Non-Invasive Estimation of Central Systolic Blood Pressure by Radial Tonometry: A Simplified Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Collection of Clinical and Laboratory Parameters
2.2. Hemodynamic Parameters
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Vlachopoulos, C.; Aznaouridis, K.; O’Rourke, M.F.; Safar, M.E.; Baou, K.; Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: A systematic review and meta-analysis. Eur. Heart J. 2010, 31, 1865–1871. [Google Scholar] [CrossRef]
- Kollias, A.; Lagou, S.; Zeniodi, M.E.; Boubouchairopoulou, N.; Stergiou, G.S. Association of central versus brachial blood pressure with target-organ damage: Systematic review and meta-analysis. Hypertension 2016, 67, 183–190. [Google Scholar]
- Huang, Q.-F.; Aparicio, L.S.; Thijs, L.; Wei, F.-F.; Melgarejo, J.D.; Cheng, Y.-B.; Sheng, C.-S.; Yang, W.-Y.; Gilis-Malinowska, N.; Boggia, J.; et al. Cardiovascular End Points and Mortality Are Not Closer Associated With Central Than Peripheral Pulsatile Blood Pressure Components. Hypertension 2020, 76, 350–358. [Google Scholar] [CrossRef]
- Laugesen, E.; Knudsen, S.T.; Hansen, K.W.; Rossen, N.B.; Jensen, L.O.; Hansen, M.S.; Lone, A.; Kristian, T.; Hannei, S.; Morten, B.; et al. Invasive aortic pulse pressure is not superior to cuff pulse pressure in cardiovascular risk prediction. J. Hypertens. 2021, 39, 607–613. [Google Scholar] [CrossRef]
- Pusterla, L.; Radovanovic, D.; Muggli, F.; Erne, P.; Schoenenberger, A.W.; Schoenenberger-Berzins, R.; Parati, G.; Suter, P.; Lava, S.A.G.; Gallino, A.; et al. Impact of Cardiovascular Risk Factors on Arterial Stiffness in a Countryside Area of Switzerland: Insights from the Swiss Longitudinal Cohort Study. Cardiol. Ther. 2022, 11, 545–557. [Google Scholar] [CrossRef]
- Agnoletti, D. Arterial pulsatility: The undisclosed driver of microvascular impairment? J. Hypertens. 2017, 35, 248–249. [Google Scholar]
- Millasseau, S.; Agnoletti, D. Non-invasive Estimation of Aortic Blood Pressures: A Close Look at Current Devices and Methods. Curr. Pharm. Des. 2014, 21, 709–718. [Google Scholar] [CrossRef]
- Stergiou, G.S.; Parati, G.; Vlachopoulos, C.; Achimastos, A.; Andreadis, E.; Asmar, R.; Avolio, A.; Benetos, A.; Bilo, G.; Boubouchairopoulou, N.; et al. Methodology and technology for peripheral and central blood pressure and blood pressure variability measurement: Current status and future directions—Position statement of the European Society of Hypertension Working Group on blood pressure monitoring and cardiovascular varia-bility. J. Hypertens. 2016, 34, 1665–1677. [Google Scholar]
- Pauca, A.L.; O’rourke, M.F.; Kon, N.D. Prospective Evaluation of a Method for Estimating Ascending Aortic Pressure From the Radial Artery Pressure Waveform. Hypertension 2001, 38, 932–937. [Google Scholar] [CrossRef]
- O’rourke, M.F.; Adji, A. Basis for use of central blood pressure measurement in office clinical practice. J. Am. Soc. Hypertens. 2008, 2, 28–38. [Google Scholar] [CrossRef]
- Sharman, J.E.; Avolio, A.P.; Baulmann, J.; Benetos, A.; Blacher, J.; Blizzard, C.L.; Boutouyrie, P.; Chen, C.-H.; Chowienczyk, P.; Cockcroft, J.R.; et al. Validation of non-invasive central blood pressure devices: ARTERY Society task force consensus statement on protocol standardization. Eur. Heart J. 2017, 38, 2805–2812. [Google Scholar] [CrossRef]
- Chemla, D.; Millasseau, S.; Hamzaoui, O.; Teboul, J.-L.; Monnet, X.; Michard, F.; Jozwiak, M. New Method to Estimate Central Systolic Blood Pressure From Peripheral Pressure: A Proof of Concept and Validation Study. Front. Cardiovasc. Med. 2021, 8, 772613. [Google Scholar] [CrossRef]
- Chemla, D.; Antony, I.; Zamani, K.; Nitenberg, A. Mean aortic pressure is the geometric mean of systolic and diastolic aortic pressure in resting humans. J. Appl. Physiol. 2005, 99, 2278–2284. [Google Scholar] [CrossRef]
- Kelly, R.P.; Gibs, H.H.; O’Rourke, M.F.; Daley, J.E.; Mang, K.; Morgen, J.J.; Avolid, A.P. Nitroglycerin has more favourable effects on left ventricular afterload than apparent from measurement of pressure in a peripheral artery. Eur. Heart J. 1990, 11, 138–144. [Google Scholar] [CrossRef]
- Nichols, W.W.; O’Rourke, M.F.; Vlachopoulos, C. McDonald’s Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles; Hodder Arnold: London, UK, 2011. [Google Scholar]
- Sung, S.-H.; Cheng, H.-M.; Chuang, S.-Y.; Shih, Y.-T.; Wang, K.-L.; Chen, Y.-H.; Lin, S.-J.; Yu, W.-C.; Chen, C.-H. Measurement of Central Systolic Blood Pressure by Pulse Volume Plethysmography With a Noninvasive Blood Pressure Monitor. Am. J. Hypertens. 2012, 25, 542–548. [Google Scholar] [CrossRef]
- Chemla, D.; Millasseau, S. A systematic review of invasive, high-fidelity pressure studies documenting the amplification of blood pressure from the aorta to the brachial and radial arteries. J. Clin. Monit. Comput. 2020, 35, 1245–1252. [Google Scholar] [CrossRef]
- Agnoletti, D.; Zhang, Y.; Salvi, P.; Borghi, C.; Topouchian, J.; Safar, M.E.; Blacher, J. Pulse pressure amplification, pressure waveform calibration and clinical applications. Atherosclerosis 2012, 224, 108–112. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Ogedegbe, G.; Pickering, T. Principles and Techniques of Blood Pressure Measurement. Cardiol. Clin. 2010, 28, 571–586. [Google Scholar] [CrossRef]
- Vera-Cala, L.M.; Orostegui, M.; Valencia-Angel, L.I.; López, N.; Bautista, L.E. Accuracy of the Omron HEM-705 CP for blood pressure measurement in large epidemiologic studies. Arq. Bras. Cardiol. 2011, 96, 393–398. [Google Scholar] [CrossRef]
- ANSI/AAMI/ISO 81060-2:2009; Association for the Advancement of Medical Instrumentation. American National Standard Non-Invasive Sphygmomanometers—Part 2: Clinical Validation of Automated Measurement Type. AAMI: Arlington, MA, USA, 2009.
- O’brien, E.; Pickering, T.; Asmar, R.; Myers, M.; Parati, G.; Staessen, J.; Mengden, T.; Imai, Y.; Waeber, B.; Palatini, P.; et al. Working Group on Blood Pressure Monitoring of the European Society of Hypertension International Protocol for validation of blood pressure measuring devices in adults. Blood Press. Monit. 2002, 7, 3–17. [Google Scholar] [CrossRef]
- Cheng, H.-M.; Lang, D.; Tufanaru, C.; Pearson, A. Measurement accuracy of non-invasively obtained central blood pressure by applanation tonometry: A systematic review and meta-analysis. Int. J. Cardiol. 2013, 167, 1867–1876. [Google Scholar] [CrossRef]
- Papaioannou, T.G.; Karageorgopoulou, T.D.; Sergentanis, T.N.; Protogerou, A.D.; Psaltopoulou, T.; Sharman, J.E.; Weber, T.; Blacher, J.; Daskalopoulou, S.S.; Wassertheurer, S.; et al. Accuracy of commercial devices and methods for noninvasive estimation of aortic systolic blood pressure a systematic review and meta-analysis of invasive validation studies. J. Hypertens. 2016, 34, 1237–1248. [Google Scholar] [CrossRef]
- Schultz, M.G.; Picone, D.S.; Armstrong, M.K.; Black, J.A.; Dwyer, N.; Roberts-Thomson, P.; Sturgess, D.; Sharman, J.E. The influence of SBP amplification on the accuracy of form-factor-derived mean arterial pressure. J. Hypertens. 2020, 38, 1033–1039. [Google Scholar] [CrossRef]
- Hope, S.A.; Tay, D.B.; Meredith, I.T.; Cameron, J.D. Comparison of generalized and gender-specific transfer functions for the derivation of aortic waveforms. Am. J. Physiol. Circ. Physiol. 2002, 283, H1150–H1156. [Google Scholar] [CrossRef][Green Version]
- Picone, D.S.; Schultz, M.G.; Otahal, P.; Aakhus, S.; Al-Jumaily, A.M.; Black, J.A.; Bos, W.J.; Chambers, J.B.; Chen, C.-H.; Cheng, H.-M.; et al. Accuracy of Cuff-Measured Blood Pressure: Systematic Reviews and Meta-Analyses. J. Am. Coll. Cardiol. 2017, 70, 572–586. [Google Scholar]
- Papaioannou, T.G.; Lekakis, J.P.; Karatzis, E.N.; Papamichael, C.M.; Stamatelopoulos, K.S.; Protogerou, A.D.; Mavrikakis, M.; Stefanadis, C. Transmission of calibration errors (input) by generalized transfer functions to the aortic pressures (output) at different he-modynamic states. Int. J. Cardiol. 2006, 110, 46–52. [Google Scholar]
- Segers, P.; Mahieu, D.; Kips, J.; Rietzschel, E.; De Buyzere, M.; De Bacquer, D.; Bekaert, S.; De Backer, G.; Gillebert, T.; Verdonck, P.; et al. Amplification of the pressure pulse in the upper limb in healthy, middle-aged men and women. Hypertension 2009, 54, 414–420. [Google Scholar] [CrossRef]
- Sharman, J.E.; Laurent, S. Central blood pressure in the management of hypertension: Soon reaching the goal? J. Hum. Hypertens. 2013, 27, 405–411. [Google Scholar]
| Variables | Mean ± SD |
|---|---|
| Age, years | 58 ± 15 |
| Men, n (%) | 87 (54) |
| Weight, kg | 76 ± 16 |
| Height, cm | 168 ± 10 |
| Waist circumference, cm | 94.9 ± 13.8 |
| Body mass index, kg/m2 (n = 158) | 27.2 ± 5.0 |
| Normal weight, n (%) | 57 (36.1) |
| Overweight, n (%) | 56 (35.4) |
| Obese, n (%) | 45 (28.5) |
| Clinical and biological data (n = 133) 1 | |
| Smoker, n (%) | 44 (33) |
| Antihypertensive therapy, n (%) | 105 (79) |
| Coronary heart disease, n (%) | 14 (11) |
| Diabetes mellitus, n (%) | 30 (22) |
| Stroke, n (%) | 2 (2) |
| Serum creatinine, mmol/L | 86.0 ± 29.7 |
| Variables | Mean ± SD | Range |
|---|---|---|
| Heart rate, beats/min | 68 ± 13 | 45–116 |
| Brachial SBP, mmHg | 136.4 ± 18.3 | 99–211 |
| Brachial DBP, mmHg | 80.7 ± 10.4 | 61–110 |
| Brachial PP, mmHg | 55.1 ± 13.3 | 33–101 |
| Radial MBP, mmHg | 98.6 ± 12.6 | 74–137 |
| cSBP (SphygmoCor), mmHg | 123.1 ± 18.3 | 86.0–181.0 |
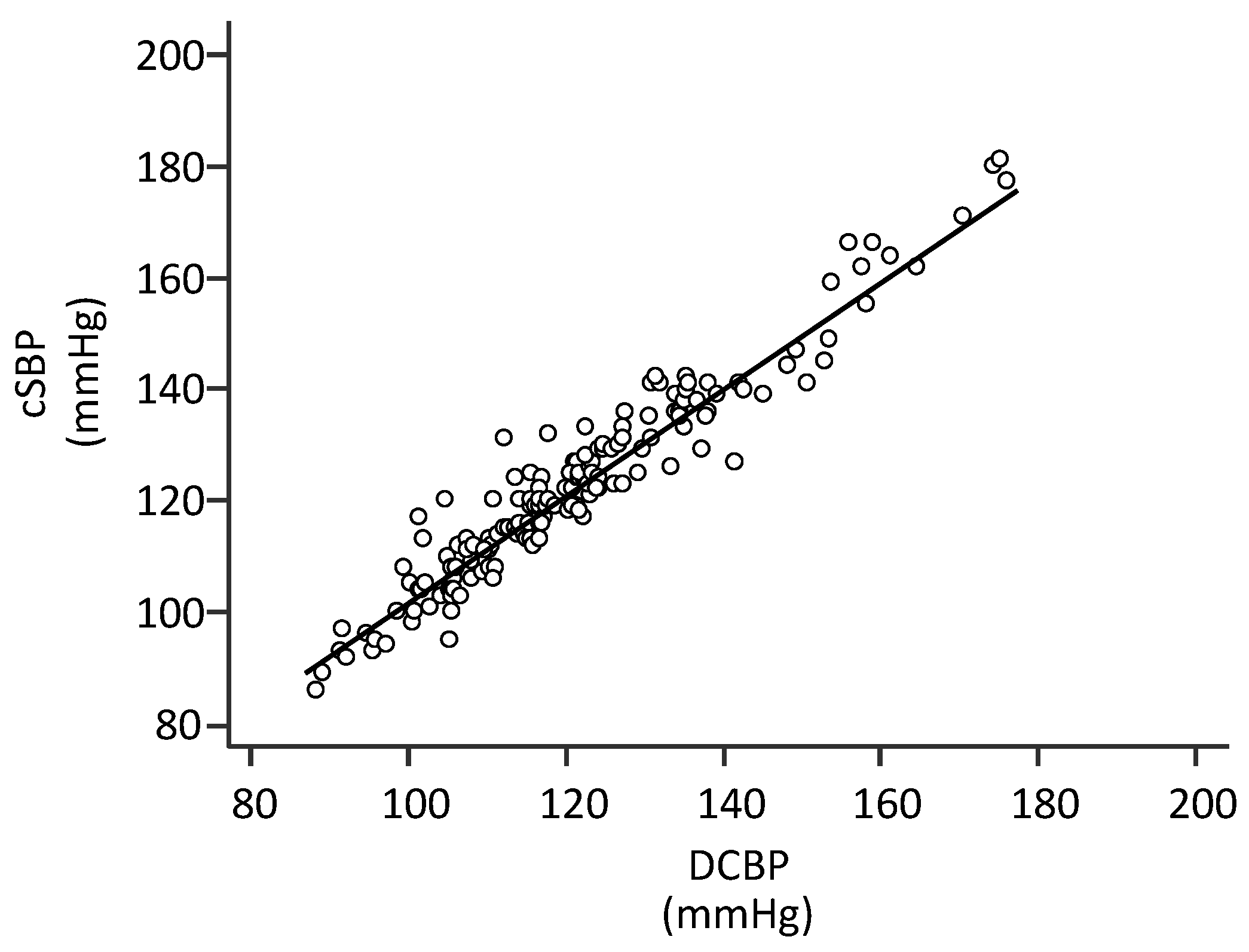
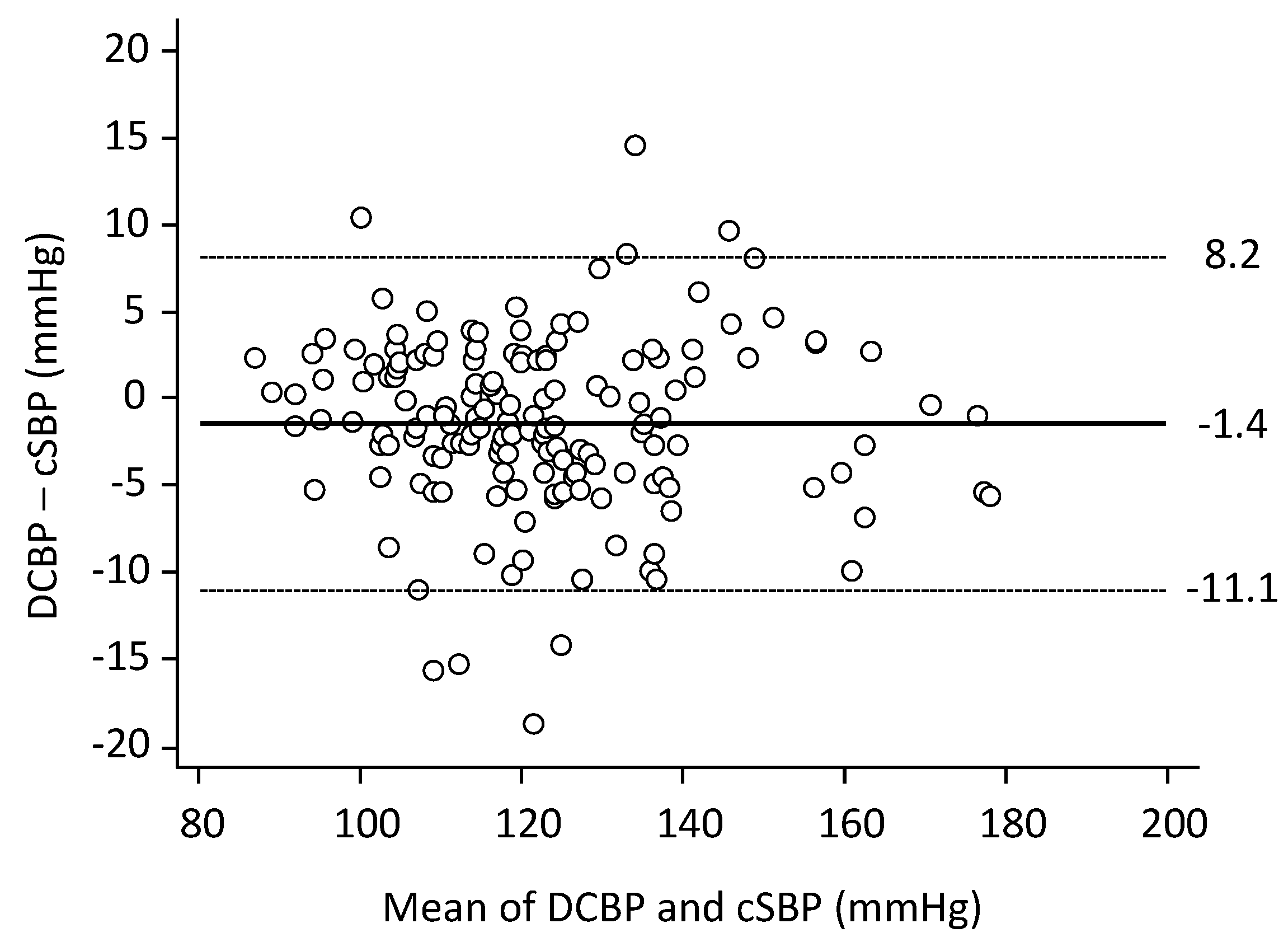
| DCBP, mmHg | 121.6 ± 18.1 | 88.3–176.0 |
| Error, mmHg | −1.4 ± 4.9 | −18.5–14.5 |
| Error, % | −1.1 ± 3.9 | −14.3–11.4 |
| Pulse Wave Velocity, m/s | 12.1 ± 3.2 | 6.9–23.1 |
| Sphygmocor cSBP < 130 mmHg | Sphygmocor cSBP ≥ 130 mmHg | Total % of Correctly Classified and Chi-sq Test | |
|---|---|---|---|
| DCBP < 130 mmHg | 110 | 8 | 93% p < 0.0001 |
| DCBP ≥ 130 mmHg | 3 | 39 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chemla, D.; Agnoletti, D.; Jozwiak, M.; Zhang, Y.; Protogerou, A.D.; Millasseau, S.; Blacher, J. Non-Invasive Estimation of Central Systolic Blood Pressure by Radial Tonometry: A Simplified Approach. J. Pers. Med. 2023, 13, 1244. https://doi.org/10.3390/jpm13081244
Chemla D, Agnoletti D, Jozwiak M, Zhang Y, Protogerou AD, Millasseau S, Blacher J. Non-Invasive Estimation of Central Systolic Blood Pressure by Radial Tonometry: A Simplified Approach. Journal of Personalized Medicine. 2023; 13(8):1244. https://doi.org/10.3390/jpm13081244
Chicago/Turabian StyleChemla, Denis, Davide Agnoletti, Mathieu Jozwiak, Yi Zhang, Athanase D. Protogerou, Sandrine Millasseau, and Jacques Blacher. 2023. "Non-Invasive Estimation of Central Systolic Blood Pressure by Radial Tonometry: A Simplified Approach" Journal of Personalized Medicine 13, no. 8: 1244. https://doi.org/10.3390/jpm13081244
APA StyleChemla, D., Agnoletti, D., Jozwiak, M., Zhang, Y., Protogerou, A. D., Millasseau, S., & Blacher, J. (2023). Non-Invasive Estimation of Central Systolic Blood Pressure by Radial Tonometry: A Simplified Approach. Journal of Personalized Medicine, 13(8), 1244. https://doi.org/10.3390/jpm13081244








