Minimally Invasive Controlled Growing Rods for the Surgical Treatment of Early-Onset Scoliosis—A Surgical Technique Video
Abstract
1. Introduction
2. Example of Patients and the Surgical Technique
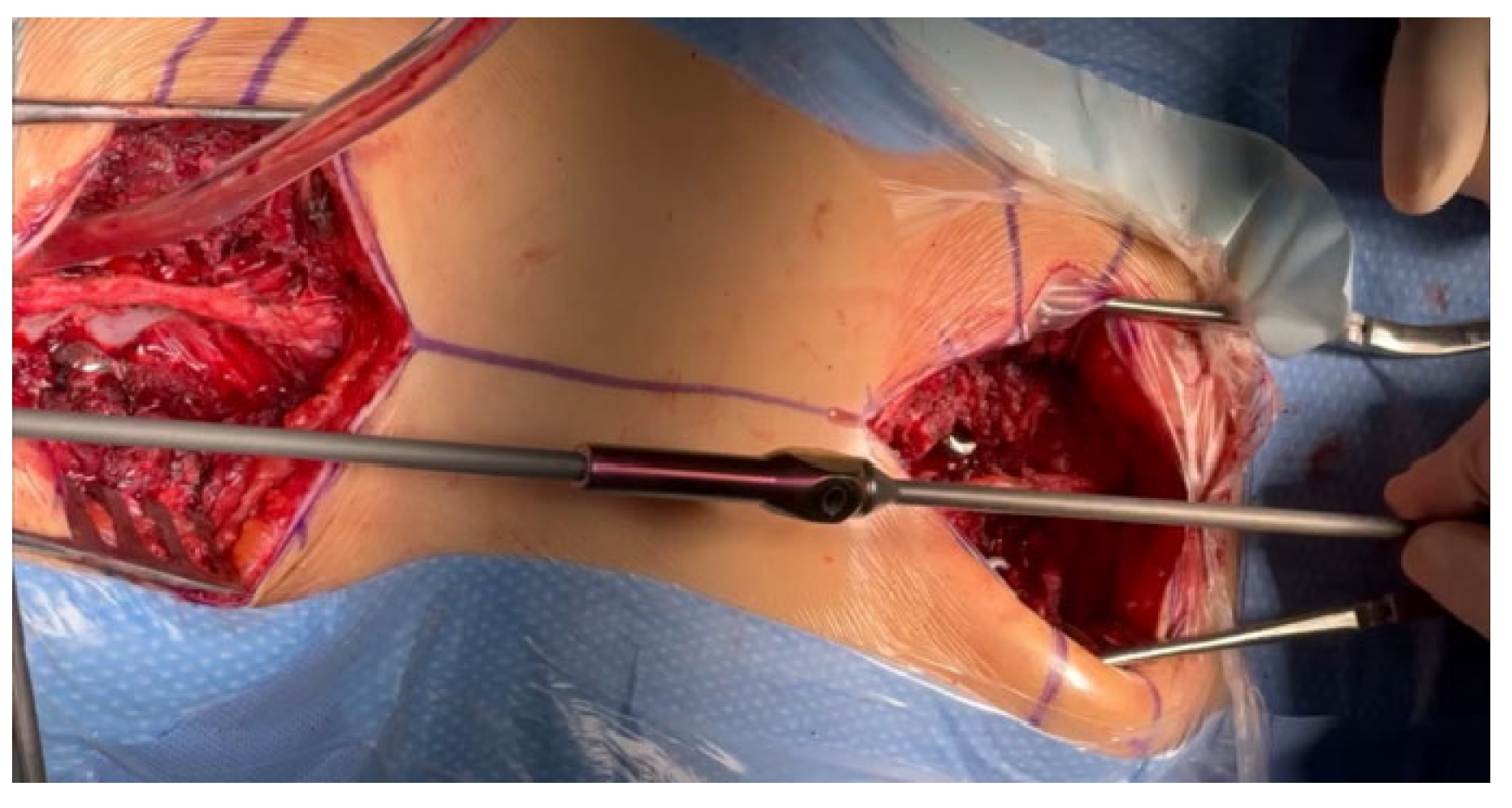
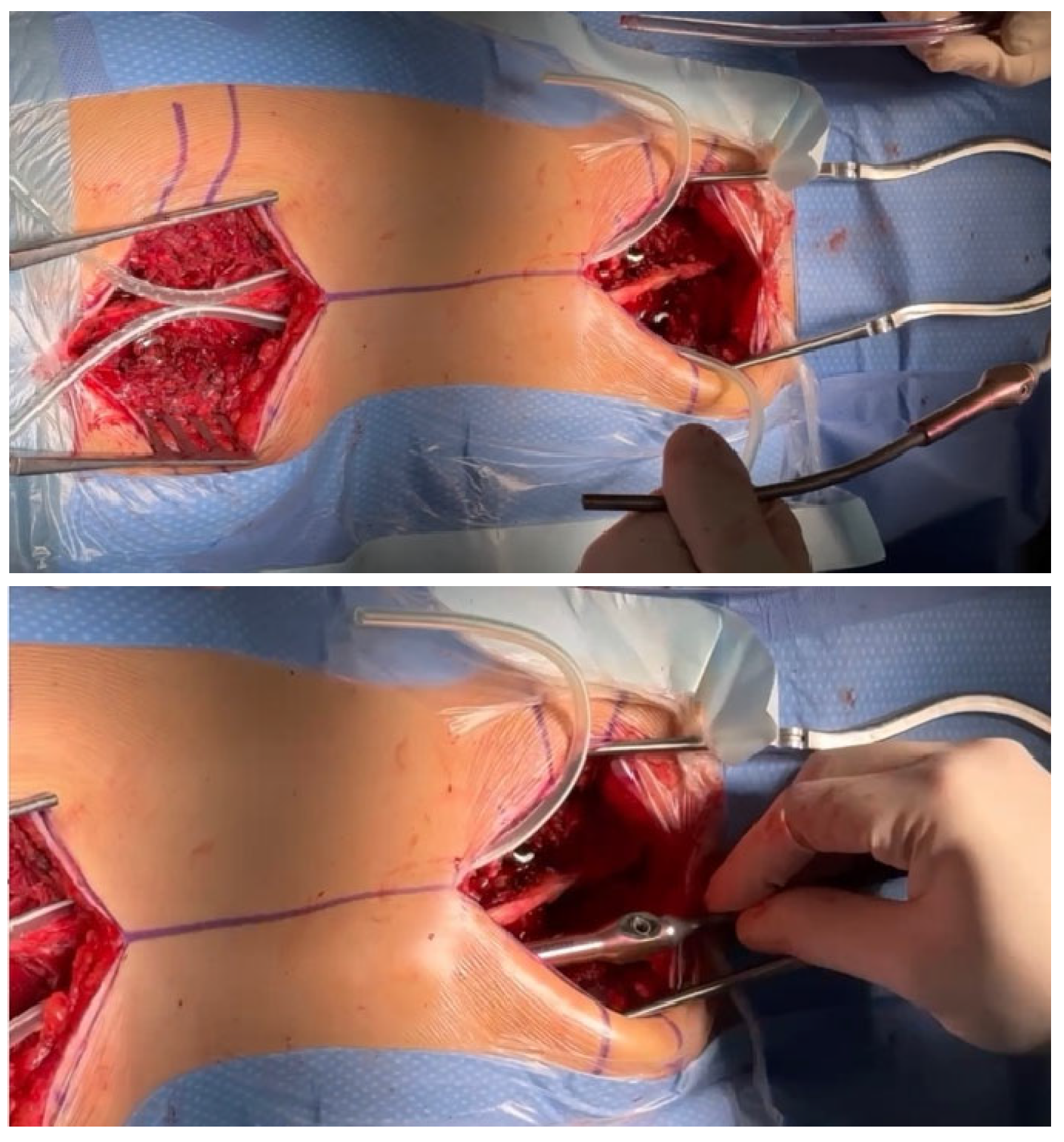
2.1. Surgical Technique
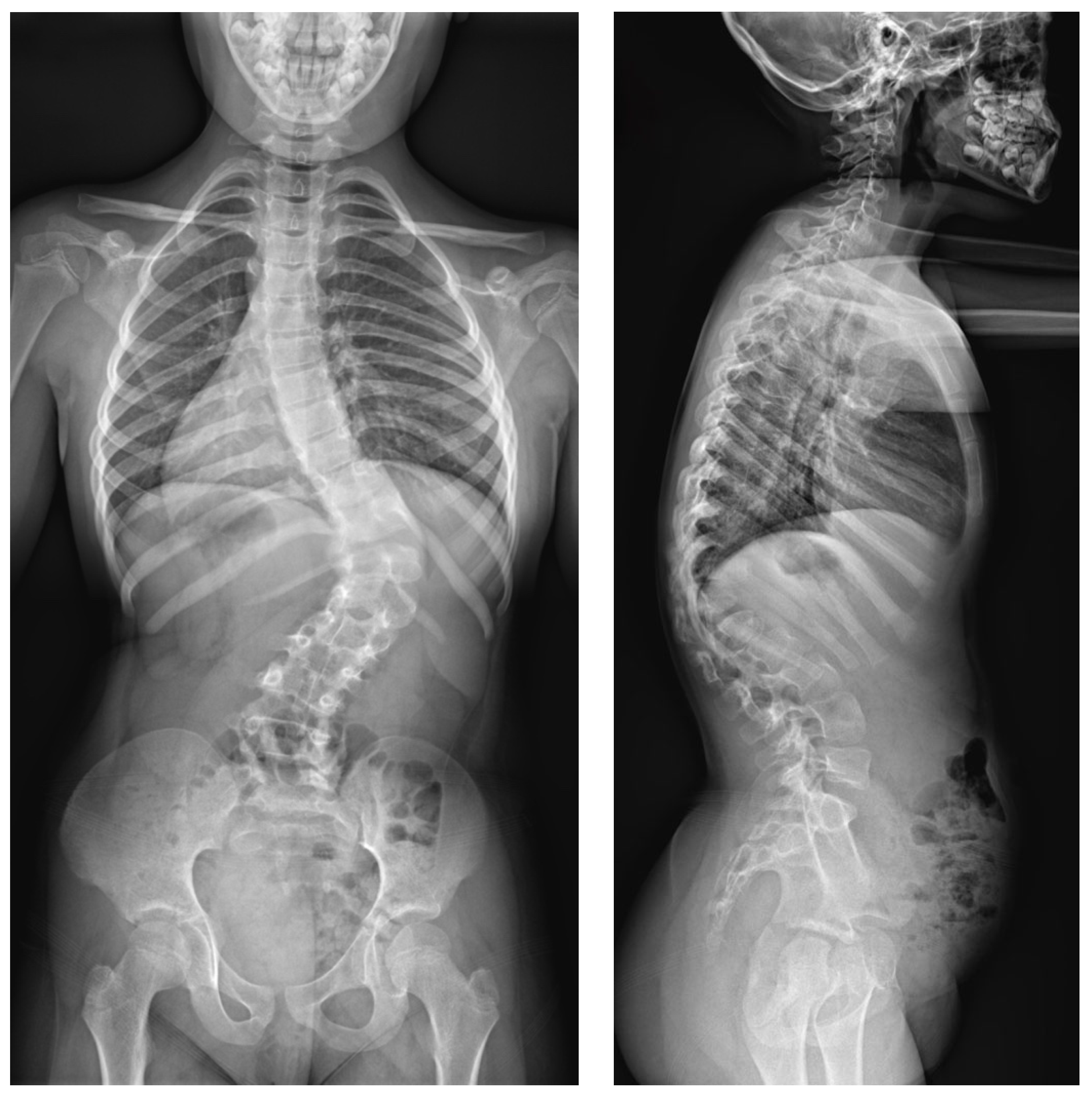
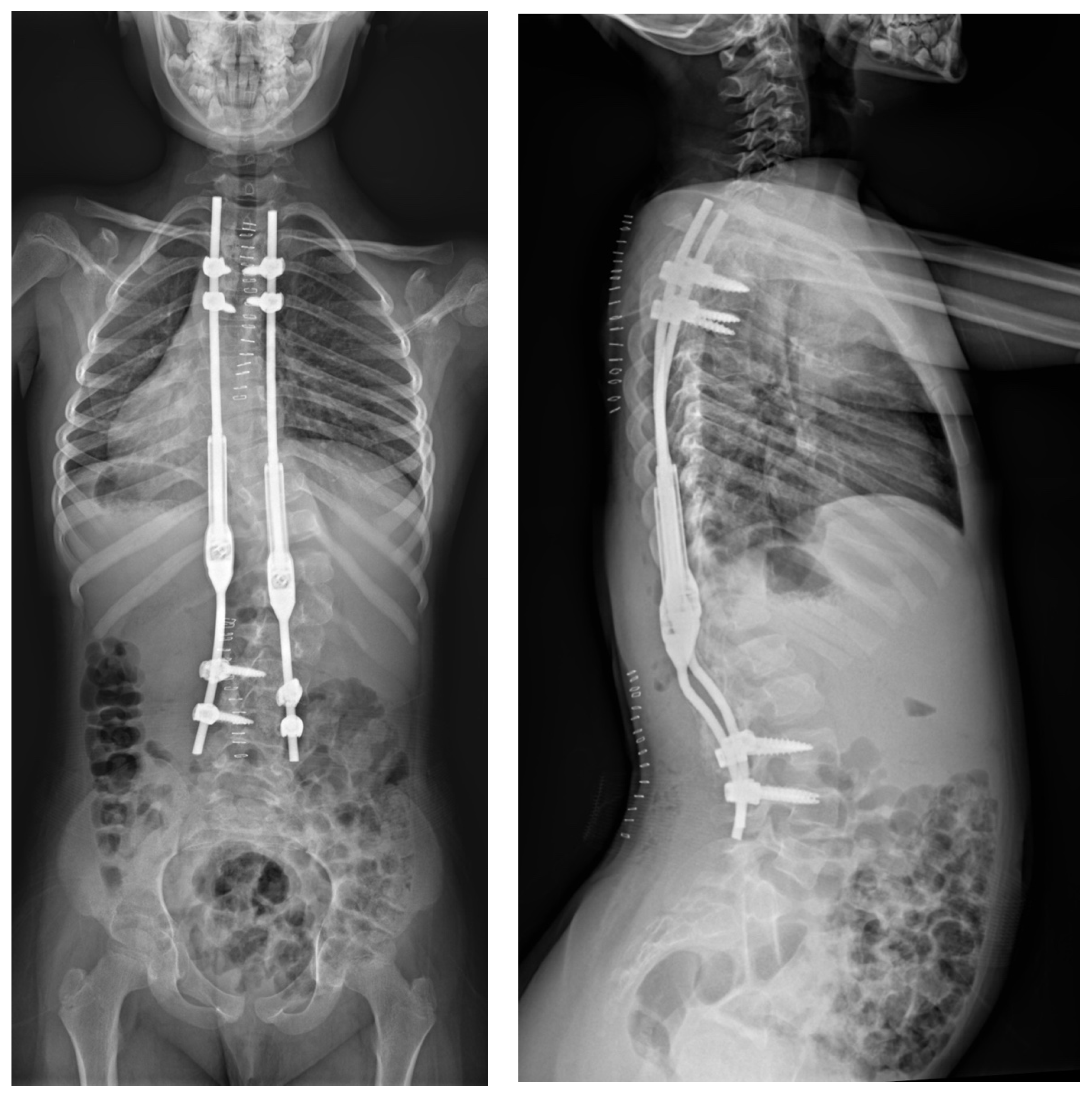
2.2. Example of Early-Onset Idiopathic Scoliosis
2.3. Example of Congenital Kyphosis
3. Discussion
4. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yang, S.; Andras, L.M.; Redding, G.J.; Skaggs, D.L. Early-onset scoliosis: A review of history, current treatment, and future directions. Pediatrics 2016, 137, e20150709. [Google Scholar] [CrossRef] [PubMed]
- Karol, L.A. The natural history of early-onset scoliosis. J. Pediatr. Orthop. 2019, 39 (Suppl. S1), S38–S43. [Google Scholar] [CrossRef] [PubMed]
- Hardesty, C.K.; Huang, R.P.; El-Hawary, R.; Samdani, A.; Hermida, P.B.; Bas, T.; Balioğlu, M.B.; Gurd, D.; Pawelek, J.; McCarthy, R.; et al. Early-onset scoliosis: Updated treatment techniques and results. Spine Deform. 2018, 6, 467–472. [Google Scholar] [CrossRef]
- Helenius, I.J. Treatment strategies for early-onset scoliosis. EFORT Open Rev. 2018, 3, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Thorsness, R.J.; Faust, J.R.; Behrend, C.J.; Sanders, J.O. Nonsurgical management of early-onset scoliosis. J. Am. Acad. Orthop. Surg. 2015, 23, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Tsirikos, A.I.; Roberts, S.B. Magnetic controlled growth rods in the treatment of scoliosis: Safety, efficacy and patient selection. Med. Devices 2020, 13, 75–85. [Google Scholar] [CrossRef]
- Mehta, J.S.; Tognini, M.; Hothi, H. Growing rods in Early Onset Scoliosis: The current scenario. J. Orthop. 2023, 42, 63–69. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Menapace, B.; Jain, V.; Sturm, P. Autofusion in early-onset scoliosis growing constructs: Occurrence, risk factors, and impacts. Spine Deform. 2024, epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Latalski, M.; Starobrat, G.; Fatyga, M.; Sowa, I.; Wójciak, M.; Wessely-Szponder, J.; Dresler, S.; Danielewicz, A. Wound-Related Complication in Growth-Friendly Spinal Surgeries for Early-Onset Scoliosis-Literature Review. J. Clin. Med. 2022, 11, 2669. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akbarnia, B.A.; Emans, J.B. Complications of growth-sparing surgery in early onset scoliosis. Spine 2010, 35, 2193–2204. [Google Scholar] [CrossRef]
- Lebel, D.E.; Rocos, B.; Helenius, I.; Sigal, A.; Struder, D.; Yazici, M.; Bekmez, S.; Hasler, C.C.; Pesenti, S.; Jouve, J.L.; et al. Magnetically Controlled Growing Rods Graduation: Deformity Control with High Complication Rate. Spine 2021, 46, E1105–E1112. [Google Scholar] [CrossRef] [PubMed]
- Bess, S.; Akbarnia, B.A.; Thompson, G.H.; Sponseller, P.D.; Shah, S.A.; El Sebaie, H.; Boachie-Adjei, O.; Karlin, L.I.; Canale, S.; Poe-Kochert, C.; et al. Complications of growing-rod treatment for early-onset scoliosis: Analysis of one hundred and forty patients. J. Bone Jt. Surg. Am. 2010, 92, 2533–2543. [Google Scholar] [CrossRef] [PubMed]
- Grabala, P.; Gupta, M.C.; Pereira, D.E.; Latalski, M.; Danielewicz, A.; Glowka, P.; Grabala, M. Radiological Outcomes of Magnetically Controlled Growing Rods for the Treatment of Children with Various Etiologies of Early-Onset Scoliosis-A Multicenter Study. J. Clin. Med. 2024, 13, 1529. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Borde, M.D.; Sapare, S.; Schutgens, E.; Ali, C.; Noordeen, H. Analysis of serum levels of titanium and aluminium ions in patients with early onset scoliosis operated upon using the magnetic growing rod-a single centre study of 14 patients. Spine Deform. 2021, 9, 1473–1478. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, M.J.; Rompala, A.; Samuel, S.P.; Samdani, A.; Pahys, J.; Hwang, S. Autofusion with Magnetically Controlled Growing Rods: A Case Report. Cureus 2023, 15, e36638. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, T.; Sze, K.Y.; Peng, Z.W.; Cheung, K.M.C.; Lui, Y.F.; Wong, Y.W.; Kwan, K.Y.H.; Cheung, J.P.Y. Systematic investigation of metallosis associated with magnetically controlled growing rod implantation for early-onset scoliosis. Bone Jt. J. 2020, 102, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Alberghina, F.; McManus, R.; Keogh, C.; Turner, H.; Moore, D.; Noël, J.; Kennedy, J.; Kiely, P. The Evaluation of Serum Metal Ion Levels and Metallosis in Graduated Patients with Magnetically Controlled Growing Rods. J. Pediatr. Orthop. 2024, 44, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Abdelaal, A.; Munigangaiah, S.; Trivedi, J.; Davidson, N. Magnetically controlled growing rods in the treatment of early onset scoliosis: A single centre experience of 44 patients with mean follow-up of 4.1 years. Bone Jt. Open 2020, 1, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Welborn, M.C.; Bouton, D. Outcomes of MCGR at >3 year average follow-up in severe scoliosis: Who undergoes elective revision vs. UPROR? Spine Deform. 2022, 10, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Grabala, P.; Helenius, I.J.; Grabala, M.; Shah, S.A. Influences of Increasing Pedicle Screw Diameter on Widening Vertebral Pedicle Size during Surgery in Spinal Deformities in Children and Adolescents without Higher Risk of Pedicle and Vertebral Breaches. J. Clin. Med. 2023, 12, 5368. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grabala, P.; Helenius, I.J.; Chamberlin, K.; Galgano, M. Less-Invasive Approach to Early-Onset Scoliosis-Surgical Technique for Magnetically Controlled Growing Rod (MCGR) Based on Treatment of 2-Year-Old Child with Severe Scoliosis. Children 2023, 10, 555. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schupper, A.J.; Lin, J.D.; Osorio, J.A.; Lee, N.J.; Steinberger, J.M.; Lombardi, J.M.; Lehman, R.A.; Lenke, L.G. Freehand Juxtapedicular Screws Placed in the Apical Concavity of Adult Idiopathic Scoliosis Patients: Technique, Computed Tomography Confirmation, and Radiographic Results. Neurospine 2022, 19, 1116–1121. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grabala, P.; Helenius, I.J.; Kowalski, P.; Grabala, M.; Zacha, S.; Deszczynski, J.M.; Albrewczynski, T.; Galgano, M.A.; Buchowski, J.M.; Chamberlin, K.; et al. The Child’s Age and the Size of the Curvature Do Not Affect the Accuracy of Screw Placement with the Free-Hand Technique in Spinal Deformities in Children and Adolescents. J. Clin. Med. 2023, 12, 3954. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stücker, R.; Mladenov, K.; Stücker, S. Mitwachsende Korrektursysteme bei Early-Onset-Skoliosen [Growth-preserving instrumentation for early onset scoliosis]. Oper. Orthop. Traumatol. 2024, 36, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, N.D.; McClung, A.; Rathjen, K.E.; Denning, J.R.; Browne, R.; Johnston, C.E., 3rd. Serial casting as a delay tactic in the treatment of moderate-to-severe early-onset scoliosis. J. Pediatr. Orthop. 2012, 32, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Sinha, R.; Roye, B.D.; Ball, J.R.; Skaggs, K.F.; Brooks, J.T.; Welborn, M.C.; Emans, J.B.; Anari, J.B.; Johnston, C.E.; et al. Contraindications to magnetically controlled growing rods: Consensus among experts in treating early onset scoliosis. Spine Deform. 2022, 10, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Lemans, J.V.C.; Wijdicks, S.P.J.; Castelein, R.M.; Kruyt, M.C. Spring distraction system for dynamic growth guidance of early onset scoliosis: Two-year prospective follow-up of 24 patients. Spine J. 2021, 21, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Lemans, J.V.C.; Top, A.; Tabeling, C.S.; Scholten, E.P.; Stempels, H.W.; Schlösser, T.P.C.; Castelein, R.M.; Kruyt, M.C. Health-related quality of life in early onset scoliosis patients treated with the spring distraction system: What to expect in the first 2 years after surgery. Spine Deform. 2024, 12, 489–499. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Studer, D.; Hasler, C.C. Diagnostic and therapeutic strategies in early onset scoliosis: A current concept review. J. Child. Orthop. 2024, 18, 113–123. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Haapala, H.; Saarinen, A.J.; Salonen, A.; Helenius, I. Shilla Growth Guidance Compared with Magnetically Controlled Growing Rods in the Treatment of Neuromuscular and Syndromic Early-onset Scoliosis. Spine 2020, 45, E1604–E1614. [Google Scholar] [CrossRef] [PubMed]
- El-Hawary, R.; Morash, K.; Kadhim, M.; Vitale, M.; Smith, J.; Samdani, A.; Flynn, J.; Children’s Spine Study Group. VEPTR Treatment of Early Onset Scoliosis in Children without Rib Abnormalities: Long-term Results of a Prospective, Multicenter Study. J. Pediatr. Orthop. 2020, 40, e406–e412. [Google Scholar] [CrossRef] [PubMed]
- Roser, M.J.; Askin, G.N.; Labrom, R.D.; Zahir, S.F.; Izatt, M.; Little, J.P. Vertebral body tethering for idiopathic scoliosis: A systematic review and meta-analysis. Spine Deform. 2023, 11, 1297–1307. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Raitio, A.; Syvänen, J.; Helenius, I. Vertebral Body Tethering: Indications, Surgical Technique, and a Systematic Review of Published Results. J. Clin. Med. 2022, 11, 2576. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mackey, C.; Hanstein, R.; Lo, Y.; Vaughan, M.; St Hilaire, T.; Luhmann, S.J.; Vitale, M.G.; Glotzbecker, M.P.; Samdani, A.; Parent, S.; et al. Magnetically Controlled Growing Rods (MCGR) Versus Single Posterior Spinal Fusion (PSF) Versus Vertebral Body Tether (VBT) in Older Early Onset Scoliosis (EOS) Patients: How Do Early Outcomes Compare? Spine 2022, 47, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Baroncini, A.; Courvoisier, A. The different applications of Vertebral Body Tethering—Narrative review and clinical experience. J. Orthop. 2023, 37, 86–92. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheung, P.W.H.; Wong, C.K.H.; Sadiang-Abay, J.T.; Lau, S.T.; Cheung, J.P.Y. Longitudinal comparison of direct medical cost, radiological and health-related quality of life treatment outcomes between traditional growing rods and magnetically controlled growing rods from preoperative to maturity. BMC Musculoskelet. Disord. 2022, 23, 791. [Google Scholar] [CrossRef] [PubMed]
- Doany, M.E.; Olgun, Z.D.; Kinikli, G.I.; Bekmez, S.; Kocyigit, A.; Demirkiran, G.; Karaagaoglu, A.E.; Yazici, M. Health-related quality of life in early-onset scoliosis patients treated surgically: EOSQ scores in traditional growing rod versus magnetically controlled growing rods. Spine 2018, 43, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Tahir, M.; Mehta, D.; Sandhu, C.; Jones, M.; Gardner, A.; Mehta, J.S. A comparison of the post-fusion outcome of patients with early-onset scoliosis treated with traditional and magnetically controlled growing rods. Bone Jt. J. 2022, 104, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.M.; Buckler, N.J.; Al Nouri, M.; Howard, J.J.; Vaughan, M.; St Hilaire, T.; Sponseller, P.D.; Smith, J.T.; Thompson, G.H.; El-Hawary, R.; et al. No difference in the rates of unplanned return to the operating room between magnetically controlled growing rods and traditional growth friendly surgery for children with cerebral palsy. J. Pediatr. Orthop. 2022, 42, 100–108. [Google Scholar] [CrossRef]
- Choi, E.; Yaszay, B.; Mundis, G.; Hosseini, P.; Pawelek, J.; Alanay, A.; Berk, H.; Cheung, K.; Demirkiran, G.; Ferguson, J.; et al. Implant complications after magnetically controlled growing rods for early onset scoliosis: A multicenter retrospective review. J. Pediatr. Orthop. 2017, 37, e588–e592. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.P.Y.; Cheung, K.M. Current status of the magnetically controlled growing rod in treatment of early-onset scoliosis: What we know after a decade of experience. J. Orthop. Surg. 2019, 27, 2309499019886945. [Google Scholar] [CrossRef]
- Bekmez, S.; Afandiyev, A.; Dede, O.; Karaismailoğlu, E.; Demirkiran, H.G.; Yazici, M. Is magnetically controlled growing rod the game changer in early-onset scoliosis? A preliminary report. J. Pediatr. Orthop. 2019, 39, e195–e200. [Google Scholar] [CrossRef]
- Green, A.H.; Brzezinski, A.; Ishmael, T.; Adolfsen, S.; Bowe, J.A. Premature spinal fusion after insertion of magnetically controlled growing rods for treatment of early-onset scoliosis: Illustrative case. J. Neurosurg. Case Lessons 2021, 2, CASE21446. [Google Scholar] [CrossRef]
- Mundis, G.M.; Kabirian, N.; Akbarnia, B.A. Dual growing rods for the treatment of early-onset scoliosis. JBJS Essent. Surg. Tech. 2013, 3, e6. [Google Scholar] [CrossRef]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabala, P. Minimally Invasive Controlled Growing Rods for the Surgical Treatment of Early-Onset Scoliosis—A Surgical Technique Video. J. Pers. Med. 2024, 14, 548. https://doi.org/10.3390/jpm14060548
Grabala P. Minimally Invasive Controlled Growing Rods for the Surgical Treatment of Early-Onset Scoliosis—A Surgical Technique Video. Journal of Personalized Medicine. 2024; 14(6):548. https://doi.org/10.3390/jpm14060548
Chicago/Turabian StyleGrabala, Pawel. 2024. "Minimally Invasive Controlled Growing Rods for the Surgical Treatment of Early-Onset Scoliosis—A Surgical Technique Video" Journal of Personalized Medicine 14, no. 6: 548. https://doi.org/10.3390/jpm14060548
APA StyleGrabala, P. (2024). Minimally Invasive Controlled Growing Rods for the Surgical Treatment of Early-Onset Scoliosis—A Surgical Technique Video. Journal of Personalized Medicine, 14(6), 548. https://doi.org/10.3390/jpm14060548







