The Use of Radio and Telemedicine by TMAS Centers in Provision of Medical Care to Seafarers: A Systematic Review
Abstract
:1. Introduction
2. Methodology
2.1. Document Search
2.2. Inclusion Exclusion Criteria
2.3. Quality and Risk Bias Assessment
3. Results
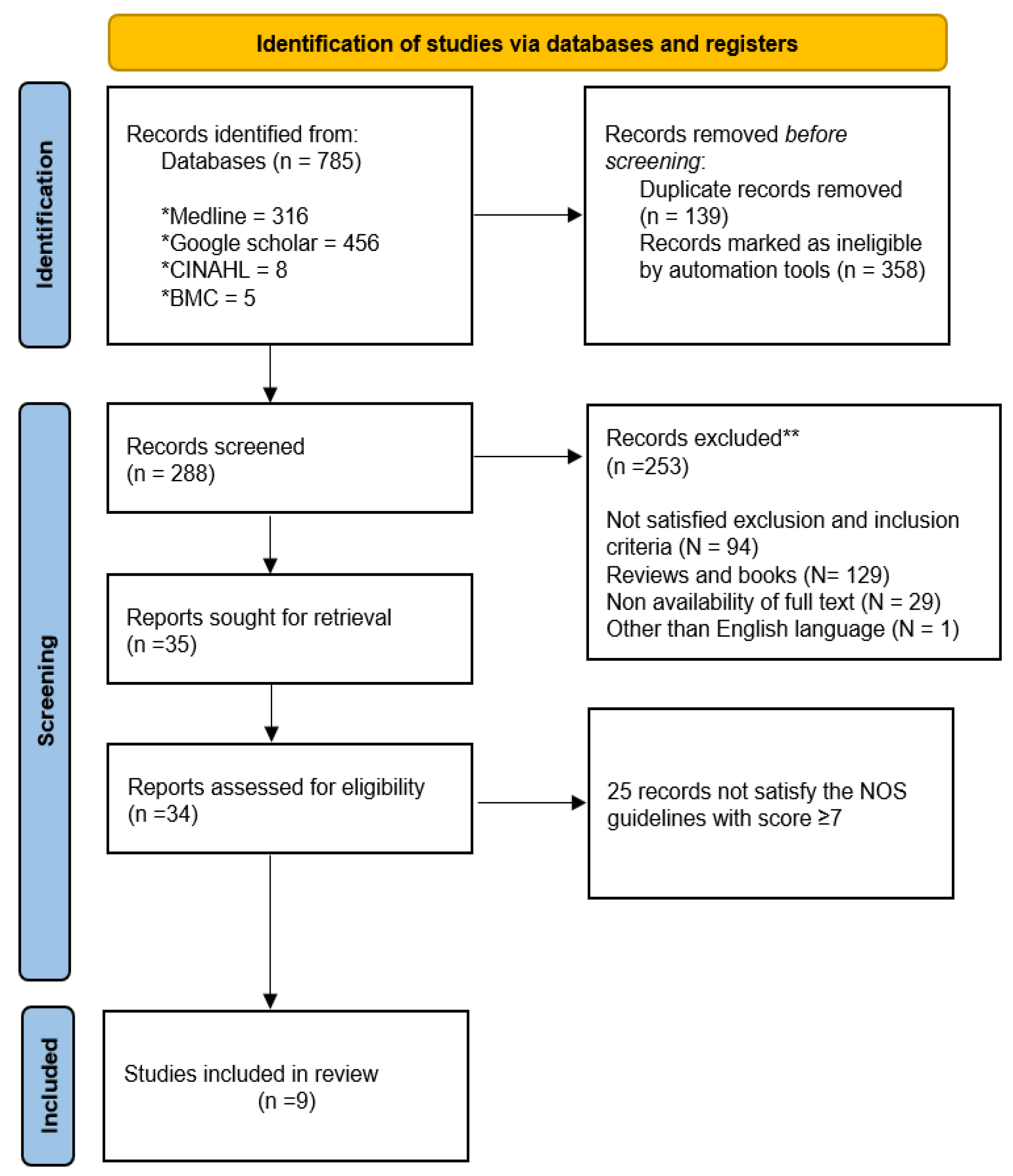
3.1. Document Selection Flowchart
3.2. Communication Channels
3.3. TMAS Centers and Means Communication
3.4. Study Characteristics
3.4.1. Medical Assistance via Radio
3.4.2. Telemedicine Technologies
4. Discussion
4.1. What Needs to Be Done?
4.1.1. Integration of Artificial Intelligence (AI) in Telemedicine
4.1.2. Satellite Telecommunications
4.2. Implications of Medical Assistance at Sea in Healthcare
4.3. Regional Context and Digital Divide Issues
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guglielmo Marconi. Available online: https://www.history.com/topics/inventions/guglielmo-marconi (accessed on 22 May 2023).
- Norman, G. Medical education: Past, present and future. Perspect. Med. Educ. 2012, 1, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flesche, C.W.; Jalowy, A. Telemedicine in medical emergency situations in terms of maritime personnel. Dtsch Med. Wochenschr. 2007, 132, 463–464. [Google Scholar] [CrossRef]
- Grappasonni, I.; Petrelli, F.; Amenta, F. Deaths on board ships assisted by the Centro internazionale radio medico in the last 25 years. Travel Med. Infect. Dis. 2012, 10, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Hunt, J.; Lucas, D.; Laforet, P.; Coulange, M.; Auffray, J.P.; Dehours, E. Medical treatment of seafarers in the Southern Indian Ocean—Interaction between the French Telemedical Maritime Assistance Service (TMAS) and the medical bases of the French Southern and Antarctic Lands (TAAF). Int. Marit. Health 2022, 73, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Westlund, K.; Attvall, S.; Nilsson, R.; Jensen, O.C. Telemedical Maritime Assistance Service (TMAS) to Swedish merchant and passengers ships 1997–2012. Int. Marit. Health 2016, 67, 24–30. [Google Scholar] [CrossRef] [Green Version]
- Mahdi, S.S.; Amenta, F. Eighty years of CIRM. A journey of commitment and dedication in providing maritime medical assistance. Int. Marit. Health 2016, 67, 187–195. [Google Scholar] [CrossRef] [Green Version]
- Sagaro, G.G.; Battineni, G.; Chintalapudi, N.; Di Canio, M.; Amenta, F. Telemedical assistance at sea in the time of COVID-19 pandemic. Int. Marit. Health 2020, 71, 229–236. [Google Scholar] [CrossRef]
- Le Gac, J.M.; Texier, S. Training in the detection of psychological distress on board ships through health simulation during the COVID-19 epidemic. Int. Marit. Health 2022, 73, 89–94. [Google Scholar] [CrossRef]
- Legido-Quigley, H.; Chuah, F.L.H.; Howard, N. Southeast Asian health system challenges and responses to the “Andaman Sea refugee crisis”: A qualitative study of health-sector perspectives from Indonesia, Malaysia, Myanmar, and Thailand. PLoS Med. 2020, 17, e1003143. [Google Scholar] [CrossRef]
- Brayley, N.F. A Review of Three Years Experience of Medical Advice to Seafarers by the Casualty Officer, Royal Naval Hospital Plymouth, via Portishead Radio (W/T Medico Portishead). J. R. Nav. Med. Serv. 1980, 66, 93–106. [Google Scholar] [CrossRef]
- Ricci, G.; Pirillo, I.; Rinuncini, C.; Amenta, F. Medical assistance at the sea: Legal and medico-legal problems. Int. Marit. Health 2014, 65, 205–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKay, J.; Bradley, N.; Lough, M.; Bowie, P. A review of significant events analysed in general practice: Implications for the quality and safety of patient care. BMC Fam. Pract. 2009, 10, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sagaro, G.G.; Amenta, F. Past, present, and future perspectives of telemedical assistance at sea: A systematic review. Int. Marit. Health 2020, 71, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada.
- Holt, T.E.; Tveten, A.; Dahl, E. Medical emergencies on large passenger ships without doctors: The Oslo-Kiel-Oslo ferry experience. Int. Marit. Health 2017, 68, 153–158. [Google Scholar] [CrossRef] [Green Version]
- Szafran-Dobrowolska, J.; Renke, M.; Wołyniec, W. Telemedical Maritime Assistance Service at the University Center of Maritime and Tropical Medicine in Gdynia. The analysis of 6 years of activity. Med. Pract. 2020, 71, 121–125. [Google Scholar] [CrossRef]
- Di Canio, M.; Burzi, L.; Ribero, S.; Amenta, F.; Quaglino, P. Role of teledermatology in the management of dermatological diseases among marine workers: A cross-sectional study comparing general practitioners and dermatological diagnoses. Front. Med. 2022, 9, 2354. [Google Scholar] [CrossRef]
- Dehours, E.; De Camaret, E.; Lucas, D.; Saccavini, A.; Roux, P. The COVID-19 pandemic and maritime telemedicine: 18-month report. Int. Marit. Health 2022, 73, 83–88. [Google Scholar] [CrossRef]
- Apostolatos, C.; Andria, V.; Licari, J. Overall comparative analysis of management and outcomes of cardiac cases reported on board merchant ships. Int. Marit. Health 2017, 68, 190–195. [Google Scholar] [CrossRef] [Green Version]
- Herttua, K.; Gerdøe-Kristensen, S.; Vork, J.C.; Nielsen, J.B. Age and nationality in relation to injuries at sea among officers and non-officers: A study based on contacts from ships to Telemedical Assistance Service in Denmark. BMJ Open 2019, 9, e034502. [Google Scholar] [CrossRef] [Green Version]
- Dehours, E.; Saccavini, A.; Roucolle, P.; Roux, P.; Bounes, V. Added value of sending photograph in diagnosing a medical disease declared at sea: Experience of the French Tele-Medical Assistance Service. Int. Marit. Health 2017, 68, 122–125. [Google Scholar] [CrossRef] [Green Version]
- Sagaro, G.G.; Dicanio, M.; Battineni, G.; Samad, M.A.; Amenta, F. Incidence of occupational injuries and diseases among seafarers: A descriptive epidemiological study based on contacts from onboard ships to the Italian Telemedical Maritime Assistance Service in Rome, Italy. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef]
- Battineni, G.; Chintalapudi, N.; Amenta, F. Maritime Telemedicine: Design and Development of an Advanced Healthcare System Called Marine Doctor. J. Pers. Med. 2022, 12, 832. [Google Scholar] [CrossRef]
- Battineni, G.; Di Canio, M.; Chintalapudi, N.; Amenta, F.; Nittari, G. Development of physical training smartphone application to maintain fitness levels in seafarers. Int. Marit. Health 2019, 70, 180–186. [Google Scholar] [CrossRef] [Green Version]
- Mariners Medico Guide. Available online: https://www.medicoguide.no/ (accessed on 17 May 2023).
- Asser, T.; Linnamägi, Ü. Telemedicine in Baltic Sea Region: Experiences of Tartu University. Croat. Med. J. 2004, 45, 523–525. [Google Scholar] [PubMed]
- Oldenburg, M.; Baur, X.; Schlaich, C. Cardiovascular diseases in modern maritime industry. Int. Marit. Health 2010, 62, 101–106. [Google Scholar] [PubMed]
- Mair, F.; Fraser, S.; Ferguson, J.; Webster, K. Telemedicine via satellite to support offshore oil platforms. J. Telemed. Telecare 2008, 14, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Çakir, E. Determinants of medical evacuations from merchant cargo ships: Evidence from Telemedical Assistance Service of Turkey data. Ocean Coast. Manag. 2021, 211, 105797. [Google Scholar] [CrossRef]
- Latournerie, G.; Dehours, É.; Roux, P.; Houze Cerfon, C.-H.; Balen, F. Teleconsultation at Sea and Acute Wound Management Onboard. Telemed. e-Health 2023, 29, 569–575. [Google Scholar] [CrossRef]
- Lateef, F.; Anantharaman, V. Maritime radio-medical services: The Singapore General Hospital experience. Am. J. Emerg. Med. 2002, 20, 349–351. [Google Scholar] [CrossRef]
- Sagaro, G.G.; Di Canio, M.; Amenta, F. Correlation between body mass index and blood pressure in seafarers. Clin. Exp. Hypertens. 2021, 43, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Amenta, F.; Dauri, A.; Rizzo, N. Organization and activities of the International Radio Medical Centre (CIRM). J. Telemed. Telecare 1996, 2, 125–131. [Google Scholar] [CrossRef]
- Al-Antari, M.A. Artificial Intelligence for Medical Diagnostics-Existing and Future AI Technology! Diagnostics 2023, 13, 688. [Google Scholar] [CrossRef] [PubMed]
- Morosi, S.; Jayaousi, S.; Falletti, E.; Araniti, G. Cooperative strategies in satellite assisted emergency services. Int. J. Satell. Commun. Netw. 2013, 31, 141–156. [Google Scholar] [CrossRef]
- Franck, L.; Berioli, M.; Boutry, P.; Harles, G.; Ronga, L.S.; Suffritti, R.; Thomasson, L. On the role of satellite communications for emergency situations with a focus on Europe. Int. J. Satell. Commun. Netw. 2011, 29, 387–399. [Google Scholar] [CrossRef] [Green Version]
- Skinnemoen, H.; Hansen, S.; Jahn, A. Satellite-Based Infrastructure for Emergency Communications. In Proceedings of the 25th AIAA International Communications Satellite Systems Conference (organized by APSCC), Seoul, Republic of Korea, 10–13 April 2007. [Google Scholar] [CrossRef]
- Anscombe, D.L. Healthcare delivery for oil rig workers: Telemedicine plays a vital role. Telemed. e-Health 2010, 16, 659–663. [Google Scholar] [CrossRef] [Green Version]
- Pengput, A.; Schwartz, D.G. Telemedicine in Southeast Asia: A Systematic Review. Telemed. J. e-Health 2022, 28, 1711–1733. [Google Scholar] [CrossRef]
- Nikolić, N.; Nilson, R.; Briggs, S.; Ulven, A.J.; Tveten, A.; Forbes, S.; Pardal, C.V.; Viruly, L.; Berbist, R. A medical support in offshore racing—Workshop on Medical Support for Offshore Yacht Races, Telemedical Advice Service (TMAS), 1-2 December 2018, London, United Kingdom. Int. Marit. Health 2019, 70, 27–41. [Google Scholar] [CrossRef] [Green Version]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Amenta, F.; Dauri, A.; Rizzo, N. Telemedicine and medical care to ships without a doctor on board. J. Telemed. Telecare 1998, 4, 44–45. [Google Scholar] [CrossRef]
- Bifulco, P.; Narducci, F.; Vertucci, R.; Ambruosi, P.; Cesarelli, M.; Romano, M. Telemedicine supported by Augmented Reality: An interactive guide for untrained people in performing an ECG test. Biomed. Eng. Online 2014, 13, 153. [Google Scholar] [CrossRef] [Green Version]
- Digital Divide Library and Information Science Education Network. Available online: https://www.lisedunetwork.com/digital-divide/ (accessed on 5 July 2023).
- Khan, Z.; Mlawa, G.; Yousif, Y.; Afghan, A.; Balami, D.; Mohammed, M.; Muhammad, S.; Warrier, V.; Gupta, A.; Ibrahim, M.; et al. The Future of Cross-Continental Telemedicine in the Management of Complicated Endocrine Patients and Its Suitability Based on a Case Report. Cureus 2022, 14, e22174. [Google Scholar] [CrossRef]


| N | Databases | Document Count |
|---|---|---|
| 1. | PubMed (Medline) | 316 |
| 2. | CINAHL | 8 |
| 3. | BMC | 5 |
| 4. | Google Scholar | 456 |
| TMAS Centre | Location and Country | Means of Communication |
|---|---|---|
| Med solutions international | New York, USA | |
| RMN | Bergen, Norway | Telephone |
| CCMM | Toulouse, France | Radiotelegraphy, Telephone |
| UCMTM | Gdynia, Poland | Telephone and Email |
| RMD | Esbjerg, Denmark | Radio |
| C.I.R.M. | Rome, Italy | Telephone, Email, and Web applications |
| Study Type | Sample | Year | Medical Advice | Observations | Ref |
|---|---|---|---|---|---|
| Descriptive | 551 | 2016 | Management of cardiac symptoms | Pre-employment medical examinations improved preventive measures. | [21] |
| Observational | 169 | 2017 | Emergency helicopter evacuations (helivacs) between the two ferries | Every two weeks, one person was airlifted. The majority of Halifax was heart-related, with more cardiac cases airlifted than ambulances | [17] |
| Case study | 5 | 2017 | Diagnoses and follows up on medical conditions were carried out | In the development of telemedical technologies, the participants demonstrate a continual interest in teleconsultations with photographs | [23] |
| Observational | 225 | 2019 | Ensure permanent access to medical advice for seafarers | Providing medical assistance for various medical problems to seafarers requires close multidisciplinary cooperation between medical officers. | [18] |
| Retrospective cohort | 1401 | 2019 | Medical advice for injuries among seafarers | Danish-flagged merchant ships carry an increased risk of injuries to non-officers and European seafarers. | [22] |
| Retrospective | 11,481 | 2020 | Proposing prevention measures in COVID-19 Control | Fever, sore throats, and shortness of breath appeared to be more common during Coronavirus outbreaks | [8] |
| Epidemiological | 423 | 2021 | Assistance to control injuries and diseases among seafarers | Non-officers reported significantly more injuries and diseases than officers | [24] |
| Cross-sectional | 420 | 2022 | Diagnosis of marine workers’ dermatological diseases | Highlighted insufficient remote management of dermatological conditions. | [19] |
| Observational | 384 | 2022 | Diagnosis of COVID-19 | Promotes social distancing and quarantine procedures at sea to limit the spread of the pandemic | [20] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Battineni, G.; Chintalapudi, N.; Gagliardi, G.; Amenta, F. The Use of Radio and Telemedicine by TMAS Centers in Provision of Medical Care to Seafarers: A Systematic Review. J. Pers. Med. 2023, 13, 1171. https://doi.org/10.3390/jpm13071171
Battineni G, Chintalapudi N, Gagliardi G, Amenta F. The Use of Radio and Telemedicine by TMAS Centers in Provision of Medical Care to Seafarers: A Systematic Review. Journal of Personalized Medicine. 2023; 13(7):1171. https://doi.org/10.3390/jpm13071171
Chicago/Turabian StyleBattineni, Gopi, Nalini Chintalapudi, Giulio Gagliardi, and Francesco Amenta. 2023. "The Use of Radio and Telemedicine by TMAS Centers in Provision of Medical Care to Seafarers: A Systematic Review" Journal of Personalized Medicine 13, no. 7: 1171. https://doi.org/10.3390/jpm13071171








