Unilateral Cleft Lip and Palate Has Asymmetry of Bony Orbits: A Retrospective Study
Abstract
:1. Introduction
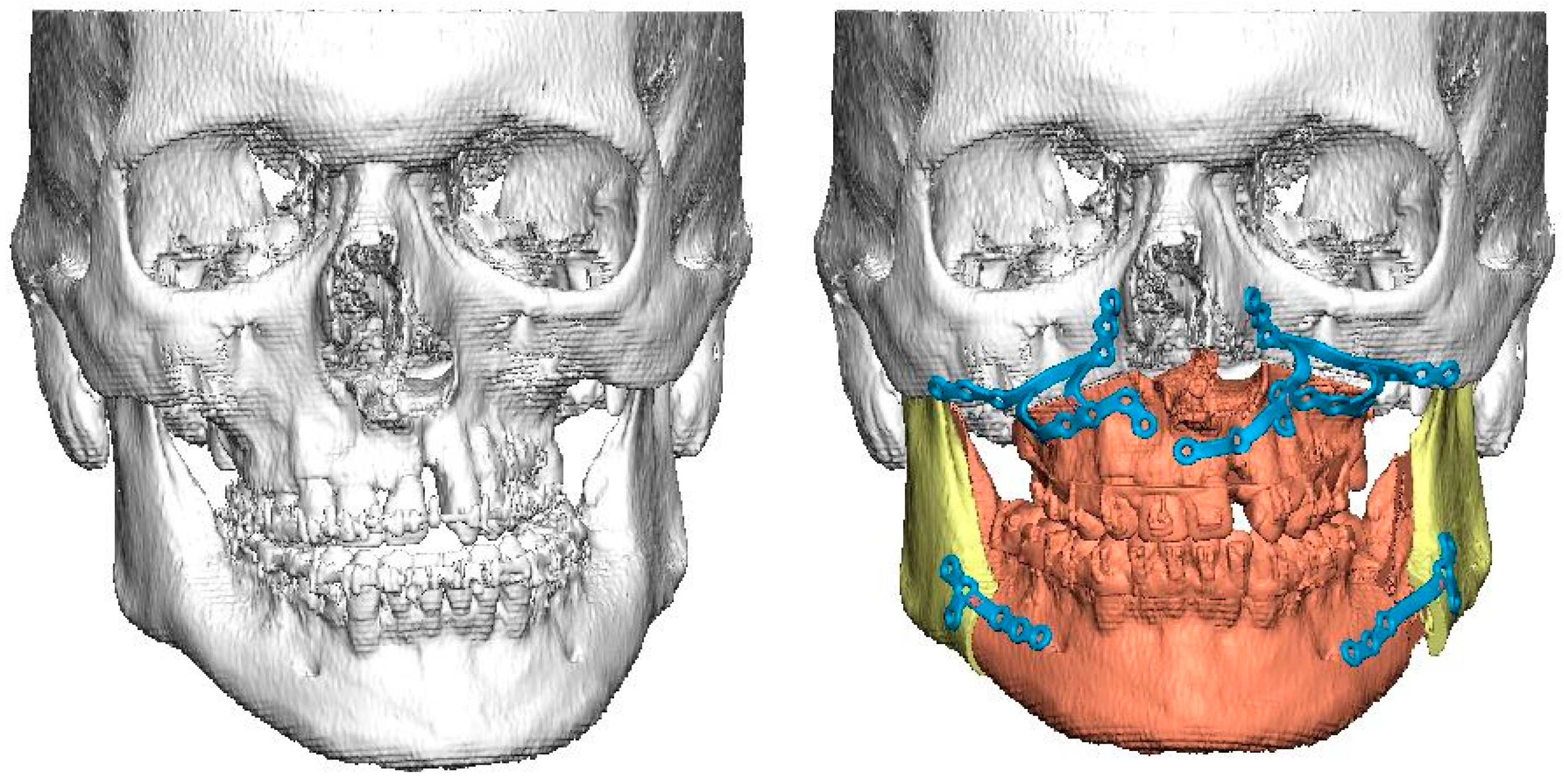
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Salari, N.; Darvishi, N.; Heydari, M.; Bokaee, S.; Darvishi, F.; Mohammadi, M. Global prevalence of cleft palate, cleft lip and cleft palate and lip: A comprehensive systematic review and meta-analysis. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Good, P.M.; Mulliken, J.B.; Padwa, B.L. Frequency of Le Fort I osteotomy after repaired cleft lip and palate or cleft palate. Cleft Palate-Craniofacial J. 2007, 44, 396–401. [Google Scholar] [CrossRef]
- Daskalogiannakis, J.; Mehta, M.; Meazzini, M.C.; Capello, A.V.; Ventrini, F.; Autelitano, L.; Morabito, A.; Garattini, G.; Brusati, R.; Wu, Y.; et al. The Need for Orthognathic Surgery in Patients with Repaired Complete Unilateral and Complete Bilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2009, 46, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Heliövaara, A.; Rautio, J. A comparison of craniofacial cephalometric morphology and the later need for orthognathic surgery in 6-year-old cleft children. J. Craniomaxillofacial Surg. 2011, 39, 173–176. [Google Scholar] [CrossRef]
- Voshol, I.; van der Wal, K.; van Adrichem, L.; Ongkosuwito, E.; Koudstaal, M. The Frequency of Le Fort I Osteotomy in Cleft Patients. Cleft Palate-Craniofacial J. 2012, 49, 160–166. [Google Scholar] [CrossRef]
- Meazzini, M.C.; Capello, A.V.; Ventrini, F.; Autelitano, L.; Morabito, A.; Garattini, G.; Brusati, R. Long-Term Follow-Up of UCLP Patients: Surgical and Orthodontic Burden of Care during Growth and Final Orthognathic Surgery Need. Cleft Palate-Craniofacial J. 2015, 52, 688–697. [Google Scholar] [CrossRef]
- Ore, C.D.; Schoenbrunner, A.; Brandel, M.; Kronstadt, N.; McIntyre, J.; Jones, M.; Gosman, A. Incidence of Le Fort Surgery in a Mature Cohort of Patients With Cleft Lip and Palate. Ann. Plast. Surg. 2017, 78 (Suppl. S4), S199–S203. [Google Scholar] [CrossRef]
- Jacob, L.; Fahradyan, A.; Paulson, P.; Wlodarczyk, J.R.; Wolfswinkel, E.M.; Jimenez, C.; Urata, M.M.; Hammoudeh, J.A. Orthognathic Surgery Rate in Cleft Care. J. Craniofacial Surg. 2022, 33, 87–92. [Google Scholar] [CrossRef]
- Mølsted, K.; Dahl, E. Asymmetry of the maxilla in children with complete unilateral cleft lip and palate. Cleft Palate J. 1990, 27, 184–190, Erratum in Cleft Palate J. 1990, 27, 444. [Google Scholar]
- Ras, F.; Habets, L.L.; Van Ginkel, F.C.; Prahl-Andersen, B. Three-Dimensional Evaluation of Facial Asymmetry in Cleft Lip and Palate. Cleft Palate-Craniofacial J. 1994, 31, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Smahel, Z.; Brejcha, M. Differences in craniofacial morphology between complete and incomplete unilateral cleft lip and palate in adults. Cleft Palate J. 1983, 20, 113–127. [Google Scholar] [PubMed]
- Kuijpers, M.A.R.; Chiu, Y.-T.; Nada, R.M.; Carels, C.E.L.; Fudalej, P.S. Three-dimensional Imaging Methods for Quantitative Analysis of Facial Soft Tissues and Skeletal Morphology in Patients with Orofacial Clefts: A Systematic Review. PLoS ONE 2014, 9, e93442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, X.; Pastewait, M.; Wu, T.; Lian, C.; Tejera, B.; Lee, Y.; Lin, F.; Wang, L.; Shen, D.; Li, S.; et al. 3D morphometric quantification of maxillae and defects for patients with unilateral cleft palate via deep learning-based CBCT image auto-segmentation. Orthod. Craniofacial Res. 2021, 24, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G.; Lindsay, W.K.; Vanderby, M.B. Morphology of the orbital region in adults following the cleft lip/palate repair in childhood. Am. J. Phys. Anthr. 1972, 37, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Harikrishnan, P.; Balakumaran, V. Analysis of Intramaxillary and Mid-Face Skeletal Asymmetry in a Three-Dimensional Model with Complete Unilateral Cleft Lip and Palate. J. Craniofacial Surg. 2018, 29, e759–e762. [Google Scholar] [CrossRef]
- Patel, D.S.; Jacobson, R.; Duan, Y.; Zhao, L.; Morris, D.; Cohen, M.N. Cleft Skeletal Asymmetry. Cleft Palate-Craniofacial J. 2018, 55, 348–355. [Google Scholar] [CrossRef]
- Zemann, W.; Santler, G.; Kärcher, H. Analysis of midface asymmetry in patients with cleft lip, alveolus and palate at the age of 3 months using 3D-COSMOS measuring system. J. Cranio-Maxillofacial Surg. 2002, 30, 148–152. [Google Scholar] [CrossRef]
- Ed-Dhahraouy, M.; Riri, H.; Ezzahmouly, M.; Bourzgui, F.; El Moutaoukkil, A. A new methodology for automatic detection of reference points in 3D cephalometry: A pilot study. Int. Orthod. 2018, 16, 328–337. [Google Scholar] [CrossRef]
- Kotaniemi, K.V.; Heliövaara, A.; Kotaniemi, M.; Stoor, P.; Leikola, J.; Palotie, T.; Suojanen, J. Comparison of postoperative skeletal stability of maxillary segments after Le Fort I osteotomy, using patient-specific implant versus mini-plate fixation. J. Cranio-Maxillofacial Surg. 2019, 47, 1020–1030. [Google Scholar] [CrossRef] [Green Version]
- Jacobson, R.; Sarver, D.M. The predictability of maxillary repositioning in LeFort I orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 142–154. [Google Scholar] [CrossRef] [Green Version]
- Wu, T.-J.; Lee, Y.-H.; Chang, Y.-J.; Lin, S.-S.; Lin, F.-C.; Kim, Y.-I.; Ko, C.-C.; Lai, J.-P. Three-Dimensional Outcome Assessments of Cleft Lip and Palate Patients Undergoing Maxillary Advancement. Plast. Reconstr. Surg. 2019, 143, 1255e–1265e. [Google Scholar] [CrossRef] [PubMed]
- Hsu, P.-J.; Denadai, R.; Pai, B.C.J.; Lin, H.-H.; Lo, L.-J. Outcome of facial contour asymmetry after conventional two-dimensional versus computer-assisted three-dimensional planning in cleft orthognathic surgery. Sci. Rep. 2020, 10, 2346. [Google Scholar] [CrossRef] [Green Version]
- Merta, M.; Heliövaara, A.; Leikola, J.; Suojanen, J. Early experience of wafer-free Le Fort I osteotomy with patient-specific implants in cleft lip and palate patients. J. Plast. Reconstr. Aesthetic Surg. 2023, 77, 78–86. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Z.; Liu, Y.; Ye, B.; Luo, E.; Li, J. Virtual Surgical Planning Assisted Management for Cleft-Related Maxillary Hypoplasia. J. Craniofacial Surg. 2019, 30, 1745–1749. [Google Scholar] [CrossRef] [PubMed]
- Chepurnyi, Y.; Chernohorskyi, D.; Prykhodko, D.; Poutala, A.; Kopchak, A. Reliability of orbital volume measurements based on computed tomography segmentation: Validation of different algorithms in orbital trauma patients. J. Cranio-Maxillofacial Surg. 2020, 48, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Kormi, E.; Männistö, V.; Lusila, N.; Naukkarinen, H.; Suojanen, J. Accuracy of Patient-Specific Meshes as a Reconstruction of Orbital Floor Blow-Out Fractures. J. Craniofacial Surg. 2021, 32, e116–e119. [Google Scholar] [CrossRef] [PubMed]
- Andrades, P.R.; Cuevas, P.E.; Hernández, R.; Danilla, S.V.; Villalobos, R. Characterization of the orbital volume in normal population. J. Cranio-Maxillofacial Surg. 2018, 46, 594–599. [Google Scholar] [CrossRef]
- Shyu, V.B.-H.; Hsu, C.-E.; Chen, C.-H.; Chen, C.-T. 3D-Assisted Quantitative Assessment of Orbital Volume Using an Open-Source Software Platform in a Taiwanese Population. PLoS ONE 2015, 10, e0119589. [Google Scholar] [CrossRef] [Green Version]
- FFuruta, M. Measurement of Orbital Volume by Computed Tomography Especially on the Growth of the Orbit. Jpn. J. Ophthalmol. 2001, 45, 600–606. [Google Scholar] [CrossRef]
- Anchlia, S.; Rao, K.S.; Bonanthaya, K.; Anupama, B.; Nayak, I.V. Ophthalmic Considerations in Cleft Lip and Palate Patients. J. Maxillofac. Oral Surg. 2011, 10, 14–19. [Google Scholar] [CrossRef] [Green Version]
- Sanchez, M.L.N.; Benjamin, R.H.; Mitchell, L.E.; Langlois, P.H.; Canfield, M.A.; Swartz, M.D.; Scheuerle, A.E.; Scott, D.A.; Northrup, H.; Schaaf, C.P.; et al. Birth Defect Co-Occurrence Patterns Among Infants With Cleft Lip and/or Palate. Cleft Palate-Craniofacial J. 2022, 59, 417–426. [Google Scholar] [CrossRef]
- Weinberg, S.; Leslie, E.J.; Hecht, J.T.; Wehby, G.L.; Deleyiannis, F.W.; Moreno, L.M.; Christensen, K.; Marazita, M.L. Hypertelorism and Orofacial Clefting Revisited: An Anthropometric Investigation. Cleft Palate-Craniofacial J. 2017, 54, 631–638. [Google Scholar] [CrossRef]
- Bill, J.; Proff, P.; Bayerlein, T.; Blens, T.; Gedrange, T.; Reuther, J. Orthognathic surgery in cleft patients. J. Cranio-Maxillofacial Surg. 2006, 34, 77–81. [Google Scholar] [CrossRef]
- Lilius, G.P. Clefts with Associated Anomalies and Syndromes in Finland. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1992, 26, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Şibar, S.; Doruk, M.; Gülşen, A.; Özdemir, A.; Tosun, G.; Üçüncü, N. Evaluation of Orbitomalar Region Projection in Patients With Operated Cleft Lip and Palate (Cephalometric Study). Cleft Palate-Craniofacial J. 2022; epub ahead of print. [Google Scholar] [CrossRef]
- Cho, R.I.; Kahana, A. Embryology of the Orbit. J. Neurol. Surg. Part B Skull Base 2021, 82, 2–6. [Google Scholar] [CrossRef]
- Schoenwolf, G.C.; Bleyl, S.B.; Brauer, P.R.; Francis-West, P.H. Larsen’s Human Embryology, 5th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2015. [Google Scholar]
- Gabrick, K.S.; Wu, R.T.; Singh, A.; Bartlett, S.P.; Taylor, J.A.; Persing, J.A.; Alperovich, M. Assessing Facial Asymmetry in Postoperative Patients With Unilateral Coronal Craniosynostosis. J. Craniofacial Surg. 2020, 31, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Kronig, S.A.J.; Kronig, O.D.M.; Zurek, M.; Van Adrichem, L.N.A. Orbital volume, ophthalmic sequelae and severity in unilateral coronal synostosis. Child’s Nerv. Syst. 2021, 37, 1687–1694. [Google Scholar] [CrossRef] [PubMed]
- Öwall, L.; Darvann, T.A.; Larsen, P.; Hove, H.D.; Hermann, N.V.; Bøgeskov, L.; Kreiborg, S. Facial Asymmetry in Children with Unicoronal Synostosis who have Undergone Craniofacial Reconstruction in Infancy. Cleft Palate-Craniofacial J. 2016, 53, 385–393. [Google Scholar] [CrossRef]
- Gribova, M.N.; Pluijmers, B.I.; Resnick, C.M.; Caron, C.J.; Borghi, A.; Koudstaal, M.; Padwa, B.L. Is There a Difference in Orbital Volume Between Affected and Unaffected Sides in Patients With Unilateral Craniofacial Microsomia? J. Oral Maxillofac. Surg. 2018, 76, 2625–2629. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Liao, Y.-F.; Chang, C.-S.; Lu, T.-C.; Chen, K.-T. Patient satisfaction and quality of life after orthodontic treatment for cleft lip and palate deformity. Clin. Oral Investig. 2021, 25, 5521–5529. [Google Scholar] [CrossRef] [PubMed]
- Suojanen, J.; Leikola, J.; Stoor, P. The use of patient-specific implants in orthognathic surgery: A series of 32 maxillary osteotomy patients. J. Cranio-Maxillofacial Surg. 2016, 44, 1913–1916. [Google Scholar] [CrossRef] [Green Version]
- Heufelder, M.; Wilde, F.; Pietzka, S.; Mascha, F.; Winter, K.; Schramm, A.; Rana, M. Clinical accuracy of waferless maxillary positioning using customized surgical guides and patient specific osteosynthesis in bimaxillary orthognathic surgery. J. Cranio-Maxillofacial Surg. 2017, 45, 1578–1585. [Google Scholar] [CrossRef]
- Järvinen, S.; Suojanen, J.; Suomalainen, A.; Stoor, P. Virtual Surgical Planning Combined With Intraoperative Navigation in Mandibular Bilateral Sagittal Split Osteotomy for Accurate Placement of Patient Specific Implants. J. Craniofacial Surg. 2021, 32, 2666–2670. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.K.; Alfawzan, A.A.; Akhter, F.; Alswairki, H.J.; Chaudhari, P.K. Evaluation of Lip Morphology and Nasolabial Angle in Non-Syndromic Cleft Lip and/Palate and Non-Cleft Individuals. Appl. Sci. 2022, 12, 357. [Google Scholar] [CrossRef]
- Kaczorowska, N.; Mikulewicz, M. Impact of Cleft Palate Anastomosis in Cleft Lip and Palate Patients with Coexisting Cleft Lip Anastomosis Scar Based on Cephalometric Measurements. Appl. Sci. 2022, 12, 1104. [Google Scholar] [CrossRef]
- Kochhar, A.S.; Nucci, L.; Sidhu, M.S.; Prabhakar, M.; Grassia, V.; Perillo, L.; Kochhar, G.K.; Bhasin, R.; Dadlani, H.; D’apuzzo, F. Reliability and Reproducibility of Landmark Identification in Unilateral Cleft Lip and Palate Patients: Digital Lateral Vis-A-Vis CBCT-Derived 3D Cephalograms. J. Clin. Med. 2021, 10, 535. [Google Scholar] [CrossRef] [PubMed]
- Krooks, L.; Pirttiniemi, P.; Kanavakis, G.; Lähdesmäki, R. Prevalence of malocclusion traits and orthodontic treatment in a Finnish adult population. Acta Odontol. Scand. 2016, 74, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Koskela, A.; Neittaanmäki, A.; Rönnberg, K.; Palotie, A.; Ripatti, S.; Palotie, T. The relation of severe malocclusion to patients’ mental and behavioral disorders, growth, and speech problems. Eur. J. Orthod. 2021, 43, 159–164. [Google Scholar] [CrossRef]



| Cleft Patients | |||
|---|---|---|---|
| W | df | Sig. | |
| Cleft height | 0.947 | 12 | 0.594 |
| Contralat height | 0.900 | 12 | 0.159 |
| Cleft width | 0.910 | 12 | 0.211 |
| Contralat width | 0.951 | 12 | 0.654 |
| Cleft depth | 0.942 | 12 | 0.520 |
| Contralat depth | 0.921 | 12 | 0.295 |
| Cleft position | 0.916 | 12 | 0.255 |
| Contralat position | 0.946 | 12 | 0.585 |
| Cleft volume | 0.933 | 12 | 0.408 |
| Contralat volume | 0.863 | 12 | 0.053 |
| Non-Cleft Patients | |||
| W | df | Sig. | |
| Right height | 0.910 | 14 | 0.157 |
| Left height | 0.934 | 14 | 0.342 |
| Right width | 0.961 | 14 | 0.733 |
| Left width | 0.896 | 14 | 0.100 |
| Right depth | 0.893 | 14 | 0.090 |
| Left depth | 0.958 | 14 | 0.687 |
| Right position | 0.923 | 14 | 0.246 |
| Left position | 0.945 | 14 | 0.487 |
| Right volume | 0.973 | 14 | 0.919 |
| Left volume | 0.959 | 14 | 0.710 |
| Age | Sex | Type | Cleft Side | Ocular | Osteotomy | Previous Operations |
|---|---|---|---|---|---|---|
| pathology | ||||||
| 20 y 7 mo | M | UCLP | Left | No | Le Fort 1 | Primary lip repair and soft palate closure 4 mo. |
| Hard palate closure 11 mo. | ||||||
| Alveolar bone graft 9 y 6 mo. | ||||||
| 18 y 3 mo | M | UCLP | Right | Myopia | Bimaxillary | Primary lip repair 3 mo and soft palate closure 3 mo. |
| astigmatism | Hard palate closure 9 mo. | |||||
| Alveolar bone graft 11 y 2 mo. | ||||||
| 18 y 10 mo | M | UCLP | Left | No | Le Fort 1 | Primary lip repair 4 mo. One-stage palatal closure 11 mo. |
| VPI surgery (Furlow Z-plasty) 6 y 7 mo. | ||||||
| Alveolar bone graft 10 y 10 mo. Early Le Fort 1 osteotomy 14 y 4 mo. | ||||||
| 20 y 7 mo | M | UCLP | Left | No | Bimaxillary | Primary lip repair and soft palate closure 4 mo. |
| Hard palate closure 11 mo. Secondary lip repair 6 y 9 mo. | ||||||
| Secondary lip repair and rhinoplasty 11 y 9 mo. Alveolar bone graft 11 y 7 mo. | ||||||
| 13 y 4 mo | F | UCLP | Left | No | Le Fort 1 | Primary lip repair 3 mo. One-stage palatal closure 1 y 2 mo. |
| Alveolar bone graft and fistula closure 9 y 2 mo. | ||||||
| 12 y 5 mo | F | UCLP | Left | No | Le Fort 1 | Primary lip repair 4 mo. One-stage palatal closure 8 mo. |
| Fistula closure 5 y 4 mo. Alveolar bone graft 9 y 3 mo. | ||||||
| 16 y 2 mo | F | UCLP | Left | No | Le Fort 1 | Primary lip repair 3 mo. One-stage palatal closure 1 y. |
| Previous operations abroad, no specific data. | ||||||
| Alveolar bone graft 10 y 8 mo. Early Le Fort 1 osteotomy 13 y 3 mo. | ||||||
| 16 y 2 mo | F | UCLP | Left | No | Le Fort 1 | Primary lip repair and palatal closure around 1 y. |
| Previous operations abroad, no specific data. | ||||||
| Alveolar bone grafts 9 y 2 mo and 10 y 2 mo. Fistula closure 11 y 3 mo. | ||||||
| 27 y 8 mo | F | UCLP | Left | No | Bimaxillary | Primary lip repair 3 mo. One-stage palatal closure 9 mo. |
| Secondary lip repair 8 y 9 mo. | ||||||
| Alveolar bone graft 9 y 1 mo. Rhinoplasty 17 y 7 mo. | ||||||
| 18 y 2 mo | F | UCLP | Right | No | Le Fort 1 | Primary lip repair and soft palate closure 3 mo. Hard palate closure 8 mo. |
| VPI surgery (muscular repair of soft palate) 7 y 2 mo. | ||||||
| Alveolar bone graft 16 y 7 mo. | ||||||
| 18 y 10 mo | M | UCLP | Left | No | Le Fort 1 | Primary lip repair and soft palate closure 3 mo. Hard palate closure 1 y. |
| Fistula closure 5 y 6 mo. | ||||||
| Alveolar bone graft 9 y 4 mo. | ||||||
| 21 y 6 mo | M | UCLP | Left | No | Bimaxillary | Primary lip repair 3 mo. One-stage palatal closure 9 mo. |
| VPI surgery (pharyngeal flap, Hogan) 5 y 6 mo. | ||||||
| Alveolar bone graft 9 y 5 mo. | ||||||
| 24 y 3 mo | M | UCLP | Right | No | Le Fort 1 | Primary lip repair 3 mo. One-stage palatal closure 10 mo. |
| Alveolar bone graft 10 y 3 mo. | ||||||
| 16 y 8 mo | F | UCLP | Left | No | Bimaxillary | Primary lip repair 7 mo. One-stage palatal closure 1 y 1 mo. |
| Alveolar bone graft 11 y 7 mo. | ||||||
| 18 y 10 mo | M | UCLP | Right | No | Le Fort 1 | Primary lip repair 3 mo. One-stage palatal closure 1 y. |
| Alveolar bone graft 10 y 1 mo. | ||||||
| Mean 18, 82 y | 8 M, 7 F | 11 left, 4 right | 10 Le Fort 1, 5 Bimax |
| Cleft Side | Contralat. Side | Mean | 95% CI | 95% CI | DF | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Difference | Lower | Upper | ||||||
| Height, cm | ||||||||
| n = 14 | 3.793 | 3.793 | 0 | −0.0751 | 0.0751 | 13 | 1.00 | NS |
| Width, cm | ||||||||
| n = 14 | 3.300 | 3.343 | −0.0429 | −0.0970 | 0.0113 | 13 | 0.111 | NS |
| Depth, cm | ||||||||
| n = 15 | 4.520 | 4.567 | −0.0467 | −0.1326 | 0.0393 | 14 | 0.264 | NS |
| Position, cm | ||||||||
| n = 15 | 6.660 | 6.888 | −0.1733 | −0.3129 | −0.0338 | 14 | 0.019 | * |
| Volume, mm3 | ||||||||
| n = 12 | 25,596.825 | 26,433.167 | −836.3417 | −1464.8051 | −207.8782 | 11 | 0.014 | * |
| Bimax, Cleft vs. Contralat. % | Le Fort 1, Cleft vs. Contralat. % | p-Value | ||
|---|---|---|---|---|
| Height | 101.56 | 99.04 | 0.518 | NS |
| Width | 98.82 | 98.72 | 0.898 | NS |
| Depth | 97.05 | 100.07 | 0.099 | NS |
| Position | 94.53 | 99.00 | 0.040 | * |
| Volume | 95.71 | 97.97 | 0.343 | NS |
| Right | Left | Mean | 95% CI | DF | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| Difference | Lower | Upper | ||||||
| Height, cm | ||||||||
| n = 14 | 3.836 | 3.867 | −0.0214 | 0.09 | 0.0472 | 13 | 0.512 | NS |
| Width, cm | ||||||||
| n = 15 | 3.49333 | 3.507 | −0.0113 | −0.0545 | −0.0545 | 14 | 0.499 | NS |
| Depth, cm | ||||||||
| n = 16 | 4.919 | 4.875 | 0.0438 | −0.0177 | 0.1052 | 15 | 0.15 | NS |
| Position, cm | ||||||||
| n = 16 | 7.19375 | 7.169 | 0.025 | −0.0465 | 0.0965 | 15 | 0.468 | NS |
| Volume, mm3 | ||||||||
| n = 14 | 24,591.429 | 24,448 | 143.571 | −78.928 | 366.071 | 13 | 0.187 | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kormi, E.; Peltola, E.; Lusila, N.; Heliövaara, A.; Leikola, J.; Suojanen, J. Unilateral Cleft Lip and Palate Has Asymmetry of Bony Orbits: A Retrospective Study. J. Pers. Med. 2023, 13, 1067. https://doi.org/10.3390/jpm13071067
Kormi E, Peltola E, Lusila N, Heliövaara A, Leikola J, Suojanen J. Unilateral Cleft Lip and Palate Has Asymmetry of Bony Orbits: A Retrospective Study. Journal of Personalized Medicine. 2023; 13(7):1067. https://doi.org/10.3390/jpm13071067
Chicago/Turabian StyleKormi, Eeva, Elina Peltola, Niilo Lusila, Arja Heliövaara, Junnu Leikola, and Juho Suojanen. 2023. "Unilateral Cleft Lip and Palate Has Asymmetry of Bony Orbits: A Retrospective Study" Journal of Personalized Medicine 13, no. 7: 1067. https://doi.org/10.3390/jpm13071067
APA StyleKormi, E., Peltola, E., Lusila, N., Heliövaara, A., Leikola, J., & Suojanen, J. (2023). Unilateral Cleft Lip and Palate Has Asymmetry of Bony Orbits: A Retrospective Study. Journal of Personalized Medicine, 13(7), 1067. https://doi.org/10.3390/jpm13071067








