The Use of Artificial Intelligence in Head and Neck Cancers: A Multidisciplinary Survey
Abstract
1. Introduction
2. Materials and Methods
Survey Content and Data Elaboration
3. Results
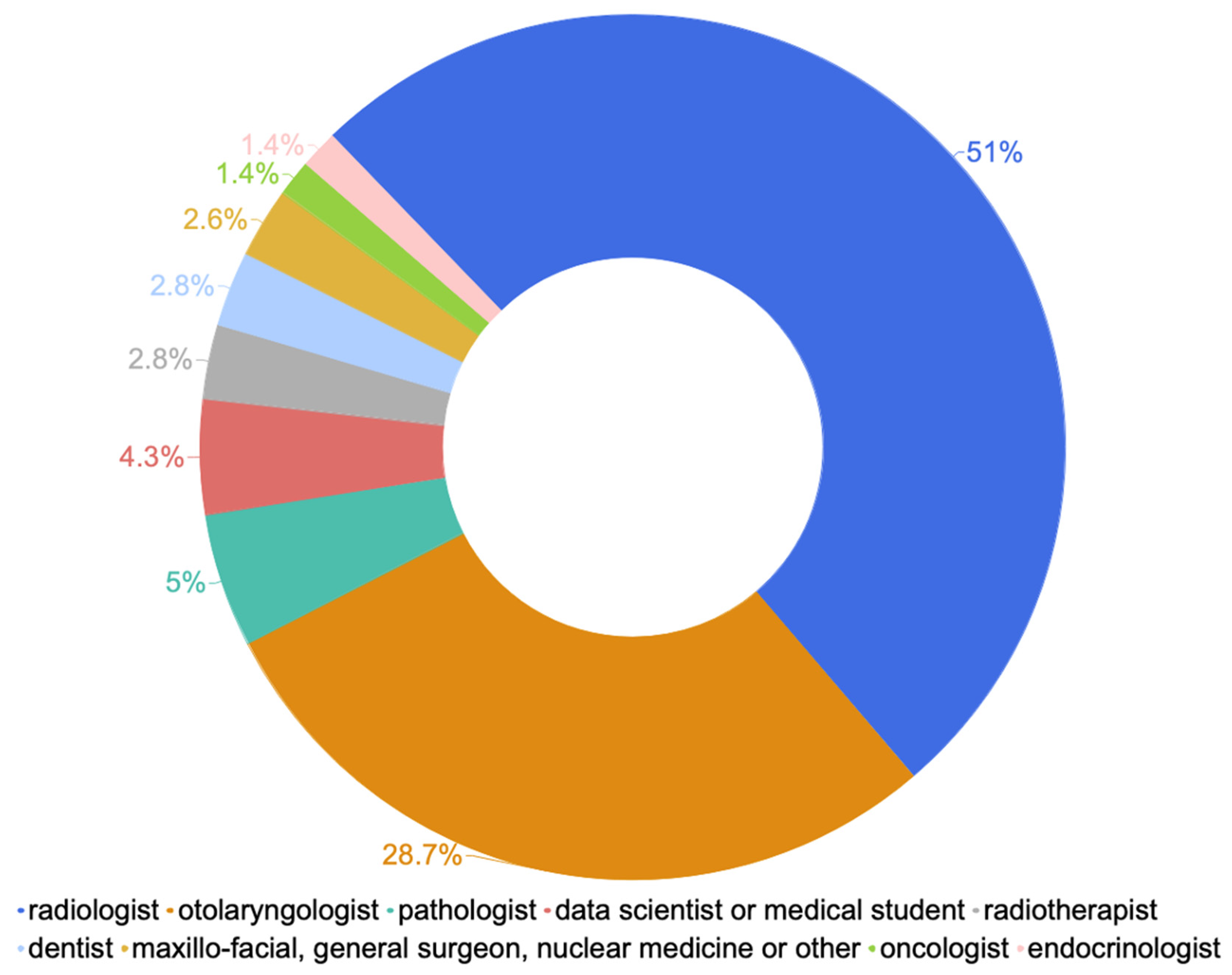
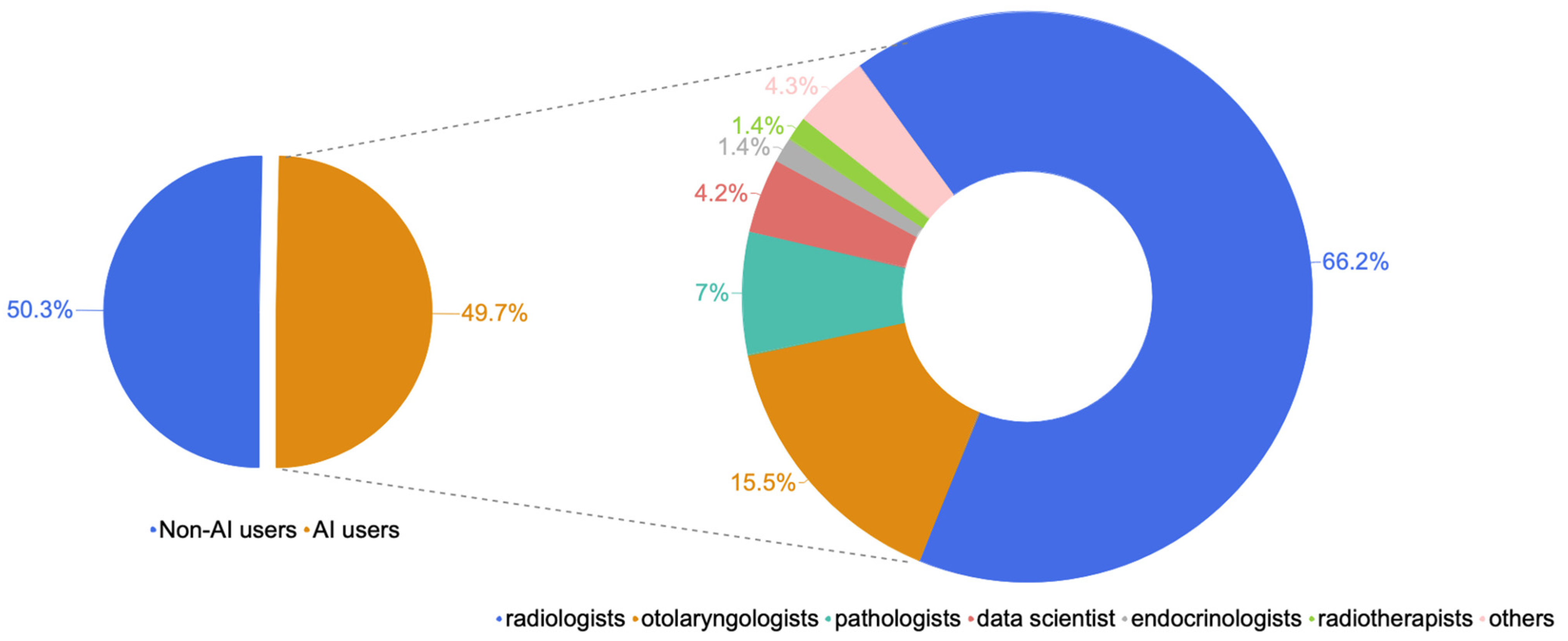
3.1. Sociodemographic Characteristics and Professional Profiles
3.2. Knowledge and Factors Associated with Use of Artificial Intelligence
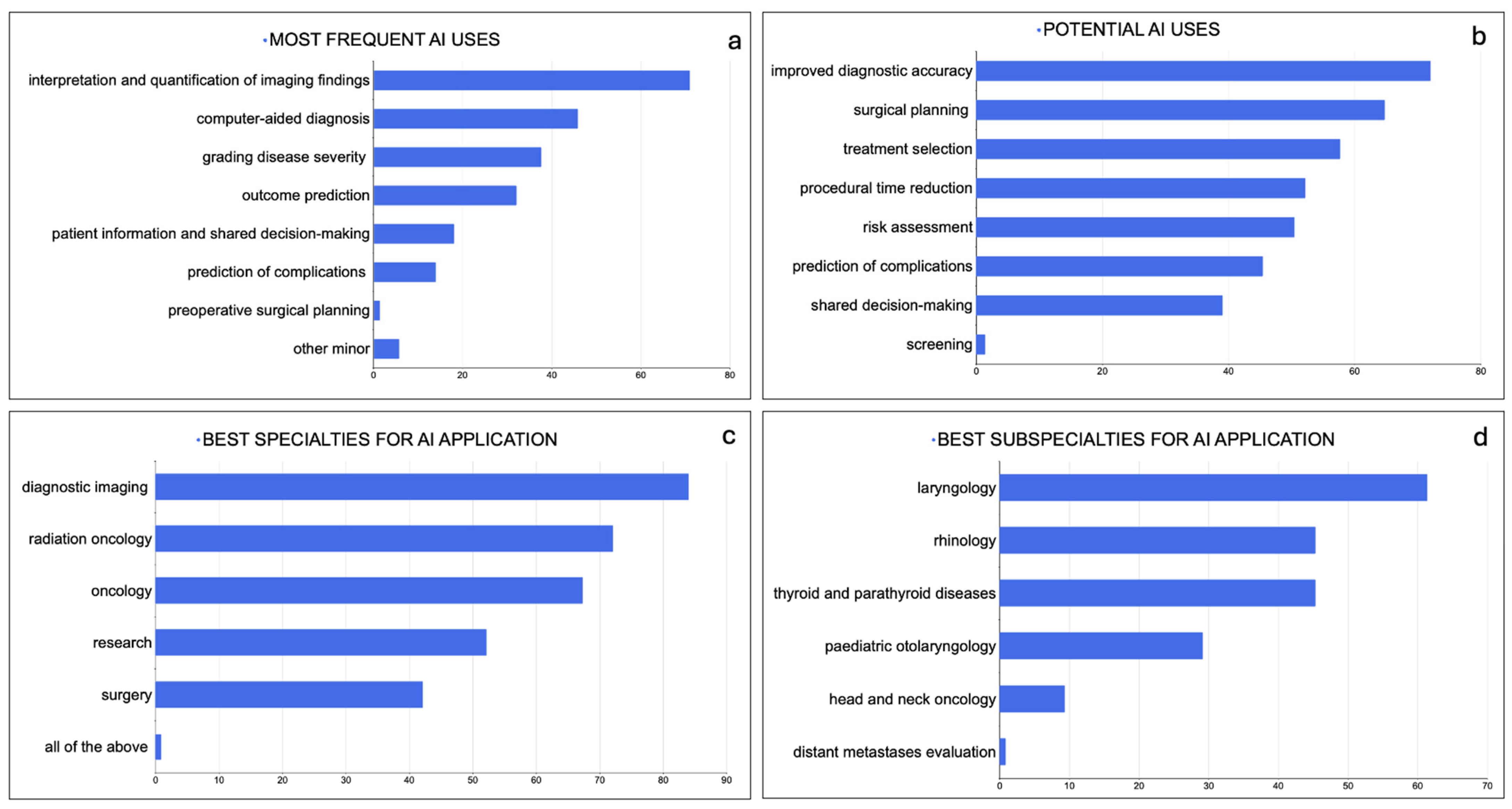
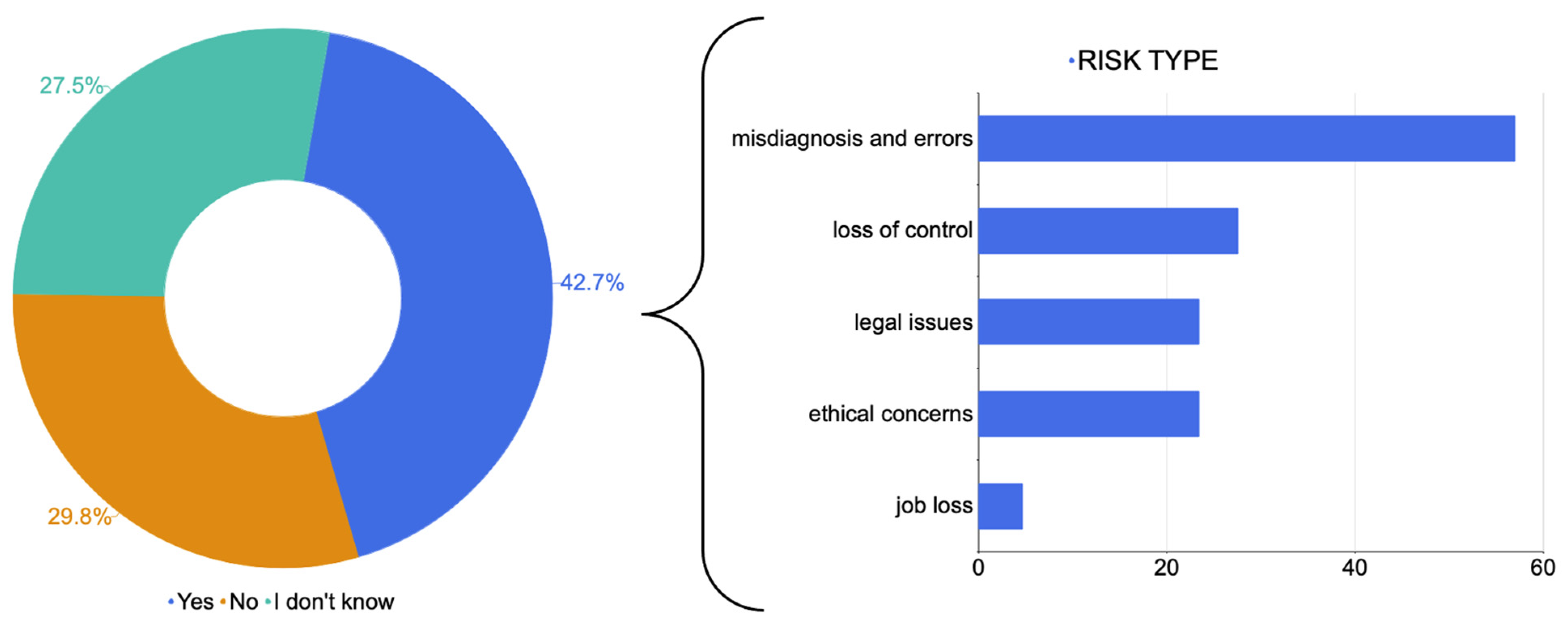
3.3. Applications, Concerns and Perceived Importance of Artificial Intelligence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kawakita, D.; Oze, I.; Iwasaki, S.; Matsuda, T.; Matsuo, K.; Ito, H. Trends in the incidence of head and neck cancer by subsite between 1993 and 2015 in Japan. Cancer Med. 2022, 11, 1553–1560. [Google Scholar] [CrossRef] [PubMed]
- Mody, M.D.; Rocco, J.W.; Yom, S.S.; Haddad, R.I.; Saba, N.F. Head and neck cancer. Lancet 2021, 398, 2289–2299. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Gormley, M.; Creaney, G.; Schache, A.; Ingarfield, K.; Conway, D.I. Reviewing the epidemiology of head and neck cancer: Definitions, trends and risk factors. Br. Dent. J. 2022, 233, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Cramer, J.D.; Burtness, B.; Le, Q.T.; Ferris, R.L. The changing therapeutic landscape of head and neck cancer. Nat. Rev. Clin. Oncol. 2019, 16, 669–683. [Google Scholar] [CrossRef]
- Caudell, J.J.; Gillison, M.L.; Maghami, E.; Spencer, S.; Pfister, D.G.; Adkins, D.; Birkeland, A.C.; Brizel, D.M.; Busse, P.M.; Cmelak, A.J.; et al. NCCN Guidelines® Insights: Head and Neck Cancers, Version 1.2022. J. Natl. Compr. Cancer Netw. 2022, 20, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.E.; Burtness, B.; Leemans, C.R.; Lui, V.W.Y.; Bauman, J.E.; Grandis, J.R. Head and neck squamous cell carcinoma. Nat. Rev. Dis. Primers 2020, 6, 92. [Google Scholar] [CrossRef]
- Kann, B.H.; Hosny, A.; Aerts, H. Artificial intelligence for clinical oncology. Cancer Cell 2021, 39, 916–927. [Google Scholar] [CrossRef]
- Angus, D.C. Fusing Randomized Trials with Big Data: The Key to Self-learning Health Care Systems? JAMA 2015, 314, 767–768. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, D.A.; Rosman, G.; Rus, D.; Meireles, O.R. Artificial Intelligence in Surgery: Promises and Perils. Ann. Surg. 2018, 268, 70–76. [Google Scholar] [CrossRef]
- Luchini, C.; Pea, A.; Scarpa, A. Artificial intelligence in oncology: Current applications and future perspectives. Br. J. Cancer 2022, 126, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, R.; Long, J.; Longacre, T.; Peng, L.; Berry, G.; Martin, B.; Higgins, J.; Rubin, D.L.; Shen, J. Deep learning model for the prediction of microsatellite instability in colorectal cancer: A diagnostic study. Lancet Oncol. 2021, 22, 132–141. [Google Scholar] [CrossRef]
- Mahmood, H.; Shaban, M.; Rajpoot, N.; Khurram, S.A. Artificial Intelligence-based methods in head and neck cancer diagnosis: An overview. Br. J. Cancer 2021, 124, 1934–1940. [Google Scholar] [CrossRef] [PubMed]
- Giannitto, C.; Mercante, G.; Ammirabile, A.; Cerri, L.; De Giorgi, T.; Lofino, L.; Vatteroni, G.; Casiraghi, E.; Marra, S.; Esposito, A.A.; et al. Radiomics-based machine learning for the diagnosis of lymph node metastases in patients with head and neck cancer: Systematic review. Head Neck 2023, 45, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Abdel Razek, A.A.K.; Khaled, R.; Helmy, E.; Naglah, A.; AbdelKhalek, A.; El-Baz, A. Artificial Intelligence and Deep Learning of Head and Neck Cancer. Magn. Reson. Imaging Clin. N. Am. 2022, 30, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Lin, B.; Tan, Z.; Mo, Y.; Yang, X.; Liu, Y.; Xu, B. Intelligent oncology: The convergence of artificial intelligence and oncology. J. Natl. Cancer Cent. 2023, 3, 83–91. [Google Scholar] [CrossRef]
- Crowson, M.G.; Ranisau, J.; Eskander, A.; Babier, A.; Xu, B.; Kahmke, R.R.; Chen, J.M.; Chan, T.C.Y. A contemporary review of machine learning in otolaryngology-head and neck surgery. Laryngoscope 2020, 130, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Artino, A.R., Jr.; Durning, S.J.; Sklar, D.P. Guidelines for Reporting Survey-Based Research Submitted to Academic Medicine. Acad. Med. 2018, 93, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Bur, A.M.; Shew, M.; New, J. Artificial Intelligence for the Otolaryngologist: A State of the Art Review. Otolaryngol. Head. Neck Surg. 2019, 160, 603–611. [Google Scholar] [CrossRef]
- Pakdemirli, E.; Wegner, U. Artificial Intelligence in Various Medical Fields with Emphasis on Radiology: Statistical Evaluation of the Literature. Cureus 2020, 12, e10961. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Vu, G.T.; Ha, G.H.; Vuong, Q.H.; Ho, M.T.; Vuong, T.T.; La, V.P.; Ho, M.T.; Nghiem, K.P.; Nguyen, H.L.T.; et al. Global Evolution of Research in Artificial Intelligence in Health and Medicine: A Bibliometric Study. J. Clin. Med. 2019, 8, 360. [Google Scholar] [CrossRef] [PubMed]
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The role of artificial intelligence in healthcare: A structured literature review. BMC Med. Inform. Decis. Mak. 2021, 21, 125. [Google Scholar] [CrossRef]
- Wu, T.; Duan, Y.; Zhang, T.; Tian, W.; Liu, H.; Deng, Y. Research Trends in the Application of Artificial Intelligence in Oncology: A Bibliometric and Network Visualization Study. Front. Biosci. Landmark Ed. 2022, 27, 254. [Google Scholar] [CrossRef]
- Wong, C. AI ‘fairness’ research held back by lack of diversity. Nature 2023. ahead of print. [Google Scholar] [CrossRef]
- Sauerbrei, A.; Kerasidou, A.; Lucivero, F.; Hallowell, N. The impact of artificial intelligence on the person-centred, doctor-patient relationship: Some problems and solutions. BMC Med. Inform. Decis. Mak. 2023, 23, 73. [Google Scholar] [CrossRef] [PubMed]
- Standiford, T.C.; Farlow, J.L.; Brenner, M.J.; Conte, M.L.; Terrell, J.E. Clinical Decision Support Systems in Otolaryngology-Head and Neck Surgery: A State of the Art Review. Otolaryngol. Head Neck Surg. 2022, 166, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Howard, F.M.; Kochanny, S.; Koshy, M.; Spiotto, M.; Pearson, A.T. Machine Learning-Guided Adjuvant Treatment of Head and Neck Cancer. JAMA Netw. Open 2020, 3, e2025881. [Google Scholar] [CrossRef] [PubMed]
- Leijenaar, R.T.; Bogowicz, M.; Jochems, A.; Hoebers, F.J.; Wesseling, F.W.; Huang, S.H.; Chan, B.; Waldron, J.N.; O’Sullivan, B.; Rietveld, D.; et al. Development and validation of a radiomic signature to predict HPV (p16) status from standard CT imaging: A multicenter study. Br. J. Radiol. 2018, 91, 20170498. [Google Scholar] [CrossRef]
- Suh, C.H.; Lee, K.H.; Choi, Y.J.; Chung, S.R.; Baek, J.H.; Lee, J.H.; Yun, J.; Ham, S.; Kim, N. Oropharyngeal squamous cell carcinoma: Radiomic machine-learning classifiers from multiparametric MR images for determination of HPV infection status. Sci. Rep. 2020, 10, 17525. [Google Scholar] [CrossRef]
- Bogowicz, M.; Tanadini-Lang, S.; Guckenberger, M.; Riesterer, O. Combined CT radiomics of primary tumor and metastatic lymph nodes improves prediction of loco-regional control in head and neck cancer. Sci. Rep. 2019, 9, 15198. [Google Scholar] [CrossRef]
- Yu, K.; Zhang, Y.; Yu, Y.; Huang, C.; Liu, R.; Li, T.; Yang, L.; Morris, J.S.; Baladandayuthapani, V.; Zhu, H. Radiomic analysis in prediction of Human Papilloma Virus status. Clin. Transl. Radiat. Oncol. 2017, 7, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Babier, A.; Mahmood, R.; McNiven, A.L.; Diamant, A.; Chan, T.C.Y. Knowledge-based automated planning with three-dimensional generative adversarial networks. Med. Phys. 2020, 47, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Babier, A.; Boutilier, J.J.; Sharpe, M.B.; McNiven, A.L.; Chan, T.C.Y. Inverse optimization of objective function weights for treatment planning using clinical dose-volume histograms. Phys. Med. Biol. 2018, 63, 105004. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, C.; Conroy, L.; Tjong, M.C.; Craig, T.; Bayley, A.; Catton, C.; Gospodarowicz, M.; Helou, J.; Isfahanian, N.; Kong, V.; et al. Clinical integration of machine learning for curative-intent radiation treatment of patients with prostate cancer. Nat. Med. 2021, 27, 999–1005. [Google Scholar] [CrossRef] [PubMed]
- Osapoetra, L.O.; Dasgupta, A.; DiCenzo, D.; Fatima, K.; Quiaoit, K.; Saifuddin, M.; Karam, I.; Poon, I.; Husain, Z.; Tran, W.T.; et al. Assessment of clinical radiosensitivity in patients with head-neck squamous cell carcinoma from pre-treatment quantitative ultrasound radiomics. Sci. Rep. 2021, 11, 6117. [Google Scholar] [CrossRef] [PubMed]
- Cavalieri, S.; De Cecco, L.; Brakenhoff, R.H.; Serafini, M.S.; Canevari, S.; Rossi, S.; Lanfranco, D.; Hoebers, F.J.P.; Wesseling, F.W.R.; Keek, S.; et al. Development of a multiomics database for personalized prognostic forecasting in head and neck cancer: The Big Data to Decide EU Project. Head Neck 2021, 43, 601–612. [Google Scholar] [CrossRef]
- Jiang, J.; Li, J.; Yunxia, Z.; Zhu, H.; Liu, J.; Pumill, C. The role of prostatitis in prostate cancer: Meta-analysis. PLoS ONE 2013, 8, e85179. [Google Scholar] [CrossRef]
- Tsutsumi, K.; Soltanzadeh-Zarandi, S.; Khosravi, P.; Goshtasbi, K.; Djalilian, H.R.; Abouzari, M. Machine Learning in the Management of Lateral Skull Base Tumors: A Systematic Review. J. Otorhinolaryngol. Hear. Balance Med. 2022, 3, 7. [Google Scholar] [CrossRef]
- Rokhshad, R.; Keyhan, S.O.; Yousefi, P. Artificial intelligence applications and ethical challenges in oral and maxillo-facial cosmetic surgery: A narrative review. Maxillofac. Plast. Reconstr. Surg. 2023, 45, 14. [Google Scholar] [CrossRef]
- Amodei, D.; Olah, C.; Steinhardt, J.; Christiano, P.F.; Schulman, J.; Mané, D. Concrete Problems in AI Safety. arXiv 2016, arXiv:1606.06565. [Google Scholar]
- Yu, K.H.; Kohane, I.S. Framing the challenges of artificial intelligence in medicine. BMJ Qual. Saf. 2019, 28, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.; Bubeck, S.; Petro, J. Benefits, Limits, and Risks of GPT-4 as an AI Chatbot for Medicine. N. Engl. J. Med. 2023, 388, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Ganapathi, S.; Duggal, S. Exploring the experiences and views of doctors working with Artificial Intelligence in English healthcare; a qualitative study. PLoS ONE 2023, 18, e0282415. [Google Scholar] [CrossRef]
- Habli, I.; Lawton, T.; Porter, Z. Artificial intelligence in health care: Accountability and safety. Bull. World Health Organ. 2020, 98, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Naik, N.; Hameed, B.M.Z.; Shetty, D.K.; Swain, D.; Shah, M.; Paul, R.; Aggarwal, K.; Ibrahim, S.; Patil, V.; Smriti, K.; et al. Legal and Ethical Consideration in Artificial Intelligence in Healthcare: Who Takes Responsibility? Front. Surg. 2022, 9, 862322. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.P.; Smith, C.; Curtis, S.; Watson, S.; Zhu, X.; Barry, B.; Sharp, R.R. Patient apprehensions about the use of artificial intelligence in healthcare. npj Digit. Med. 2021, 4, 140. [Google Scholar] [CrossRef]
- Kostick-Quenet, K.M.; Gerke, S. AI in the hands of imperfect users. npj Digit. Med. 2022, 5, 197. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giannitto, C.; Carnicelli, G.; Lusi, S.; Ammirabile, A.; Casiraghi, E.; De Virgilio, A.; Esposito, A.A.; Farina, D.; Ferreli, F.; Franzese, C.; et al. The Use of Artificial Intelligence in Head and Neck Cancers: A Multidisciplinary Survey. J. Pers. Med. 2024, 14, 341. https://doi.org/10.3390/jpm14040341
Giannitto C, Carnicelli G, Lusi S, Ammirabile A, Casiraghi E, De Virgilio A, Esposito AA, Farina D, Ferreli F, Franzese C, et al. The Use of Artificial Intelligence in Head and Neck Cancers: A Multidisciplinary Survey. Journal of Personalized Medicine. 2024; 14(4):341. https://doi.org/10.3390/jpm14040341
Chicago/Turabian StyleGiannitto, Caterina, Giorgia Carnicelli, Stefano Lusi, Angela Ammirabile, Elena Casiraghi, Armando De Virgilio, Andrea Alessandro Esposito, Davide Farina, Fabio Ferreli, Ciro Franzese, and et al. 2024. "The Use of Artificial Intelligence in Head and Neck Cancers: A Multidisciplinary Survey" Journal of Personalized Medicine 14, no. 4: 341. https://doi.org/10.3390/jpm14040341
APA StyleGiannitto, C., Carnicelli, G., Lusi, S., Ammirabile, A., Casiraghi, E., De Virgilio, A., Esposito, A. A., Farina, D., Ferreli, F., Franzese, C., Frigerio, G. M., Lo Casto, A., Malvezzi, L., Lorini, L., Othman, A. E., Preda, L., Scorsetti, M., Bossi, P., Mercante, G., ... Francone, M. (2024). The Use of Artificial Intelligence in Head and Neck Cancers: A Multidisciplinary Survey. Journal of Personalized Medicine, 14(4), 341. https://doi.org/10.3390/jpm14040341








