperative Period of Orthopedics: A Systematic Review. Journal of Personalized Medicine, 13(3), 421. https://doi.org/10.3390/jpm13030421




