Use, Abuse, and Misuse of Nasal Medications: Real-Life Survey on Community Pharmacist’s Perceptions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Analysis
3. Results
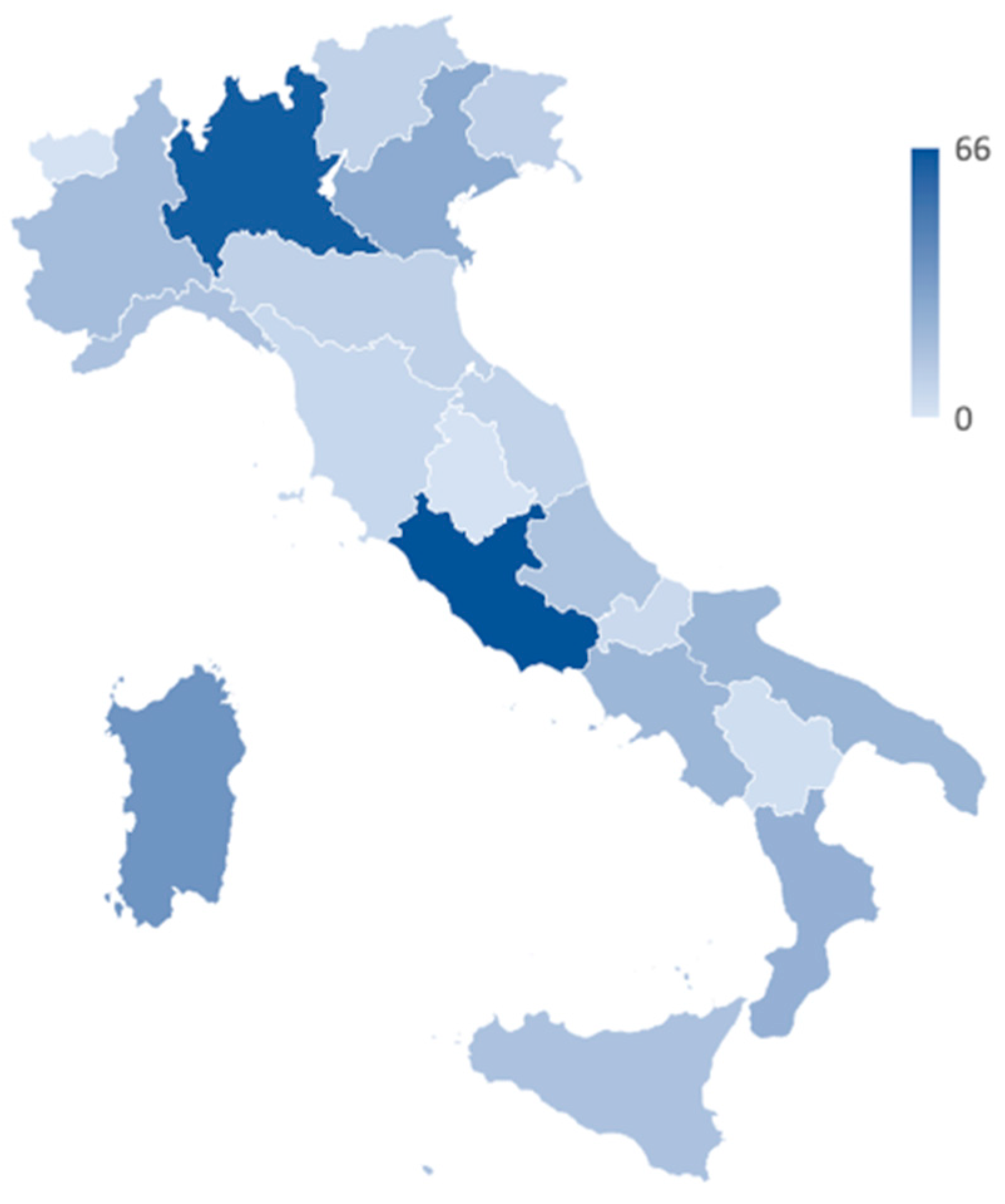
3.1. General Characteristics of the Study Population
3.2. Medication Use
4. Discussion
- -
- The number of membrane alpha-adrenergic receptors would be decreased by downregulation due to the chronic assumption of exogenous sympathomimetic amines. Consequently, endogenous noradrenaline production would be decreased by presynaptic negative feedback, thus inducing relative dilatation of the submucosal sinusoid venous plexuses [33];
- -
- Adrenergic receptors’ intracellular pathway may become refractory to nasal decongestants, causing the patient to increase the doses of nasal decongestants needed to achieve an effective pharmacological effect, a phenomenon also known as “tachyphylaxis” [34];
- -
- The stimulation of adrenergic receptors may induce intense vasoconstriction of submucosal arterioles thus promoting the development of mucosal ischemia and consequent interstitial edema [35].
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Survey
| Q1. Region * _____________ | |
| Q2. Province * _____________ | |
Q3. Type of pharmacy *
| |
Q4. Years since graduation *
| |
Q5. Educational qualification *
| |
| Q6. What are the most frequent age groups among the patients requiring intranasal decongestants? * Evaluation score: 1 = never; 2 = sometimes; 3 = usually; 4 = very often; 5 = always | |
| 0/17 Childhood/Adolescents | □1 □2 □3 □4 □5 |
| 18/35 Young adults | □1 □2 □3 □4 □5 |
| 36/60 Adults | □1 □2 □3 □4 □5 |
| 61/74 Late adults | □1 □2 □3 □4 □5 |
| 75/84 Elderly | □1 □2 □3 □4 □5 |
| Over 85 Seniors | □1 □2 □3 □4 □5 |
| Q7. How often do you dispense nasal sprays containing the following active principles on your own initiative? Evaluation score: 1 = 0 times a week; 2 = 1–10 times a week; 3 = 10 times a day; 4 = >10 times a day. | |
| Alpha-agonists | □1 □2 □3 □4 |
| Corticosteroids (over the counter) | □1 □2 □3 □4 |
| Alpha-agonists combined with antihistamines | □1 □2 □3 □4 |
| Saline solutions | □1 □2 □3 □4 |
| Marine or hypertonic solutions | □1 □2 □3 □4 |
| Q8. How often does the patient specifically request nasal sprays containing the following active principles? Evaluation score: 1 = 0 times a week; 2 = 1–10 times a week; 3 = 10 times a day; 4 = >10 times a day. | |
| Alpha-agonists | □1 □2 □3 □4 |
| Corticosteroids (over the counter) | □1 □2 □3 □4 |
| Alpha-agonists combined with antihistamines | □1 □2 □3 □4 |
| Saline solutions | □1 □2 □3 □4 |
| Marine or hypertonic solutions | □1 □2 □3 □4 |
| Q9. Based on your experience, how often do the patients require alpha-agonist decongestants in the following rhinology diseases? Evaluation score: 1 = 0 times a week; 2 = 1–10 times a week; 3 = 10 times a day; 4 = >10 times a day. | |
| Viral rhinitis | □1 □2 □3 □4 |
| Allergic rhinitis | □1 □2 □3 □4 |
| Non-allergic vasomotor rhinitis | □1 □2 □3 □4 |
| Rhinosinusitis without nasal polyps | □1 □2 □3 □4 |
| Rhinosinusitis with nasal polyps | □1 □2 □3 □4 |
Q10. What is the average dosage used by your patients for alpha-agonist nasal sprays?
| |
| Q11. On an average sample of ten patients, how many in your opinion use nasal sprays at a higher dosage than that reported in the technical data sheet? ⓪ ① ② ③ ④ ⑤ ⑥ ⑦ ⑧ ⑨ ⑩ | |
Q12. What is the average duration of alpha-agonist nasal-spray therapy in your patients?
| |
| Q13. On an average sample of 10 patients, how many buy nasal sprays recurrently (i.e., at least one pack every two weeks)? ⓪ ① ② ③ ④ ⑤ ⑥ ⑦ ⑧ ⑨ ⑩ | |
References
- Hoehle, L.; Phillips, K.; Bergmark, R.; Caradonna, D.; Gray, S.; Sedaghat, A. Symptoms of chronic rhinosinusitis differentially impact general health-related quality of life. Rhinology 2016, 54, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.A.; Orlandi, R.R.; Rudmik, L. Cost of adult chronic rhinosinusitis: A systematic review. Laryngoscope 2015, 125, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.V.; Dykewicz, M.S.; Bernstein, D.I.; Blessing-Moore, J.; Cox, L.; Khan, D.A.; Lang, D.M.; Nicklas, R.A.; Oppenheimer, J.; Portnoy, J.M. The diagnosis and management of rhinitis: An updated practice parameter. J. Allergy Clin. Immunol. 2008, 122 (Suppl. S2), S1–S84, Erratum in J. Allergy Clin. Immunol. 2008, 122, 1237. [Google Scholar] [CrossRef] [PubMed]
- Maurer, M.; Zuberbier, T. Undertreatment of rhinitis symptoms in Europe: Findings from a cross-sectional questionnaire survey. Allergy 2007, 62, 1057–1063. [Google Scholar] [CrossRef]
- Demoly, P.; Allaert, F.; Lecasble, M. Pragma ERASM, a pharmacoepidemiologic survey on management of intermittent allergic rhinitis in every day general medical practice in France. Allergy 2002, 57, 546–554. [Google Scholar] [CrossRef]
- Parvinroo, S.; Pargam, H.R.K.; Asli, R.H.; Rafiei, E.; Nemati, S. Frequency and causes of self-medication in patients with chronic rhinosinusitis, North of Iran, 2018–2019. Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 3973–3980. [Google Scholar] [CrossRef]
- Fromer, L.M.; Ortiz, G.; Ryan, S.F.; Stoloff, S.W. Insights on allergic rhinitis from the patient perspective. J. Fam. Pract. 2012, 61 (Suppl. S2), S16–S22. [Google Scholar]
- Mehuys, E.; Gevaert, P.; Brusselle, G.; Van Hees, T.; Adriaens, E.; Christiaens, T.; Van Bortel, L.; Van Tongelen, I.; Remon, J.-P.; Boussery, K. Self-Medication in Persistent Rhinitis: Overuse of Decongestants in Half of the Patients. J. Allergy Clin. Immunol. Pract. 2014, 2, 313–319. [Google Scholar] [CrossRef]
- Lockey, R.F. Rhinitis medicamentosa and the stuffy nose. J. Allergy Clin. Immunol. 2006, 118, 1017–1018. [Google Scholar] [CrossRef]
- Graf, P. Rbtis medicamentosa: Aspects of pathophysiology and treatment. Allergy 1997, 52 (Suppl. S40), 28–34. [Google Scholar] [CrossRef]
- Marcinowicz, L.; Konstantynowicz, J.; Godlewski, C. Patients’ perceptions of GP non-verbal communication: A qualitative study. Br. J. Gen. Pract. 2010, 60, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Gopichandran, V.; Sakthivel, K. Doctor-patient communication and trust in doctors during COVID 19 times—A cross sectional study in Chennai, India. PLoS ONE 2021, 16, e0253497. [Google Scholar] [CrossRef] [PubMed]
- Sebastiani, G.; Massa, M.; Riboli, E. Covid-19 epidemic in Italy: Evolution, projections and impact of government measures. Eur. J. Epidemiol. 2020, 35, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Giua, C.; Paoletti, G.; Minerba, L.; Malipiero, G.; Melone, G.; Heffler, E.; Pistone, A.; Keber, E.; Cimino, V.; Fimiani, G.; et al. Community pharmacist’s professional adaptation amid Covid-19 emergency: A national survey on Italian pharmacists. Pharm. Weekbl. 2021, 43, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 2020, 58, 1–464. [Google Scholar] [CrossRef]
- Karatzanis, A.; Chatzidakis, A.; Milioni, A.; Vlaminck, S.; Kawauchi, H.; Velegrakis, S.; Prokopakis, E. Contemporary Use of Corticosteroids in Rhinology. Curr. Allergy Asthma Rep. 2017, 17, 11. [Google Scholar] [CrossRef]
- Fernandes, A.M.; Valera, F.C.P.; Anselmo-Lima, W.T. Mechanism of action of glucocorticoids in nasal polyposis. Braz. J. Otorhinolaryngol. 2008, 74, 279–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canonica, G.W.; Malvezzi, L.; Blasi, F.; Paggiaro, P.; Mantero, M.; Senna, G.; Heffler, E.; Bonavia, M.; Caiaffa, P.; Calabrese, C.; et al. Chronic rhinosinusitis with nasal polyps impact in severe asthma patients: Evidences from the Severe Asthma Network Italy (SANI) registry. Respir. Med. 2020, 166, 105947. [Google Scholar] [CrossRef]
- Hox, V.; Lourijsen, E.; Jordens, A.; Aasbjerg, K.; Agache, I.; Alobid, I.; Bachert, C.; Boussery, K.; Campo, P.; Fokkens, W.; et al. Benefits and harm of systemic steroids for short- and long-term use in rhinitis and rhinosinusitis: An EAACI position paper. Clin. Transl. Allergy 2020, 10, 1. [Google Scholar] [CrossRef]
- Canonica, G.W.; Colombo, G.L.; Bruno, G.M.; Di Matteo, S.; Martinotti, C.; Blasi, F.; Bucca, C.; Crimi, N.; Paggiaro, P.; Pelaia, G.; et al. Shadow cost of oral corticosteroids-related adverse events: A pharmacoeconomic evaluation applied to real-life data from the Severe Asthma Network in Italy (SANI) registry. World Allergy Organ. J. 2019, 12, 100007. [Google Scholar] [CrossRef] [Green Version]
- A Levine, D. ‘Pharming’: The abuse of prescription and over-the-counter drugs in teens. Curr. Opin. Pediatr. 2007, 19, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Schifano, F.; Chiappini, S.; Miuli, A.; Mosca, A.; Santovito, M.C.; Corkery, J.M.; Guirguis, A.; Pettorruso, M.; Di Giannantonio, M.; Martinotti, G. Focus on Over-the-Counter Drugs’ Misuse: A Systematic Review on Antihistamines, Cough Medicines, and Decongestants. Front. Psychiatry 2021, 12, 657397. [Google Scholar] [CrossRef]
- Almutairi, H.; Almutairi, A.; Althwiny, F.; Almutairi, A.; Alwasil, S.; Albadrani, N.; Aljeri, Y.; Alawad, M. Awareness of the Unaizah populations in Al-Qassim province in Saudi Arabia regarding nasal decongestant use for allergic rhinitis and their side effect. J. Fam. Med. Prim. Care 2022, 11, 1070–1076. [Google Scholar] [CrossRef]
- Williams, S.N.; Armitage, C.J.; Tampe, T.; Dienes, K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: A UK-based focus group study. BMJ Open 2020, 10, e039334. [Google Scholar] [CrossRef]
- Xu, B. The impact of COVID-19 on the doctor-patient relationship in China. Front. Public Heal. 2022, 10, 907009. [Google Scholar] [CrossRef] [PubMed]
- Brożek, J.L.; Bousquet, J.; Agache, I.; Agarwal, A.; Bachert, C.; Bosnic-Anticevich, S.; Brignardello-Petersen, R.; Canonica, G.W.; Casale, T.; Chavannes, N.H.; et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines—2016 revision. J. Allergy Clin. Immunol. 2017, 140, 950–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hellings, P.W.; Dobbels, F.; Denhaerynck, K.; Piessens, M.; Ceuppens, J.L.; De Geest, S. Extended Global Allergy and Asthma European Network, World Allergy Organization and Allergic Rhinitis and its Impact on Asthma Study Group. Explorative study on patient’s perceived knowledge level, expectations, preferences and fear of side effects for treatment for allergic rhinitis. Clin. Transl. Allergy 2012, 2, 9. [Google Scholar] [CrossRef] [Green Version]
- Bousquet, J.; Bachert, C.; Canonica, G.W.; Casale, T.B.; Cruz, A.A.; Lockey, R.J.; Zuberbier, T. Unmet needs in severe chronic upper airway disease (SCUAD). J. Allergy Clin. Immunol. 2009, 124, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Corboz, M.; Rivelli, M.; Mingo, G.; McLeod, R.; Varty, L.; Jia, Y.; Hey, J. Mechanism of decongestant activity of α2-adrenoceptor agonists. Pulm. Pharmacol. Ther. 2008, 21, 449–454. [Google Scholar] [CrossRef]
- Sperber, S.J.; Sorrentino, J.V.; Riker, D.K.; Hayden, F.G. Evaluation of an alpha agonist alone and in combination with a nonsteroidal antiinflammatory agent in the treatment of experimental rhinovirus colds. Bull. N. Y. Acad. Med. 1989, 65, 145–160. [Google Scholar]
- Ramey, J.T.; Bailen, E.; Lockey, R.F. Rhinitis medicamentosa. J. Investig. Allergol. Clin. Immunol. 2006, 16, 148–155. [Google Scholar]
- Feinberg, S.M.; Friedlaender, S. Nasal Congestion from Frequent Use of Privine Hydrochloride. JAMA 1945, 128, 1095–1096. [Google Scholar] [CrossRef]
- Hein, P.; Martin, M.C. Signal transduction and regulation: Are all a1-adrenergic receptor subtypes created equal? Biochem. Pharm. 2007, 73, 1097–1106. [Google Scholar] [CrossRef]
- Passali, D.; Salerni, L.; Passali, G.C.; Passàli, F.M.; Bellussi, L. Nasal decongestants in the treatment of chronic nasal obstruction: Efficacy and safety of use. Expert Opin. Drug Saf. 2006, 5, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Graf, P.M.; Hallén, H. Changes in Nasal Reactivity in Patients with Rhinitis medicamentosa after Treatment with Fluticasone Propionate and Placebo Nasal Spray. ORL 1998, 60, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, S.; Williamson, P.; Clearie, K.; Khan, F.; Lipworth, B. Fluticasone Reverses Oxymetazoline-induced Tachyphylaxis of Response and Rebound Congestion. Am. J. Respir. Crit. Care Med. 2010, 182, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Graf, P. Long-term use of oxy- and xylometazoline nasal sprays induces rebound swelling, tolerance, and nasal hyperreactivity. Rhinology 1996, 34, 9–13. [Google Scholar]
- Levy, S.; Abaza, M.M.; Hawkshaw, M.J.; Sataloff, R.T. Psychiatric manifestations of medications commonly prescribed in otolaryngology. Ear Nose Throat J. 2001, 80, 266–268, 270–271. [Google Scholar] [CrossRef]




| n | % | ||
|---|---|---|---|
| Setting | Rural pharmacy | 100 | 26.6 |
| Urban pharmacy | 276 | 73.4 | |
| Years since graduation | <5 years | 88 | 23.4 |
| 5–10 years | 143 | 38.0 | |
| 11–20 years | 100 | 26.6 | |
| >20 years | 45 | 12.0 | |
| Educational qualification | Bachelor’s | 244 | 64.9 |
| Bachelor’s, PhD | 3 | 0.8 | |
| Bachelor’s, Master’s II degree | 111 | 29.5 | |
| Bachelor’s, Master’s II degree, PhD | 1 | 0.3 | |
| Bachelor’s, Master’s II degree, Residency | 7 | 1.9 | |
| Bachelor’s, Residency | 10 | 2.7 |
| <18 | 18–35 | 36–60 | 61–75 | 76–84 | ≥85 | |
|---|---|---|---|---|---|---|
| <18 | - | <0.001 | 0.002 | <0.001 | 0.001 | 0.004 |
| 18–35 | <0.001 | - | 0.001 | 0.549 | 0.002 | <0.001 |
| 36–60 | 0.002 | 0.001 | - | <0.001 | 0.819 | <0.001 |
| 61–75 | <0.001 | 0.549 | <0.001 | - | <0.001 | <0.001 |
| 76–84 | 0.001 | 0.002 | 0.819 | <0.001 | - | <0.001 |
| ≥85 | 0.004 | <0.001 | <0.001 | <0.001 | <0.001 | - |
| Viral | Allergic | Vasomotor | CRSsNP | CRSwNP | |
|---|---|---|---|---|---|
| Viral | - | 0.093 | 0.124 | 0.001 | 0.001 |
| Allergic | 0.093 | - | 0.001 | <0.001 | <0.001 |
| Vasomotor | 0.124 | 0.001 | - | 0.089 | 0.025 |
| CRSsNP | 0.001 | <0.001 | 0.089 | - | 0.586 |
| CRSwNP | 0.001 | <0.001 | 0.025 | 0.586 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russo, E.; Giombi, F.; Paoletti, G.; Heffler, E.; Canonica, G.W.; Pirola, F.; Mercante, G.; Spriano, G.; Malvezzi, L.; Keber, E.; et al. Use, Abuse, and Misuse of Nasal Medications: Real-Life Survey on Community Pharmacist’s Perceptions. J. Pers. Med. 2023, 13, 579. https://doi.org/10.3390/jpm13040579
Russo E, Giombi F, Paoletti G, Heffler E, Canonica GW, Pirola F, Mercante G, Spriano G, Malvezzi L, Keber E, et al. Use, Abuse, and Misuse of Nasal Medications: Real-Life Survey on Community Pharmacist’s Perceptions. Journal of Personalized Medicine. 2023; 13(4):579. https://doi.org/10.3390/jpm13040579
Chicago/Turabian StyleRusso, Elena, Francesco Giombi, Giovanni Paoletti, Enrico Heffler, Giorgio Walter Canonica, Francesca Pirola, Giuseppe Mercante, Giuseppe Spriano, Luca Malvezzi, Enrico Keber, and et al. 2023. "Use, Abuse, and Misuse of Nasal Medications: Real-Life Survey on Community Pharmacist’s Perceptions" Journal of Personalized Medicine 13, no. 4: 579. https://doi.org/10.3390/jpm13040579
APA StyleRusso, E., Giombi, F., Paoletti, G., Heffler, E., Canonica, G. W., Pirola, F., Mercante, G., Spriano, G., Malvezzi, L., Keber, E., SGCP, & Giua, C. (2023). Use, Abuse, and Misuse of Nasal Medications: Real-Life Survey on Community Pharmacist’s Perceptions. Journal of Personalized Medicine, 13(4), 579. https://doi.org/10.3390/jpm13040579










