Drinking from the Holy Grail—Does a Perfect Triage System Exist? And Where to Look for It?
Abstract
1. Introduction
- (a)
- The design and function of a triage system
- (b)
- Its validation
- (c)
- Its performance
- (d)
- The comparison between the two triage systems
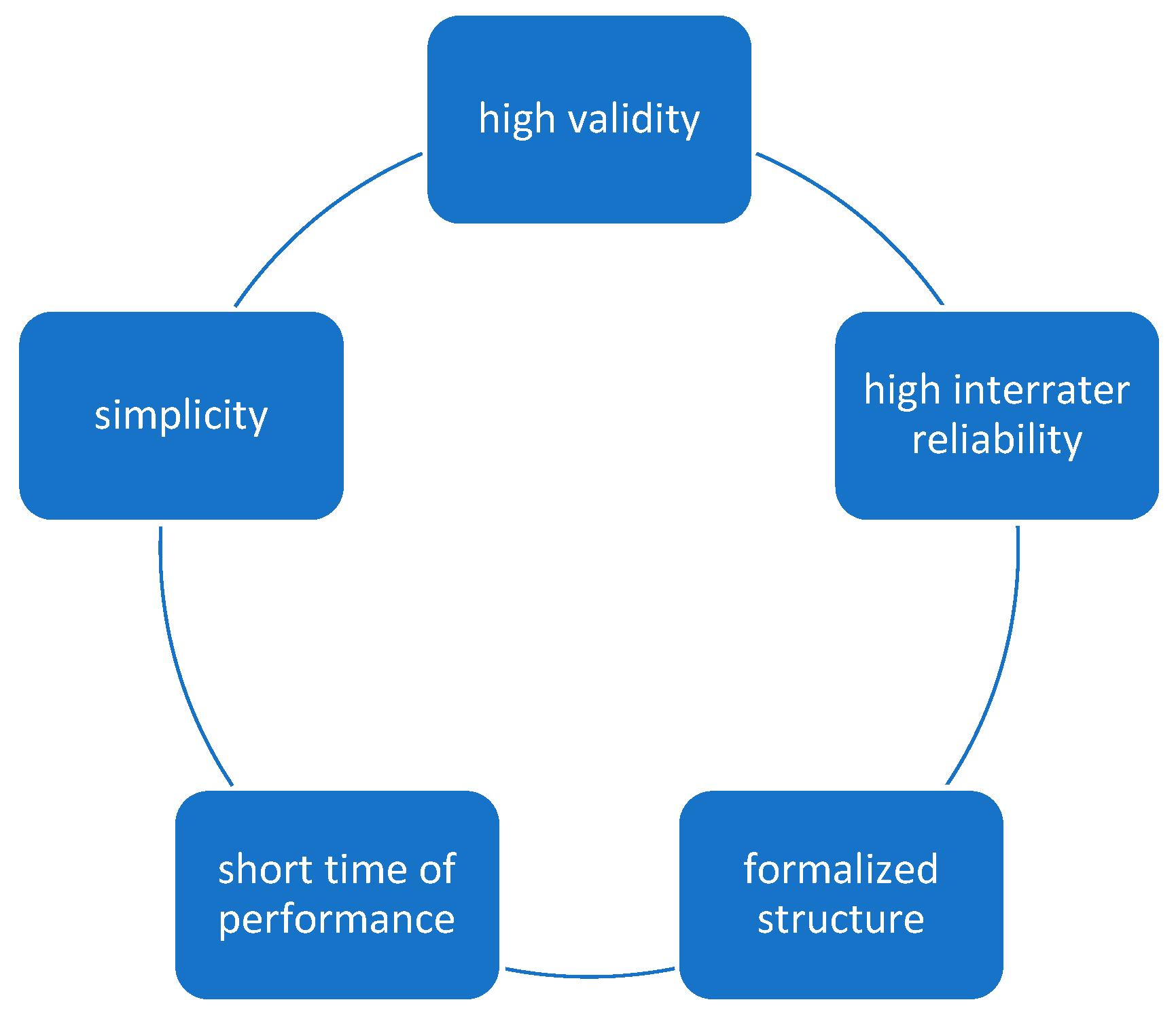
2. Ideal Triage System
3. Most Common Triage Systems
- I.
- ATS (Australian Triage Scale)
- 0 min. for priority 1 (red)
- Up to 10 min for priority 2 (orange)
- Up to 30 min for priority 3 (green)
- Up to 60 min for priority 4 (blue)
- Up to 120 min. for priority 5 (white) [27].
- II.
- CTAS (Canadian Triage and Acuity Scale)
- For priority 1 (blue), assistance must be provided immediately,
- Priority 2 (red) can wait up to 15 min,
- Priority 3 (yellow) waiting time up to 30 min,
- Priority 4 (green) waiting time up to 60 min,
- Priority 5 (white) waiting time up to 120 min [26].
- “Critical Look”—A short, several-second assessment according to the ABCD scheme, aimed at quick recognition of patients in priorities 1 and 2
- Assessment for infectious diseases—Aimed at the rapid isolation of potentially dangerous patients or their decontamination
- Identify the patient’s main or major complaints, collect objective data (including, for example, vital signs, injury assessment, bleeding severity), use a list of “modifiers”. They are grouped into 17 categories, there are about 177 of them in total, and some of them are additionally graded, so that after confirming a given modifier, the priority can be read from the table
- The prioritization of the CTAS
- III.
- ESI (Emergency Severity Index)
- Immediately for priority 1
- Up to 10 min for priority [25]
- Point A—The nurse must assess whether the patient requires life-saving procedures. If so, give priority 1.
- Point B—Features of a high-risk state for the patient are looked for, the presence of severe pain or disturbances of consciousness—if the result is positive, priority 2 is given.
- Point C—it is necessary to assess what will be the “consumption” of resources while supplying the patient to the ED. This is a feature that distinguishes the ESI system from others. Patients requiring one or none of the resources receive Priority 4 and 5, respectively. Patients requiring two or more resources go to the next point.
- Point D—vital parameters are assessed: saturation O2, pulse rate, respiratory rate, and temperature in children, based on the table, it is determined whether the patient “promotes” to the priority 2 group or receives priority 3. This point is a kind of “Fuse”, enabling reconsideration of the prioritization of 2 patients [24].
- IV.
- MTS (Manchester Triage System)
- Priority 1 (red)—immediate aid,
- Priority 2 (orange)—up to 10 min,
- Priority 3 (yellow)—up to 60 min,
- Priority 4 (green)—up to 120 min.
- Priority 5 (blue)—up to 240 min [22].
4. Triage System Comparisons
5. Future of Triage
6. Summary
7. Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cameron, A.; Rodgers, K.; Ireland, A.; Jamdar, R.; McKay, G.A. A simple tool to predict admission at the time of triage. Emerg. Med. J. 2015, 32, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Christ, M.; Grossmann, F.; Winter, D.; Bingisser, R.; Platz, E. Modern triage in the emergency department. Dtsch. Arztebl. Int. 2010, 107, 892–898. [Google Scholar] [CrossRef]
- Brouns, S.H.A.; Mignot-Evers, L.; Derkx, F.; Lambooij, S.L.; Dieleman, J.P.; Haak, H.R. Performance of the Manchester triage system in older emergency department patients: A retrospective cohort study. BMC Emerg. Med. 2019, 19, 3. [Google Scholar] [CrossRef] [PubMed]
- Grossmann, F.F.; Zumbrunn, T.; Frauchiger, A.; Delport, K.; Bingisser, R.; Nickel, C.H. At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann. Emerg. Med. 2012, 60, 317–325.e3. [Google Scholar] [CrossRef]
- Azeredo, T.R.M.; Guedes, H.M.; Rebelo de Almeida, R.A.; Chianca, T.C.M.; Martins, J.C.A. Efficacy of the Manchester Triage System: A systematic review. Int. Emerg. Nurs. 2015, 23, 47–52. [Google Scholar] [CrossRef]
- Barfod, C.; Lauritzen, M.M.P.; Danker, J.K.; Sölétormos, G.; Forberg, J.L.; Berlac, P.A.; Lippert, F.; Lundstrøm, L.H.; Antonsen, K.; Lange, K.H.W. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department—A prospective cohort study. Scand. J. Trauma. Resusc. Emerg. Med. 2012, 20, 28. [Google Scholar] [CrossRef] [PubMed]
- Artificial Intelligence Algorithm to Predict the Need for Critical Care in Prehospital Emergency Medical Services|Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine|Full Text. Available online: https://sjtrem.biomedcentral.com/articles/10.1186/s13049-020-0713-4 (accessed on 21 May 2024).
- Karlafti, E.; Anagnostis, A.; Simou, T.; Kollatou, A.S.; Paramythiotis, D.; Kaiafa, G.; Didaggelos, T.; Savvopoulos, C.; Fyntanidou, V. Support Systems of Clinical Decisions in the Triage of the Emergency Department Using Artificial Intelligence: The Efficiency to Support Triage. Acta Medica Litu. 2023, 30, 19–25. [Google Scholar] [CrossRef]
- Ilicki, J. Challenges in evaluating the accuracy of AI-containing digital triage systems: A systematic review. PLoS ONE 2022, 17, e0279636. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.-J.; Chien, C.-Y.; Seak, J.C.-J.; Tsai, S.-L.; Weng, Y.-M.; Chaou, C.-H.; Kuo, C.-W.; Chen, J.-C.; Hsu, K.-H. Validation of the five-tier Taiwan Triage and Acuity Scale for prehospital use by Emergency Medical Technicians. Emerg. Med. J. 2019, 36, 472–478. [Google Scholar] [CrossRef]
- Leeies, M.; Ffrench, C.; Strome, T.; Weldon, E.; Bullard, M.; Grierson, R. Prehospital Application of the Canadian Triage and Acuity Scale by Emergency Medical Services. Can. J. Emerg. Med. 2017, 19, 26–31. [Google Scholar] [CrossRef]
- Emergency Medical Services Triage Using the Emergency Severity Index: Is It Reliable and Valid? Available online: https://pubmed.ncbi.nlm.nih.gov/22244546/ (accessed on 21 May 2024).
- Abe, D.; Inaji, M.; Hase, T.; Takahashi, S.; Sakai, R.; Ayabe, F.; Tanaka, Y.; Otomo, Y.; Maehara, T. A Prehospital Triage System to Detect Traumatic Intracranial Hemorrhage Using Machine Learning Algorithms. JAMA Netw. Open 2022, 5, e2216393. [Google Scholar] [CrossRef] [PubMed]
- Implementation of an All-Day Artificial Intelligence-Based Triage System to Accelerate Door-to-Balloon Times. Available online: https://pubmed.ncbi.nlm.nih.gov/36336511/ (accessed on 18 May 2024).
- Tu, K.-C.; Eric Nyam, T.-T.; Wang, C.-C.; Chen, N.-C.; Chen, K.-T.; Chen, C.-J.; Liu, C.-F.; Kuo, J.-R. A Computer-Assisted System for Early Mortality Risk Prediction in Patients with Traumatic Brain Injury Using Artificial Intelligence Algorithms in Emergency Room Triage. Brain Sci. 2022, 12, 612. [Google Scholar] [CrossRef] [PubMed]
- Brandao-de-Resende, C.; Melo, M.; Lee, E.; Jindal, A.; Neo, Y.N.; Sanghi, P.; Freitas, J.R.; Castro, P.V.I.P.; Rosa, V.O.M.; Valentim, G.F.S.; et al. A machine learning system to optimise triage in an adult ophthalmic emergency department: A model development and validation study. eClinicalMedicine 2023, 66, 102331. [Google Scholar] [CrossRef] [PubMed]
- Hunter, O.F.; Perry, F.; Salehi, M.; Bandurski, H.; Hubbard, A.; Ball, C.G.; Morad Hameed, S. Science fiction or clinical reality: A review of the applications of artificial intelligence along the continuum of trauma care. World J. Emerg. Surg. 2023, 18, 16. [Google Scholar] [CrossRef] [PubMed]
- Aubrion, A.; Clanet, R.; Jourdan, J.P.; Creveuil, C.; Roupie, E.; Macrez, R. FRENCH versus ESI: Comparison between two nurse triage emergency scales with referent scenarios. BMC Emerg. Med. 2022, 22, 201. [Google Scholar] [CrossRef] [PubMed]
- Roquette, B.P.; Nagano, H.; Marujo, E.C.; Maiorano, A.C. Prediction of admission in pediatric emergency department with deep neural networks and triage textual data. Neural Netw. 2020, 126, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Lucke, J.A.; Mooijaart, S.P.; Conroy, S.; Blomaard, L.C.; De Groot, B.; Nickel, C.H. Mortality risk for different presenting complaints amongst older patients assessed with the Manchester triage system. Eur. Geriatr. Med. 2022, 123, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, S.; Littmann, J.; Stempien, J.; Kapur, P.; Bryce, R.; Betz, M. A Comparison Between Computer-Assisted Self-Triage by Patients and Triage Performed by Nurses in the Emergency Department. Cureus 2021, 13, e14002. [Google Scholar] [CrossRef] [PubMed]
- Emergency Triage: Manchester Triage Group, 3rd Edition (Version 3.8, 2023)|Wiley. Available online: https://www.wiley.com/en-fr/Emergency+Triage%3A+Manchester+Triage+Group%2C+3rd+Edition+(Version+3.8%2C+2023)-p-9781118299067 (accessed on 21 May 2024).
- Cairós-Ventura, L.M.; de Las Mercedes Novo-Muñoz, M.; Rodríguez-Gómez, J.Á.; Ortega-Benítez, Á.M.; Ortega-Barreda, E.M.; Aguirre-Jaime, A. Validity and Reliability of the Emergency Severity Index in a Spanish Hospital. Int. J. Environ. Res. Public. Health 2019, 16, 4567. [Google Scholar] [CrossRef]
- Baumann, M.R.; Strout, T.D. Triage of geriatric patients in the emergency department: Validity and survival with the Emergency Severity Index. Ann. Emerg. Med. 2007, 49, 234–240. [Google Scholar] [CrossRef]
- Esi-Implementation-Handbook-2020—Implementation Handbook 2020 Edition Esi Emergency Severity Index a Triage Tool for Emergency Department. Available online: https://www.sgnor.ch/fileadmin/user_upload/Dokumente/Downloads/Esi_Handbook.pdf (accessed on 21 May 2024).
- Murray, M.J. The Canadian Triage and Acuity Scale: A Canadian perspective on emergency department triage. Emerg. Med. Fremantle WA 2003, 15, 6–10. [Google Scholar] [CrossRef] [PubMed]
- ACEM—Triage. Available online: https://acem.org.au/Content-Sources/Advancing-Emergency-Medicine/Better-Outcomes-for-Patients/Triage (accessed on 21 May 2024).
- Travers, D.A.; Waller, A.E.; Bowling, J.M.; Flowers, D.; Tintinalli, J. Five-level triage system more effective than three-level in tertiary emergency department. J. Emerg. Nurs. 2002, 28, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Jelinek, G.A.; Little, M. Inter-rater reliability of the National Triage Scale over 11,500 simulated occasions of triage. Emerg. Med. 1996, 8, 226–230. [Google Scholar] [CrossRef]
- Beveridge, R.; Ducharme, J.; Janes, L.; Beaulieu, S.; Walter, S. Reliability of the Canadian emergency department triage and acuity scale: Interrater agreement. Ann. Emerg. Med. 1999, 34, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Hinson, J.S.; Martinez, D.A.; Schmitz, P.S.K.; Toerper, M.; Radu, D.; Scheulen, J.; Stewart de Ramirez, S.A.; Levin, S. Accuracy of emergency department triage using the Emergency Severity Index and independent predictors of under-triage and over-triage in Brazil: A retrospective cohort analysis. Int. J. Emerg. Med. 2018, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Larburu, N.; Azkue, L.; Kerexeta, J. Predicting Hospital Ward Admission from the Emergency Department: A Systematic Review. J. Pers. Med. 2023, 13, 849. [Google Scholar] [CrossRef] [PubMed]
- McLeod, S.L.; McCarron, J.; Ahmed, T.; Grewal, K.; Mittmann, N.; Scott, S.; Ovens, H.; Garay, J.; Bullard, M.; Rowe, B.H.; et al. Interrater Reliability, Accuracy, and Triage Time Pre- and Post-implementation of a Real-Time Electronic Triage Decision-Support Tool. Ann. Emerg. Med. 2020, 75, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Aeimchanbanjong, K.; Pandee, U. Validation of different pediatric triage systems in the emergency department. World J. Emerg. Med. 2017, 8, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Rashid, K.; Ullah, M.; Ahmed, S.T.; Sajid, M.Z.; Hayat, M.A.; Nawaz, B.; Abbas, K. Accuracy of Emergency Room Triage Using Emergency Severity Index (ESI): Independent Predictor of Under and Over Triage. Cureus 2021, 13, e20229. [Google Scholar] [CrossRef]
- Saberian, S.M.; Chester, D.J.; Udobi, K.F.; Childs, E.W.; Danner, O.K.; Sola, R. A Comparative Analysis of Hospital Triage Systems in the Geriatric Adult Trauma Patients: A Quality Improvement Pilot Study. Am. Surg. 2023, 89, 2300–2305. [Google Scholar] [CrossRef]
- Chi, C.-H.; Huang, C.-M. Comparison of the Emergency Severity Index (ESI) and the Taiwan Triage System in predicting resource utilization. J. Formos. Med. Assoc. Taiwan. Yi Zhi 2006, 105, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Zakeri, H.; Afshari Saleh, L.; Niroumand, S.; Ziadi-Lotfabadi, M. Comparison the Emergency Severity Index and Manchester Triage System in Trauma Patients. Bull. Emerg. Trauma. 2022, 10, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Storm-Versloot, M.N.; Ubbink, D.T.; Kappelhof, J.; Luitse, J.S.K. Comparison of an informally structured triage system, the emergency severity index, and the manchester triage system to distinguish patient priority in the emergency department. Acad. Emerg. Med. 2011, 18, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Cooke, M.W.; Jinks, S. Does the Manchester triage system detect the critically ill? J. Accid. Emerg. Med. 1999, 16, 179–181. [Google Scholar] [CrossRef]
- Dippenaar, E. Reliability and validity of three international triage systems within a private health-care group in the Middle East. Int. Emerg. Nurs. 2020, 51, 100870. [Google Scholar] [CrossRef]
- Ebrahimi, M.; Mirhaghi, A.; Najafi, Z.; Shafaee, H.; Hamechizfahm Roudi, M. Are Pediatric Triage Systems Reliable in the Emergency Department? Emerg. Med. Int. 2020, 2020, 9825730. [Google Scholar] [CrossRef] [PubMed]
- Beck, N.; Michel, M.; Binder, E.; Kapelari, K.; Maurer, M.; Lamina, C.; Müller, T.; Karall, D.; Scholl-Bürgi, S. The Manchester Triage System in a Pediatric Emergency Department of an Austrian University Hospital: A Retrospective Analysis of Urgency Levels. Pediatr. Emerg. Care 2022, 38, e639–e643. [Google Scholar] [CrossRef]
- Araz, O.M.; Olson, D.; Ramirez-Nafarrate, A. Predictive analytics for hospital admissions from the emergency department using triage information. Int. J. Prod. Econ. 2019, 208, 199–207. [Google Scholar] [CrossRef]
- Predicting Hospital Admission at Emergency Department Triage Using Machine Learning. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0201016 (accessed on 21 May 2024).
- Parker, C.A.; Liu, N.; Wu, S.X.; Shen, Y.; Lam, S.S.W.; Ong, M.E.H. Predicting hospital admission at the emergency department triage: A novel prediction model. Am. J. Emerg. Med. 2019, 37, 1498–1504. [Google Scholar] [CrossRef]
- Coslovsky, M.; Takala, J.; Exadaktylos, A.K.; Martinolli, L.; Merz, T.M. A clinical prediction model to identify patients at high risk of death in the emergency department. Intensive Care Med. 2015, 41, 1029–1036. [Google Scholar] [CrossRef]
- Dinh, M.M.; Russell, S.B.; Bein, K.J.; Rogers, K.; Muscatello, D.; Paoloni, R.; Hayman, J.; Chalkley, D.R.; Ivers, R. The Sydney Triage to Admission Risk Tool (START) to predict Emergency Department Disposition: A derivation and internal validation study using retrospective state-wide data from New South Wales, Australia. BMC Emerg. Med. 2016, 16, 46. [Google Scholar] [CrossRef]
- Ebker-White, A.A.; Bein, K.J.; Dinh, M.M. The Sydney Triage to Admission Risk Tool (START): A prospective validation study. Emerg. Med. Australas. EMA 2018, 30, 511–516. [Google Scholar] [CrossRef]
- Raita, Y.; Goto, T.; Faridi, M.K.; Brown, D.F.M.; Camargo, C.A.; Hasegawa, K. Emergency department triage prediction of clinical outcomes using machine learning models. Crit. Care Lond. Engl. 2019, 23, 64. [Google Scholar] [CrossRef]
- Sánchez-Salmerón, R.; Gómez-Urquiza, J.L.; Albendín-García, L.; Correa-Rodríguez, M.; Martos-Cabrera, M.B.; Velando-Soriano, A.; Suleiman-Martos, N. Machine learning methods applied to triage in emergency services: A systematic review. Int. Emerg. Nurs. 2022, 60, 101109. [Google Scholar] [CrossRef]
- Hwang, S.; Lee, B. Machine learning-based prediction of critical illness in children visiting the emergency department. PLoS ONE 2022, 17, e0264184. [Google Scholar] [CrossRef] [PubMed]
- Lu, T.-C.; Wang, C.-H.; Chou, F.-Y.; Sun, J.-T.; Chou, E.H.; Huang, E.P.-C.; Tsai, C.-L.; Ma, M.H.-M.; Fang, C.-C.; Huang, C.-H. Machine learning to predict in-hospital cardiac arrest from patients presenting to the emergency department. Intern. Emerg. Med. 2023, 18, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Yao, L.-H.; Leung, K.-C.; Tsai, C.-L.; Huang, C.-H.; Fu, L.-C. A Novel Deep Learning-Based System for Triage in the Emergency Department Using Electronic Medical Records: Retrospective Cohort Study. J. Med. Internet Res. 2021, 23, e27008. [Google Scholar] [CrossRef]
- Miles, J.; Turner, J.; Jacques, R.; Williams, J.; Mason, S. Using machine-learning risk prediction models to triage the acuity of undifferentiated patients entering the emergency care system: A systematic review. Diagn. Progn. Res. 2020, 4, 16. [Google Scholar] [CrossRef]
- Levin, S.; Toerper, M.; Hamrock, E.; Hinson, J.S.; Barnes, S.; Gardner, H.; Dugas, A.; Linton, B.; Kirsch, T.; Kelen, G. Machine-Learning-Based Electronic Triage More Accurately Differentiates Patients With Respect to Clinical Outcomes Compared With the Emergency Severity Index. Ann. Emerg. Med. 2018, 71, 565–574.e2. [Google Scholar] [CrossRef]
- Fernandes, M.; Mendes, R.; Vieira, S.M.; Leite, F.; Palos, C.; Johnson, A.; Finkelstein, S.; Horng, S.; Celi, L.A. Predicting Intensive Care Unit admission among patients presenting to the emergency department using machine learning and natural language processing. PLoS ONE 2020, 15, e0229331. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kang, W.S.; Kim, D.W.; Seo, S.H.; Kim, J.; Jeong, S.T.; Yon, D.K.; Lee, J. An Artificial Intelligence Model for Predicting Trauma Mortality Among Emergency Department Patients in South Korea: Retrospective Cohort Study. J. Med. Internet Res. 2023, 25, e49283. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, S.K.; Choi, J.; Lee, Y. Reliability of ChatGPT for performing triage task in the emergency department using the Korean Triage and Acuity Scale. Digit. Health 2024, 10, 1–9. [Google Scholar] [CrossRef]
- Akhlaghi, H.; Freeman, S.; Vari, C.; McKenna, B.; Braitberg, G.; Karro, J.; Tahayori, B. Machine learning in clinical practice: Evaluation of an artificial intelligence tool after implementation. Emerg. Med. Australas. EMA 2024, 36, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Meral, G.; Ateş, S.; Günay, S.; Öztürk, A.; Kuşdoğan, M. Comparative analysis of ChatGPT, Gemini and emergency medicine specialist in ESI triage assessment. Am. J. Emerg. Med. 2024, 81, 146–150. [Google Scholar] [CrossRef]
- Sarty, J.; Fitzpatrick, E.A.; Taghavi, M.; VanBerkel, P.T.; Hurley, K.F. Machine learning to identify attributes that predict patients who leave without being seen in a pediatric emergency department. CJEM 2023, 25, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Ahun, E.; Demir, A.; Yiğit, Y.; Tulgar, Y.K.; Doğan, M.; Thomas, D.T.; Tulgar, S. Perceptions and concerns of emergency medicine practitioners about artificial intelligence in emergency triage management during the pandemic: A national survey-based study. Front. Public Health 2023, 11, 1285390. [Google Scholar] [CrossRef]
- Okada, Y.; Ning, Y.; Ong, M.E.H. Explainable artificial intelligence in emergency medicine: An overview. Clin. Exp. Emerg. Med. 2023, 10, 354–362. [Google Scholar] [CrossRef]
- Zachariasse, J.M.; van der Hagen, V.; Seiger, N.; Mackway-Jones, K.; van Veen, M.; Moll, H.A. Performance of triage systems in emergency care: A systematic review and meta-analysis. BMJ Open 2019, 9, e026471. [Google Scholar] [CrossRef]
- Parenti, N.; Reggiani, M.L.B.; Iannone, P.; Percudani, D.; Dowding, D. A systematic review on the validity and reliability of an emergency department triage scale, the Manchester Triage System. Int. J. Nurs. Stud. 2014, 51, 1062–1069. [Google Scholar] [CrossRef]
| ATS | CTAS | ESI | MTS | |
|---|---|---|---|---|
| Validity | +/? Little research [2] | +/? Good [2] | +/? [2] Different results analyses in research, though seems more accurate in a group of children and elderly people than MTS [19,21,22] | +/? [2] Contradictory data depending on the study. Probably depending on the age of the patient and distance hospital from place uprising triage system |
| Reliability Kappa value | 0.25 to 0.56, but decreases in the group of patients with mental disorders [2] | Adults 0.68–0.89 Children 0.51–0.72 [2] | Adults 0.46–0.91 Children 0.82 [2] | Adults 0.31–0.62 [2] |
| Simplicity (subjective evaluation) | ++ | + | +(+) Seems to depend on the presence of clear guidelines (diagnostic and treatment standards) in the hospital | ++ |
| Short time of performance | Time depends on patient priority, the higher the priority the shorter the time | Time depends on patient priority, the higher the priority the shorter the time | Time depends on patient priority, the higher the priority the shorter the time | Time depends on patient priority, the higher the priority the shorter the time |
| Formalized structure | + | + | + | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ingielewicz, A.; Rychlik, P.; Sieminski, M. Drinking from the Holy Grail—Does a Perfect Triage System Exist? And Where to Look for It? J. Pers. Med. 2024, 14, 590. https://doi.org/10.3390/jpm14060590
Ingielewicz A, Rychlik P, Sieminski M. Drinking from the Holy Grail—Does a Perfect Triage System Exist? And Where to Look for It? Journal of Personalized Medicine. 2024; 14(6):590. https://doi.org/10.3390/jpm14060590
Chicago/Turabian StyleIngielewicz, Anna, Piotr Rychlik, and Mariusz Sieminski. 2024. "Drinking from the Holy Grail—Does a Perfect Triage System Exist? And Where to Look for It?" Journal of Personalized Medicine 14, no. 6: 590. https://doi.org/10.3390/jpm14060590
APA StyleIngielewicz, A., Rychlik, P., & Sieminski, M. (2024). Drinking from the Holy Grail—Does a Perfect Triage System Exist? And Where to Look for It? Journal of Personalized Medicine, 14(6), 590. https://doi.org/10.3390/jpm14060590






