Voiding Dysfunction Due to Urethral Sphincter Dysfunction Might Be an Early Neurological Presentation of Central Nervous System Disorders in Aged Patients
Abstract
:1. Introduction
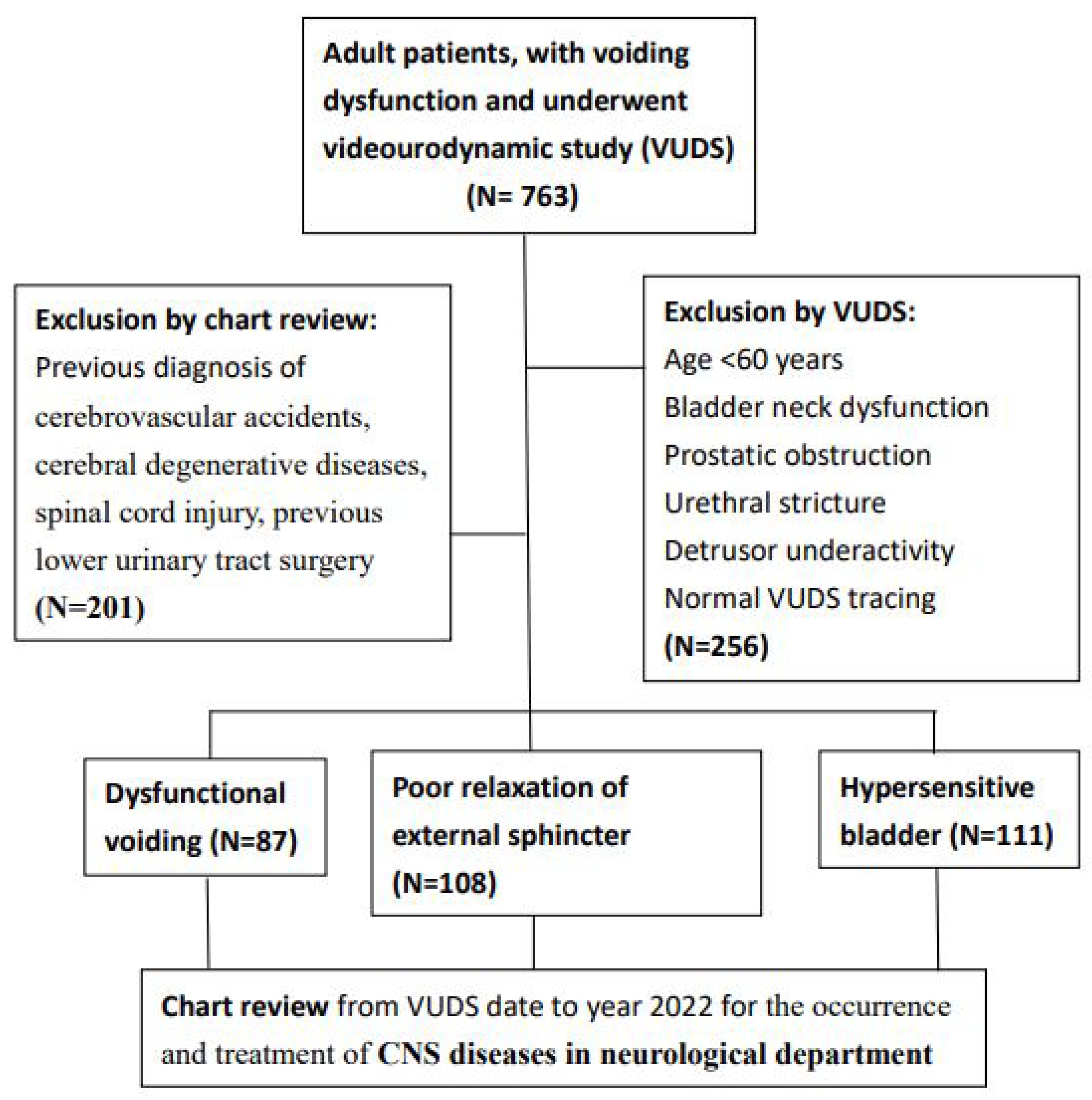
2. Materials and Methods
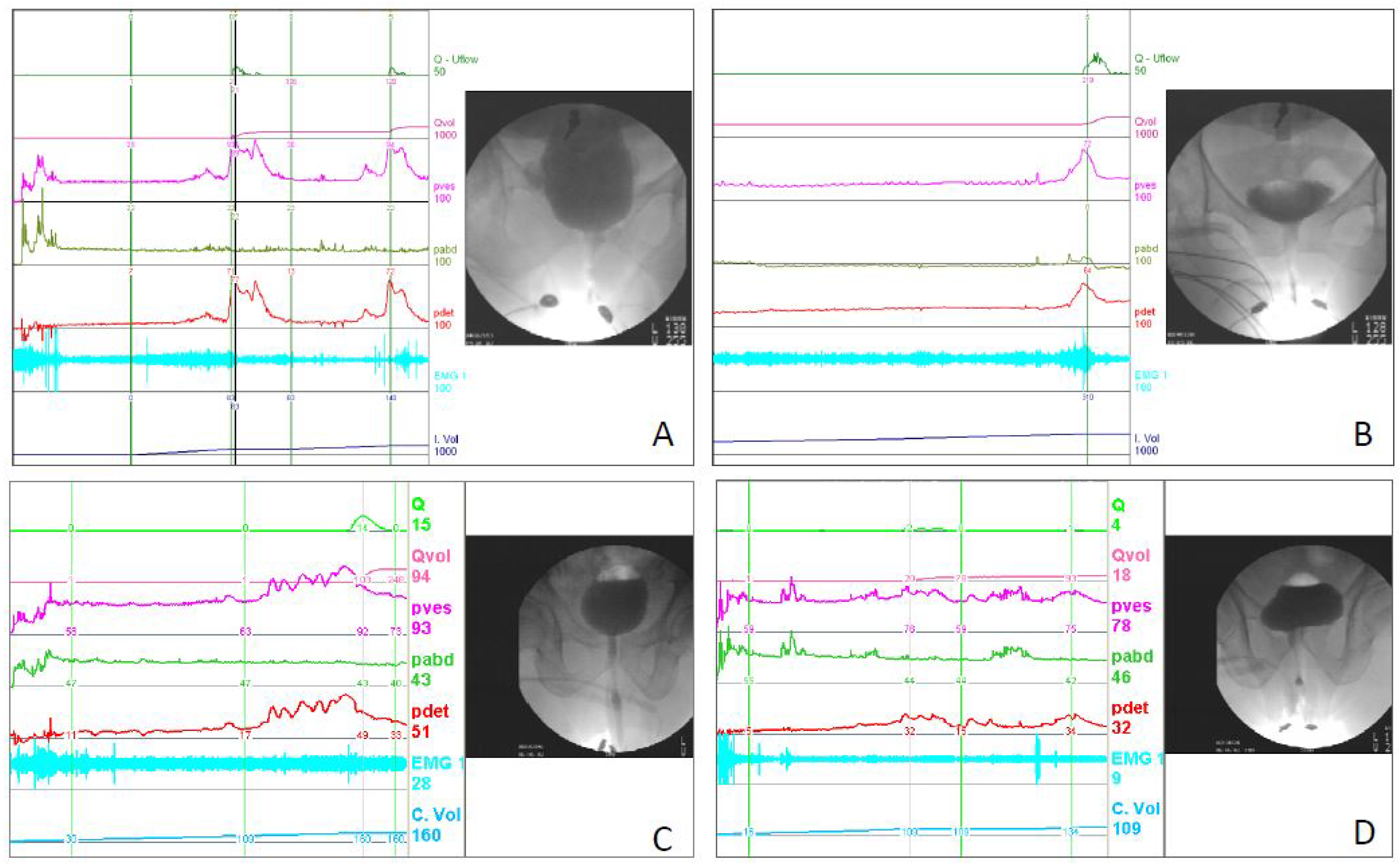
3. Videourodynamic Study
4. Statistical Analyses
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A. Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: Report. from the standardisation sub-committee of the International Continence Society. Urology 2003, 61, 37–49. [Google Scholar] [PubMed]
- Haylen, B.T.; de Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. International Urogynecological Association, International Continence Society. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol. Urodyn. 2010, 29, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Sinha, S. Dysfunctional voiding: A review of the terminology, presentation, evaluation and management in children and adults. Indian J. Urol. 2011, 27, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, S.M.; Lin, H.H.; Kuo, H.C. Videourodynamic studies of women with voiding dysfunction. Sci. Rep. 2017, 7, 6845. [Google Scholar] [CrossRef]
- Minardi, D.; d’Anzeo, G.; Parri, G.; Polito, M., Jr.; Piergallina, M.; El Asmar, Z.; Marchetti, M.; Muzzonigro, G. The role of uroflowmetry biofeedback and biofeedback training of the pelvic floor muscles in the treatment of recurrent urinary tract infections in women with dysfunctional voiding: A randomized controlled prospective study. Urology 2010, 75, 1299–1304. [Google Scholar] [CrossRef]
- Chiang, C.H.; Jiang, Y.H.; Kuo, H.C. Therapeutic efficacy of biofeedback pelvic floor muscle exercise in women with dysfunctional voiding. Sci. Rep. 2021, 11, 13757. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.H.; Jan, H.C.; Kuo, H.C.; Kao, Y.L.; Tsai, K.J. Therapeutic Efficacy of Urethral Sphincteric Botulinum Toxin Injections for Female Sphincter Dysfunctions and a Search for Predictive Factors. Toxins 2021, 13, 398. [Google Scholar]
- Akkoc, Y.; Ersoz, M.; Yuceyar, N. Neurogenic Bladder Turkish Research, G. Overactive bladder symptoms in patients with multiple sclerosis: Frequency, severity, diagnosis and treatment. J. Spinal Cord. Med. 2016, 39, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Araki, I.; Kitahara, M.; Oida, T.; Kuno, S. Voiding dysfunction and Parkinson’s disease: Urodynamic abnormalities and urinary symptoms. J. Urol. 2000, 164, 1640–1643. [Google Scholar] [CrossRef]
- Ransmayr, G.N.; Holliger, S.; Schletterer, K.; Heidler, H.; Deibl, M.; Poewe, W.; Madersbacher, H.; Kiss, G. Lower urinary tract symptoms in dementia with Lewy bodies, Parkinson disease, and Alzheimer disease. Neurology 2008, 70, 299–303. [Google Scholar] [CrossRef]
- Asche, C.V.; Kim, J.; Kulkarni, A.S.; Chakravarti, P.; Andersson, K.E. Presence of central nervous system, cardiovascular and overall co-morbidity burden in patients with overactive bladder disorder in a real-world setting. BJU Int. 2012, 109, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.J.; Weng, S.F.; Yang, C.M.; Wu, M.P. Risk of hospitalization for acute cardiovascular events among subjects with lower urinary tract symptoms: A nationwide population-based study. PLoS ONE 2013, 8, e66661. [Google Scholar] [CrossRef] [PubMed]
- Newman, A.B.; Fitzpatrick, A.L.; Lopez, O.; Jackson, S.; Lyketsos, C.; Jagust, W.; Ives, D.; Dekosky, S.T.; Kuller, L.H. Dementia and Alzheimer’s disease incidence in relationship to cardiovascular disease in the Cardiovascular Health Study cohort. J. Am. Geriatr. Soc. 2005, 53, 1101–1107. [Google Scholar] [CrossRef] [PubMed]
- Allen, C.L.; Bayraktutan, U. Risk factors for ischaemic stroke. Int. J. Stroke 2008, 3, 105–116. [Google Scholar] [CrossRef]
- Chiang, C.H.; Wu, M.P.; Ho, C.H.; Weng, S.F.; Huang, C.C.; Hsieh, W.T.; Hsu, Y.W.; Chen, P.J. Lower Urinary Tract Symptoms Are Associated with Increased Risk of Dementia among the Elderly: A Nationwide Study. Biomed. Res. Int. 2015, 2015, 187819. [Google Scholar] [CrossRef]
- Liao, C.C.; Li, T.C.; Lin, R.S.; Sung, F.C. Urban and Rural Difference in Prevalence and Incidence of Stroke in 2000 in Taiwan. Taiwan J. Public Health 2006, 25, 223–230. [Google Scholar]
- Homma, Y. Hypersensitive bladder: A solution to confused terminology and ignorance concerning interstitial cystitis. Int. J. Urol. 2014, 21 (Suppl. S1), 43–47. [Google Scholar] [CrossRef]
- Hu, H.H.; Sheng, W.Y.; Chu, F.L.; Lan, C.F.; Chiang, B.N. Incidence of stroke in Taiwan. Stroke 1992, 23, 1237–1241. [Google Scholar] [CrossRef]
- Tsai, C.F.; Wang, Y.H.; Teng, N.C.; Yip, P.K.; Chen, L.K. Incidence, subtypes, sex differences and trends of stroke in Taiwan. PLoS ONE 2022, 17, e0277296. [Google Scholar] [CrossRef]
- Feigin, V.L.; Lawes, C.M.; Bennett, D.A.; Anderson, C.S. Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003, 2, 43–53. [Google Scholar] [CrossRef]
- Chen, R.C.; Chang, S.F.; Su, C.L.; Chen, T.H.; Yen, M.F.; Wu, H.M.; Chen, Z.Y.; Liou, H.H. Prevalence, incidence, and mortality of PD: A door-to-door survey in Ilan county, Taiwan. Neurology 2001, 57, 1679–1686. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.C.; Li, C.Y.; Lee, P.C.; Sun, Y. Variations in Incidence and Prevalence of Parkinson’s Disease in Taiwan: A Population-Based Nationwide Study. Parkinsons Dis. 2016, 2016, 8756359. [Google Scholar] [CrossRef] [PubMed]
- Willis, A.W.; Roberts, E.; Beck, J.C.; Fiske, B.; Ross, W.; Savica, R.; Van Den Eeden, S.K.; Tanner, C.M.; Marras, C. Parkinson’s Foundation P4 Group. Incidence of Parkinson disease in North America. NPJ Parkinsons Dis. 2022, 8, 170. [Google Scholar] [CrossRef]
- Fowler, C.J.; Griffiths, D.; de Groat, W.C. The neural control of micturition. Nat. Rev. Neurosci. 2008, 9, 453–466. [Google Scholar] [CrossRef]
- Deindl, F.M.; Vodusek, D.B.; Bischoff, C.; Hofmann, R.; Hartung, R. Dysfunctional voiding in women: Which muscles are responsible? Br. J. Urol. 1998, 82, 814–819. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, O.; Yoshiyama, M.; Namiki, M.; de Groat, W.C. Changes in dopaminergic and glutamatergic excitatory mechanisms of micturition reflex after middle cerebral artery occlusion in conscious rats. Exp. Neurol. 2002, 173, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, O.; Yotsuyanagi, S.; Akino, H.; Moriyama, H.; Matsuta, Y.; Namiki, M. RNA synthesis in pons necessary for maintenance of bladder overactivity after cerebral infarction in rat. J. Urol. 2003, 169, 1878–1884. [Google Scholar] [CrossRef]
- Chen, Y.C.; Kuo, H.C. Clinical and video urodynamic characteristics of adult women with dysfunctional voiding. J. Formos. Med. Assoc. 2014, 113, 161–165. [Google Scholar] [CrossRef]
- Brittain, K.R.; Peet, S.M.; Castleden, C.M. Stroke and incontinence. Stroke 1998, 29, 524–528. [Google Scholar] [CrossRef]
- Pavlakis, A.J.; Siroky, M.B.; Goldstein, I.; Krane, R.J. Neurourologic findings in Parkinson’s disease. J. Urol. 1983, 129, 80–83. [Google Scholar] [CrossRef]
- Galloway, N.T. Urethral sphincter abnormalities in Parkinsonism. Br. J. Urol. 1983, 55, 691–693. [Google Scholar] [CrossRef] [PubMed]
- Sakakibara, R.; Panicker, J.; Finazzi-Agro, E.; Iacovelli, V.; Bruschini, H. Parkinson’s Disease Subcomittee, The Neurourology Promotion Committee in The International Continence Society. A guideline for the management of bladder dysfunction in Parkinson’s disease and other gait disorders. Neurourol. Urodyn. 2016, 35, 551–563. [Google Scholar] [CrossRef]
- Cai, W.; Zhang, K.; Li, P.; Zhu, L.; Xu, J.; Yang, B.; Hu, X.; Lu, Z.; Chen, J. Dysfunction of the neurovascular unit in ischemic stroke and neurodegenerative diseases: An aging effect. Ageing Res. Rev. 2017, 34, 77–87. [Google Scholar] [CrossRef]
- Murray, C.J.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global Burden of Diseases, Injuries, and Risk Factors Study 2010 (GBD 2010) and the GBD Stroke Experts Group. Lancet 2014, 383, 245–254. [Google Scholar] [CrossRef]
- Sherzai, A.Z.; Elkind, M.S. Advances in stroke prevention. Ann. N. Y. Acad. Sci. 2015, 1338, 1–15. [Google Scholar] [CrossRef]
- Lee, M.; Saver, J.L.; Hong, K.S.; Hao, Q.; Ovbiagele, B. Does achieving an intensive versus usual blood pressure level prevent stroke? Ann. Neurol. 2012, 71, 133–140. [Google Scholar] [CrossRef]
- Everaert, K.; Van Laecke, E.; De Muynck, M.; Peeters, H.; Hoebeke, P. Urodynamic assessment of voiding dysfunction and dysfunctional voiding in girls and women. Int. Urogynecol. J. Pelvic Floor. Dysfunct. 2000, 11, 254–264. [Google Scholar] [CrossRef]
- Jiang, Y.H.; Chen, S.F.; Kuo, H.C. Role of videourodynamic study in precision diagnosis and treatment for lower urinary tract dysfunction. Ci Ji Yi Xue Za Zhi 2020, 32, 121–130. [Google Scholar]
| All (n = 306) | DV (n = 87) | PRES (n = 108) | HSB (n = 111) | p Value | |
|---|---|---|---|---|---|
| Age | 69.7 ± 6.9 | 71.9 ± 7.6 | 69.9 ± 6.7 | 67.8 ± 5.9 | p < 0.001 |
| Male gender | 69 (22.5%) | 28 (32.2%) | 34 (31.5%) | 7 (6.3%) | p < 0.001 |
| Hypertension | 154 (50.3%) | 45 (51.7%) | 62 (57.4%) | 47 (42.3%) | p = 0.061 |
| Diabetes | 86 (28.1%) | 31 (35.6%) | 31 (28.7%) | 24 (21.6%) | p = 0.113 |
| Dyslipidemia | 92 (30.1%) | 24 (27.6%) | 32 (29.6%) | 36 (32.4%) | p = 0.771 |
| Constipation | 79 (25.8%) | 24 (27.6%) | 34 (31.5%) | 21 (18.9%) | p = 0.087 |
| BMI > 24 | 97 (31.7%) | 32 (36.8%) | 33 (30.6%) | 32 (28.8%) | p = 0.382 |
| Urodynamic DO | 90 (29.4%) | 56 (66.7%) | 25 (23.1%) | 9 (8.1%) | p < 0.001 |
| DV (n = 87) | PRES (n = 108) | HSB (n = 111) | Total (n = 306) | |
|---|---|---|---|---|
| CNS diseases | 16 (18.4%) | 12 (11.1%) | 8 (7.2%) | 36 (11.8%) |
| CVA | 11 (12.6%) | 8 (7.4%) | 4 (3.6%) | 23 (7.5%) |
| Dementia | 2 (2.3%) | 3 (2.8%) | 4 (3.6%) | 9 (2.9%) |
| PD | 3 (3.5%) | 1 (1.0%) | 0 | 4 (1.3%) |
| DV (n = 16) | PRES (n = 12) | HSB (n = 8) | Total (n = 36) | p | Post Hoc | |
|---|---|---|---|---|---|---|
| PVR (mL) | 211 ± 222 | 163 ± 191 | 100 ± 80.2 | 171 ± 189 | 0.405 | |
| FSF (mL) | 141 ± 59.2 | 151 ± 64.0 | 147 ± 66.4 | 146 ± 60.8 | 0.909 | |
| FS (mL) | 207 ± 109 | 279 ± 121 | 237 ± 66.4 | 238 ± 108 | 0.220 | |
| US (mL) | 234 ± 126 | 338 ± 142 | 325 ± 107 | 289 ± 134 | 0.084 | |
| Compliance | 54.3 ± 64.8 | 65.4 ± 53.2 | 118 ± 118 | 72.2 ± 78.3 | 0.159 | |
| Pdet (cmH2O) | 35.4 ± 19.6 | 17.5 ± 10.3 | 18.8 ± 9 | 25.7 ± 17.0 | 0.006 | DV vs. PRES |
| DO | 8 (50.0%) | 4 (33.3%) | 0 | 12 (33.3%) | 0.064 | |
| Qmax (mL/s) | 6.91 ± 4.68 | 5.67 ± 4.31 | 14 ± 9.44 | 8.1 ± 6.6 | 0.010 | DV/PRES |
| Volume (mL) | 167 ± 130 | 168 ± 163 | 312 ± 114 | 200 ± 148 | 0.047 | |
| CBC (mL) | 379 ± 185 | 332 ± 170 | 412 ± 77.3 | 370 ± 161 | 0.538 | |
| cQmax | 0.38 ± 0.26 | 0.31 ± 0.22 | 0.69 ± 0.46 | 0.43 ± 0.33 | 0.026 | PRES vs. HSB |
| BCI | 69.9 ± 31.7 | 45.8 ± 28.3 | 88.8 ± 46.6 | 66.1 ± 37.2 | 0.030 | PRES vs. HSB |
| VE | 0.49 ± 0.37 | 0.52 ± 0.44 | 0.75 ± 0.2 | 0.56 ± 0.37 | 0.274 | |
| BOOI | 21.6 ± 21.0 | 6.17 ± 9.40 | −9.25 ± 22.2 | 9.58 ± 21.6 | 0.002 | DV vs. HSB |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, G.-R.; Wei, C.-W.; Kuo, H.-C. Voiding Dysfunction Due to Urethral Sphincter Dysfunction Might Be an Early Neurological Presentation of Central Nervous System Disorders in Aged Patients. J. Pers. Med. 2023, 13, 693. https://doi.org/10.3390/jpm13040693
Ho G-R, Wei C-W, Kuo H-C. Voiding Dysfunction Due to Urethral Sphincter Dysfunction Might Be an Early Neurological Presentation of Central Nervous System Disorders in Aged Patients. Journal of Personalized Medicine. 2023; 13(4):693. https://doi.org/10.3390/jpm13040693
Chicago/Turabian StyleHo, Guan-Ru, Chiao-Wen Wei, and Hann-Chorng Kuo. 2023. "Voiding Dysfunction Due to Urethral Sphincter Dysfunction Might Be an Early Neurological Presentation of Central Nervous System Disorders in Aged Patients" Journal of Personalized Medicine 13, no. 4: 693. https://doi.org/10.3390/jpm13040693
APA StyleHo, G.-R., Wei, C.-W., & Kuo, H.-C. (2023). Voiding Dysfunction Due to Urethral Sphincter Dysfunction Might Be an Early Neurological Presentation of Central Nervous System Disorders in Aged Patients. Journal of Personalized Medicine, 13(4), 693. https://doi.org/10.3390/jpm13040693







