Clinical Characteristics of Minimal Lumbar Disc Herniation and Efficacy of Percutaneous Endoscopic Lumbar Discectomy via Transforaminal Approach: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Compliance
2.2. Patient Population
2.3. Medical History Collection and Radiologic Features
2.4. Outcome Measurements and Follow-Up
2.5. Surgical Procedure
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Imaging Features
3.3. Clinical Outcomes
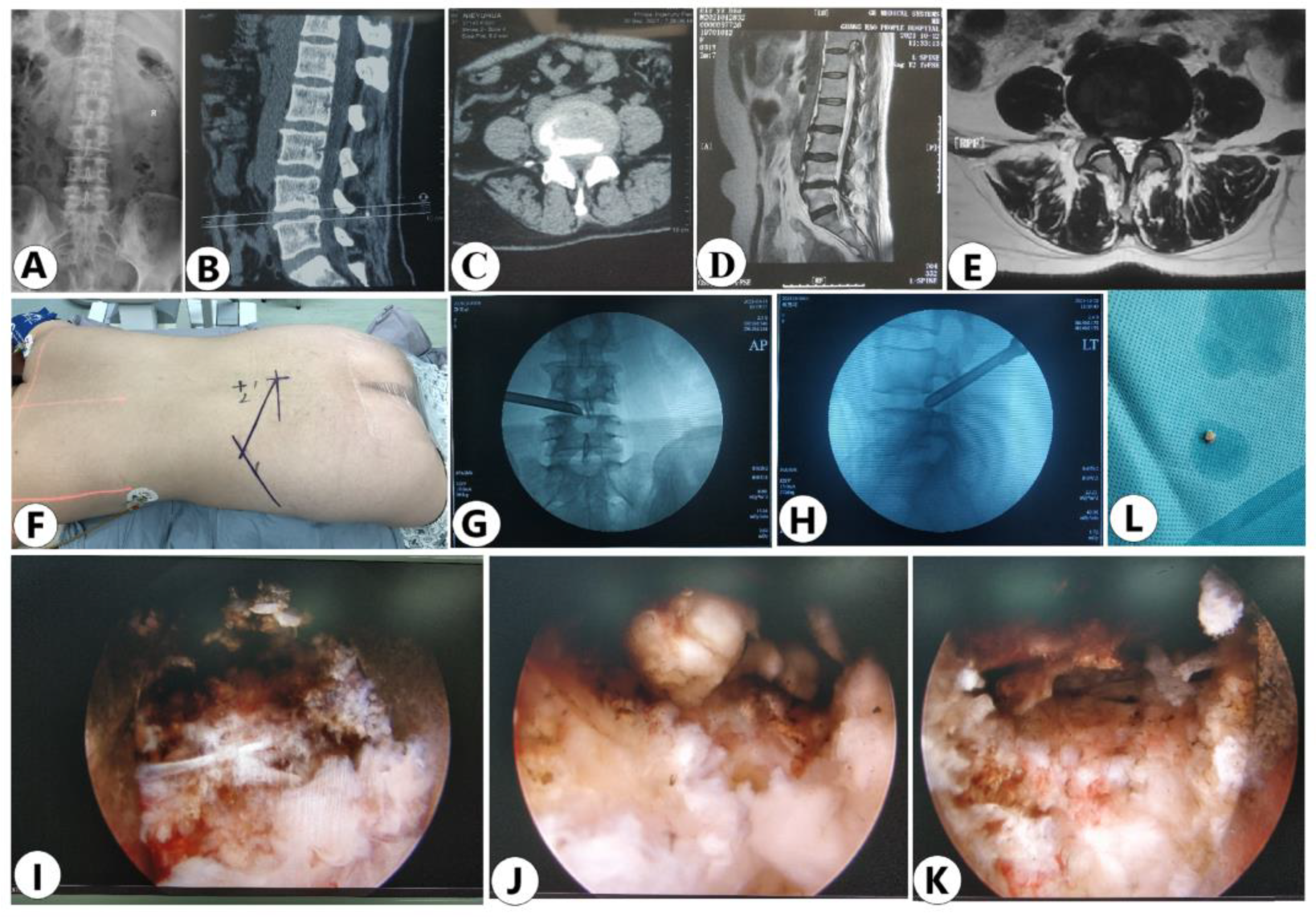
3.4. Case Presentation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Amin, R.M.; Andrade, N.S.; Neuman, B.J. Lumbar disc herniation. Curr. Rev. Musculoskelet. Med. 2017, 10, 507–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kreiner, D.S.; Hwang, S.W.; Easa, J.E.; Resnick, D.K.; Baisden, J.L.; Bess, S.; Cho, C.H.; DePalma, M.J.; Dougherty, P., II; Fernand, R.; et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014, 14, 180–191. [Google Scholar] [CrossRef]
- Jordan, J.; Konstantinou, K.; O’Dowd, J. Herniated lumbar disc. BMJ Clin. Evid. 2009, 2009, 1118. [Google Scholar] [PubMed]
- Vialle, L.R.; Vialle, E.N.; Su’arez Henao, J.E.; Giraldo, G. Lumbar disc herniation. Rev. Bras. Ortop. 2010, 45, 17–22. [Google Scholar] [CrossRef]
- Huang, S.; Wakaizumi, K.; Wu, B.; Shen, B.; Wu, B.; Fan, L.; Baliki, M.N.; Zhan, G.; Apkarian, A.V.; Huang, L. Whole-brain functional network disruption in chronic pain with disk herniation. Pain 2019, 160, 2829–2840. [Google Scholar] [CrossRef]
- Wang, G.J.; Wang, G.J.; Peng, J.M.; Cai, K.M.; Zhang, J.S.; Song, W.H.; Xiao, J. Epidemiology study ON pathogenic factors of lumbar disc herniation. Mod. Prev. Med. 2009, 36, 2401–2403. (In Chinese) [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eun, S.S.; Lee, S.H.; Sabal, L.A. Long-term follow-up results of percutaneous endoscopic lumbar discectomy. Pain Physician 2016, 19, E1161–E1166. [Google Scholar]
- Nie, H.; Zeng, J.; Song, Y.; Chen, G.; Wang, X.; Li, Z.; Jiang, H.; Kong, Q. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation via an interlaminar approach versus a transforaminal approach: A prospective randomized controlled study with 2-year follow up. Spine 2016, 41 (Suppl. 19), B30–B37. [Google Scholar] [CrossRef]
- Choi, K.C.; Shim, H.K.; Park, C.J.; Lee, D.C.; Park, C.K. Usefulness of percutaneous endoscopic lumbar foraminoplasty for lumbar disc herniation. World Neurosurg. 2017, 106, 484. [Google Scholar] [CrossRef]
- Chen, F.; Xin, J.; Su, C.; Liu, X.; Cui, X. Pain Variability of Tissues Under Endoscope in Percutaneous Endoscopic Lumbar Discectomy and Its Significance: A Retrospective Study. Pain Physician 2021, 24, E877–E882. [Google Scholar]
- Xu, J.; Li, Y.; Wang, B.; Lv, G.H.; Wu, P.; Dai, Y.; Jiang, B.; Zheng, Z.; Xiao, S. Percutaneous Endoscopic Lumbar Discectomy for Lumbar Disc Herniation with Modic Changes via a Transforaminal Approach: A Retrospective Study. Pain Physician 2019, 22, E601–E608. [Google Scholar]
- Ru, N.; Su, C.; Li, J.; Li, Y.; Chen, F.; Wang, G.; Sun, J.; Cui, X. Varied Low Back Pain Induced by Different Spinal Tissues in Percutaneous Endoscopic Lumbar Discectomy: A Retrospective Study. Pain Physician 2022, 25, E331–E339. [Google Scholar]
- Fagerlund, M.K.; Thelander, U.; Friberg, S. Size of lumbar disc hernias measured using computed tomography and related to sciatic symptoms. Acta Radiol. 1990, 31, 555–558. [Google Scholar] [CrossRef]
- Van der Windt, D.A.; Simons, E.; Riphagen, I.I.; Ammendolia, C.; Verhagen, A.P.; Laslett, M.; Deville, W.; Deyo, R.A.; Bouter, L.M.; de Vet, H.C.; et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst. Rev. 2010, 2, CD007431. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Li, Y.; Wang, B.; Lv, G.; Li, L.; Dai, Y.; Jiang, B.; Zheng, Z. Minimum 2-Year Efficacy of Percutaneous Endoscopic Lumbar Discectomy versus Microendoscopic Discectomy: A Meta-Analysis. World Neurosurg. 2020, 138, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Gibson, J.N.; Waddell, G. Surgical interventions for lumbar disc prolapse. Cochrane Database Syst. Rev. 2007, 2007, CD001350. [Google Scholar] [PubMed]
- el Barzouhi, A.; Vleggeert-Lankamp, C.L.; Nijeholt, G.J.L.; Van der Kallen, B.F.; Hout, W.B.V.D.; Jacobs, W.C.; Koes, B.W.; Peul, W.C. Magnetic resonance imaging in follow-up assessment of sciatica. N. Engl. J. Med. 2013, 368, 999–1007. [Google Scholar] [CrossRef] [Green Version]
- Nowakowski, A.; Kubaszewski, L.; Kaczmarczyk, J. Przepuklina krazka miedzykregowego w cześci lediźwiowej kregosłupa [Lumbar disc herniation]. Chir. Narz. Ruchu Ortop. Pol. 2007, 72, 95–97. [Google Scholar]
- Deyo, R.A.; Cherkin, D.C.; Weinstein, J.; Howe, J.; Ciol, M.; Mulley, A.G. Involving patients in clinical decisions: Impact of an interactive video program on use of back surgery. Med. Care 2000, 38, 959–969. [Google Scholar] [CrossRef] [Green Version]
- Yu, P.F.; Jiang, F.D.; Liu, J.T.; Jiang, H. Outcomes of conservative treatment for ruptured lumbar disc herniation. Acta Orthop. Belg. 2013, 79, 726–730. [Google Scholar] [PubMed]
- Chiu, C.C.; Chuang, T.Y.; Chang, K.H.; Wu, C.H.; Lin, P.W.; Hsu, W.Y. The probability of spontaneous regression of lumbar herniated disc: A systematic review. Clin. Rehabil. 2015, 29, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Macki, M.; Hernandez-Hermann, M.; Bydon, M.; Gokaslan, A.; McGovern, K.; Bydon, A. Spontaneous regression of sequestrated lumbar disc herniations: Literature review. Clin. Neurol. Neurosurg. 2014, 120, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Mao, F.; Chen, J.; Ma, X.; Dai, Y.; Liu, G.; Dai, F.; Liu, J. Characteristics and mechanisms of resorption in lumbar disc herniation. Arthritis Res. Ther. 2022, 24, 205. [Google Scholar] [CrossRef]
- Sutheerayongprasert, C.; Paiboonsirijit, S.; Kuansongtham, V.; Anuraklekha, S.; Hiranyasthiti, N.; Neti, S. Factors predicting failure of conservative treatment in lumbar-disc herniation. J. Med. Assoc. Thail. 2012, 95, 674–680. [Google Scholar]
- Gugliotta, M.; da Costa, B.R.; Dabis, E.; Theiler, R.; Jüni, P.; Reichenbach, S.; Landolt, H.; Hasler, P. Surgical versus conservative treatment for lumbar disc herniation: A prospective cohort study. BMJ Open 2016, 6, e012938. [Google Scholar] [CrossRef] [Green Version]
- Çitişli, V.; İbrahimoğlu, M. Spontaneous remission of a big subligamentous extruded disc herniation: Case report and review of the literature. Korean J. Spine 2015, 12, 19–21. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Upadhyaya, S.; Yeung, C.M.; Ostergaard, P.J.; Fogel, H.A.; Cha, T.; Schwab, J.; Bono, C.; Hershman, S. Does size matter? An analysis of the efect of lumbar disc herniation size on the success of nonoperative treatment. Glob. Spine J. 2020, 10, 881–887. [Google Scholar] [CrossRef]
- Daffner, S.D.; Hymanson, H.J.; Wang, J.C. Cost and use of conservative management of lumbar disc herniation before surgical discectomy. Spine J. 2010, 10, 463–468. [Google Scholar] [CrossRef]
- Chen, P.; Hu, Y.; Li, Z. Percutaneous endoscopic transforaminal discectomy precedes interlaminar discectomy in the efcacy and safety for lumbar disc herniation. Biosci. Rep. 2019, 39, BSR20181866. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.-S.; Chu, L.; Chen, C.-M.; Wang, X.-F.; Xie, P.-G.; Deng, R.; Yu, K.-X.; Shi, L.; Zhang, Z.-X.; Rong, L.-M.; et al. Foraminoplasty at the tip or base of the superior articular process for lateral recess stenosis in percutaneous endoscopic lumbar discectomy: A multicenter, retrospective, controlled study with 2-year follow-Up. BioMed Res. Int. 2018, 2018, 7692794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Yuan, S.; Tian, Y.; Wang, L.; Gong, L.; Zheng, Y.; Li, J. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: Minimum 2-year follow-up results. J. Neurosurg. Spine 2018, 28, 317–325. [Google Scholar] [CrossRef] [Green Version]
- Ren, C.; Qin, R.; Li, Y.; Wang, P. Microendoscopic discectomy combined with annular suture versus percutaneous transforaminal endoscopic discectomy for lumbar disc herniation: A prospective observational study. Pain Physician 2020, 23, E713–E721. [Google Scholar] [PubMed]
- Choi, K.-C.; Shim, H.-K.; Hwang, J.-S.; Shin, S.H.; Lee, D.C.; Jung, H.H.; Park, H.A.; Park, C.-K. Comparison of surgical invasiveness between microdiscectomy and 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg. 2018, 116, e750–e758. [Google Scholar] [CrossRef] [PubMed]






| Item | Average (%) | |
|---|---|---|
| Total Number | 72 | |
| Gender | Male | 32 (44.44%) |
| Female | 40 (55.56%) | |
| Segments | L1/2 | 2 (2.78%) |
| L2/3 | 3 (4.17%) | |
| L3/4 | 7 (9.72%) | |
| L4/5 | 32 (44.44%) | |
| L5-S1 | 28 (38.89%) | |
| OP method | TF-PELD | 72 (100%) |
| Side | Left | 34 (47.22%) |
| Right | 38 (52.78%) | |
| Age | <30 years | 10 (13.89%) |
| 30–40 years | 36 (50.00%) | |
| 40–50 years | 14 (19.44%) | |
| >50 years | 12 (16.67%) | |
| Number of outpatient visits | <3 | 12 (16.67%) |
| ≥3 | 60 (83.33%) | |
| Duration of onset | <1 month | 67(93.06%) |
| ≥1 months | 5(6.94%) | |
| Speed of onset | Acute | 69(95.83%) |
| Chronic | 3(4.17%) | |
| Duration of conservative treatment | <1 month | 3 (4.17%) |
| (1 month, 3 months) | 17(23.61%) | |
| ≥3 months | 52 (72.22%) | |
| Straight leg raising test | Positive | 70 (97.22%) |
| Negative | 2 (2.78%) | |
| Heel and toe walk | Normal | 69 (95.83%) |
| Impaired | 3 (4.17%) | |
| Item | Average (%) | |
|---|---|---|
| Total Number | 72 | |
| The integrity of PLL | YES | 68 (94.44%) |
| NO | 4 (5.56%) | |
| Disc Location | Central | 0 (0.00%) |
| Paracentral | 72 (100.0%) | |
| Foraminal | 0 (0.00%) | |
| Extraforaminal | 0 (0.00%) | |
| Disc Type | Shoulder | 60 (83.33%) |
| Axillary | 12 (16.67%) | |
| Disc Size | ≥50% canal compromise | 0 (0.00%) |
| <50% canal compromise | 72 (100.0%) | |
| Migration | Overly up-migrated | 0 (0.00%) |
| Overly down-migrated | 0 (0.00%) | |
| Moderately up-migrated | 5(6.94%) | |
| Moderately down-migrated | 7(9.72%) | |
| Slightly up-migrated | 33 (45.83%) | |
| Slightly down-migrated | 27(37.50%) | |
| DHI | <1/16 | 4 (5.56%) |
| [1/16, 1/8) | 66 (91.67%) | |
| [1/8, 1/4) | 2 (2.78%) | |
| [1/4, 1/2) | 0 (0.00%) | |
| ≥1/2 | 0 (0.00%) | |
| Calcification | YES | 2 (2.78%) |
| NO | 70 (97.22%) | |
| Variables | N | VAS-Back | VAS-Leg | ODI | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (Min-Max) | Mean ± SD | Median (Min-Max) | Mean ± SD | Median (Min-Max) | ||
| Preoperative | 72 | 5.96 ± 2.10 | 6.00 (1.00–10.00) | 7.83 ± 1.31 | 8.00 (1.00–10.00) | 47.60 ± 12.13 | 50.00 (10.00–90.00) |
| Postop. 1st day | 72 | 3.37 ± 0.97 * | 3.00 (1.00–8.00) | 3.12 ± 1.00 * | 3.00 (1.00–6.00) | 20.59 ± 11.43 * | 30.00 (5.00–55.00) |
| Postop. 1st month | 72 | 3.01 ± 1.07 | 3.00 (1.00–8.00) | 2.74 ± 1.20 | 3.00 (1.00–6.00) | 20.04 ± 10.43 | 20.00 (5.00–45.00) |
| Postop. 3rd month | 72 | 2.63 ± 1.08 | 1.00 (1.00–5.00) | 2.00 ± 0.97 | 2.00 (1.00–4.00) | 19.64 ± 9.87 | 20.00 (5.00–40.00) |
| Postop. 6th month | 72 | 2.40 ± 0.86 | 1.00 (1.00–5.00) | 1.49 ± 1.07 | 1.00 (1.00–3.00) | 19.00 ± 7.05 | 20.00 (5.00–35.00) |
| Postop. 12th month | 72 | 1.98 ± 1.01 | 1.00 (1.00–5.00) | 1.23 ± 0.77 | 1.00 (1.00–3.00) | 13.00 ± 3.01 | 13.00 (0.00–25.00) |
| Postop. 24th month | 46 | 1.57 ± 1.01 | 1.00 (1.00–5.00) | 1.17 ± 0.89 | 1.00 (1.00–3.00) | 11.00 ± 3.26 | 11.00 (0.00–20.00) |
| Grade | Excellent | Good | Fair | Poor |
|---|---|---|---|---|
| Patients (n) | 36 | 30 | 6 | 0 |
| Percentage (%) | 50.00 | 41.67 | 8.33 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, F.; Yang, G.; Wang, J.; Ge, Z.; Wang, H.; Guo, Y.; Yang, H.; Jing, X.; Liu, X.; Cui, X. Clinical Characteristics of Minimal Lumbar Disc Herniation and Efficacy of Percutaneous Endoscopic Lumbar Discectomy via Transforaminal Approach: A Retrospective Study. J. Pers. Med. 2023, 13, 552. https://doi.org/10.3390/jpm13030552
Chen F, Yang G, Wang J, Ge Z, Wang H, Guo Y, Yang H, Jing X, Liu X, Cui X. Clinical Characteristics of Minimal Lumbar Disc Herniation and Efficacy of Percutaneous Endoscopic Lumbar Discectomy via Transforaminal Approach: A Retrospective Study. Journal of Personalized Medicine. 2023; 13(3):552. https://doi.org/10.3390/jpm13030552
Chicago/Turabian StyleChen, Feifei, Guihe Yang, Jinjin Wang, Zhongpeng Ge, Heran Wang, Yifei Guo, Heng Yang, Xingzhi Jing, Xiaoyang Liu, and Xingang Cui. 2023. "Clinical Characteristics of Minimal Lumbar Disc Herniation and Efficacy of Percutaneous Endoscopic Lumbar Discectomy via Transforaminal Approach: A Retrospective Study" Journal of Personalized Medicine 13, no. 3: 552. https://doi.org/10.3390/jpm13030552
APA StyleChen, F., Yang, G., Wang, J., Ge, Z., Wang, H., Guo, Y., Yang, H., Jing, X., Liu, X., & Cui, X. (2023). Clinical Characteristics of Minimal Lumbar Disc Herniation and Efficacy of Percutaneous Endoscopic Lumbar Discectomy via Transforaminal Approach: A Retrospective Study. Journal of Personalized Medicine, 13(3), 552. https://doi.org/10.3390/jpm13030552








