Factors Deciding Conservative or Intervention Treatment for Prostate Abscess: A Retrospective Case-Control Study
Abstract
:1. Introduction
2. Materials and Methods
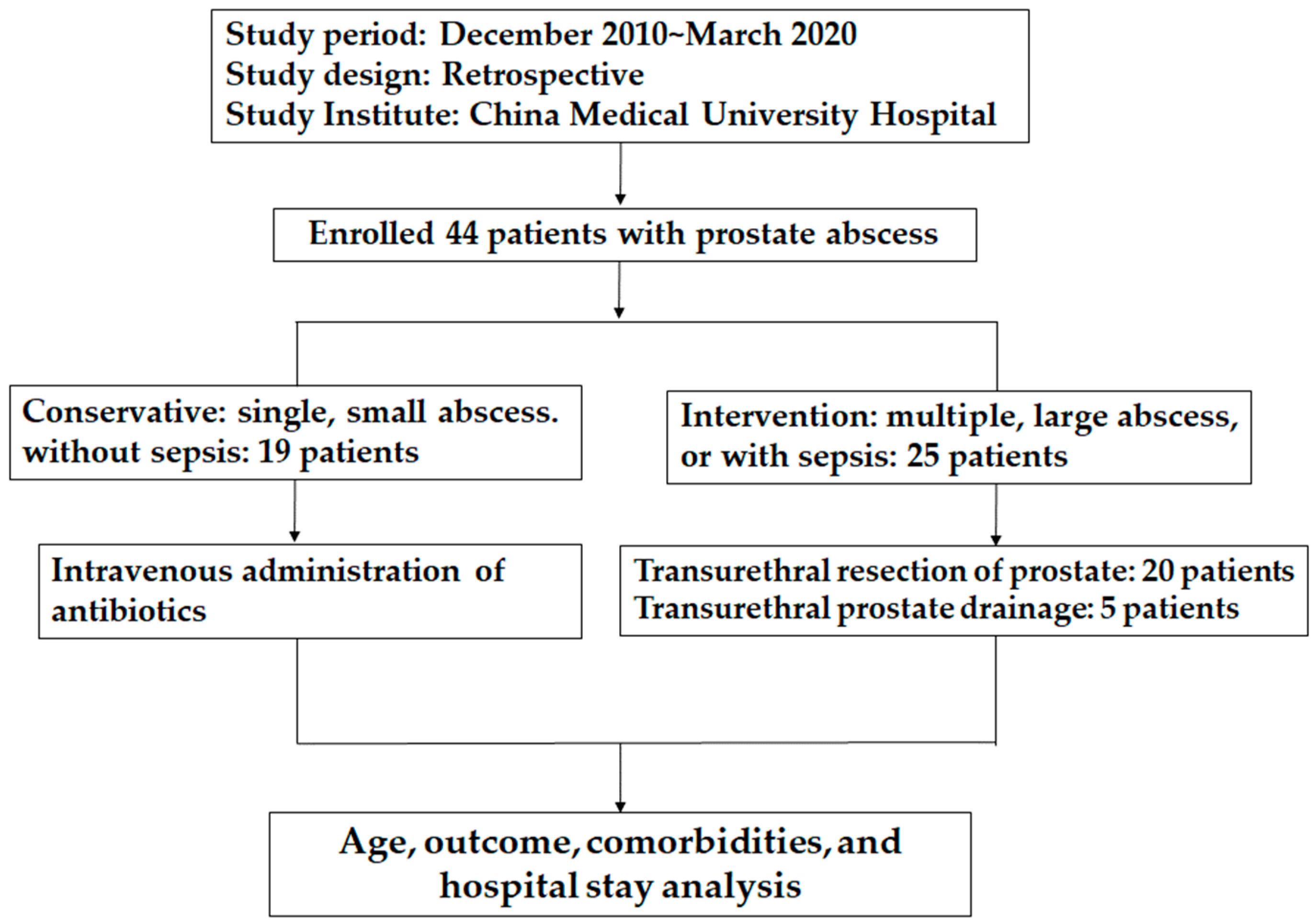
2.1. Patients and Study Design
2.2. Statistical Assay
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, Y.C.; Chen, H.W.; Huang, S.P.; Lin, S.H.; Chu, T.Y.; Li, C.C.; Juan, Y.S.; Wu, W.J. Association of Warmer Weather and Infectious Complications Following Transrectal Ultrasound-Guided Prostate Biopsy. J. Pers. Med. 2022, 12, 446. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.Y.; Kuo, H.C. Satisfaction with Surgical Procedures and Bladder Management of Chronic Spinal Cord Injured Patients with Voiding Dysfunction Who Desire Spontaneous Voiding. J. Pers. Med. 2022, 12, 1751. [Google Scholar] [CrossRef]
- Abdelmoteleb, H.; Rashed, F.; Hawary, A. Management of prostate abscess in the absence of guidelines. Int. Braz. J. Urol. 2017, 43, 835–840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ackerman, A.L.; Parameshwar, P.S.; Anger, J.T. Diagnosis and treatment of patients with prostatic abscess in the post-antibiotic era. Int. J. Urol. 2018, 25, 103–110. [Google Scholar] [CrossRef] [Green Version]
- Liu, W.L.; Chang, J.M.; Chong, I.W.; Hung, Y.L.; Chen, Y.H.; Huang, W.T.; Kuo, H.F.; Hsieh, C.C.; Liu, P.L. Curcumin Inhibits LIN-28A through the Activation of miRNA-98 in the Lung Cancer Cell Line A549. Molecules 2017, 22, 929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paterick, T.E.; Patel, N.; Tajik, A.J.; Chandrasekaran, K. Improving health outcomes through patient education and partnerships with patients. Proc. (Bayl. Univ. Med. Cent.) 2017, 30, 112–113. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.W.; Lin, F.Y.; Chen, Y.H.; Wu, T.C.; Chen, Y.L.; Lin, S.J. Carvedilol inhibits tumor necrosis factor-alpha-induced endothelial transcription factor activation, adhesion molecule expression, and adhesiveness to human mononuclear cells. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 2075–2081. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, P.; Andrade, J.A.; Porto, H.C.; Filho, J.E.; Vinhaes, A.F. Diagnosis and treatment of prostatic abscess. Int. Braz. J. Urol. 2003, 29, 30–34. [Google Scholar] [CrossRef] [Green Version]
- Oshinomi, K.; Matsui, Y.; Unoki, T.; Shimoyama, H.; Nakasato, T.; Morita, J.; Maeda, Y.; Naoe, M.; Fuji, K.; Ogawa, Y. Treatment strategy for prostatic abscess: Eighteen cases’ report and review of literature. Urol. Sci. 2018, 29, 206–209. [Google Scholar] [CrossRef]
- El-Ghar, M.A.; Farg, H.; Sharaf, D.E.; El-Diasty, T. CT and MRI in Urinary Tract Infections: A Spectrum of Different Imaging Findings. Medicina 2021, 57, 32. [Google Scholar] [CrossRef]
- Li, S.; Sun, Z.; Di, N.; Liu, Q.; Wu, F. Prostatic Abscess Combined with Spleen Abscess Due to Multi-Drug-Resistant Gram-Negative Bacilli: A Case Report and Literature Review. Am. J. Men’s Health 2022, 16, 15579883221108898. [Google Scholar] [CrossRef]
- Lam, J.C.; Lang, R.; Stokes, W. How I manage bacterial prostatitis. Clin. Microbiol. Infect. 2023, 29, 32–37. [Google Scholar] [CrossRef]
- Chen, W.C.; Wu, S.Y.; Liu, H.P.; Chang, C.H.; Chen, H.Y.; Chen, H.Y.; Tsai, C.H.; Chang, Y.C.; Tsai, F.J.; Man, K.M.; et al. Identification of melamine/cyanuric acid-containing nephrolithiasis by infrared spectroscopy. J. Clin. Lab. Anal. 2010, 24, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Lan, S.; Guo, Z.; He, Y.; Liu, W.; Guo, H. Brucella prostatic abscess: A retrospective study of eight cases and a literature review. J. Int. Med. Res. 2021, 49, 3000605211027442. [Google Scholar] [CrossRef] [PubMed]
- Frenk, J.; Chen, L.C.; Chandran, L.; Groff, E.O.H.; King, R.; Meleis, A.; Fineberg, H.V. Challenges and opportunities for educating health professionals after the COVID-19 pandemic. Lancet 2022, 400, 1539–1556. [Google Scholar] [CrossRef] [PubMed]
- Battelino, T.; Alexander, C.M.; Amiel, S.A.; Arreaza-Rubin, G.; Beck, R.W.; Bergenstal, R.M.; Buckingham, B.A.; Carroll, J.; Ceriello, A.; Chow, E.; et al. Continuous glucose monitoring and metrics for clinical trials: An international consensus statement. Lancet Diabetes Endocrinol. 2023, 11, 42–57. [Google Scholar] [CrossRef] [PubMed]
- Turco, F.; Gillessen, S.; Cathomas, R.; Buttigliero, C.; Vogl, U.M. Treatment Landscape for Patients with Castration-Resistant Prostate Cancer: Patient Selection and Unmet Clinical Needs. Res. Rep. Urol. 2022, 14, 339–350. [Google Scholar] [CrossRef]
- Nomura, S.; Toyama, Y.; Akatsuka, J.; Endo, Y.; Kimata, R.; Suzuki, Y.; Hamasaki, T.; Kimura, G.; Kondo, Y. Prostatic abscess with infected aneurysms and spondylodiscitis after transrectal ultrasound-guided prostate biopsy: A case report and literature review. BMC Urol. 2021, 21, 11. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, J.D.; Kvist, E. Prostatic abscess. A review of literature and a presentation of 5 cases. Scand. J. Urol. Nephrol. 1993, 27, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Alnadhari, I.; Sampige, V.R.P.; Abdeljaleel, O.; El Ansari, W.; Ali, O.; Salah, M.; Shamsodini, A. Presentation, diagnosis, management, and outcomes of prostatic abscess: Comparison of three treatment modalities. Ther. Adv. Urol. 2020, 12, 1756287220930627. [Google Scholar] [CrossRef]
- Ha, U.S.; Kim, M.E.; Kim, C.S.; Shim, B.S.; Han, C.H.; Lee, S.D.; Cho, Y.H. Acute bacterial prostatitis in Korea: Clinical outcome, including symptoms, management, microbiology and course of disease. Int. J. Antimicrob Agents 2008, 31 (Suppl. S1), S96–S101. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.H.; Mouraviev, V.; Mayes, J.M.; Polascik, T.J. Prostatic abscess as a delayed complication following cryosurgery for primary prostate cancer. Can. J. Urol. 2007, 14, 3646–3648. [Google Scholar] [PubMed]
- Liu, P.L.; Tsai, J.R.; Chiu, C.C.; Hwang, J.J.; Chou, S.H.; Wang, C.K.; Wu, S.J.; Chen, Y.L.; Chen, W.C.; Chen, Y.H.; et al. Decreased expression of thrombomodulin is correlated with tumor cell invasiveness and poor prognosis in non-small cell lung cancer. Mol. Carcinog. 2010, 49, 874–881. [Google Scholar] [CrossRef]
- Uchiyama, J.; Tanaka, Y.; Kurita, Y.; Sano, C.; Ohta, R. Multiple Prostatic Abscesses Caused by Staphylococcus aureus Without Physical Findings in an Immunosuppressed Older Patient. Cureus 2023, 15, e33555. [Google Scholar] [CrossRef]
- Weinberger, M.; Cytron, S.; Servadio, C.; Block, C.; Rosenfeld, J.B.; Pitlik, S.D. Prostatic abscess in the antibiotic era. Rev. Infect. Dis. 1988, 10, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Granados, E.A.; Caffaratti, J.; Farina, L.; Hocsman, H. Prostatic abscess drainage: Clinical-sonography correlation. Urol. Int. 1992, 48, 358–361. [Google Scholar]
- Morse, L.P.; Moller, C.-C.B.; Harvey, E.; Ward, L.; Cheng, A.C.; Carson, P.J.; Currie, B.J. Prostatic Abscess Due to Burkholderia pseudomallei: 81 Cases From a 19-Year Prospective Melioidosis Study. J. Urol. 2009, 182, 542–547. [Google Scholar] [CrossRef]
- Mitterberger, M.; Horninger, W.; Aigner, F.; Pinggera, G.M.; Steppan, I.; Rehder, P.; Frauscher, F. Ultrasound of the prostate. Cancer Imaging 2010, 10, 40–48. [Google Scholar] [CrossRef] [Green Version]
- Calace, F.P.; Napolitano, L.; Arcaniolo, D.; Stizzo, M.; Barone, B.; Crocetto, F.; Olivetta, M.; Amicuzi, U.; Cirillo, L.; Rubinacci, A.; et al. Micro-Ultrasound in the Diagnosis and Staging of Prostate and Bladder Cancer: A Comprehensive Review. Medicina 2022, 58, 1624. [Google Scholar] [CrossRef]
- Lee, D.S.; Choe, H.S.; Kim, H.Y.; Kim, S.W.; Bae, S.R.; Yoon, B.I.; Lee, S.J. Acute bacterial prostatitis and abscess formation. BMC Urol. 2016, 16, 38. [Google Scholar] [CrossRef] [Green Version]

| Conservative | Intervention | p Value | |
|---|---|---|---|
| Patient number | 19 | 25 | |
| Age (years) | 57.1 | 59.6 | 0.61 |
| Hospital days | 11.6 | 18.5 | 0.02 |
| Abscess | |||
| Number | 1.3 ± 0.5 | 1.8 ± 0.7 | 0.025 |
| Size (cm) | 2.2 ± 0.6 | 3.1 ± 1.0 | 0.001 |
| Volume (cm3) | 7.5 ± 6.9 | 25.4 ± 21.7 | 0.001 |
| Percentage (%) | 14.2 ± 9.1 | 32.3 ± 18.3 | <0.001 |
| Prostate volume (cm3) | 48 ± 14 | 71 ± 27 | 0.003 |
| Comorbidities | Conservative (n = 19) | Intervention (n = 25) | p Value |
|---|---|---|---|
| Diabetes | 15 (78%) | 11 (44%) | 0.02 * |
| Hypertension | 5 (26.3%) | 4 (16%) | 0.40 |
| CAD | 5 (26.3%) | 3 (12%) | 0.22 |
| Cirrhosis | 2 (10.5%) | 6 (24%) | 0.25 |
| HIV | 1 (5.3%) | 2 (8%) | 0.77 |
| Laboratory | Conservative (n = 19) | Intervention (n = 25) | p Value |
|---|---|---|---|
| WBC (average) | 12.1 ± 7.0 | 17.6 ± 9.7 | 0.04 * |
| Urine WBC | 598.0 ± 439.8 | 627.0 ± 434.3 | 0.86 |
| CRP | 9.3 ± 11.8 | 10.3 ± 10.7 | 0.41 |
| Serum creatinine | 1.16 ± 0.51 | 1.47 ± 1.26 | 0.46 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-H.; Pan, S.-Y.; Lin, C.-Y.; Huang, C.-P.; Chung, C.-J.; Chen, Y.-H.; Chen, W.-C. Factors Deciding Conservative or Intervention Treatment for Prostate Abscess: A Retrospective Case-Control Study. J. Pers. Med. 2023, 13, 484. https://doi.org/10.3390/jpm13030484
Chang Y-H, Pan S-Y, Lin C-Y, Huang C-P, Chung C-J, Chen Y-H, Chen W-C. Factors Deciding Conservative or Intervention Treatment for Prostate Abscess: A Retrospective Case-Control Study. Journal of Personalized Medicine. 2023; 13(3):484. https://doi.org/10.3390/jpm13030484
Chicago/Turabian StyleChang, Yi-Huei, Szu-Ying Pan, Chia-Yu Lin, Chi-Ping Huang, Chi-Jung Chung, Yung-Hsiang Chen, and Wen-Chi Chen. 2023. "Factors Deciding Conservative or Intervention Treatment for Prostate Abscess: A Retrospective Case-Control Study" Journal of Personalized Medicine 13, no. 3: 484. https://doi.org/10.3390/jpm13030484
APA StyleChang, Y.-H., Pan, S.-Y., Lin, C.-Y., Huang, C.-P., Chung, C.-J., Chen, Y.-H., & Chen, W.-C. (2023). Factors Deciding Conservative or Intervention Treatment for Prostate Abscess: A Retrospective Case-Control Study. Journal of Personalized Medicine, 13(3), 484. https://doi.org/10.3390/jpm13030484







