Cost-Effectiveness Analysis of Personalized Hypertension Prevention
Abstract
:1. Introduction
2. Materials and Methods
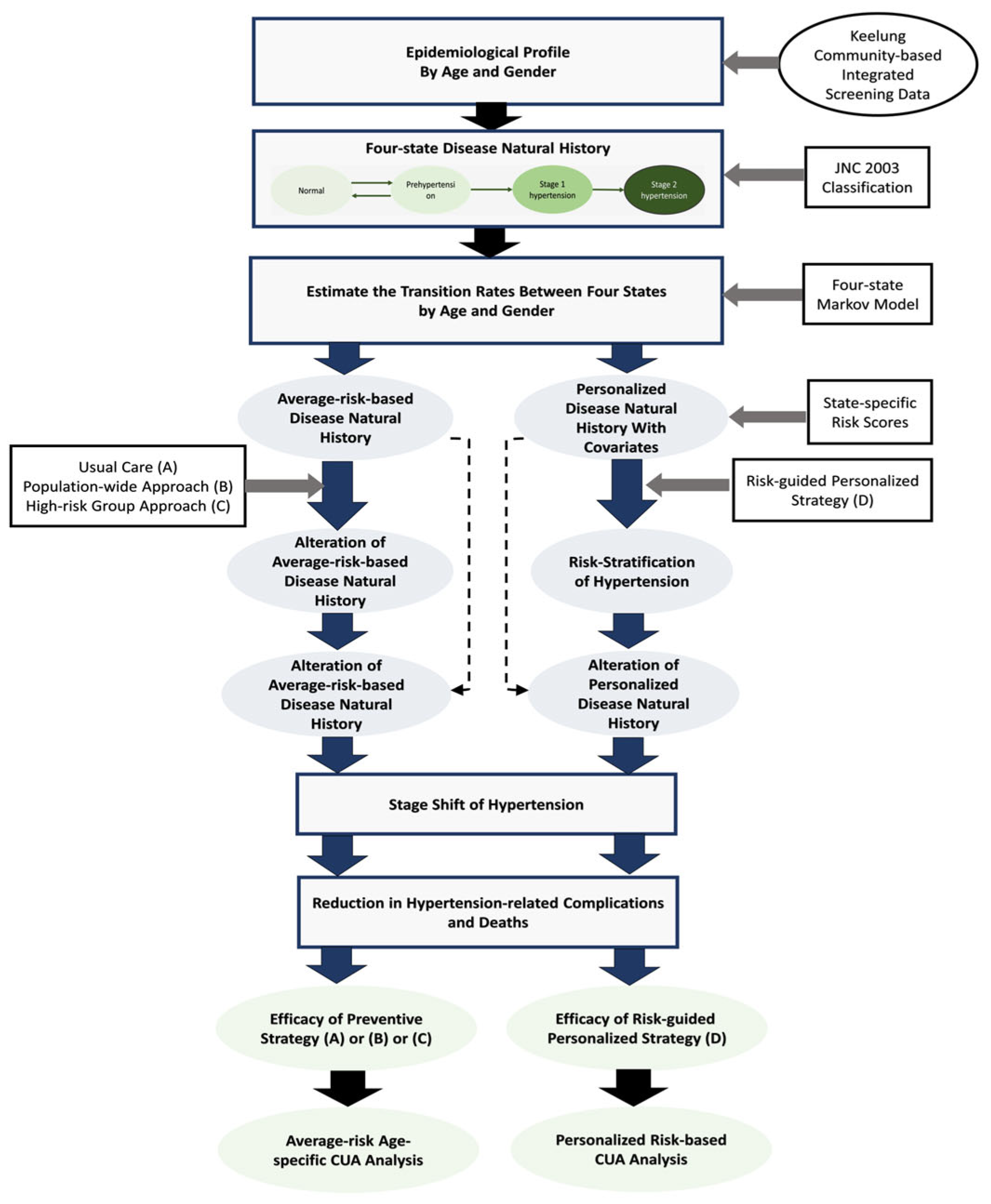
2.1. Study Framework
2.2. State-Specific Risk Scores
2.3. Markov Decision Model
 ) was defined in the Markov cycle with a one-year follow-up for one cycle. The final states were denoted as terminal nodes (◁) after the simulation.
) was defined in the Markov cycle with a one-year follow-up for one cycle. The final states were denoted as terminal nodes (◁) after the simulation.2.4. Cost-Utility Analysis
3. Results
4. Discussion
4.1. Methodological Aspects during the Economic Appraisal of Preventive Strategies for Hypertension
4.2. Natural History of Hypertension for an Average-Risk-Based Population and a Personalized-Risk-Based Population
4.3. Economical Aspecst of the Universal and Personalized Prevention Strategies for Hypertension
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tseng, C.D.; Yen, A.M.; Chiu, S.Y.; Chen, L.S.; Chen, H.H.; Chang, S.H. A predictive model for risk of prehypertension and hypertension and expected benefit after population-based life-style modification (KCIS No. 24). Am. J. Hypertens. 2012, 25, 171–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, Y.H.; Wu, S.C.; Tseng, C.D.; Yen, M.F.; Chen, T.H. Progression of pre-hypertension, stage 1 and 2 hypertension (JNC 7): A population-based study in Keelung, Taiwan (Keelung Community-based Integrated Screening No. 9). J. Hypertens. 2006, 24, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Daugherty, S.L.; Masoudi, F.A.; Ellis, J.L.; Ho, P.M.; Schmittdiel, J.A.; Tavel, H.M.; Selby, J.V.; O’Connor, P.J.; Margolis, K.L.; Magid, D.J. Age-dependent gender differences in hypertension management. J. Hypertens. 2011, 29, 1005–1011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moran, A.E.; Odden, M.C.; Thanataveerat, A.; Tzong, K.Y.; Rasmussen, P.W.; Guzman, D.; Williams, L.; Bibbins-Domingo, K.; Coxson, P.G.; Goldman, L. Cost-effectiveness of hypertension therapy according to 2014 guidelines. N. Engl. J. Med. 2015, 372, 447–455. [Google Scholar] [CrossRef] [Green Version]
- Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 2001, 30, 427–432. [Google Scholar] [CrossRef] [Green Version]
- Zhang, D.; Wang, G.; Joo, H. A Systematic Review of Economic Evidence on Community Hypertension Interventions. Am. J. Prev. Med. 2017, 53, S121–S130. [Google Scholar] [CrossRef] [Green Version]
- Schorling, E.; Niebuhr, D.; Kroke, A. Cost-effectiveness of salt reduction to prevent hypertension and CVD: A systematic review. Public. Health Nutr. 2017, 20, 1993–2003. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, T.P.; Wright, E.P.; Nguyen, T.T.; Schuiling-Veninga, C.C.; Bijlsma, M.J.; Nguyen, T.B.; Postma, M.J. Cost-Effectiveness Analysis of Screening for and Managing Identified Hypertension for Cardiovascular Disease Prevention in Vietnam. PLoS ONE 2016, 11, e0155699. [Google Scholar] [CrossRef] [Green Version]
- Rosendaal, N.T.; Hendriks, M.E.; Verhagen, M.D.; Bolarinwa, O.A.; Sanya, E.O.; Kolo, P.M.; Adenusi, P.; Agbede, K.; van Eck, D.; Tan, S.S.; et al. Costs and Cost-Effectiveness of Hypertension Screening and Treatment in Adults with Hypertension in Rural Nigeria in the Context of a Health Insurance Program. PLoS ONE 2016, 11, e0157925. [Google Scholar] [CrossRef] [Green Version]
- Bautista, L.E.; Vera-Cala, L.M.; Ferrante, D.; Herrera, V.M.; Miranda, J.J.; Pichardo, R.; Abanto, J.R.S.; Ferreccio, C.; Silva, E.; Arenas, M.O.; et al. A ‘polypill’ aimed at preventing cardiovascular disease could prove highly cost-effective for use in Latin America. Health Aff. 2013, 32, 155–164. [Google Scholar] [CrossRef] [Green Version]
- Khonputsa, P.; Veerman, L.J.; Bertram, M.; Lim, S.S.; Chaiyakunnaphruk, N.; Vos, T. Generalised Cost-Effectiveness analysis of pharmaceutical interventions for primary prevention of Cardiovascular disease in Thailand. Value Health Reg. Issues 2012, 1, 15–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaziano Thomas, A.; Bertram, M.; Tollman, S.M.; Hofman, K.J. Hypertension education and adherence in South Africa: A cost-effectiveness analysis of community health workers. BMC Public Health 2014, 14, 240. [Google Scholar]
- Kostova, D.; Spencer, G.; Moran, A.E.; Cobb, L.K.; Husain, M.J.; Datta, B.K.; Matsushita, K.; Nugent, R. The cost-effectiveness of hypertension management in low-income and middle-income countries: A review. BMJ Glob. Health 2020, 5, e002213. [Google Scholar] [CrossRef] [PubMed]
- Aminde, L.N.; Takah, N.F.; Zapata-Diomedi, B.; Veerman, J.L. Primary and secondary prevention interventions for cardiovascular disease in low-income and middle-income countries: A systematic review of economic evaluations. Cost. Eff. Resour. Alloc. 2018, 14, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- JNC 7 Express. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; U.S. Department of Health and Human Services; NIH Publication: Rockville, MD, USA, 2003. [Google Scholar]
- Yen, A.M.; Chen, T.H. Kinetic epidemiological model for elucidating sexual difference of hypertension (KCIS no.20). J. Eval. Clin. Pract. 2011, 17, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Carlos, R.C.; Axelrod, D.A.; Ellis, J.H.; Abrahamse, R.H.; Fendrick, A.M. Incorporating patient-centered outcomes in the analysis of cost-effectiveness: Imaging strategies for renovascular hypertension. Am. J. Roentgenol. 2003, 181, 1653–1661. [Google Scholar] [CrossRef] [Green Version]
- Hansson, L.; Lindholm, L.H.; Niskanen, L.; Lanke, J.; Hedner, T.; Niklason, A.; Luomanmäki, K.; Dahlöf, B.; de Faire, U.; Mörlin, C.; et al. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: The Captopril Prevention Project (CAPPP) randomised trial. Lancet 1999, 353, 611–616. [Google Scholar] [CrossRef]
- Nelemans, P.J.; Kessels, A.G.; De Leeuw, P.; De Haan, M.; van Engelshoven, J. The cost-effectiveness of the diagnosis of renal artery stenosis. Eur. J. Radiol. 1998, 27, 95–107. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller ER 3rd Simons-Morton, D.G.; Karanja, N.; et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Insua, J.T.; Sacks, H.S.; Lau, T.S.; Lau, J.; Reitman, D.; Pagano, D.; Chalmers, T.C. Drug treatment of hypertension in the elderly: A meta-analysis. Ann. Intern. Med. 1994, 121, 355–362. [Google Scholar] [CrossRef]
- Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.Y.; Chien, K.L.; Chiu, Y.H.; Chuang, P.C.; Yen, M.F.; Chen, H.H. Dynamics of detailed components of metabolic syndrome associated with the risk of cardiovascular disease and death. Sci. Rep. 2021, 11, 3677. [Google Scholar] [CrossRef] [PubMed]
- Coorey, G.; Figtree, G.A.; Fletcher, D.F.; Redfern, J. The health digital twin: Advancing precision cardiovascular medicine. Nat. Rev. Cardiol. 2021, 18, 803–804. [Google Scholar] [CrossRef]
- Filippou, C.D.; Tsioufis, C.P.; Thomopoulos, C.G.; Mihas, C.C.; Dimitriadis, K.S.; Sotiropoulou, L.I.; Chrysochoou, C.A.; Nihoyannopoulos, P.I.; Tousoulis, D.M. Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 1150–1160. [Google Scholar] [CrossRef] [PubMed]
- Anchala, R.; Kaptoge, S.; Pant, H.; Di Angelantonio, E.; Franco, O.H.; Prabhakaran, D. Evaluation of effectiveness and cost-effectiveness of a clinical decision support system in managing hypertension in resource constrained primary health care settings: Results from a cluster randomized trial. J. Am. Heart Assoc. 2015, 4, e001213. [Google Scholar] [CrossRef] [Green Version]
- Colhoun, H.M.; Betteridge, D.J.; Durrington, P.N.; Hitman, G.A.; Neil, H.A.; Livingstone, S.J.; Thomason, M.J.; Mackness, M.I.; Charlton-Menys, V.; Fuller, J.H.; et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): Multicentre randomised placebo-controlled trial. Lancet 2004, 364, 685–696. [Google Scholar] [CrossRef]
- Roshandel, G.; Khoshnia, M.; Poustchi, H.; Hemming, K.; Kamangar, F.; Gharavi, A.; Ostovaneh, M.R.; Nateghi, A.; Majed, M.; Navabakhsh, B.; et al. Effectiveness of polypill for primary and secondary prevention of cardiovascular diseases (PolyIran): A pragmatic, cluster-randomised trial. Lancet 2019, 394, 672–683. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [Green Version]




| Variable | Base-Case Values | Distribution | Reference |
|---|---|---|---|
| Prevalence and disease natural history | |||
| Prevalence of hypertension | Refer to Supplementary Tables S1–S3 | Empirical data in Taiwanese community | |
| Transition probabilities in subsequent years | Tseng et al., 2012 [1] | ||
| Specific hazard for blood pressure | Tseng et al., 2012 [1] | ||
| Myocardial infarction | Carlos et al., 2003 [17]; Hansson et al., 1999 [18]; Nelemans et al., 1998 [19] | ||
| Normal | 0.003/yr | Beta (30, 9970) | |
| Prehypertension | 0.003748/yr | Beta (32, 9968) | |
| Stage I | 0.00633/yr | Beta (68, 9932) | |
| Stage II | 0.008737/yr | Beta (95, 9905) | |
| Mortality, immediate | 0.15 | Beta (15, 85) | |
| Mortality, yearly | 0.0311 | Beta (311, 9689) | |
| Stroke | Carlos et al., 2003 [17]; Hansson et al., 1999 [18]; Nelemans et al., 1998 [19] | ||
| Normal | 0.00075/yr | Beta (7.5, 9992.5) | |
| Prehypertension | 0.000937/yr | Beta (9.37, 9990.63) | |
| Stage I | 0.001675/yr | Beta (18, 9982) | |
| Stage II | 0.00333/yr | Beta (72, 9928) | |
| Mortality, immediate | 0.19 | Beta (19, 81) | |
| Mortality, yearly | 0.0201 | Beta (201, 9799) | |
| ESRD | Carlos et al., 2003 [17]; Nelemans et al., 1998 [19] | ||
| Normal | 0.000075/yr | Beta (0.75, 9999.25) | |
| Prehypertension | 0.0000937/yr | Beta (20, 9980) | |
| Stage I | 0.001213/yr | Beta (321, 9679) | |
| Stage II | 0.001716/yr | Beta (462, 4538) | |
| Mortality | 0.30 | ||
| Screening efficacy, lowering blood pressure | |||
| For prehypertension | 7/3 mm Hg | Sacks et al., 2001 [20] | |
| For Stage I | 16/-- mm Hg | ||
| For Stage II | 19.5/8.1 mm Hg | Insua et al., 1994 [21], Prospective Studies Collaboration, 2002 [22] | |
| Compliance | |||
| Life modification | 60% | Beta (60, 40) | |
| Screening | 70% | Beta (70, 30) | |
| Prophylactic medicine | 50% | Beta (50, 50) | |
| Cost for myocardial infarction | |||
| Cost of myocardial infarction per admission | Triangular (2706, 3006, 3068) | National Health Insurance Program, Taiwan | |
| Cost of myocardial infarction per visit | Triangular (50, 55, 66) | ||
| Cost for stroke | |||
| Cost of stroke per admission | Triangular (1027, 1141, 1370) | ||
| Cost of stoke per visit | Triangular (54, 59, 71) | ||
| Cost for ESRD | |||
| Annual Cost of ESRD (outpatients and administration included) | Triangular (18,000, 20,000, 24,000) | ||
| Cost for hypertension | |||
| Cost of hypertension per admission | Triangular (583, 647, 777) | ||
| Cost of hypertension per visit | Triangular (45, 40, 54) | ||
| Cost for life modification | |||
| Cost for life modification low | Triangular (300, 450, 600) | ||
| Cost for life modification mid | Triangular (300, 600, 900) | ||
| Cost for advanced health check up | Triangular (300, 400, 500) | ||
| Cost for life modification | Triangular (900, 1200, 1500) | ||
| Cost for others | |||
| Cost for screening/low awareness | Triangular (40, 80, 120) | ||
| Cost for regular health checkup | Triangular (100, 200, 300) | ||
| Cost of terminal care | Triangular (2000, 5000, 10,000) | ||
| Cost of prophylactic drug | Triangular (60, 120, 180) | ||
| Discount rate | 3% (0–5%) | Triangular (0, 0.03, 0.05) |
| Strategy | Cost | QALY | Increment Cost | Increment QALY | ICUR |
|---|---|---|---|---|---|
| Usual care | 16,455 | 13.4622 | |||
| Population-wide approach | 18,681 | 13.4806 | 2226 | 0.0184 | 120,781 |
| High-risk group approach | 17,801 | 13.4875 | 1346 | 0.0253 | 53,223 |
| Personalized approach | 14,872 | 13.9394 | −1583 | 0.4772 | −3317 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.-T.; Lin, T.-Y.; Chen, T.H.-H.; Chen, S.L.-S.; Fann, J.C.-Y. Cost-Effectiveness Analysis of Personalized Hypertension Prevention. J. Pers. Med. 2023, 13, 1001. https://doi.org/10.3390/jpm13061001
Wang S-T, Lin T-Y, Chen TH-H, Chen SL-S, Fann JC-Y. Cost-Effectiveness Analysis of Personalized Hypertension Prevention. Journal of Personalized Medicine. 2023; 13(6):1001. https://doi.org/10.3390/jpm13061001
Chicago/Turabian StyleWang, Sen-Te, Ting-Yu Lin, Tony Hsiu-Hsi Chen, Sam Li-Sheng Chen, and Jean Ching-Yuan Fann. 2023. "Cost-Effectiveness Analysis of Personalized Hypertension Prevention" Journal of Personalized Medicine 13, no. 6: 1001. https://doi.org/10.3390/jpm13061001
APA StyleWang, S.-T., Lin, T.-Y., Chen, T. H.-H., Chen, S. L.-S., & Fann, J. C.-Y. (2023). Cost-Effectiveness Analysis of Personalized Hypertension Prevention. Journal of Personalized Medicine, 13(6), 1001. https://doi.org/10.3390/jpm13061001






