Exploring the Clinical Efficacy of Venous Thromboembolism Management in Saudi Arabian Hospitals: An Insight into Patient Outcomes
Abstract
:1. Introduction
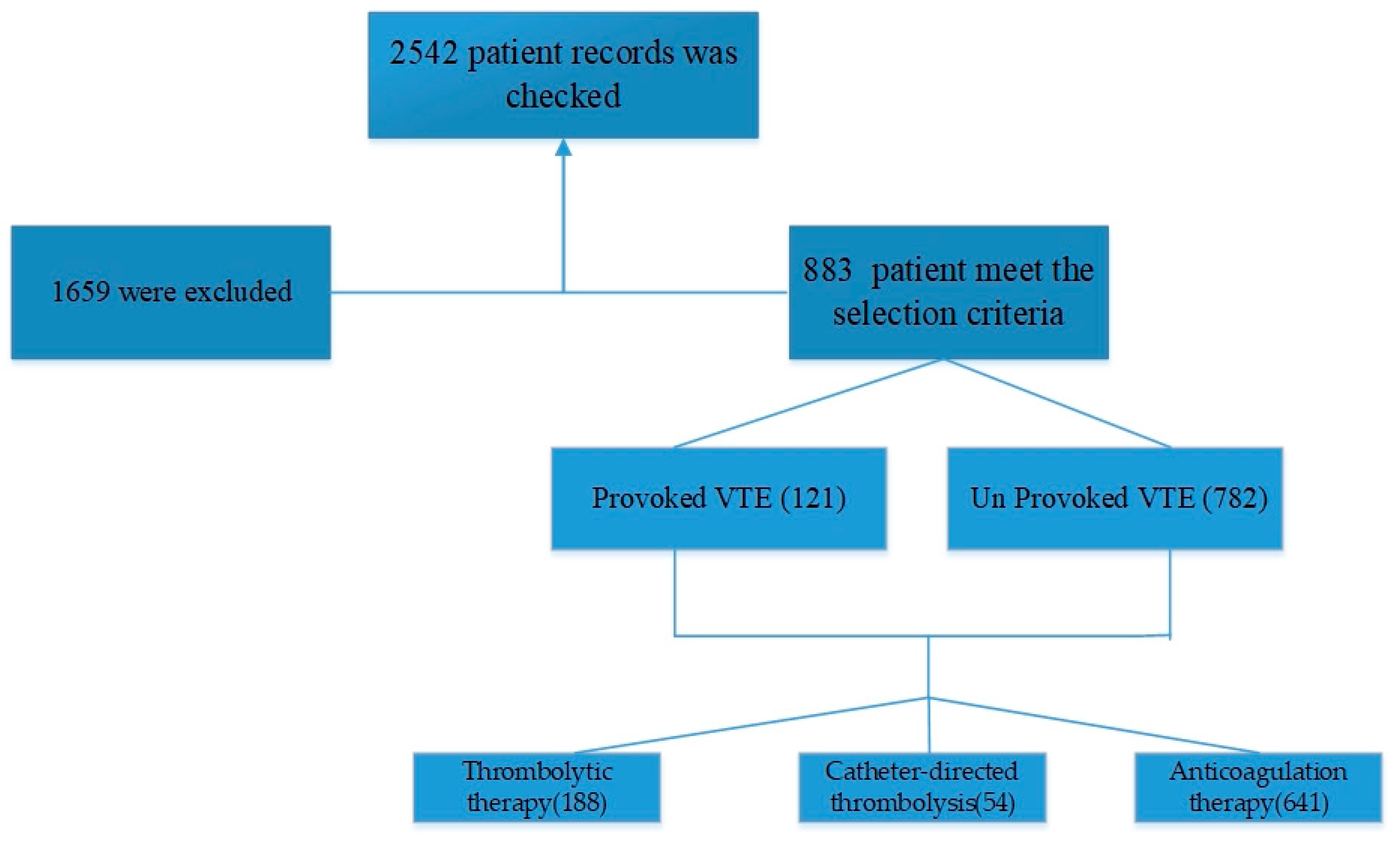
2. Materials and Methods
Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sakr, Y.; Giovini, M.; Leone, M.; Pizzilli, G.; Kortgen, A.; Bauer, M.; Tonetti, T.; Duclos, G.; Zieleskiewicz, L.; Buschbeck, S.; et al. Pulmonary Embolism in Patients with Coronavirus Disease-2019 (COVID-19) Pneumonia: A Narrative Review. Ann. Intensive Care 2020, 10, 124. [Google Scholar] [CrossRef] [PubMed]
- Al-Hameed, F.; Essam, A.-E.-N.; Sharif, G. Venous Thromboembolism-Related Mortality and Morbidity in King Fahd General Hospital, Jeddah, Kingdom of Saudi Arabia. Ann. Thorac. Med. 2011, 6, 193. [Google Scholar] [CrossRef] [PubMed]
- Bosaeed, M.S.; Balubaid, R.N.; Alharbi, A.R.; Alhothali, O.S.; Haji, A.K.; Alkaabi, H.E.; Miyajan, R.A. Assessment of Venous Thromboembolism Awareness Among Surgical Ward Patients in Makkah, Saudi Arabia: A Cross-Sectional Study. Cureus 2022, 14, e27897. [Google Scholar] [CrossRef] [PubMed]
- Burgazli, K.M.; Bilgin, M.; Kavukcu, E.; Altay, M.M.; Ozkan, H.T.; Coskun, U.; Akdere, H.; Ertan, A.K. Diagnosis and Treatment of Deep-Vein Thrombosis and Approach to Venous Thromboembolism in Obstetrics and Gynecology. J. Turk. Ger. Gynecol. Assoc. 2011, 12, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Nopp, S.; Moik, F.; Jilma, B.; Pabinger, I.; Ay, C. Risk of Venous Thromboembolism in Patients with COVID-19: A Systematic Review and Meta-analysis. Res. Pract. Thromb. Haemost. 2020, 4, 1178–1191. [Google Scholar] [CrossRef]
- Behravesh, S.; Hoang, P.; Nanda, A.; Wallace, A.; Sheth, R.A.; Deipolyi, A.R.; Memic, A.; Naidu, S.; Oklu, R. Pathogenesis of Thromboembolism and Endovascular Management. Thrombosis 2017, 2017, 1–13. [Google Scholar] [CrossRef]
- Al-Hameed, F.; Al-Dorzi, H.; Qadhi, A.; Shaker, A.; Al-Gahtani, F.; Al-Jassir, F.; Zahir, G.; Al-Khuwaitir, T.; Addar, M.; Al-Hajjaj, M.; et al. Thromboprophylaxis and Mortality among Patients Who Developed Venous Thromboembolism in Seven Major Hospitals in Saudi Arabia. Ann. Thorac. Med. 2017, 12, 282. [Google Scholar] [CrossRef]
- Beckman, M.G.; Hooper, W.C.; Critchley, S.E.; Ortel, T.L. Venous Thromboembolism. Am. J. Prev. Med. 2010, 38, S495–S501. [Google Scholar] [CrossRef]
- Nalivaeva, N.N.; Turner, A.J.; Zhuravin, I.A. Role of Prenatal Hypoxia in Brain Development, Cognitive Functions, and Neurodegeneration. Front. Neurosci. 2018, 12, 825. [Google Scholar] [CrossRef]
- Ageno, W.; Farjat, A.; Haas, S.; Weitz, J.I.; Goldhaber, S.Z.; Turpie, A.G.G.; Goto, S.; Angchaisuksiri, P.; Dalsgaard Nielsen, J.; Kayani, G.; et al. Provoked versus Unprovoked Venous Thromboembolism: Findings from GARFIELD-VTE. Res. Pract. Thromb. Haemost. 2021, 5, 326–341. [Google Scholar] [CrossRef]
- Baglin, T.; Bauer, K.; Douketis, J.; Buller, H.; Srivastava, A.; Johnson, G. Duration of Anticoagulant Therapy after a First Episode of an Unprovoked Pulmonary Embolus or Deep Vein Thrombosis: Guidance from the SSC of the ISTH. J. Thromb. Haemost. 2012, 10, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Keo, H.H.; Fahrni, J.; Husmann, M.; Gretener, S.B. Assessing the Risk of Recurrent Venous Thromboembolism—A Practical Approach. Vasc. Health Risk Manag. 2015, 17, 451. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Rahman, A.; Carrier, M.; Kearon, C.; Weitz, J.I.; Schulman, S.; Couturaud, F.; Eichinger, S.; Kyrle, P.A.; Becattini, C.; et al. Long Term Risk of Symptomatic Recurrent Venous Thromboembolism after Discontinuation of Anticoagulant Treatment for First Unprovoked Venous Thromboembolism Event: Systematic Review and Meta-Analysis. BMJ 2019, 366, l4363. [Google Scholar] [CrossRef] [PubMed]
- Arnesen, C.A.L.; Veres, K.; Horváth-Puhó, E.; Hansen, J.-B.; Sørensen, H.T.; Brækkan, S.K. Estimated Lifetime Risk of Venous Thromboembolism in Men and Women in a Danish Nationwide Cohort: Impact of Competing Risk of Death. Eur. J. Epidemiol. 2022, 37, 195–203. [Google Scholar] [CrossRef]
- Assareh, H.; Chen, J.; Ou, L.; Hillman, K.; Flabouris, A. Incidences and Variations of Hospital Acquired Venous Thromboembolism in Australian Hospitals: A Population-Based Study. BMC Health Serv. Res. 2016, 16, 511. [Google Scholar] [CrossRef] [PubMed]
- Kupelian, V.; Viscidi, E.; Hall, S.; Li, L.; Eaton, S.; Dilley, A.; Currier, N.; Ferguson, T.; Fanning, L. Increased Risk of Venous Thromboembolism in Patients With Amyotrophic Lateral Sclerosis. Neurol. Clin. Pract. 2023, 13, e200110. [Google Scholar] [CrossRef] [PubMed]
- Ciarambino, T.; Crispino, P.; Para, O.; Giordano, M. Gender Medicine: A New Possible Frontiers of Venous Thromboembolism. Stresses 2023, 3, 167–181. [Google Scholar] [CrossRef]
- Nicholson, M.; Chan, N.; Bhagirath, V.; Ginsberg, J. Prevention of Venous Thromboembolism in 2020 and Beyond. J. Clin. Med. 2020, 9, 2467. [Google Scholar] [CrossRef]
- Salomon, B.; Dasa, V.; Krause, P.C.; Hall, L.; Chapple, A.G. Hospital Length of Stay Is Associated With Increased Likelihood for Venous Thromboembolism After Total Joint Arthroplasty. Arthroplast. Today 2021, 8, 254–257.e1. [Google Scholar] [CrossRef]
- Amin, A.; Neuman, W.R.; Lingohr-Smith, M.; Menges, B.; Lin, J. Influence of the Duration of Hospital Length of Stay on Frequency of Prophylaxis and Risk for Venous Thromboembolism among Patients Hospitalized for Acute Medical Illnesses in the USA. Drugs Context 2019, 8, 212568. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Cushman, M.; Burnett, A.E.; Kahn, S.R.; Beyer-Westendorf, J.; Spencer, F.A.; Rezende, S.M.; Zakai, N.A.; Bauer, K.A.; Dentali, F.; et al. American Society of Hematology 2018 Guidelines for Management of Venous Thromboembolism: Prophylaxis for Hospitalized and Nonhospitalized Medical Patients. Blood Adv. 2018, 2, 3198–3225. [Google Scholar] [CrossRef] [PubMed]
- Barkoudah, E.; Piazza, G.; Hecht, T.E.H.; Grant, P.; Deitelzweig, S.; Fang, M.C.; Fanikos, J.; Kao, C.-K.; Barnes, G.D.; Chen, T.; et al. Extended Venous Thromboembolism Prophylaxis in Medically Ill Patients: An NATF Anticoagulation Action Initiative. Am. J. Med. 2020, 133, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Almodaimegh, H.; Alfehaid, L.; Alsuhebany, N.; Bustami, R.; Alharbi, S.; Alkatheri, A.; Albekairy, A. Awareness of Venous Thromboembolism and Thromboprophylaxis among Hospitalized Patients: A Cross-Sectional Study. Thromb. J. 2017, 15, 19. [Google Scholar] [CrossRef]
- Engbers, M.J.; van Hylckama Vlieg, A.; Rosendaal, F.R. Venous Thrombosis in the Elderly: Incidence, Risk Factors and Risk Groups. J. Thromb. Haemost. 2010, 8, 2105–2112. [Google Scholar] [CrossRef] [PubMed]
- Khalafallah, A.A.; Kirkby, B.E.; Wong, S.; Foong, Y.C.; Ranjan, N.; Luttrell, J.; Mathew, R.; Chilvers, C.M.; Mauldon, E.; Sharp, C.; et al. Venous Thromboembolism in Medical Patients during Hospitalisation and 3 Months after Hospitalisation: A Prospective Observational Study. BMJ Open 2016, 6, e012346. [Google Scholar] [CrossRef]
- Ambra, N.; Mohammad, O.H.; Naushad, V.A.; Purayil, N.K.; Mohamedali, M.G.; Elzouki, A.N.; Khalid, M.K.; Illahi, M.N.; Palol, A.; Barman, M.; et al. Venous Thromboembolism Among Hospitalized Patients: Incidence and Adequacy of Thromboprophylaxis—A Retrospective Study. Vasc. Health Risk Manag. 2022, 18, 575–587. [Google Scholar] [CrossRef]
- Alexander, P.; Visagan, S.; Issa, R.; Gorantla, V.R.; Thomas, S.E. Current Trends in the Duration of Anticoagulant Therapy for Venous Thromboembolism: A Systematic Review. Cureus 2021, 13, e18992. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Majeed, A.; Powell, R. Heparin Induced Thrombocytopenia: Diagnosis and Management Update. Postgrad. Med. J. 2007, 83, 575–582. [Google Scholar] [CrossRef]
- Skeik, N.; Westergard, E. Recommendations for VTE Prophylaxis in Medically Ill Patients. Ann. Vasc. Dis. 2020, 13, 38–44. [Google Scholar] [CrossRef]
- Klok, F.A.; Kooiman, J.; Huisman, M.V.; Konstantinides, S.; Lankeit, M. Predicting Anticoagulant-Related Bleeding in Patients with Venous Thromboembolism: A Clinically Oriented Review. Eur. Respir. J. 2015, 45, 201–210. [Google Scholar] [CrossRef]
- Du, G.-C.; Zhang, M.-C.; Zhao, J.-C. Catheter-Directed Thrombolysis plus Anticoagulation versus Anticoagulation Alone in the Treatment of Proximal Deep Vein Thrombosis—A Meta-Analysis. Vasa 2015, 44, 0195–0202. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Kim, D.H.; il Kim, D.; Kim, H.-Y.; Lee, S.S.; Jung, H.J. Comparison of Treatment Result Between Anticoagulation Alone and Catheter-Directed Thrombolysis Plus Anticoagulation in Acute Lower Extremity Deep Vein Thrombosis. Vasc. Spec. Int. 2019, 35, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Palareti, G. Recurrent Venous Thromboembolism: What Is the Risk and How to Prevent It. Scientifica 2012, 2012, 391734. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Tan, J.; Deng, Y.; Hua, L.; Guo, T. Clinical and Safety Outcomes Associated with Extended Treatment of Venous Thromboembolism: A Network Meta-Analysis. J. Cardiovasc. Dev. Dis. 2022, 9, 414. [Google Scholar] [CrossRef]
| Provoked | Unprovoked | |||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Frequency | 29 | 92 | 195 | 567 |
| Percentage | 24.0 | 76.0 | 25.6 | 74.4 |
| Mean age ± SD | 44.7 ± 20.4 | 40.5 ± 16.3 | 43.3 ± 17.5 | 43.0 ± 16.5 |
| p-value | 0.103 | 0.592 | 0.241 | 0.765 |
| Frequency | Percent | |
|---|---|---|
| Family History | ||
| +ve | 47 | 5.3 |
| -ve | 836 | 94.5 |
| Patient Hospitalized | ||
| Yes | 188 | 21.2 |
| No | 695 | 78.7 |
| Duration of Hospitalization | ||
| ≤3 days | 56 | 6.3 |
| 3–7 days | 77 | 8.7 |
| 7–10 days | 22 | 2.5 |
| ≥10 days | 33 | 3.7 |
| Disease Outcome | ||
| Improved and Discharged | 790 | 89.3 |
| Died | 93 | 10.6 |
| Admitted to ICU | ||
| Yes | 16 | 1.8 |
| No | 867 | 98.2 |
| Management Strategy | N | % | ||
|---|---|---|---|---|
| Thrombolytic therapy | 188 | 21.7% | ||
| Catheter-directed thrombolysis | 54 | 6.2% | ||
| Anticoagulation therapy | Initial and maintenance | 626 | 72.1% | |
| Initiation anticoagulation therapy | LMWH-unfractionated heparin | 37 | 5.9% | |
| factor Xa inhibitor | 69 | 11% | ||
| oral anticoagulants | 167 | 26.9% | ||
| LMWH | 175 | 27.9% | ||
| combination of two or three therapeutic options | 178 | 28.4% | ||
| Maintenance anticoagulation therapy | factor Xa inhibitor | 90 | 14.3% | |
| oral anticoagulants | 98 | 15,6% | ||
| warfarin | 145 | 23.1% | ||
| direct thrombin inhibitor | 62 | 9.9% | ||
| combination therapy | 232 | 37.1% | ||
| Follow-Up after Treatment | N | % | |
|---|---|---|---|
| Duration of treatment | 3 months | 123 | 19.7% |
| 6 months | 227 | 36.2% | |
| 12 months | 131 | 20.7% | |
| Long-term treatment | 146 | 23.3% | |
| Adherence | Did not adhere to treatment | 548 | 87.6% |
| Adhered to treatment | 78 | 12.4% | |
| Recurrence | 500 | 79.9% | |
| Independent Variable | Coefficient | Odds Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|---|
| Thrombolytic Therapy | −0.47 | 0.62 | (0.41, 0.93) | 0.02 |
| Catheter-directed thrombolysis | −0.36 | 0.69 | (0.48, 0.99) | 0.04 |
| Anticoagulation Therapy | 0.25 | 1.28 | (1.08, 1.52) | 0.007 |
| Oral anticoagulant | 0.51 | 1.67 | (1.12, 2.49) | 0.003 |
| Vitamin K antagonist (warfarin) | 0.63 | 1.88 | (1.26, 2.80) | 0.001 |
| Factor Xa inhibitor (rivaroxiban) | 0.32 | 1.37 | (0.92, 2.04) | 0.01 |
| Direct thrombin inhibitor (dabigatran) | −0.08 | 0.92 | (0.52, 1.63) | 0.05 |
| Combination therapy | −0.17 | 0.85 | (0.46, 1.56) | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bakhsh, E.; Shaban, M.; Al Subaie, S.; Al Moshary, M.; AlSheef, M. Exploring the Clinical Efficacy of Venous Thromboembolism Management in Saudi Arabian Hospitals: An Insight into Patient Outcomes. J. Pers. Med. 2023, 13, 612. https://doi.org/10.3390/jpm13040612
Bakhsh E, Shaban M, Al Subaie S, Al Moshary M, AlSheef M. Exploring the Clinical Efficacy of Venous Thromboembolism Management in Saudi Arabian Hospitals: An Insight into Patient Outcomes. Journal of Personalized Medicine. 2023; 13(4):612. https://doi.org/10.3390/jpm13040612
Chicago/Turabian StyleBakhsh, Ebtisam, Mostafa Shaban, Sarah Al Subaie, May Al Moshary, and Mohammed AlSheef. 2023. "Exploring the Clinical Efficacy of Venous Thromboembolism Management in Saudi Arabian Hospitals: An Insight into Patient Outcomes" Journal of Personalized Medicine 13, no. 4: 612. https://doi.org/10.3390/jpm13040612
APA StyleBakhsh, E., Shaban, M., Al Subaie, S., Al Moshary, M., & AlSheef, M. (2023). Exploring the Clinical Efficacy of Venous Thromboembolism Management in Saudi Arabian Hospitals: An Insight into Patient Outcomes. Journal of Personalized Medicine, 13(4), 612. https://doi.org/10.3390/jpm13040612







