Perception of Pathologists in Poland of Artificial Intelligence and Machine Learning in Medical Diagnosis—A Cross-Sectional Study
Abstract
:1. Introduction
1.1. The Role of Artificial Intelligence (AI) and Machine Learning (ML) in Medical Diagnosis
1.2. Artificial Intelligence and Machine Learning Drawbacks and Legal Considerations
1.3. Highlighting the Gap and Hypothesis Formulation
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Study Tool
2.4. Statistical Analysis
3. Results
3.1. Demographic Data of the Participants
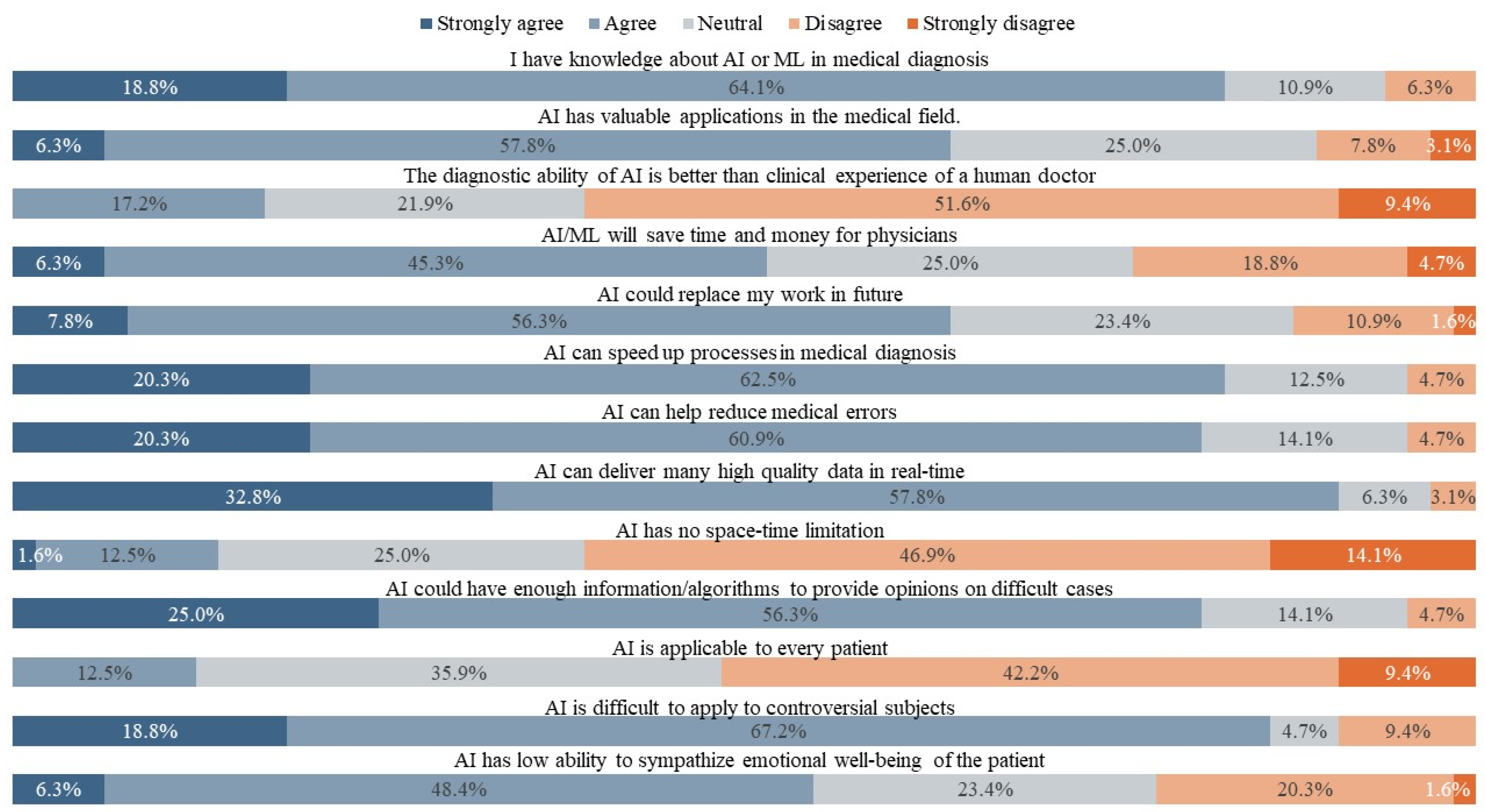
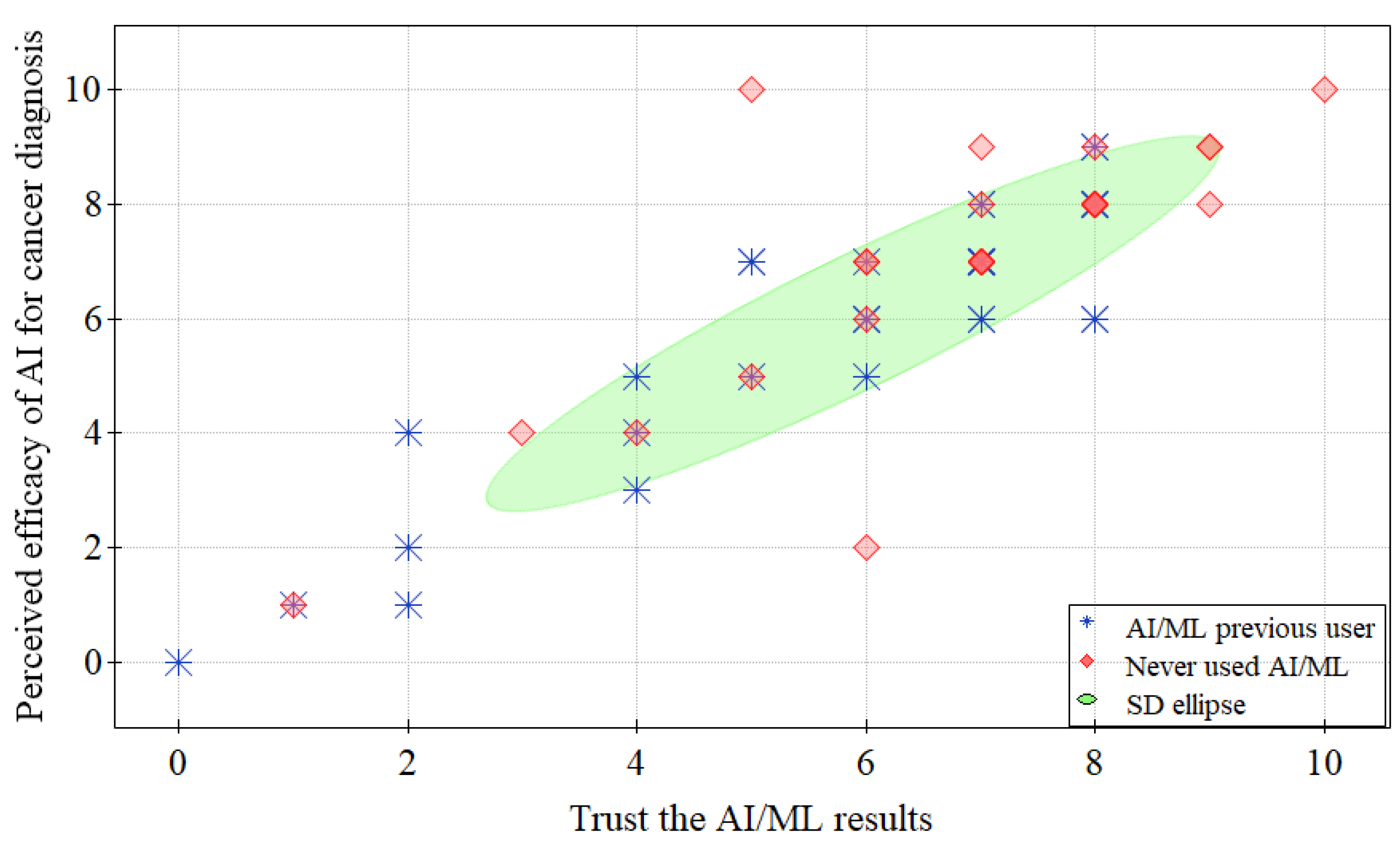
3.2. Level of Agreement with AI/ML in Clinical Use
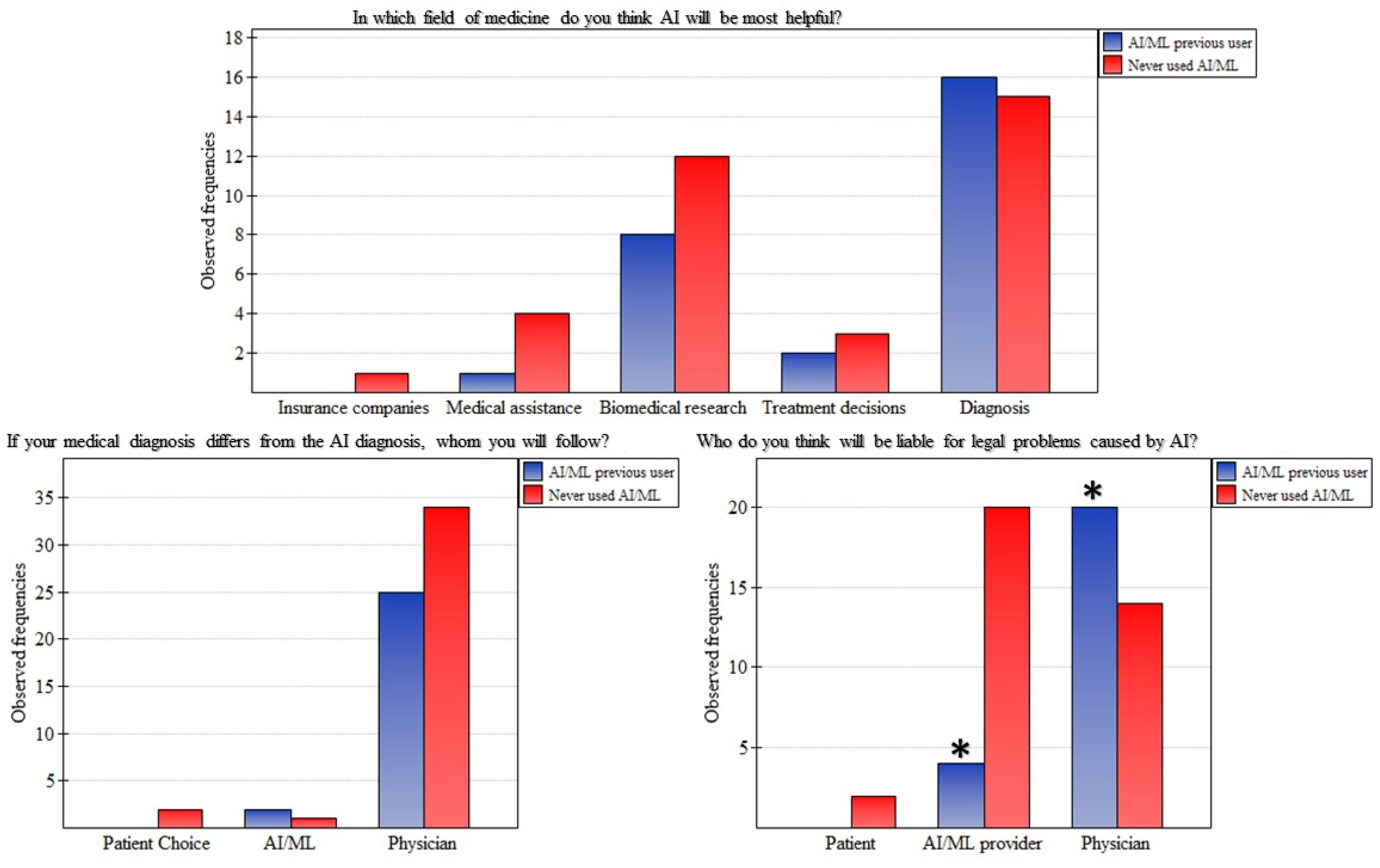
3.3. Concerns with AI/ML
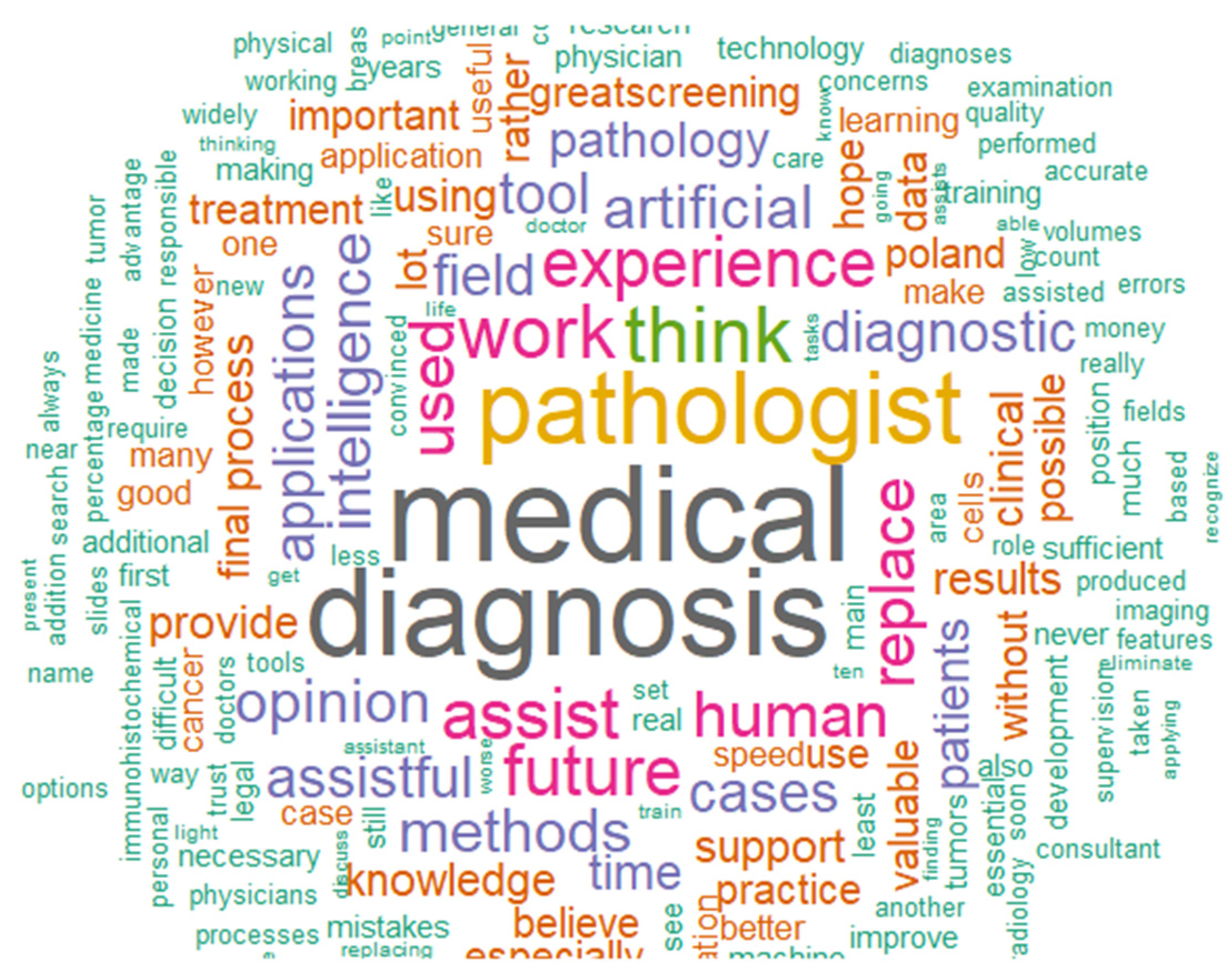
3.4. Future Expectations for AI/ML
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dlamini, Z.; Francies, F.Z.; Hull, R.; Marima, R. Artificial Intelligence (AI) and Big Data in Cancer and Precision Oncology. Comput. Struct. Biotechnol. J. 2020, 18, 2300–2311. [Google Scholar] [CrossRef] [PubMed]
- Benke, K.; Benke, G. Artificial Intelligence and Big Data in Public Health. Int. J. Environ. Res. Public Health 2018, 15, 2796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, A.A.; Abouzid, M.; Kaczmarek, E. Deep Learning Approaches in Histopathology. Cancers 2022, 14, 5264. [Google Scholar] [CrossRef] [PubMed]
- Försch, S.; Klauschen, F.; Hufnagl, P.; Roth, W. Artificial Intelligence in Pathology. Dtsch. Arztebl. Int. 2021, 118, 194–204. [Google Scholar] [CrossRef]
- Prabhakar, B.; Singh, R.K.; Yadav, K.S. Artificial Intelligence (AI) Impacting Diagnosis of Glaucoma and Understanding the Regulatory Aspects of AI-Based Software as Medical Device. Comput. Med. Imaging Graph. 2021, 87, 101818. [Google Scholar] [CrossRef]
- Alagappan, M.; Brown, J.R.G.; Mori, Y.; Berzin, T.M. Artificial Intelligence in Gastrointestinal Endoscopy: The Future Is Almost Here. WJGE 2018, 10, 239–249. [Google Scholar] [CrossRef]
- Meyer, J.; Khademi, A.; Têtu, B.; Han, W.; Nippak, P.; Remisch, D. Impact of Artificial Intelligence on Pathologists’ Decisions: An Experiment. J. Am. Med. Inform. Assoc. 2022, 29, 1688–1695. [Google Scholar] [CrossRef]
- Gu, H.; Huang, J.; Hung, L.; Chen, X. “Anthony” Lessons Learned from Designing an AI-Enabled Diagnosis Tool for Pathologists. Proc. ACM Hum.-Comput. Interact. 2021, 5, 10. [Google Scholar] [CrossRef]
- Tasci, E.; Zhuge, Y.; Camphausen, K.; Krauze, A.V. Bias and Class Imbalance in Oncologic Data—Towards Inclusive and Transferrable AI in Large Scale Oncology Data Sets. Cancers 2022, 14, 2897. [Google Scholar] [CrossRef]
- Chen, C.; Zheng, S.; Guo, L.; Yang, X.; Song, Y.; Li, Z.; Zhu, Y.; Liu, X.; Li, Q.; Zhang, H.; et al. Identification of Misdiagnosis by Deep Neural Networks on a Histopathologic Review of Breast Cancer Lymph Node Metastases. Sci. Rep. 2022, 12, 13482. [Google Scholar] [CrossRef]
- Sarwar, S.; Dent, A.; Faust, K.; Richer, M.; Djuric, U.; Van Ommeren, R.; Diamandis, P. Physician Perspectives on Integration of Artificial Intelligence into Diagnostic Pathology. npj Digit. Med. 2019, 2, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guillen, A.; Smallwood, K.; Killick, D.R. Molecular Pathology in the Cancer Clinic—Where Are We Now and Where Are We Headed? J. Small Anim. Pract. 2021, 62, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Steiner, D.F.; Chen, P.-H.C.; Mermel, C.H. Closing the Translation Gap: AI Applications in Digital Pathology. Biochim. Et Biophys. Acta (BBA)—Rev. Cancer 2021, 1875, 188452. [Google Scholar] [CrossRef] [PubMed]
- Religioni, U. Cancer Incidence and Mortality in Poland. Clin. Epidemiol. Glob. Health 2020, 8, 329–334. [Google Scholar] [CrossRef] [Green Version]
- Najwyższej Izbie Kontroli Organizacja, Dostępność I Jakość Diagnostyki Patomorfologicznej. Available online: https://www.nik.gov.pl/kontrole/P/19/062/ (accessed on 15 May 2023).
- Grzela, E. Prof. Marszałek: Braki Kadrowe w Patomorfologii Nie Są Jedynie Polskim Problemem. Available online: https://pulsmedycyny.pl/prof-marszalek-braki-kadrowe-w-patomorfologii-nie-sa-jedynie-polskim-problemem-1149337 (accessed on 15 May 2023).
- Märkl, B.; Füzesi, L.; Huss, R.; Bauer, S.; Schaller, T. Number of Pathologists in Germany: Comparison with European Countries, USA, and Canada. Virchows Arch. 2021, 478, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Dzikowski, A.; Szarek, J.; Gulda, D.; Babińska, I.; Felsmann, M.Z.; Popławski, K.; Szynaka, B. Where Are We with Polish Pathology at the Turn of the Centuries in the Light of the Congresses of the Polish Society of Pathologists? Pol. J. Pathol. 2018, 69, 114–117. [Google Scholar] [CrossRef]
- Kerasidou, A. Artificial Intelligence and the Ongoing Need for Empathy, Compassion and Trust in Healthcare. Bull. World Health Organ. 2020, 98, 245–250. [Google Scholar] [CrossRef]
- Shreve, J.T.; Khanani, S.A.; Haddad, T.C. Artificial Intelligence in Oncology: Current Capabilities, Future Opportunities, and Ethical Considerations. Am. Soc. Clin. Oncol. Educ. Book 2022, 42, 842–851. [Google Scholar] [CrossRef]
- Erickson, B.J.; Korfiatis, P.; Kline, T.L.; Akkus, Z.; Philbrick, K.; Weston, A.D. Deep Learning in Radiology: Does One Size Fit All? J. Am. Coll. Radiol. 2018, 15, 521–526. [Google Scholar] [CrossRef] [Green Version]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef] [Green Version]
- Orseau, L.; Ring, M. Space-Time Embedded Intelligence. In Artificial General Intelligence; Bach, J., Goertzel, B., Iklé, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2012; pp. 209–218. [Google Scholar]
- Oh, S.; Kim, J.H.; Choi, S.W.; Lee, H.J.; Hong, J.; Kwon, S.H. Physician Confidence in Artificial Intelligence: An Online Mobile Survey. J. Med. Internet Res. 2019, 21, e12422. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, R.; Fakieh, B. Health Care Employees’ Perceptions of the Use of Artificial Intelligence Applications: Survey Study. J. Med. Internet Res. 2020, 22, e17620. [Google Scholar] [CrossRef] [PubMed]
- Scheetz, J.; Rothschild, P.; McGuinness, M.; Hadoux, X.; Soyer, H.P.; Janda, M.; Condon, J.J.J.; Oakden-Rayner, L.; Palmer, L.J.; Keel, S.; et al. A Survey of Clinicians on the Use of Artificial Intelligence in Ophthalmology, Dermatology, Radiology and Radiation Oncology. Sci. Rep. 2021, 11, 5193. [Google Scholar] [CrossRef]
- Ebrahimian, S.; Kalra, M.K.; Agarwal, S.; Bizzo, B.C.; Elkholy, M.; Wald, C.; Allen, B.; Dreyer, K.J. FDA-Regulated AI Algorithms: Trends, Strengths, and Gaps of Validation Studies. Acad. Radiol. 2022, 29, 559–566. [Google Scholar] [CrossRef]
- Silkens, M.E.W.M.; Ross, J.; Hall, M.; Scarbrough, H.; Rockall, A. The Time Is Now: Making the Case for a UK Registry of Deployment of Radiology Artificial Intelligence Applications. Clin. Radiol. 2023, 78, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Andrew, M.; Irina, B. The Future of Medical Device Regulation and Standards: Dealing with Critical Challenges for Connected, Intelligent Medical Devices; Zenodo: Geneva, Switzerland, 2022. [Google Scholar]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods 2016, 18, 59–82. [Google Scholar] [CrossRef]
- Hagaman, A.K.; Wutich, A. How Many Interviews Are Enough to Identify Metathemes in Multisited and Cross-Cultural Research? Another Perspective on Guest, Bunce, and Johnson’s (2006) Landmark Study. Field Methods 2016, 29, 23–41. [Google Scholar] [CrossRef]
| Question No. | Question | Alpha |
|---|---|---|
| Q1 | I have knowledge about AI or ML in medical diagnosis | 0.778 |
| Q2 | AI has valuable applications in the medical field. | 0.752 |
| Q3 | The diagnostic ability of AI is better than the clinical experience of a human doctor | 0.763 |
| Q4 | AI/ML approaches will save time and money for physicians | 0.735 |
| Q5 | AI could replace my work in the future | 0.781 |
| Q6 | AI can speed up processes in medical diagnosis | 0.754 |
| Q7 | AI can help reduce medical errors | 0.745 |
| Q8 | AI can deliver much high-quality data in real-time | 0.756 |
| Q9 | AI has no space–time limitation | 0.764 |
| Q10 | AI could have enough information/algorithms to provide opinions on difficult cases | 0.754 |
| Q11 | AI is applicable to every patient | 0.781 |
| Q12 | AI is challenging to apply to controversial subjects | 0.811 |
| Q13 | AI has a low ability to sympathize with the emotional well-being of the patient | 0.814 |
| Standardized alpha | 0.793 |
| Age * | 37 (33–41.5) | |
| Years of medical practice experience * | 10 (6.75–15.25) | |
| Sex ** | Male | 25 (36.77) |
| Female | 36 (52.94) | |
| Prefer not to say | 7 (10.29) | |
| Did you use any AI/ML models before? *,**,*** | Yes | 27 (42.19) |
| No | 37 (57.81) | |
| How much do you trust the AI/ML results in a scale-out of 10? * | 7 (5.75–8) | |
| How do you evaluate the AI/ML in diagnosing cancer cells on a scale-out of 10 * | 7 (6–8) | |
| Question No. | Question | Never Used AI/ML | AI/ML Previous User | Mann–Whitney U Test | Chi-Squared Test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) * | No. (%) Disagree ** | No. (%) Agree *** | Median (IQR) * | No. (%) Disagree ** | No. (%) Agree *** | Z | p | χ2 | p | ||
| Q1 | I have knowledge about AI or ML in medical diagnosis | 3 (2-4) | 14 (58.33) | 10 (41.67) | 4 (4-4) | 0 (0.00) | 25 (100.00) | −5.284 | <0.001 **** | 20.417 | <0.001 |
| Q2 | AI has valuable applications in the medical field. | 4 (4-4) | 4 (11.76) | 30 (88.24) | 4 (4-4.5) | 2 (7.41) | 25 (92.59) | −1.588 | 0.112 | 0.322 | 0.570 |
| Q3 | The diagnostic ability of AI is better than the clinical experience of a human doctor | 2 (2-3) | 21 (84.00) | 4 (16.00) | 3 (2-3) | 12 (75.00) | 4 (25.00) | −1.206 | 0.228 | 0.503 | 0.478 |
| Q4 | AI/ML approaches will save time and money for physicians | 4 (4-4) | 2 (6.67) | 28 (93.33) | 4 (4-5) | 1 (4.00) | 24 (96.00) | −2.403 | 0.016 | 0.188 | 0.665 |
| Q5 | AI could replace my work in the future | 2 (2-3) | 22 (78.57) | 6 (21.43) | 2 (2-3) | 17 (85.00) | 3 (15.00) | −0.123 | 0.902 | 0.316 | 0.574 |
| Q6 | AI can speed up processes in medical diagnosis | 4 (4-4) | 1 (3.03) | 32 (96.97) | 4 (4-5) | 1 (3.70) | 26 (96.30) | −2.337 | 0.019 | 0.021 | 0.885 |
| Q7 | AI can help reduce medical errors | 4 (4-4) | 2 (6.06) | 31 (93.94) | 4 (4-5) | 1 (4.55) | 21 (95.45) | −1.097 | 0.272 | 0.059 | 0.808 |
| Q8 | AI can deliver much high-quality data in real-time | 4 (4-4) | 2 (6.45) | 29 (93.55) | 4 (4-5) | 1 (4.00) | 24 (96.00) | −1.692 | 0.091 | 0.164 | 0.685 |
| Q9 | AI has no space–time limitation | 4 (3-4) | 5 (18.52) | 22 (81.48) | 4 (3-4) | 3 (13.64) | 19 (86.36) | −1.271 | 0.204 | 0.212 | 0.646 |
| Q10 | AI could have enough information/algorithms to provide opinions on difficult cases | 3 (3-4) | 9 (36.00) | 16 (64.00) | 4 (3-4) | 6 (26.09) | 17 (73.91) | −1.409 | 0.159 | 0.548 | 0.459 |
| Q11 | AI is applicable to every patient | 2 (2-3) | 21 (84.00) | 4 (16.00) | 2 (2-3.5) | 18 (72.00) | 7 (28.00) | −0.052 | 0.959 | 1.049 | 0.306 |
| Q12 | AI is challenging to apply to controversial subjects | 4 (3-4) | 3 (10.34) | 26 (89.66) | 4 (3-4) | 4 (21.05) | 15 (78.95) | −1.689 | 0.091 | 1.057 | 0.304 |
| Q13 | AI has a low ability to sympathize with the emotional well-being of the patient | 4 (4-4) | 2 (5.71) | 33 (94.29) | 4 (3.5-4) | 2 (9.09) | 20 (90.91) | −1.799 | 0.072 | 0.236 | 0.627 |
| Question No. | Question | b Coeff. | b Error | Wald Stat. | p | Odds Ratio | −95% CI | +95% CI |
|---|---|---|---|---|---|---|---|---|
| Univariate predictors | ||||||||
| Q1 | I have knowledge about AI or ML in medical diagnosis | 2.842 | 0.769 | 13.655 | <0.001 | 17.158 | 3.799 | 77.488 |
| Q2 | AI has valuable applications in the medical field. | 0.488 | 0.361 | 1.829 | 0.176 | 1.628 | 0.803 | 3.301 |
| Q3 | The diagnostic ability of AI is better than the clinical experience of a human doctor | 0.387 | 0.314 | 1.520 | 0.218 | 1.472 | 0.796 | 2.723 |
| Q4 | AI/ML approaches will save time and money for physicians | 0.825 | 0.393 | 4.408 | 0.036 | 2.281 | 1.056 | 4.926 |
| Q5 | AI could replace my work in the future | −0.072 | 0.273 | 0.069 | 0.792 | 0.931 | 0.545 | 1.589 |
| Q6 | AI can speed up processes in medical diagnosis | 0.848 | 0.434 | 3.819 | 0.051 | 2.336 | 0.998 | 5.468 |
| Q7 | AI can help reduce medical errors | 0.355 | 0.363 | 0.959 | 0.328 | 1.426 | 0.701 | 2.903 |
| Q8 | AI can deliver much high-quality data in real-time | 0.593 | 0.390 | 2.312 | 0.128 | 1.810 | 0.843 | 3.886 |
| Q9 | AI has no space–time limitation | 0.316 | 0.313 | 1.014 | 0.314 | 1.371 | 0.742 | 2.535 |
| Q10 | AI could have enough information/algorithms to provide opinions on difficult cases | 0.334 | 0.267 | 1.572 | 0.210 | 1.397 | 0.828 | 2.355 |
| Q11 | AI is applicable to every patient | 0.110 | 0.286 | 0.148 | 0.700 | 1.116 | 0.637 | 1.957 |
| Q12 | AI is challenging to apply to controversial subjects | −0.576 | 0.323 | 3.186 | 0.074 | 0.562 | 0.299 | 1.058 |
| Q13 | AI has a low ability to sympathize with the emotional well-being of the patient | −0.574 | 0.365 | 2.484 | 0.115 | 0.563 | 0.276 | 1.150 |
| Backward stepwise multi-regression analysis | ||||||||
| Q1 | I have knowledge about AI or ML in medical diagnosis | 2.885 | 0.823 | 12.297 | <0.001 | 17.903 | 3.570 | 89.787 |
| Q2 | AI can speed up processes in medical diagnosis | 1.541 | 0.762 | 4.090 | 0.043 | 4.668 | 1.049 | 20.777 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, A.A.; Brychcy, A.; Abouzid, M.; Witt, M.; Kaczmarek, E. Perception of Pathologists in Poland of Artificial Intelligence and Machine Learning in Medical Diagnosis—A Cross-Sectional Study. J. Pers. Med. 2023, 13, 962. https://doi.org/10.3390/jpm13060962
Ahmed AA, Brychcy A, Abouzid M, Witt M, Kaczmarek E. Perception of Pathologists in Poland of Artificial Intelligence and Machine Learning in Medical Diagnosis—A Cross-Sectional Study. Journal of Personalized Medicine. 2023; 13(6):962. https://doi.org/10.3390/jpm13060962
Chicago/Turabian StyleAhmed, Alhassan Ali, Agnieszka Brychcy, Mohamed Abouzid, Martin Witt, and Elżbieta Kaczmarek. 2023. "Perception of Pathologists in Poland of Artificial Intelligence and Machine Learning in Medical Diagnosis—A Cross-Sectional Study" Journal of Personalized Medicine 13, no. 6: 962. https://doi.org/10.3390/jpm13060962
APA StyleAhmed, A. A., Brychcy, A., Abouzid, M., Witt, M., & Kaczmarek, E. (2023). Perception of Pathologists in Poland of Artificial Intelligence and Machine Learning in Medical Diagnosis—A Cross-Sectional Study. Journal of Personalized Medicine, 13(6), 962. https://doi.org/10.3390/jpm13060962









