The Changing Environment in Postgraduate Education in Orthopedic Surgery and Neurosurgery and Its Impact on Technology-Driven Targeted Interventional and Surgical Pain Management: Perspectives from Europe, Latin America, Asia, and The United States
Abstract
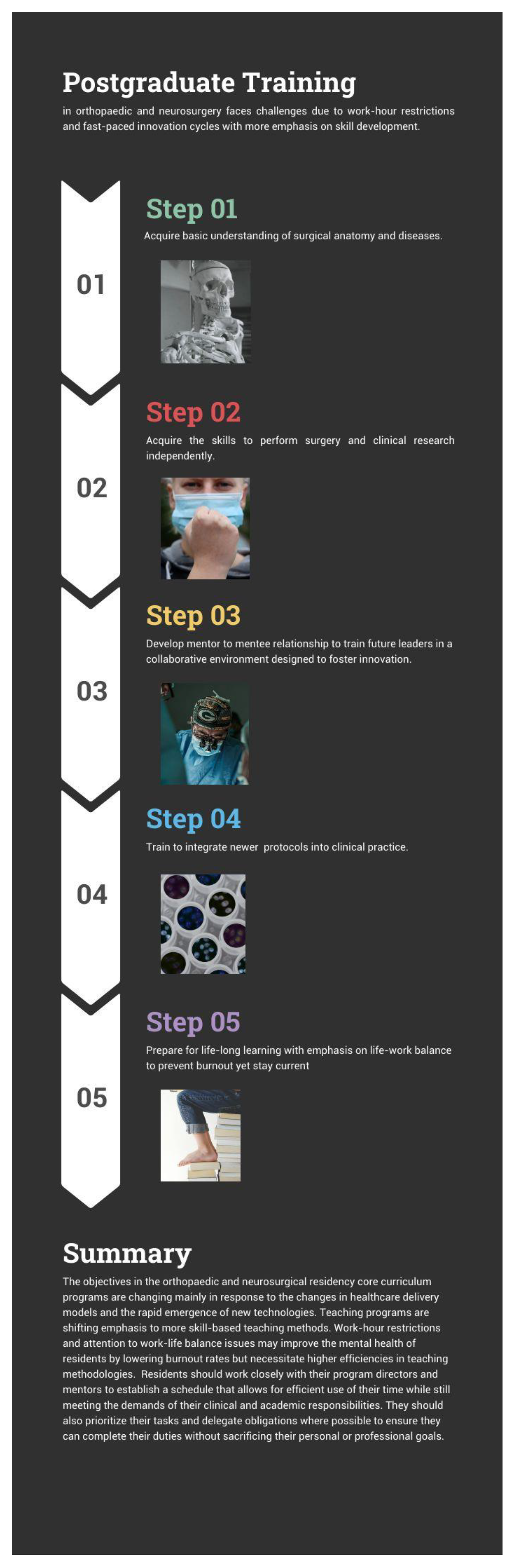
:1. Introduction
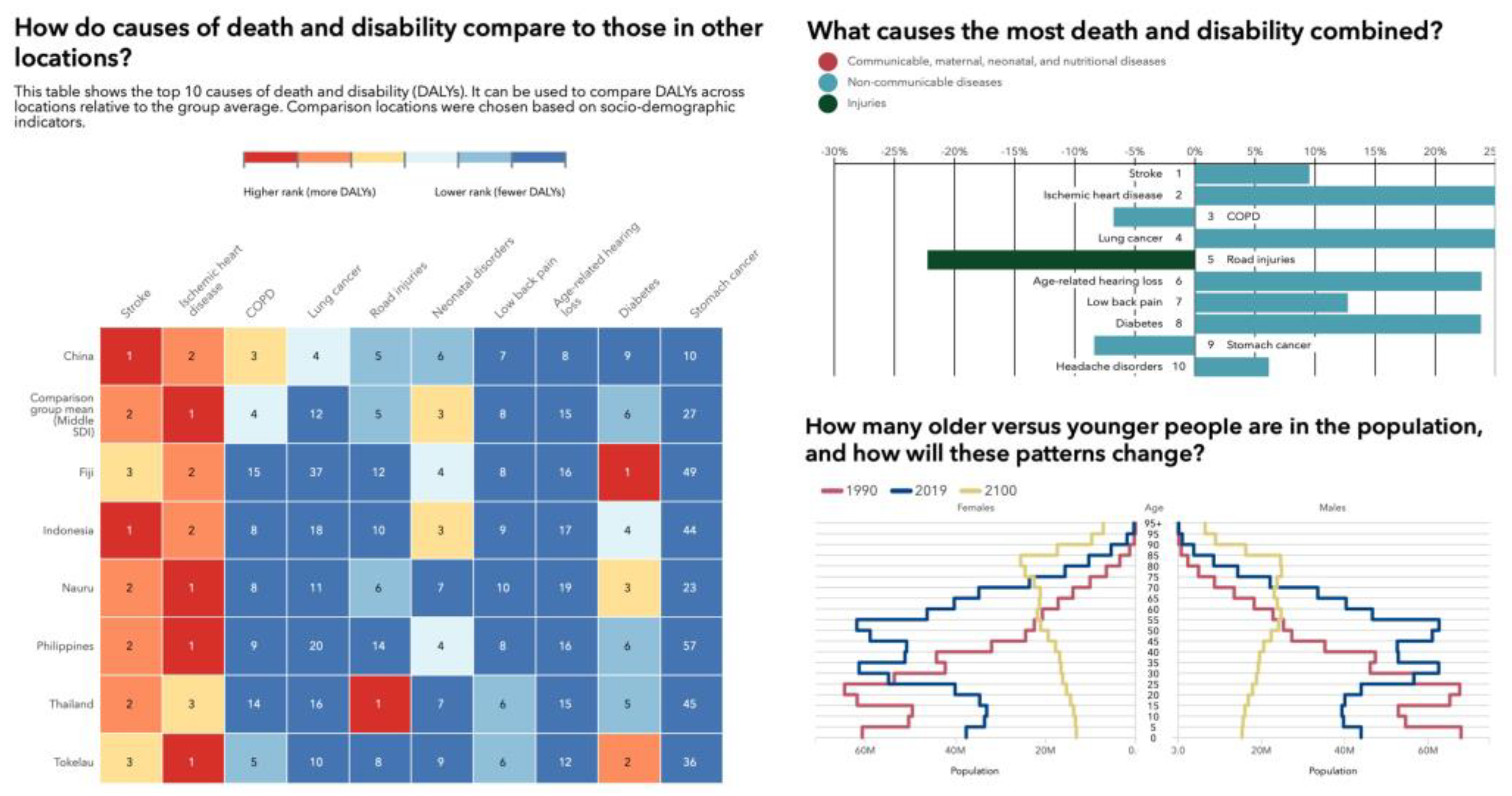
2. Shifting Trends
3. The Residents’ Perspective
4. The Mentors Perspective
5. Work-Hour Restrictions
6. Examples of Slow Adoption in Postgraduate Training
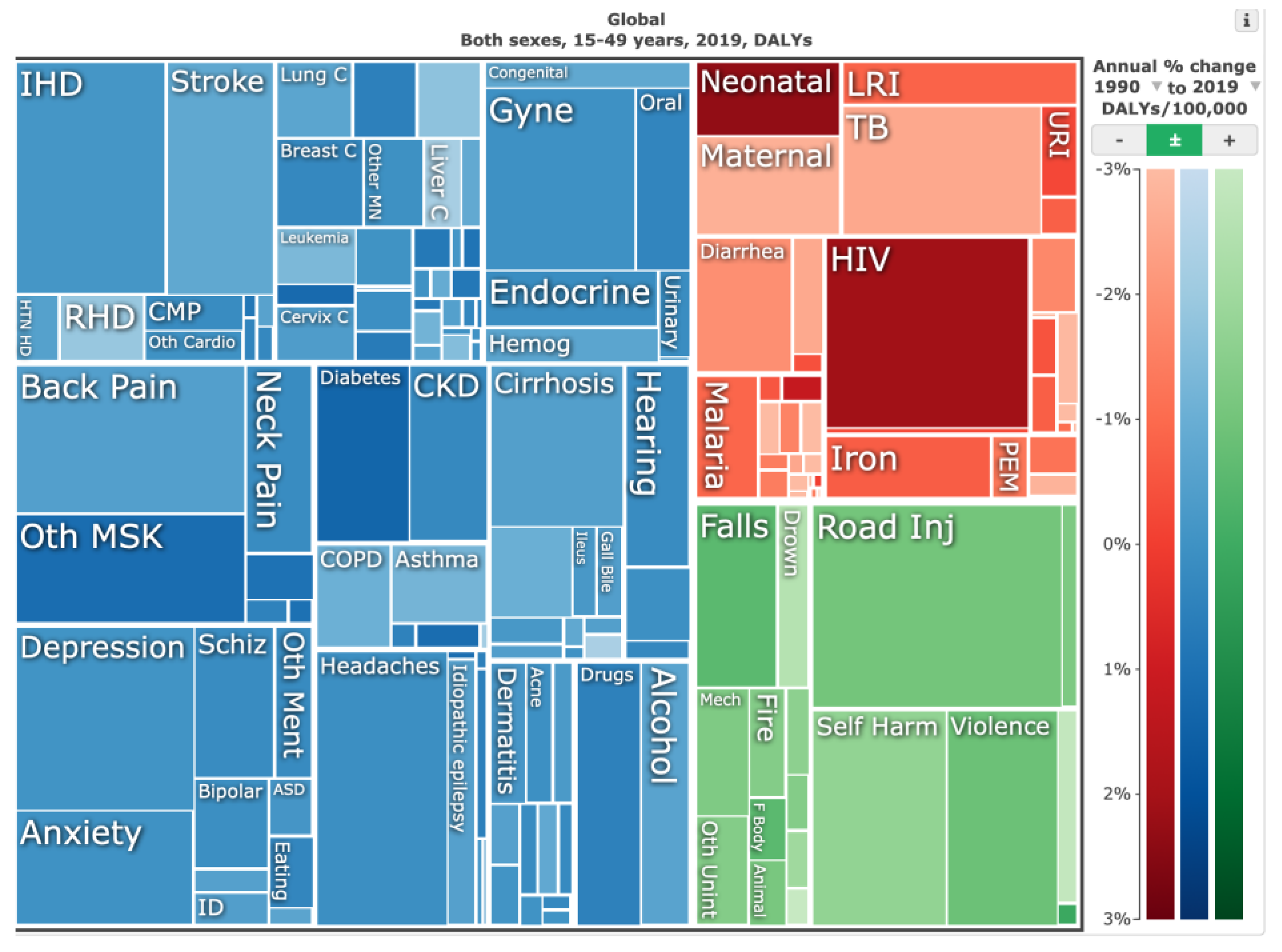
7. Resident Clinical Research and Solutions
8. Impact of Transformative Technologies and Targeted Care Models
9. Discussion
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Brien, B.C.; Forrest, K.; Wijnen-Meijer, M.; ten Cate, O. A global view of structures and trends in medical education. In Understanding Medical Education: Evidence, Theory, and Practice; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2018; pp. 7–22. [Google Scholar]
- Alman, B.A.; Ferguson, P.; Kraemer, W.; Nousiainen, M.T.; Reznick, R.K. 49: Competency-based education: A new model for teaching orthopaedics. Instr. Course Lect. 2013, 62, 565–570. [Google Scholar]
- Harris, K.A.; Nousiainen, M.T.; Reznick, R. Competency-based resident education—The Canadian perspective. Surgery 2020, 167, 681–684. [Google Scholar] [CrossRef] [PubMed]
- Nousiainen, M.; McQueen, S.; Hall, J.; Kraemer, W.; Ferguson, P.; Marsh, J.; Reznick, R.; Reed, M.; Sonnadara, R. Resident education in orthopaedic trauma: The future role of competency-based medical education. Bone Jt. J. 2016, 98, 1320–1325. [Google Scholar] [CrossRef]
- Nousiainen, M.T.; McQueen, S.A.; Ferguson, P.; Alman, B.; Kraemer, W.; Safir, O.; Reznick, R.; Sonnadara, R. Simulation for teaching orthopaedic residents in a competency-based curriculum: Do the benefits justify the increased costs? Clin. Orthop. Relat. Res. 2016, 474, 935–944. [Google Scholar] [CrossRef]
- Nousiainen, M.T.; Mironova, P.; Hynes, M.; Glover Takahashi, S.; Reznick, R.; Kraemer, W.; Alman, B.; Ferguson, P.; CBC Planning Committee. Eight-year outcomes of a competency-based residency training program in orthopedic surgery. Med. Teach. 2018, 40, 1042–1054. [Google Scholar] [CrossRef]
- Sonnadara, R.R.; Mui, C.; McQueen, S.; Mironova, P.; Nousiainen, M.; Safir, O.; Kraemer, W.; Ferguson, P.; Alman, B.; Reznick, R. Reflections on competency-based education and training for surgical residents. J. Surg. Educ. 2014, 71, 151–158. [Google Scholar] [CrossRef]
- Van Heest, A.E.; Armstrong, A.D.; Bednar, M.S.; Carpenter, J.E.; Garvin, K.L.; Harrast, J.J.; Martin, D.F.; Murray, P.M.; Peabody, T.D.; Saltzman, C.L. American Board of Orthopaedic Surgery’s Initiatives toward Competency-Based Education. JBJS Open Access 2022, 7, e21. [Google Scholar] [CrossRef]
- Choules, A. The use of elearning in medical education: A review of the current situation. Postgrad. Med. J. 2007, 83, 212–216. [Google Scholar] [CrossRef]
- Harden, R. Trends and the future of postgraduate medical education. Emerg. Med. J. 2006, 23, 798–802. [Google Scholar] [CrossRef]
- Teo, A. The current state of medical education in Japan: A system under reform. Med. Educ. 2007, 41, 302–308. [Google Scholar] [CrossRef]
- Bhashyam, A.R.; Dyer, G.S. “Virtual” boot camp: Orthopaedic intern education in the time of COVID-19 and beyond. JAAOS-J. Am. Acad. Orthop. Surg. 2020, 28, e735–e743. [Google Scholar] [CrossRef] [PubMed]
- Bostrom, M.P.; Lewis, K.O.; Berger, G. The role of electronic learning in orthopaedic graduate medical training: A consensus from leaders in orthopaedic training programs. JAAOS-J. Am. Acad. Orthop. Surg. 2021, 29, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Mun, F.; Suresh, K.V.; Pollak, A.N.; Morris, C.D. Professional Society Opportunities and Involvement for Early-Career Orthopaedic Surgeons. JAAOS-J. Am. Acad. Orthop. Surg. 2022, 31, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.; Clough, M. The Internet and the Orthopaedic Surgeon. In The Internet for Orthopaedists; Springer: Cham, Switzerland, 2003; pp. 50–62. [Google Scholar]
- Rogers, M.J.; Zeidan, M.; Flinders, Z.S.; Presson, A.P.; Burks, R. Educational resource utilization by current orthopaedic surgical residents: A nation-wide survey. JAAOS Glob. Res. Rev. 2019, 3, e041. [Google Scholar] [CrossRef]
- Chhabra, H.S.; Bagaraia, V.; Keny, S.; Kalidindi, K.K.V.; Mallepally, A.; Dhillon, M.S.; Malhotra, R.; Rajasekharan, S. COVID-19: Current knowledge and best practices for orthopaedic surgeons. Indian J. Orthop. 2020, 54, 411–425. [Google Scholar] [CrossRef]
- Dattani, R.; Morgan, C.; Li, L.; Bennett-Brown, K.; Wharton, R.M. The impact of COVID-19 on the future of orthopaedic training in the UK. Acta Orthop. 2020, 91, 627–632. [Google Scholar] [CrossRef]
- Hardie, J.; Green, G.; Bor, R.; Brennan, P. Cutting edge selection: Learning from high reliability organisations for virtual recruitment in surgery during the COVID-19 pandemic. Ann. R. Coll. Surg. Engl. 2021, 103, 385–389. [Google Scholar] [CrossRef]
- Kogan, M.; Klein, S.E.; Hannon, C.P.; Nolte, M.T. Orthopaedic education during the COVID-19 pandemic. J. Am. Acad. Orthop. Surg. 2020, 28, e456–e464. [Google Scholar] [CrossRef]
- Aïm, F.; Lonjon, G.; Hannouche, D.; Nizard, R. Effectiveness of virtual reality training in orthopaedic surgery. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 224–232. [Google Scholar] [CrossRef]
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A. Virtual reality, augmented reality, gamification, and telerehabilitation: Psychological impact on orthopedic patients’ rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef]
- Iyengar, K.P.; Jain, V.K.; Vaishya, R. Virtual postgraduate orthopaedic practical examination: A pilot model. Postgrad. Med. J. 2021, 97, 650–654. [Google Scholar] [PubMed]
- Kamarudin, M.F.B.; Zary, N. Augmented Reality, Virtual Reality and Mixed Reality in Medical Education: A Comparative Web of Science Scoping Review. 2019. Available online: https://www.semanticscholar.org/paper/Augmented-Reality%2C-Virtual-Reality-and-Mixed-in-A-Kamarudin-Zary/dba7a6a58f96f6ffffe18975c1e106a8d5467c1c (accessed on 15 April 2023).
- Jayakumar, P.; Moore, M.L.; Bozic, K.J. Value-based healthcare: Can artificial intelligence provide value in orthopaedic surgery? Clin. Orthop. Relat. Res. 2019, 477, 1777. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.G.; Ramkumar, P.N.; Ricciardi, B.F.; Urish, K.L.; Kipper, J.; Ketonis, C. Artificial intelligence and orthopaedics: An introduction for clinicians. J. Bone Jt. Surgery. Am. 2020, 102, 830–840. [Google Scholar] [CrossRef]
- St Mart, J.-P.; Goh, E.L.; Liew, I.; Shah, Z.; Sinha, J. Artificial intelligence in orthopaedics surgery: Transforming technological innovation in patient care and surgical training. Postgrad. Med. J. 2022; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Gardner, A.K.; Scott, D.J.; Pedowitz, R.A.; Sweet, R.M.; Feins, R.H.; Deutsch, E.S.; Sachdeva, A.K. Best practices across surgical specialties relating to simulation-based training. Surgery 2015, 158, 1395–1402. [Google Scholar] [CrossRef]
- Milburn, J.; Khera, G.; Hornby, S.; Malone, P.; Fitzgerald, J. Introduction, availability and role of simulation in surgical education and training: Review of current evidence and recommendations from the Association of Surgeons in Training. Int. J. Surg. 2012, 10, 393–398. [Google Scholar] [CrossRef]
- Pedowitz, R.A.; Marsh, L.J. Motor skills training in orthopaedic surgery: A paradigm shift toward a simulation-based educational curriculum. JAAOS-J. Am. Acad. Orthop. Surg. 2012, 20, 407–409. [Google Scholar] [CrossRef]
- Hollenbeck, S.M.; Bomar, J.D.; Wenger, D.R.; Yaszay, B. Electronic medical record adoption: The effect on efficiency, completeness, and accuracy in an academic orthopaedic practice. J. Pediatr. Orthop. 2017, 37, 424–428. [Google Scholar] [CrossRef]
- Scott, D.J.; Labro, E.; Penrose, C.T.; Bolognesi, M.P.; Wellman, S.S.; Mather III, R.C. The impact of electronic medical record implementation on labor cost and productivity at an outpatient orthopaedic clinic. JBJS 2018, 100, 1549–1556. [Google Scholar] [CrossRef]
- Shaha, J.S.; El-Othmani, M.M.; Saleh, J.K.; Bozic, K.J.; Wright, J.; Tokish, J.M.; Shaha, S.H.; Saleh, K.J. The growing gap in electronic medical record satisfaction between clinicians and information technology professionals: Issues of most concern and suggested remediations. JBJS 2015, 97, 1979–1984. [Google Scholar] [CrossRef]
- Syed, S.; Mirza, A.H.; Ali, A. A brief comparison of orthopaedic training in English-speaking countries. Ann. R. Coll. Surg. Engl. 2009, 91, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, J.; Giddings, C.; Khera, G.; Marron, C. Improving the Future of Surgical Training and Education: Consensus Recommendations from the Association of Surgeons in Training; Elsevier: Amsterdam, The Netherlands, 2012; Volume 10, pp. 389–392. [Google Scholar]
- Fritz, T.; Stachel, N.; Braun, B.J. Evidence in surgical training—A review. Innov. Surg. Sci. 2019, 4, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Stienen, M.N.; Freyschlag, C.F.; Schaller, K.; Meling, T. Procedures performed during neurosurgery residency in Europe. Acta Neurochir 2020, 162, 2303–2311. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, B.W.; Oertel, J.M.; Hendrix, P. Neurosurgical procedures performed during residency in Europe—Preliminary numbers and time trends. Acta Neurochir 2019, 161, 1975–1976. [Google Scholar] [CrossRef]
- Stienen, M.N.; Bartek, J., Jr.; Czabanka, M.A.; Freyschlag, C.F.; Kolias, A.; Krieg, S.M.; Moojen, W.; Renovanz, M.; Sampron, N.; Adib, S.D.; et al. Response to: Neurosurgical procedures performed during residency in Europe-preliminary numbers and time trends. Acta Neurochir 2019, 161, 1977–1979. [Google Scholar] [CrossRef]
- Tarifeinigung zum TV-Ärzte: Neue Vorgaben zur Arbeitszeit, Zusatzurlaub und Entgelterhöhungen. Available online: https://www.marburger-bund.de/bundesverband/tarifpolitik/tarifeinigung-zum-tv-aerzte-neue-vorgaben-zur-arbeitszeit-zusatzurlaub (accessed on 15 April 2023).
- Murguia-Fuentes, R.; Husein, N.; Vega, A.; Rangel-Castilla, L.; Rotta, J.M.; Quinones-Hinojosa, A.; Guinto, G.; Esquenazi, Y. Neurosurgical residency training in Latin America: Current status, challenges, and future opportunities. World Neurosurg. 2018, 120, e1079–e1097. [Google Scholar] [CrossRef]
- Beltrán, J.Q.; Ogando-Rivas, E.; Nettel-Rueda, B.; Velasco-Campos, F.; Navarro-Olvera, J.L.; Aguado-Carrillo, G.; Soriano-Sanchez, J.A.; Alpizar-Aguirre, A.; Carrillo-Ruiz, J.D. Women in neurosurgery: First neurosurgeon in Latin America and current Mexican leaders. World Neurosurg. 2021, 150, 114–120. [Google Scholar] [CrossRef]
- Zanon, N.; Niquen-Jimenez, M.; Kim, E.E.; Zegarra, A.B.; Ramírez-Reyes, A.G.; Quiroga, D.P.; Molina, E.I.M.; Santana, N.V.; Garcia, R.M.; Rosseau, G. Progress in neurosurgery: Contributions of women neurosurgeons in Latin America. J. Clin. Neurosci. 2021, 86, 347–356. [Google Scholar] [CrossRef]
- Rasouli, J.J.; Shin, J.H.; Than, K.D.; Gibbs, W.N.; Baum, G.R.; Baaj, A.A. Virtual spine: A novel, international teleconferencing program developed to increase the accessibility of spine education during the COVID-19 pandemic. World Neurosurg. 2020, 140, e367–e372. [Google Scholar] [CrossRef]
- Hussein, A.; Bauer, I.; Cavagnaro, M.; Farhadi, D.S.; Prim, M.; Baaj, A.; Orenday, J.M. Virtual learning in Neurosurgery During the COVID-19 Pandemic, A Systematic Literature Review. Pan Arab J. Neurosurg. 2022, 17, 3–8. [Google Scholar] [CrossRef]
- Drossard, S. Structured surgical residency training in Germany: An overview of existing training programs in 10 surgical subspecialties. Innov. Surg. Sci. 2019, 4, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Görgen, J. Berufswechsel als Arzt: Viele Wählen Alternative Berufsfelder. Available online: https://www.praktischarzt.ch/arzt/berufswechsel-als-arzt-viele-waehlen-alternative-berufsfelder/ (accessed on 6 March 2023).
- Marwan, Y.; Luo, L.; Toobaie, A.; Benaroch, T.; Snell, L. Operating Room Educational Environment in Canada: Perceptions of Surgical Residents. J. Surg. Educ. 2021, 78, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Oladeji, L.O.; Ponce, B.A.; Worley, J.R.; Keeney, J.A. Mentorship in Orthopedics: A National Survey of Orthopedic Surgery Residents. J. Surg. Educ. 2018, 75, 1606–1614. [Google Scholar] [CrossRef] [PubMed]
- Bartoletta, J.J.; Hinchcliff, K.; Rhee, P. Learner Preferences and Perceptions of Virtual Hand Surgery Education during the COVID-19 Pandemic. J. Hand Surg. Am. 2021, 48, 405.e1–405.e8. [Google Scholar] [CrossRef] [PubMed]
- Brook, E.M.; Hu, C.H.; Li, X.; Smith, E.L.; Matzkin, E.G. The influence of mentors in orthopedic surgery. Orthopedics 2020, 43, e37–e42. [Google Scholar] [CrossRef] [PubMed]
- Flint, J.H.; Jahangir, A.A.; Browner, B.D.; Mehta, S. The value of mentorship in orthopaedic surgery resident education: The residents’ perspective. J. Bone Jt. Surg. Am. 2009, 91, 1017–1022. [Google Scholar] [CrossRef]
- Hart, R.A.; Eltorai, A.E.M.; Yanney, K.; Marsh, J.L.; Mulcahey, M.K.; Daniels, A.H. Update on Mentorship in Orthopaedic Resident Education: A Report from the American Orthopaedic Association. J. Bone Jt. Surg. Am. 2020, 102, e20. [Google Scholar] [CrossRef]
- Winfrey, S.R.; Parameswaran, P.; Gerull, K.M.; LaPorte, D.; Cipriano, C.A. Effective Mentorship of Women and Underrepresented Minorities in Orthopaedic Surgery: A Mixed-Methods Investigation. JB JS Open Access 2022, 7, e22.00053. [Google Scholar] [CrossRef]
- Choo, K.J.; Arora, V.M.; Barach, P.; Johnson, J.K.; Farnan, J.M. How do supervising physicians decide to entrust residents with unsupervised tasks? A qualitative analysis. J. Hosp. Med. 2014, 9, 169–175. [Google Scholar] [CrossRef]
- Fabricant, P.D.; Dy, C.J.; Dare, D.M.; Bostrom, M.P. A narrative review of surgical resident duty hour limits: Where do we go from here? J. Grad. Med. Educ. 2013, 5, 19–24. [Google Scholar] [CrossRef]
- Akhigbe, T.; Zolnourian, A.; Bulters, D. Mentoring models in neurosurgical training: Review of literature. J. Clin. Neurosci. 2017, 45, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Mulcahey, M.K.; Waterman, B.R.; Hart, R.; Daniels, A.H. The role of mentoring in the development of successful orthopaedic surgeons. JAAOS-J. Am. Acad. Orthop. Surg. 2018, 26, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef]
- Bailit, J.L.; Weisberger, A.; Knotek, J. Resident job satisfaction and quality of life before and after work hour reform. J. Reprod. Med. 2005, 50, 649–652. [Google Scholar] [PubMed]
- Jena, A.B.; Farid, M.; Blumenthal, D.; Bhattacharya, J. Association of residency work hour reform with long term quality and costs of care of US physicians: Observational study. Bmj 2019, 366, l4134. [Google Scholar] [CrossRef]
- Whang, E.E.; Perez, A.; Ito, H.; Mello, M.M.; Ashley, S.W.; Zinner, M.J. Work hours reform: Perceptions and desires of contemporary surgical residents. J. Am. Coll. Surg. 2003, 197, 624–630. [Google Scholar] [CrossRef]
- Ransom, N.A.; Gollogly, S.; Lewandrowski, K.U.; Yeung, A. Navigating the learning curve of spinal endoscopy as an established traditionally trained spine surgeon. J. Spine Surg. 2020, 6 (Suppl. 1), S197–S207. [Google Scholar] [CrossRef]
- Huber, M. Zürcher Assistenzärzte kündigen den Gesamtarbeitsvertrag. Sie wollen pro Woche acht Stunden weniger arbeiten—Aber ist das realistisch? Neue Zürcher Zeitung. 2023. Available online: https://www.nzz.ch/zuerich/belastung-von-assistenzaerzten-42-statt-50-wochenstunden-verlangt-ld.1733149?reduced=true (accessed on 3 May 2023).
- Reulen, H.J.; März, U. 5 years’ experience with a structured operative training programme for neurosurgical residents. Acta Neurochir 1998, 140, 1197–1203. [Google Scholar] [CrossRef]
- Friedlaender, G.E. The 80-hour duty week: Rationale, early attitudes, and future questions. Clin. Orthop. Relat. Res. 2006, 449, 138–142. [Google Scholar] [CrossRef]
- Jeray, K.J.; Frick, S.L. A survey of resident perspectives on surgical case minimums and the impact on milestones, graduation, credentialing, and preparation for practice: AOA critical issues. J. Bone Jt. Surg. Am. 2014, 96, e195. [Google Scholar] [CrossRef]
- Hopmans, C.J.; den Hoed, P.T.; van der Laan, L.; van der Harst, E.; van der Elst, M.; Mannaerts, G.H.; Dawson, I.; Timman, R.; Wijnhoven, B.P.; JN, I.J. Impact of the European Working Time Directive (EWTD) on the operative experience of surgery residents. Surgery 2015, 157, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman, J.D.; Kubiak, E.N.; Immerman, I.; Dicesare, P. The early effects of code 405 work rules on attitudes of orthopaedic residents and attending surgeons. J. Bone Jt. Surg. Am. 2005, 87, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.T.-Y.; Ling, S.K.-K.; Wong, R.M.-Y.; Ho, K.K.-W.; Chow, S.K.-H.; Cheung, L.W.-H.; Yung, P.S.-H. Impact of COVID-19 on orthopaedic clinical service, education and research in a university hospital. J. Orthop. Transl. 2020, 25, 125–127. [Google Scholar] [CrossRef]
- Sugano, N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin. Orthop. Surg. 2013, 5, 1–9. [Google Scholar] [CrossRef]
- Zhang, Q.; Han, X.G.; Xu, Y.F.; Fan, M.X.; Zhao, J.W.; Liu, Y.J.; He, D.; Tian, W. Robotic navigation during spine surgery. Expert Rev. Med. Devices 2020, 17, 27–32. [Google Scholar] [CrossRef]
- McAfee, P.C.; Lieberman, I.H.; Theodore, N. Innovations in Robotics and Navigation, Part 2. Int. J. Spine Surg. 2022, 16 (Suppl. 2), S6–S7. [Google Scholar] [CrossRef] [PubMed]
- Mezger, U.; Jendrewski, C.; Bartels, M. Navigation in surgery. Langenbecks Arch. Surg. 2013, 398, 501–514. [Google Scholar] [CrossRef]
- Karkenny, A.J.; Mendelis, J.R.; Geller, D.S.; Gomez, J.A. The Role of Intraoperative Navigation in Orthopaedic Surgery. J. Am. Acad. Orthop. Surg. 2019, 27, e849–e858. [Google Scholar] [CrossRef]
- Kochanski, R.B.; Lombardi, J.M.; Laratta, J.L.; Lehman, R.A.; O’Toole, J.E. Image-Guided Navigation and Robotics in Spine Surgery. Neurosurgery 2019, 84, 1179–1189. [Google Scholar] [CrossRef]
- Huang, M.; Tetreault, T.A.; Vaishnav, A.; York, P.J.; Staub, B.N. The current state of navigation in robotic spine surgery. Ann. Transl. Med. 2021, 9, 86. [Google Scholar] [CrossRef]
- Hagan, M.J.; Remacle, T.; Leary, O.P.; Feler, J.; Shaaya, E.; Ali, R.; Zheng, B.; Bajaj, A.; Traupe, E.; Kraus, M.; et al. Navigation Techniques in Endoscopic Spine Surgery. Biomed. Res. Int. 2022, 2022, 8419739. [Google Scholar] [CrossRef] [PubMed]
- Hersh, A.; Mahapatra, S.; Weber-Levine, C.; Awosika, T.; Theodore, J.N.; Zakaria, H.M.; Liu, A.; Witham, T.F.; Theodore, N. Augmented Reality in Spine Surgery: A Narrative Review. HSS J. 2021, 17, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Uddin, S.A.; Hanna, G.; Ross, L.; Molina, C.; Urakov, T.; Johnson, P.; Kim, T.; Drazin, D. Augmented Reality in Spinal Surgery: Highlights From Augmented Reality Lectures at the Emerging Technologies Annual Meetings. Cureus 2021, 13, e19165. [Google Scholar] [CrossRef] [PubMed]
- Van Gestel, F.; Frantz, T.; Soomro, M.H.; Elprama, S.A.; Vannerom, C.; Jacobs, A.; Vandemeulebroucke, J.; Jansen, B.; Scheerlinck, T.; Duerinck, J. Augmented Reality-Assisted Neurosurgical Drain Placement (ARANED): Technical Note. Acta Neurochir Suppl. 2021, 131, 267–273. [Google Scholar]
- Yuk, F.J.; Maragkos, G.A.; Sato, K.; Steinberger, J. Current innovation in virtual and augmented reality in spine surgery. Ann. Transl. Med. 2021, 9, 94. [Google Scholar] [CrossRef]
- Panchmatia, J.R.; Visenio, M.R.; Panch, T. The role of artificial intelligence in orthopaedic surgery. Br. J. Hosp. Med. 2018, 79, 676–681. [Google Scholar] [CrossRef]
- Langerhuizen, D.W.G.; Janssen, S.J.; Mallee, W.H.; van den Bekerom, M.P.J.; Ring, D.; Kerkhoffs, G.; Jaarsma, R.L.; Doornberg, J.N. What Are the Applications and Limitations of Artificial Intelligence for Fracture Detection and Classification in Orthopaedic Trauma Imaging? A Systematic Review. Clin. Orthop. Relat. Res. 2019, 477, 2482–2491. [Google Scholar] [CrossRef]
- Loftus, T.J.; Tighe, P.J.; Filiberto, A.C.; Efron, P.A.; Brakenridge, S.C.; Mohr, A.M.; Rashidi, P.; Upchurch, G.R., Jr.; Bihorac, A. Artificial Intelligence and Surgical Decision-making. JAMA Surg. 2020, 155, 148–158. [Google Scholar] [CrossRef]
- D’Antoni, F.; Russo, F.; Ambrosio, L.; Vollero, L.; Vadalà, G.; Merone, M.; Papalia, R.; Denaro, V. Artificial Intelligence and Computer Vision in Low Back Pain: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 10909. [Google Scholar] [CrossRef]
- Martin, R.K.; Ley, C.; Pareek, A.; Groll, A.; Tischer, T.; Seil, R. Artificial intelligence and machine learning: An introduction for orthopaedic surgeons. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 361–364. [Google Scholar] [CrossRef]
- Rohde, S.; Münnich, N. [Artificial intelligence in orthopaedic and trauma surgery imaging]. Orthopadie 2022, 51, 748–756. [Google Scholar] [PubMed]
- Cai, H.; Liu, Z.; Wei, F.; Yu, M.; Xu, N.; Li, Z. 3D Printing in Spine Surgery. Adv. Exp. Med. Biol. 2018, 1093, 345–359. [Google Scholar] [PubMed]
- Hasan, O.; Atif, M.; Jessar, M.M.; Hashmi, P. Application of 3D printing in orthopaedic surgery. A new affordable horizon for cost-conscious care. J. Pak. Med. Assoc. 2019, 69 (Suppl. 1), S46–S50. [Google Scholar]
- Zamborsky, R.; Kilian, M.; Jacko, P.; Bernadic, M.; Hudak, R. Perspectives of 3D printing technology in orthopaedic surgery. Bratisl. Lek. Listy 2019, 120, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.P.; McHale, K.J.; Parvizi, J.; Mehta, S. Nanotechnology: Current concepts in orthopaedic surgery and future directions. Bone Jt. J. 2014, 96, 569–573. [Google Scholar] [CrossRef]
- Viswanathan, V.K.; Rajaram Manoharan, S.R.; Subramanian, S.; Moon, A. Nanotechnology in Spine Surgery: A Current Update and Critical Review of the Literature. World Neurosurg. 2019, 123, 142–155. [Google Scholar] [CrossRef]
- Samsonraj, R.M.; Raghunath, M.; Nurcombe, V.; Hui, J.H.; van Wijnen, A.J.; Cool, S.M. Concise Review: Multifaceted Characterization of Human Mesenchymal Stem Cells for Use in Regenerative Medicine. Stem. Cells Transl. Med. 2017, 6, 2173–2185. [Google Scholar] [CrossRef]
- Matai, I.; Kaur, G.; Seyedsalehi, A.; McClinton, A.; Laurencin, C.T. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials 2020, 226, 119536. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, G.; Johnson, B.N.; Jia, X. Three-dimensional (3D) printed scaffold and material selection for bone repair. Acta Biomater. 2019, 84, 16–33. [Google Scholar] [CrossRef]
- Thomas, C.N.; Mavrommatis, S.; Schroder, L.K.; Cole, P.A. An overview of 3D printing and the orthopaedic application of patient-specific models in malunion surgery. Injury 2022, 53, 977–983. [Google Scholar] [CrossRef]
- Suresh, D.; Aydin, A.; James, S.; Ahmed, K.; Dasgupta, P. The Role of Augmented Reality in Surgical Training: A Systematic Review. Surg. Innov. 2022, 2022, 15533506221140506. [Google Scholar] [CrossRef] [PubMed]
- Tarrant, S.A.; Behzadpour, V.; McCormack, T.J.; Cline, J.A.; Willis, J.T.; Mendez, G.M.; Zackula, R.E.; Dart, B.R.; Hearon, B.F. Improving Medical Student Mentorship in Orthopaedic Surgery. Kans. J. Med. 2023, 16, 48–52. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewandrowski, K.-U.; Elfar, J.C.; Li, Z.-M.; Burkhardt, B.W.; Lorio, M.P.; Winkler, P.A.; Oertel, J.M.; Telfeian, A.E.; Dowling, Á.; Vargas, R.A.A.; et al. The Changing Environment in Postgraduate Education in Orthopedic Surgery and Neurosurgery and Its Impact on Technology-Driven Targeted Interventional and Surgical Pain Management: Perspectives from Europe, Latin America, Asia, and The United States. J. Pers. Med. 2023, 13, 852. https://doi.org/10.3390/jpm13050852
Lewandrowski K-U, Elfar JC, Li Z-M, Burkhardt BW, Lorio MP, Winkler PA, Oertel JM, Telfeian AE, Dowling Á, Vargas RAA, et al. The Changing Environment in Postgraduate Education in Orthopedic Surgery and Neurosurgery and Its Impact on Technology-Driven Targeted Interventional and Surgical Pain Management: Perspectives from Europe, Latin America, Asia, and The United States. Journal of Personalized Medicine. 2023; 13(5):852. https://doi.org/10.3390/jpm13050852
Chicago/Turabian StyleLewandrowski, Kai-Uwe, John C. Elfar, Zong-Ming Li, Benedikt W. Burkhardt, Morgan P. Lorio, Peter A. Winkler, Joachim M. Oertel, Albert E. Telfeian, Álvaro Dowling, Roth A. A. Vargas, and et al. 2023. "The Changing Environment in Postgraduate Education in Orthopedic Surgery and Neurosurgery and Its Impact on Technology-Driven Targeted Interventional and Surgical Pain Management: Perspectives from Europe, Latin America, Asia, and The United States" Journal of Personalized Medicine 13, no. 5: 852. https://doi.org/10.3390/jpm13050852
APA StyleLewandrowski, K.-U., Elfar, J. C., Li, Z.-M., Burkhardt, B. W., Lorio, M. P., Winkler, P. A., Oertel, J. M., Telfeian, A. E., Dowling, Á., Vargas, R. A. A., Ramina, R., Abraham, I., Assefi, M., Yang, H., Zhang, X., Ramírez León, J. F., Fiorelli, R. K. A., Pereira, M. G., de Carvalho, P. S. T., ... Novellino, P. (2023). The Changing Environment in Postgraduate Education in Orthopedic Surgery and Neurosurgery and Its Impact on Technology-Driven Targeted Interventional and Surgical Pain Management: Perspectives from Europe, Latin America, Asia, and The United States. Journal of Personalized Medicine, 13(5), 852. https://doi.org/10.3390/jpm13050852













