Exploring Health Informatics in the Battle against Drug Addiction: Digital Solutions for the Rising Concern
Abstract
:1. Introduction
2. The Growing Drug Addiction Crisis
2.1. Current Status of Drug Addiction in the US and Related Regulations
2.2. The Growing Opioid Epidemic
2.3. The Mental Health Consequences and Social Impact
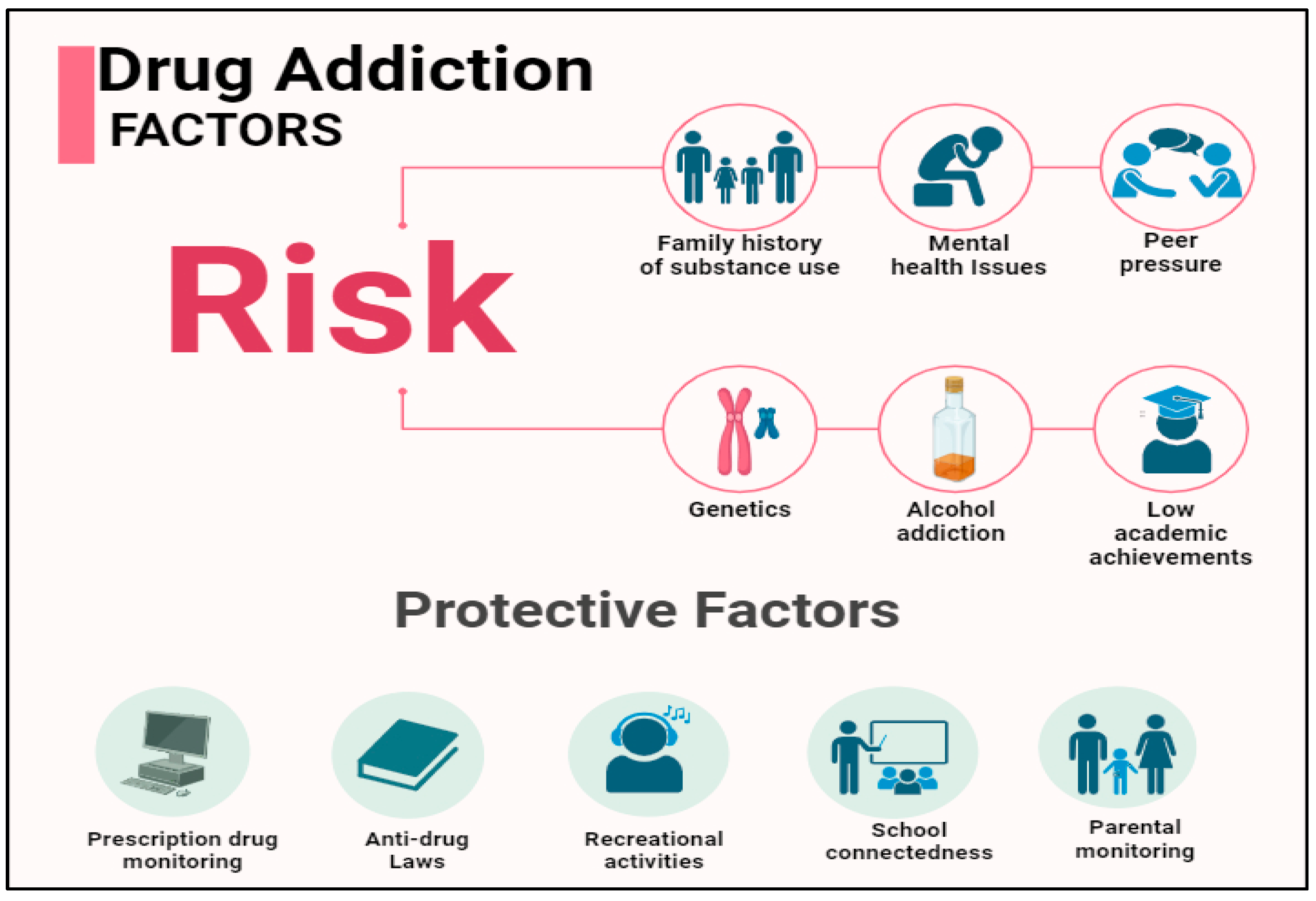
2.4. Associated Risk Factors of Drug Addiction
2.4.1. Record of Addiction within a Family
2.4.2. Mental Health Disorder
2.4.3. Peer Pressure, Lack of Family Involvement and Early Use
3. Health Information Management and Addiction
3.1. Health Informatics and Various Platforms
3.2. Applications of Health Informatics in Drug Addiction Management
3.3. Prescription Drug Monitoring Programs (PDMPs) and Their Effectiveness
4. Development of Novel Interventions
4.1. Drug and Alcohol Services Information Systems (DASIS)
4.2. Developing a Collaboration between EHRs and AI
5. Challenges in Implying Health Informatics for Drug Addiction
6. Conclusions and Future Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goldstein, R.Z.; Volkow, N.D. Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. Nat. Rev. Neurosci. 2011, 12, 652–669. [Google Scholar] [CrossRef] [PubMed]
- National Drug Intelligence Center. The Economic Impact of Illicit Drug Use on American Society; United States Department of Justice: Washington, DC, USA, 2011.
- Rehm, J.; Mathers, C.; Popova, S.; Thavorncharoensap, M.; Teerawattananon, Y.; Patra, J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009, 373, 2223–2233. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2014.
- Centers for Disease Control and Prevention. Drug and opioid-involved overdose deaths—United States, 2017–2018. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 290–297. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6911a4.htm (accessed on 5 January 2024). [CrossRef] [PubMed]
- American Addiction Centres. Alcohol and Drug Abuse Statistics (Facts about Addiction); American Addiction Centres: Rockville, MD, USA, 2024. [Google Scholar]
- National Center for Drug Abuse Statistics. Drug Abuse Statistics; National Center for Drug Abuse Statistics: Rockville, MD, USA, 2020. [Google Scholar]
- Kelly, T.M.; Daley, D.C. Integrated treatment of substance use and psychiatric disorders. Soc. Work Public Health 2013, 28, 388–406. [Google Scholar] [CrossRef] [PubMed]
- Cone, E.J.; Bigelow, G.E.; Herrmann, E.S. Non-smoker exposure to secondhand cannabis smoke. I. Urine screening and confirmation results. J. Anal. Toxicol. 2015, 39, 1–12. [Google Scholar] [CrossRef] [PubMed]
- NIDA. Addiction and Health; NIDA: Rockville, MD, USA, 2022.
- Michie, S.; Yardley, L.; West, R.; Patrick, K.; Greaves, F. Developing and evaluating digital interventions to promote behavior change in health and health care: Recommendations resulting from an international workshop. J. Med. Internet Res. 2017, 19, e232. [Google Scholar] [CrossRef] [PubMed]
- Arigo, D.; Jake-Schoffman, D.E.; Wolin, K.; Beckjord, E.; Hekler, E.B.; Pagoto, S.L. The history and future of digital health in the field of behavioral medicine. J. Behav. Med. 2019, 42, 67–83. [Google Scholar] [CrossRef] [PubMed]
- Wisdom, J.P.; Ford, J.H.; McCarty, D. The use of health information technology in publicly-funded US substance abuse treatment agencies. Contemp. Drug Probl. 2010, 37, 315–339. [Google Scholar] [CrossRef]
- Substance Abuse and Mental Health Services Administration (SAMHSA). National Survey on Drug Abuse and Mental Health; Substance Abuse and Mental Health Services Administration (SAMHSA): Rockville, MD, USA, 2020. [Google Scholar]
- NIDA. Cannabis (Marijuana) DrugFacts; NIDA: Rockville, MD, USA, 2019.
- NIDA. Prescription Opioids DrugFacts; NIDA: Rockville, MD, USA, 2021.
- NIDA. What Are the Long-Term Effects of Cocaine Use? NIDA: Rockville, MD, USA, 2021.
- NIDA. What Are the Immediate (Short-Term) Effects of Heroin Use? NIDA: Rockville, MD, USA, 2021.
- Farzam, K.; Faizy, R.M.; Saadabadi, A. Stimulants. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK539896/ (accessed on 10 January 2024).
- Bounds, C.G.; Patel, P.; Nelson, V.L. Benzodiazepines. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470159/ (accessed on 12 December 2023).
- Suddock, J.T.; Kent, K.J.; Cain, M.D. Barbiturate Toxicity. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499875/ (accessed on 9 December 2023).
- Chou, R.; Fanciullo, G.J.; Fine, P.G. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J. Pain. 2009, 10, 113–130. [Google Scholar] [CrossRef]
- Beheshti, D. Adverse health effects of abuse-deterrent opioids: Evidence from the reformulation of OxyContin. Health Econ. 2019, 28, 1449–1461. [Google Scholar] [CrossRef]
- Radke, J.B.; Owen, K.P.; Sutter, M.E.; Ford, J.B.; Albertson, T.E. The effects of opioids on the lung. Clin. Rev. Allergy Immunol. 2014, 46, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Compton, W.M.; Jones, C.M.; Baldwin, G.T. Relationship between nonmedical prescription-opioid use and heroin use. N. Engl. J. Med. 2016, 374, 154–163. [Google Scholar] [CrossRef]
- Toro, D. A Qualitative Analysis of the Health Informatics Role in Addressing the Public Health Crisis of Addiction and Overall Effectiveness of Treatment; Department of Health Informatics and Information Management: Chicago, IL, USA, 2016. [Google Scholar]
- Barry, C.L.; McGinty, E.E.; Pescosolido, B.A.; Goldman, H.H. Stigma, discrimination, treatment effectiveness, and policy: Public views about drug addiction and mental illness. Psychiatr. Serv. 2014, 65, 1269–1272. [Google Scholar] [CrossRef]
- Wani, M.A.; Sankar, R. Impact of drug addiction on mental health. J. Ment. Disord. Treat. 2016, 2, 1–3. [Google Scholar]
- Grant, B.F.; Saha, T.D.; Ruan, W.J. Epidemiology of DSM-5 drug use disorder: Results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiatry 2016, 73, 39–47. [Google Scholar] [CrossRef]
- Schaefer, M.; Sarkar, R.; Diez-Quevedo, C. Management of mental health problems prior to and during treatment of hepatitis C virus infection in patients with drug addiction. Clin. Infect. Dis. 2013, 57 (Suppl. 2), S111–S117. [Google Scholar] [CrossRef]
- McGinty, E.E.; Goldman, H.H.; Pescosolido, B.; Barry, C.L. Portraying mental illness and drug addiction as treatable health conditions: Effects of a randomized experiment on stigma and discrimination. Soc. Sci. Med. 2015, 126, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Walsh, Z.; Gonzalez, R.; Crosby, K.; Thiessen, M.S.; Carroll, C.; Bonn-Miller, M.O. Medical cannabis and mental health: A guided systematic review. Clin. Psychol. Rev. 2017, 51, 15–29. [Google Scholar] [CrossRef]
- Chamberlain, S.R.; Lust, K.; Grant, J.E. Cocaine use in university students: Relationships with demographics, mental health, risky sexual practices, and trait impulsivity. CNS Spectr. 2021, 26, 501–508. [Google Scholar] [CrossRef]
- Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health; Center for Behavioral Health Statistics and Quality: Rockville, MD, USA, 2015; Volume 2015. [Google Scholar]
- Meier, M.H.; Hall, W.; Caspi, A. Which adolescents develop persistent substance dependence in adulthood? Using population-representative longitudinal data to inform universal risk assessment. Psychol. Med. 2016, 46, 877–889. [Google Scholar] [CrossRef]
- Groenman, A.P.; Janssen, T.W.P.; Oosterlaan, J. Childhood psychiatric disorders as risk factor for subsequent substance abuse: A meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 556–569. [Google Scholar] [CrossRef] [PubMed]
- Van Ryzin, M.J.; Dishion, T.J. Adolescent deviant peer clustering as an amplifying mechanism underlying the progression from early substance use to late adolescent dependence. J. Child Psychol. Psychiatry 2014, 55, 1153–1161. [Google Scholar] [CrossRef] [PubMed]
- Pingault, J.B.; Cote, S.M.; Galera, C.; Genolini, C.; Falissard, B.; Vitaro, F. Childhood trajectories of inattention, hyperactivity and oppositional behaviors and prediction of substance abuse/dependence: A 15-year longitudinal population-based study. Mol. Psychiatry 2013, 18, 806–812. [Google Scholar] [CrossRef] [PubMed]
- Bertholet, N.; Cunningham, J.A. Information technology and addiction science: Promises and challenges. Addict. Sci. Clin. Pract. 2021, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, B.; Wang, J.; Wu, S. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann. Intern. Med. 2006, 144, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, J.A.; Gulliver, A.; Farrer, L.; Bennett, K.; Carron-Arthur, B. Internet interventions for mental health and addictions: Current fndings and future directions. Curr. Psychiatry Rep. 2014, 16, 521. [Google Scholar] [CrossRef] [PubMed]
- Ekström, V.; Johansson, M. Sort of a nice distance: A qualitative study of the experiences of therapists working with internet-based treatment of problematic substance use. Addict. Sci. Clin. Pract. 2019, 14, 44. [Google Scholar] [CrossRef] [PubMed]
- Harpaz, R.; Vilar, S.; DuMouchel, W. Combing signals from spontaneous reports and electronic health records for detection of adverse drug reactions. J. Am. Med. Inform. Assoc. 2013, 20, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; McPeek Hinz, E.R.; Matheny, M.E. Comparative analysis of pharmacovigilance methods in the detection of adverse drug reactions using electronic medical records. J. Am. Med. Inform. Assoc. 2013, 20, 420–426. [Google Scholar] [CrossRef]
- Goldzweig, C.L.; Towfigh, A.; Maglione, M.; Shekelle, P.G. Costs and benefits of health information technology: New trends from the literature. Health Aff. 2009, 28, w282–w293. [Google Scholar] [CrossRef]
- Winhusen, T.; Theobald, J.; Kaelber, D.C.; Lewis, D. Medical complications associated with substance use disorders in patients with type 2 diabetes and hypertension: Electronic health record findings. Addiction 2019, 114, 1462–1470. [Google Scholar] [CrossRef] [PubMed]
- Caballeria, E.; López-Pelayo, H.; Matrai, S.; Gual, A. Telemedicine in the treatment of addictions. Curr. Opin. Psychiatry 2022, 35, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Valdes, E.G.; Reist, C.; Aamar, R.; Hallisey, B.; Stanton, E.S.; Williams, L.; Andel, R.; Gorman, J. Use of predictive analytics to identify unhealthy opioid use and guide intervention. Psychiatr. Serv. 2023, 1, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Haffajee, R.L.; Jena, A.B.; Weiner, S.G. Mandatory use of prescription drug monitoring programs. JAMA 2015, 313, 891–892. [Google Scholar] [CrossRef]
- Yokell, M.A.; Green, T.C.; Rich, J.D. Prescription drug monitoring programs. JAMA 2012, 307, 912–913. [Google Scholar] [CrossRef] [PubMed]
- Irvine, J.M.; Hallvik, S.E.; Hildebran, C.; Marino, M.; Beran, T.; Deyo, R.A. Who uses a prescription drug monitoring program and how? Insights from a statewide survey of Oregon clinicians. J. Pain 2014, 15, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Dormuth, C.R.; Miller, T.A.; Huang, A.; Mamdani, M.M.; Juurlink, D.N. Effect of a centralized prescription network on inappropriate prescriptions for opioid analgesics and benzodiazepines. CMAJ Can. Med. Assoc. J. 2012, 184, E852–E856. [Google Scholar] [CrossRef]
- Hildebran, C.; Cohen, D.J.; Irvine, J.M. How clinicians use prescription drug monitoring programs: A qualitative inquiry. Pain Med. 2014, 15, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.M.; McRae, I.S. An inevitable wave of prescription drug monitoring programs in the context of prescription opioids: Pros, cons and tensions. BMC Pharmacol. Toxicol. 2014, 15, 46. [Google Scholar] [CrossRef]
- Ajami, S.; Mellat-Karkevandi, Z. The advantages and barriers in the implementation of a substance dependence treatment information system (SDTIS). J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2015, 20, 1105–1111. [Google Scholar] [CrossRef]
- Ajami, S.; Mellat-Karkevandi, Z.; Saghaeiannejad-Isfahani, S.; Salehi, M.; Jahanbakhsh, M. A comparison of substance dependence treatment information system in America, England, and Iran. J. Educ. Health Promot. 2014, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Shahriar, A.; Faisal, F.; Mahmud, S.U.; Chakrabarti, A.; Alam, M.G. A machine learning approach to predict vulnerability to drug addiction. In Proceedings of the 2019 22nd International Conference on Computer and Information Technology (ICCIT), Dhaka, Bangladesh, 18–20 December 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 1–7. [Google Scholar]
- Dong, X.; Deng, J.; Rashidian, S. Identifying risk of opioid use disorder for patients taking opioid medications with deep learning. J. Am. Med. Inform. Assoc. 2021, 28, 1683–1693. [Google Scholar] [CrossRef] [PubMed]
- Ovalle, A.; Goldstein, O.; Kachuee, M.; Wu, E.S.C.; Hong, C.; Holloway, I.W.; Sarrafzadeh, M. Leveraging Social Media Activity and Machine Learning for HIV and Substance Abuse Risk Assessment: Development and Validation Study. J. Med. Internet Res. 2021, 23, e22042. [Google Scholar] [CrossRef] [PubMed]
- Barenholtz, E.; Fitzgerald, N.D.; Hahn, W.E. Machine-learning approaches to substance-abuse research: Emerging trends and their implications. Curr. Opin. Psychiatry. 2020, 33, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Conway, K.P.; Levy, J.; Vanyukov, M. Measuring addiction propensity and severity: The need for a new instrument. Drug Alcohol. Depend. 2010, 111, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Guttha, N.; Miao, Z.; Shamsuddin, R. Towards the development of a substance abuse index (SEI) through informatics. Healthcare 2021, 9, 1596. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chhetri, B.; Goyal, L.M.; Mittal, M. How machine learning is used to study addiction in digital healthcare: A systematic review. Int. J. Inf. Manag. Data Insights 2023, 3, 100175. [Google Scholar] [CrossRef]
- Kuperman, G.J.; Bobb, A.; Payne, T.H.; Avery, A.J.; Gandhi, T.K.; Burns, G.; Classen, D.C.; Bates, D.W. Medication-related clinical decision support in computerized provider order entry systems: A review. J. Am. Med. Inform. Assoc. 2007, 14, 29–40. [Google Scholar] [CrossRef]
- Luna, D.; Almerares, A.; Mayan, J.C.; González Bernaldo de Quirós, F.G.B.; Otero, C. Health informatics in developing countries: Going beyond pilot practices to sustainable implementations: A review of the current challenges. Healthc. Inform. Res. 2014, 20, 3–10. [Google Scholar] [CrossRef]
- Gostin, L.O.; Levit, L.A.; Nass, S.J. (Eds.) Beyond the HIPAA Privacy Rule: Enhancing Privacy, Improving Health Through Research; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Afzal, M.; Riazul Islam, S.M.; Hussain, M.; Lee, S. Precision medicine informatics: Principles, prospects, and challenges. IEEE Access 2020, 8, 13593–13612. [Google Scholar] [CrossRef]



| Substance | Estimated Number of People Affected | Physical/Mental Health Consequences | References |
|---|---|---|---|
| Marijuana | 5.1% (or 14.2 million) | Alterations in senses, Mood swings, Diminished bodily movement, Difficulty in problem-solving, Decreased memory, Hallucinations, Psychosis | [14,15] |
| Opioids | 1.1% (or 2.7 million) | Falling unconscious, Slow and shallow breathing, Choking, Vomiting, Slower heart rate | [14,16] |
| Cocaine | 0.5% (or 1.3 million) | Weight loss, Damage to cardiovascular system, Risk of stroke, Intracerebral hemorrhage, Ulcerations in the GI tract, Cognitive impairments | [14,17] |
| Heroin | 0.3% (or 902,000) | Hot flashes, Dry mouth, Lack of concentration, Slower heart rate, Coma and Permanent brain damage | [14,18] |
| Stimulant use disorder | 0.2% (roughly 500,000) | Decreased appetite, Anxiety, Jitteriness, Headaches, Weight loss, Insomnia, Psychosis. | [14,19] |
| Benzodiazepines | 2% (5 million) | Respiratory depression, Respiratory arrest, Drowsiness, Confusion, Syncope, Nausea/vomiting, Diarrhea. | [14,20] |
| Barbiturates | 0.2% (or 500,000) | Lack of consciousness, Bradycardia, Difficulty in coordination, Vertigo, Weak muscles | [14,21] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimu, S.J.; Patil, S.M.; Dadzie, E.; Tesfaye, T.; Alag, P.; Więckiewicz, G. Exploring Health Informatics in the Battle against Drug Addiction: Digital Solutions for the Rising Concern. J. Pers. Med. 2024, 14, 556. https://doi.org/10.3390/jpm14060556
Shimu SJ, Patil SM, Dadzie E, Tesfaye T, Alag P, Więckiewicz G. Exploring Health Informatics in the Battle against Drug Addiction: Digital Solutions for the Rising Concern. Journal of Personalized Medicine. 2024; 14(6):556. https://doi.org/10.3390/jpm14060556
Chicago/Turabian StyleShimu, Shakila Jahan, Srushti Moreshwar Patil, Ebenezer Dadzie, Tadele Tesfaye, Poorvanshi Alag, and Gniewko Więckiewicz. 2024. "Exploring Health Informatics in the Battle against Drug Addiction: Digital Solutions for the Rising Concern" Journal of Personalized Medicine 14, no. 6: 556. https://doi.org/10.3390/jpm14060556
APA StyleShimu, S. J., Patil, S. M., Dadzie, E., Tesfaye, T., Alag, P., & Więckiewicz, G. (2024). Exploring Health Informatics in the Battle against Drug Addiction: Digital Solutions for the Rising Concern. Journal of Personalized Medicine, 14(6), 556. https://doi.org/10.3390/jpm14060556







