A Microscopy Evaluation of Emergence Profile Surfaces of Dental Custom CAD-CAM Implant Abutments and Dental Implant Stock Abutments
Abstract
1. Introduction
2. Materials and Methods
- Five-axis milling machine with power of 2.7 kW Yenadent D43 (Yena, Istanbul, Turkey);
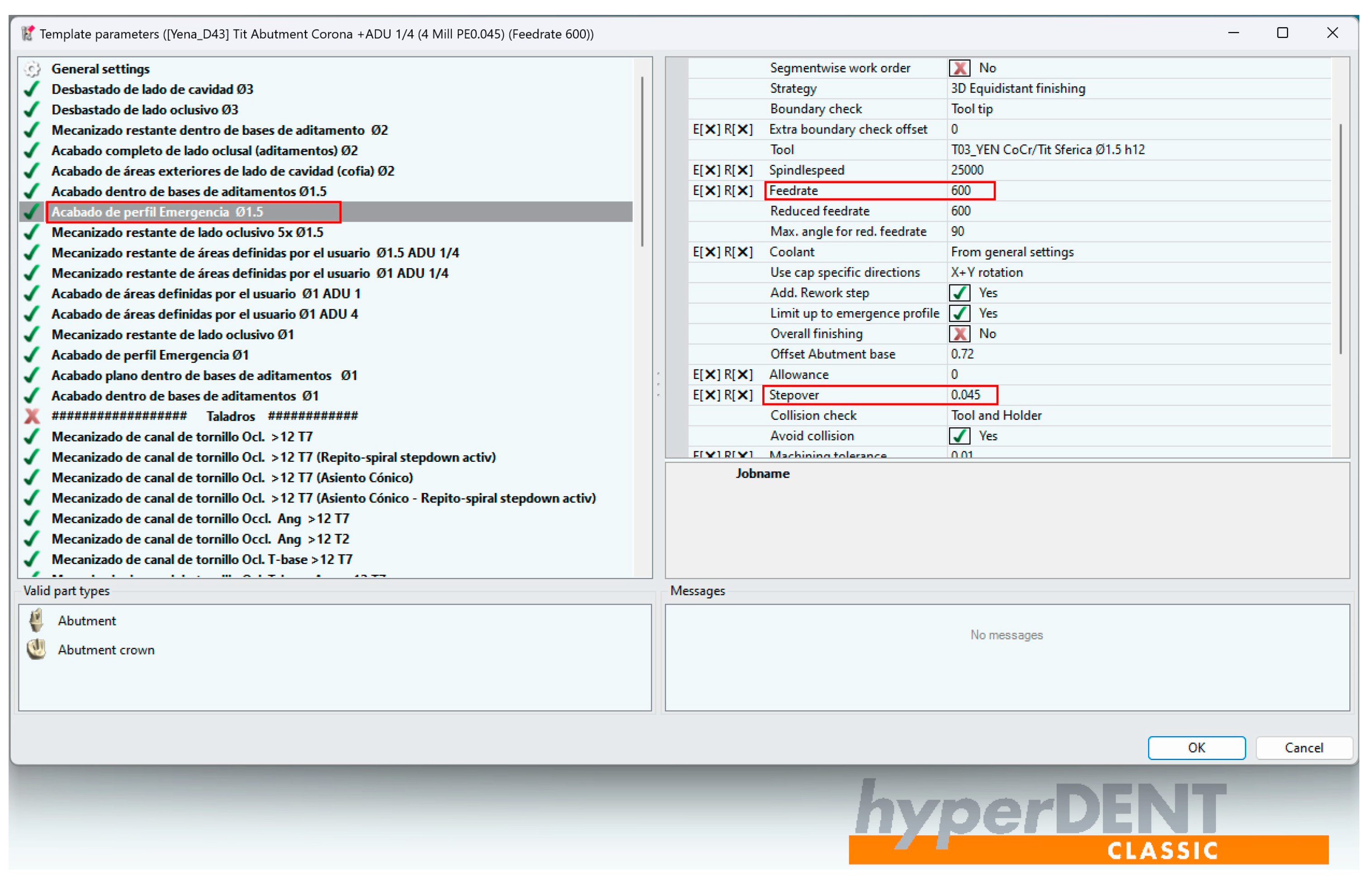
- hyperDENT Classic v9.4 CAM software (FOLLOW-ME!Technology Group, Munich, Germany;
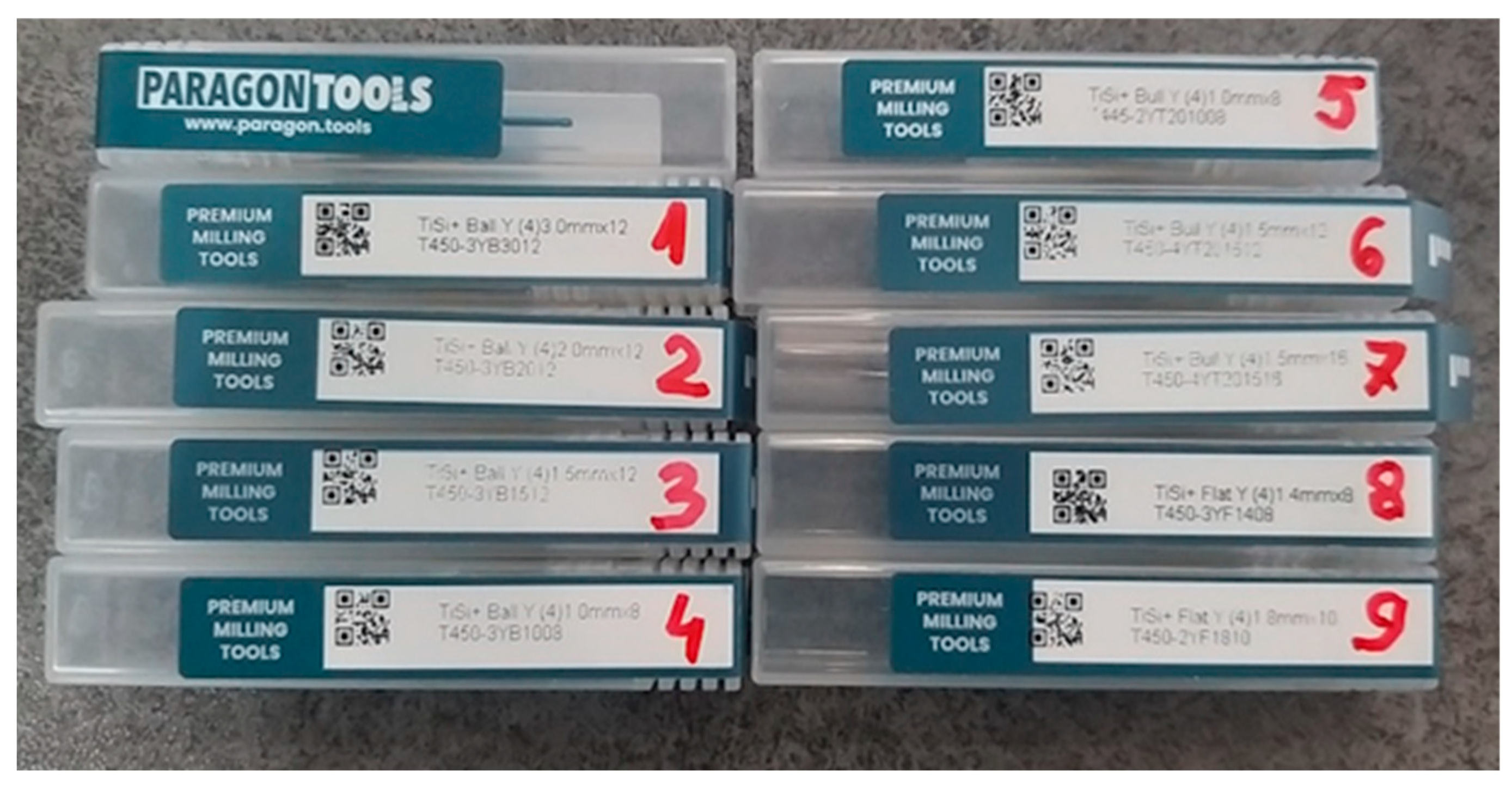
- Yenadent compatible metal milling tools from Paragon Tools (Paragon Tools, Barcelona, Spain);
- Specialized design software Exocad DentalCAD v3.2 Elefsina (Exocad GmgH, Darmstadt, Germany);
- CAD/CAM Implant Library from Yenadent (Yena, Istanbul, Turkey);
- Titanium disc type 5 grade 23 Nicrallium TA6V ELI diameter of 98.5 mm, and thickness of 14 mm (BCS Dental Alloys, Chassieu, France).
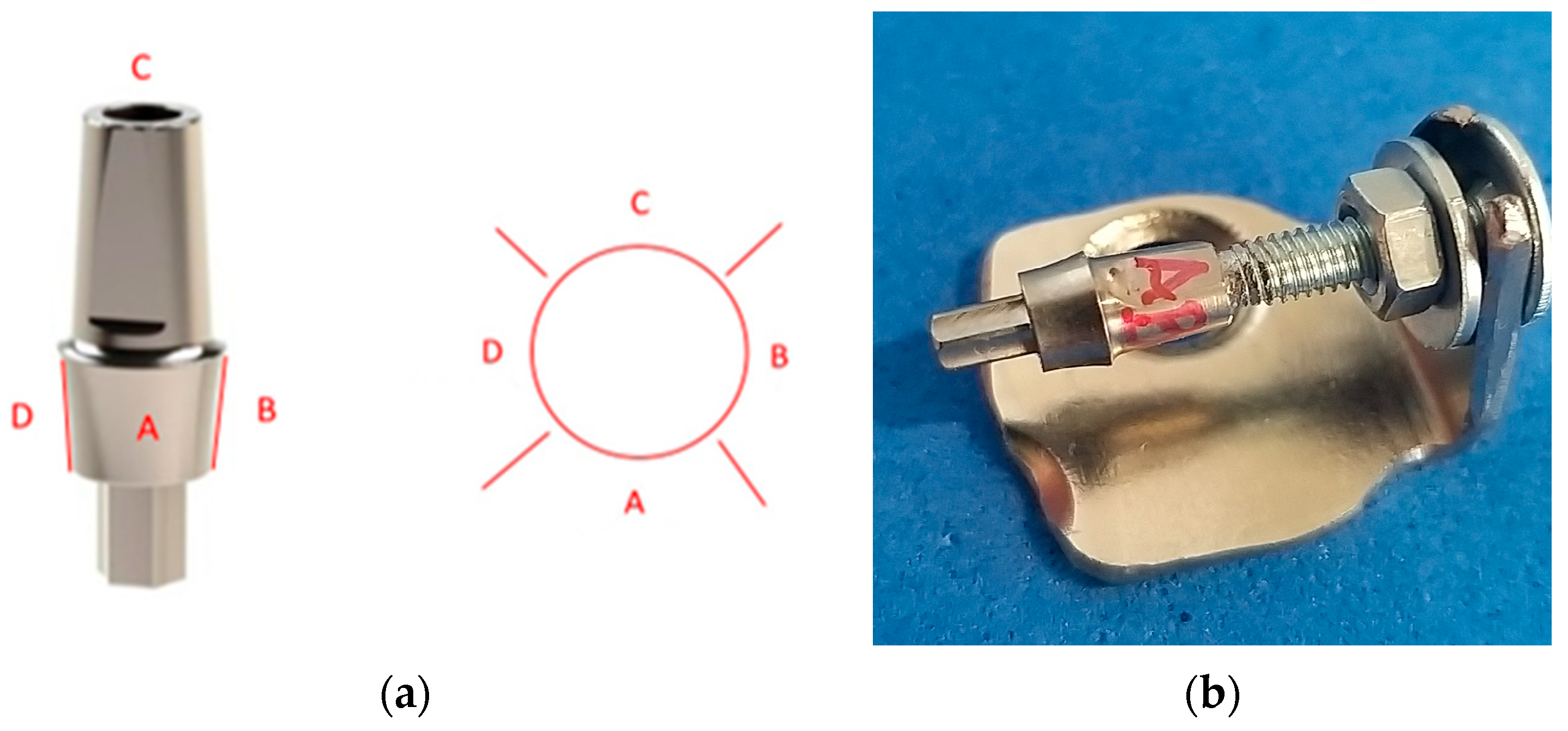
2.1. Compatible Custom CAD/CAM Dental Implant Design
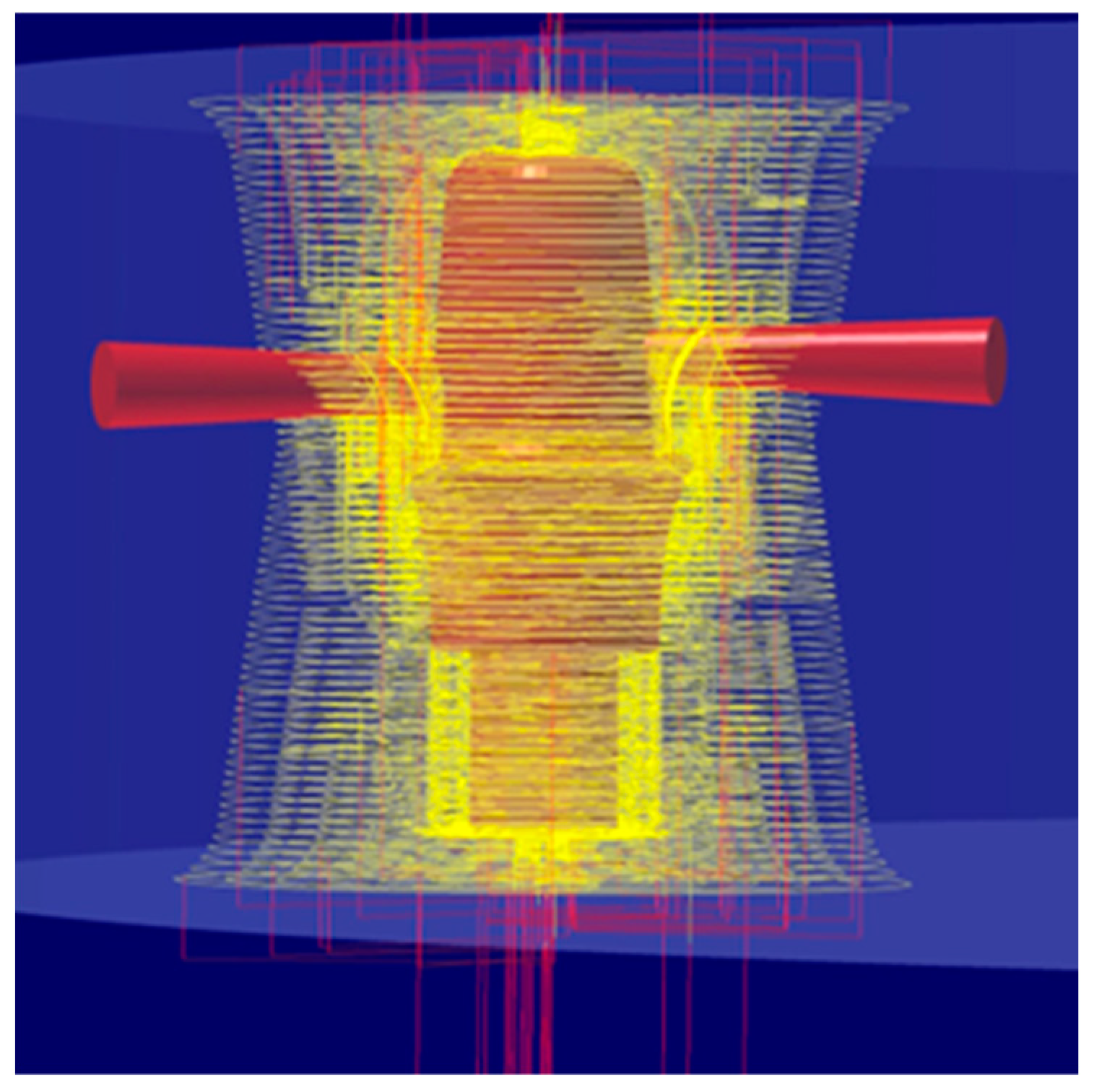
2.2. Adjustment of Parameters Using the CAM hyperDENT Software and Settings of Tools from Paragon Tools
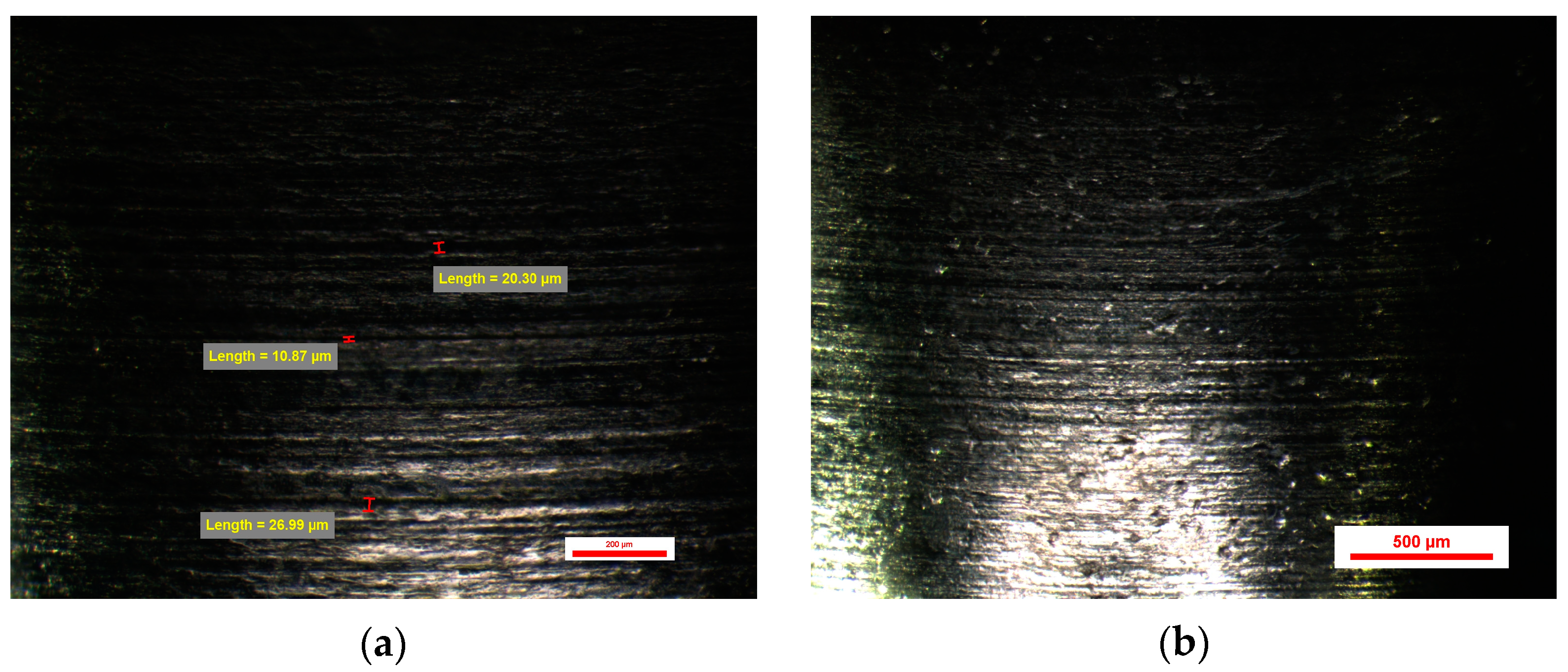
2.3. Nikon Stereomicroscope SMZ745T
2.4. Statistical Analysis
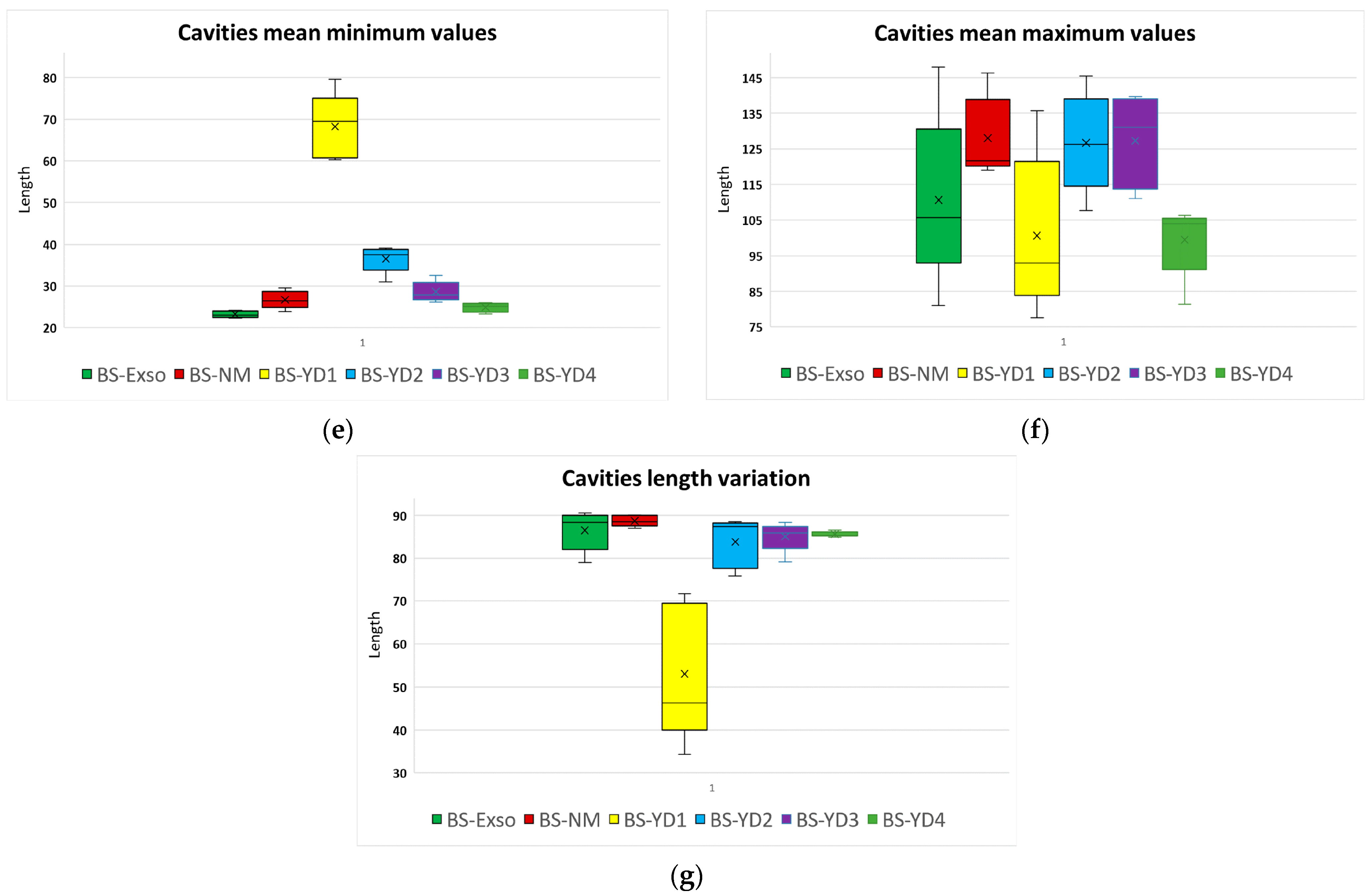
- Total number of micro-cavities, obtained by summing the cavities identified on each face.
- The smallest and the largest cavities, by comparing the min and max values for each face; these values express the exact range of cavities’ sizes present all over the abutment surface.
- Length variation, computed as the ratio between the size range and the maximum length (expressed as percentages); this is a percentual variation of the size of cavities from the entire surface of the abutment.
- The arithmetic mean of the three initial parameters identified for each face; these values express the overall surface of the abutment.
- The variance of the min values and max values measured for the four faces (defined as the degree of spreading of the values within the smallest and largest value).
3. Results
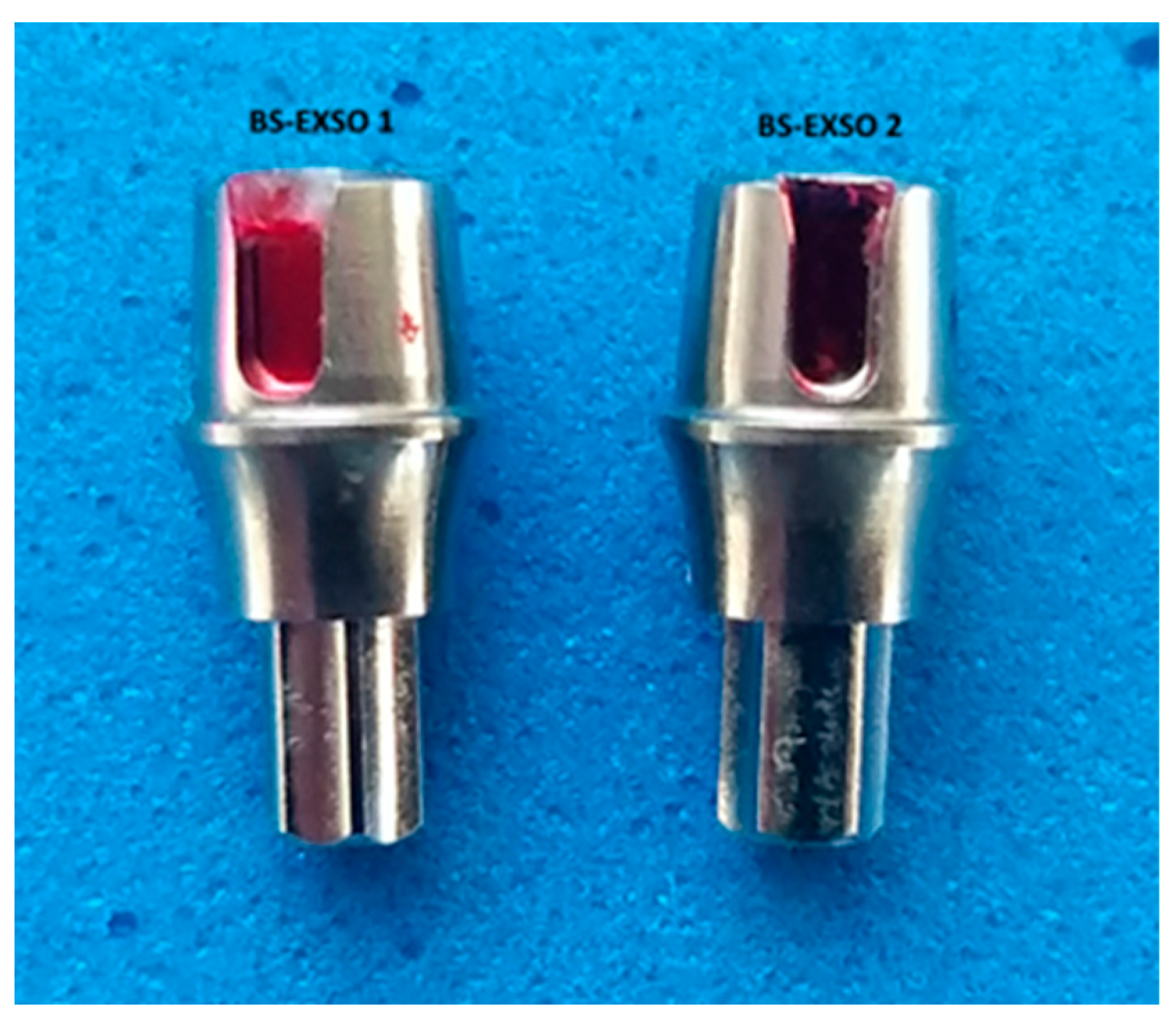
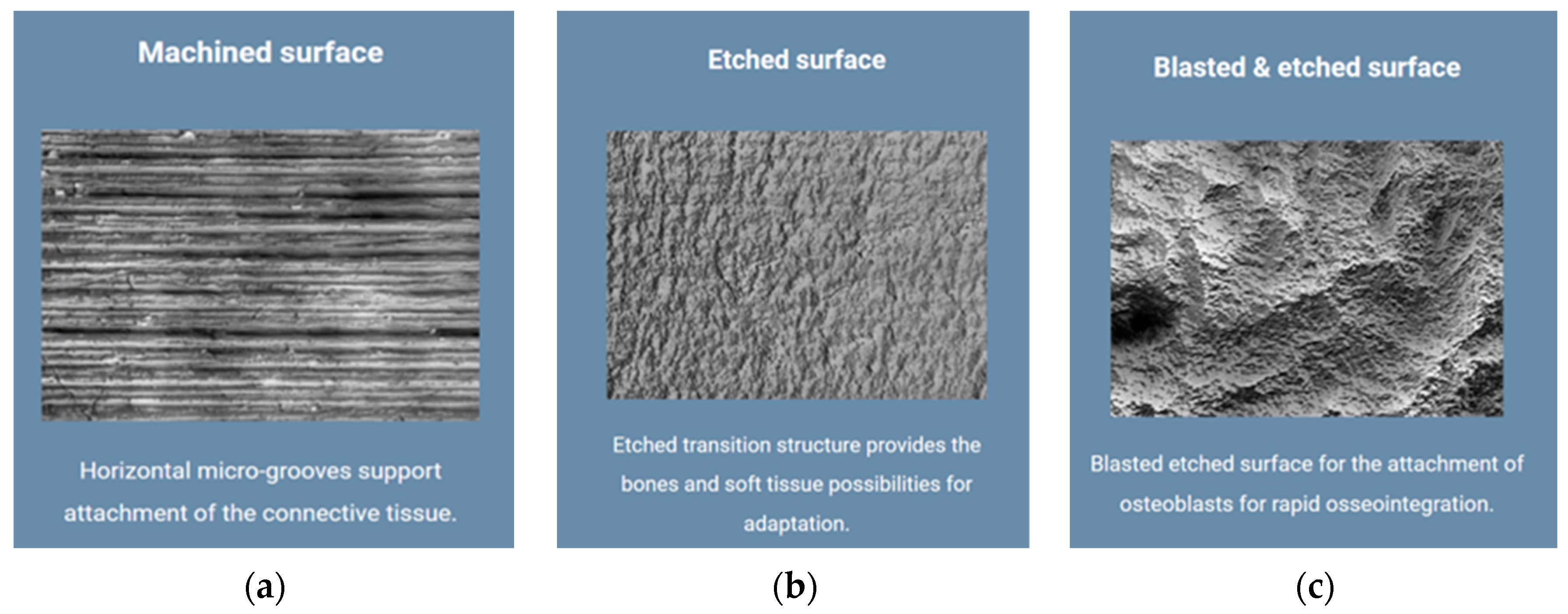
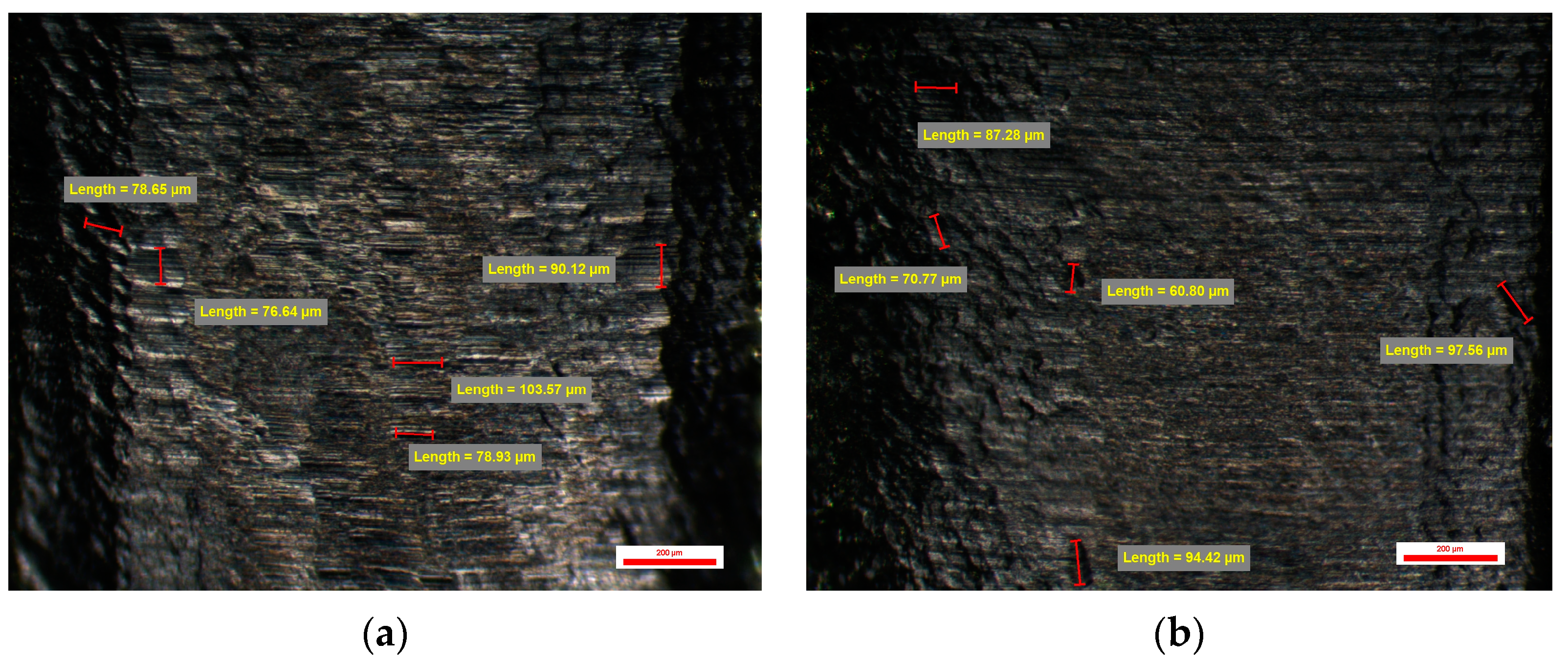
3.1. Surface Quality of the Emergence Profile of the Original Dental Implant Abutments (Control Group BS-Exso)
3.2. Surface Quality of the Emergence Profile of the Compatible Dental Implant Abutments (Study Group BS-NM)
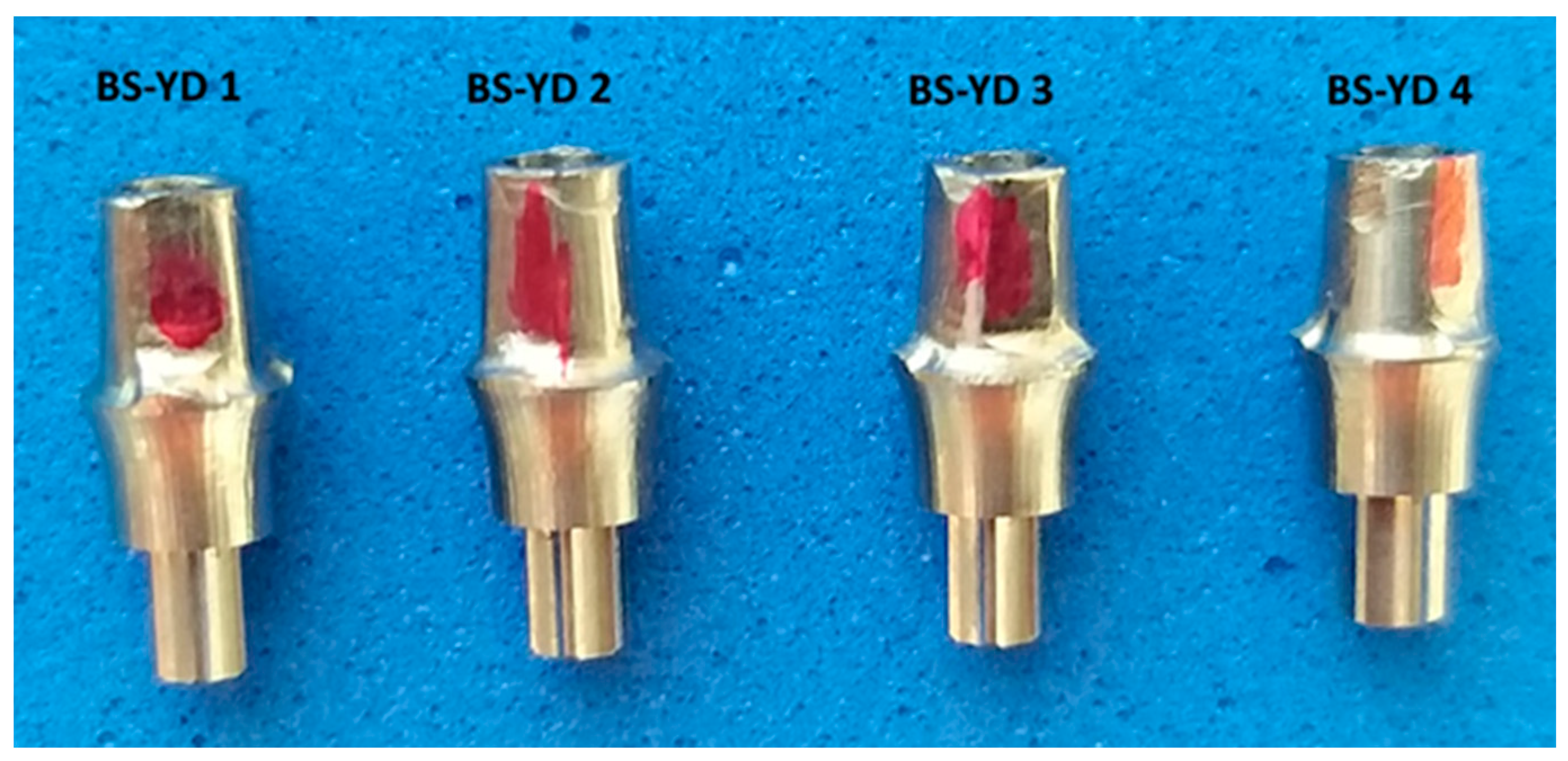
3.3. Surface Quality of the Emergence Profile of the Customized Dental Implant Abutments (Study Groups)
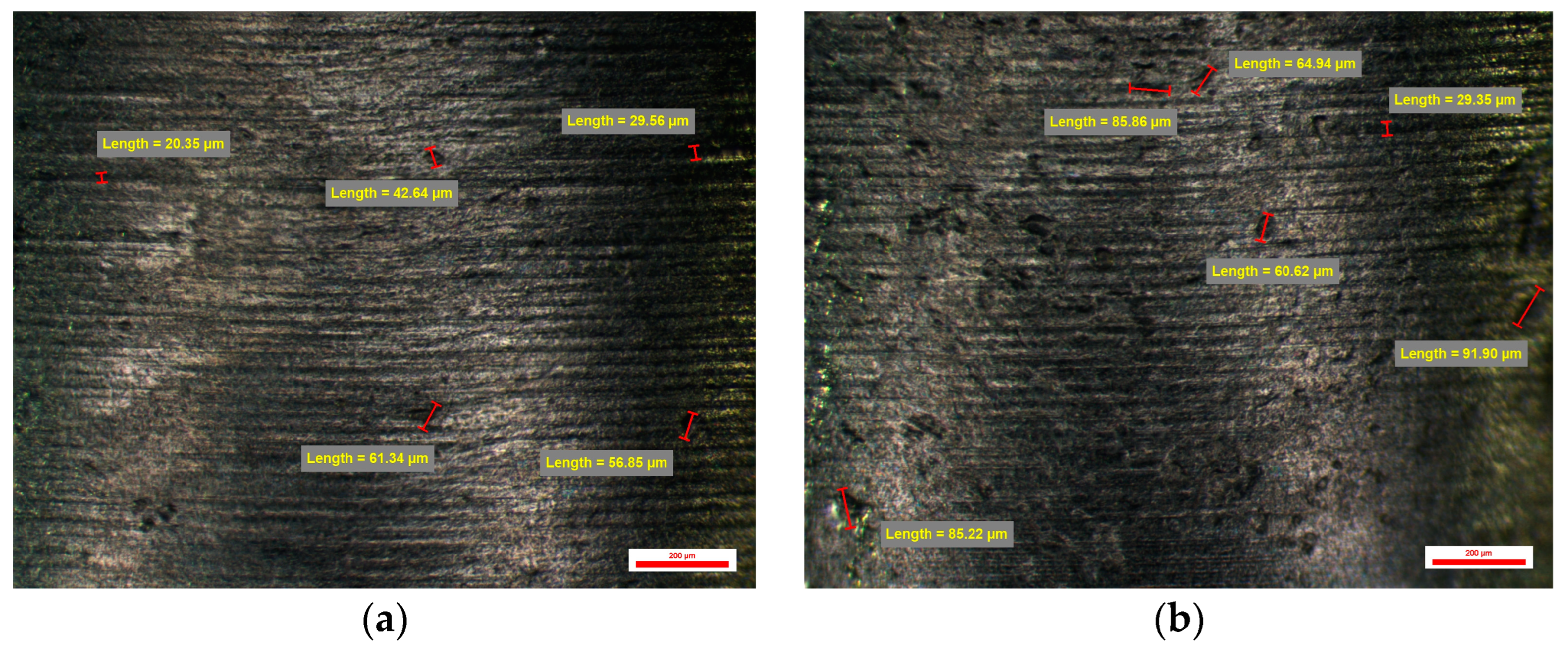
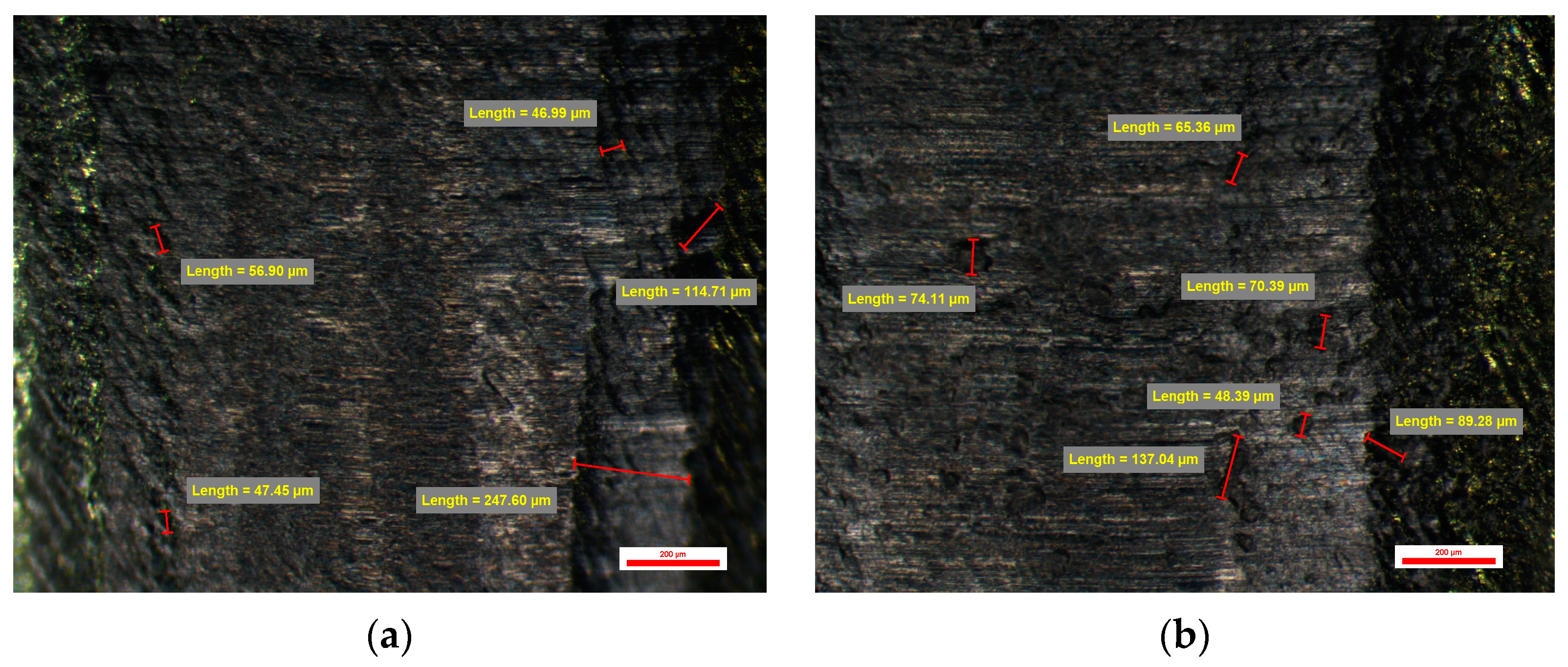
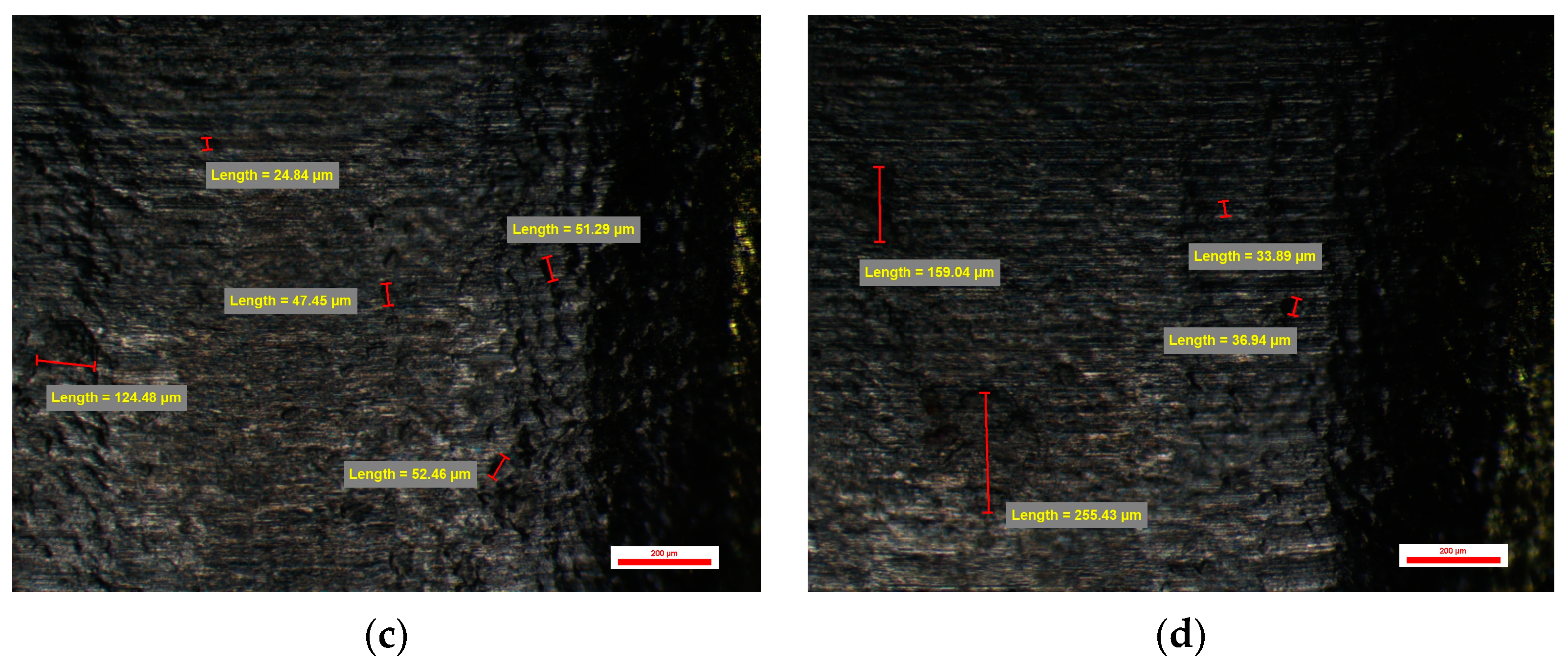
3.3.1. Surface Quality of the Emergence Profile of the Customized Dental Implant Abutments from Lot 3 (Study Group BS-YD1)
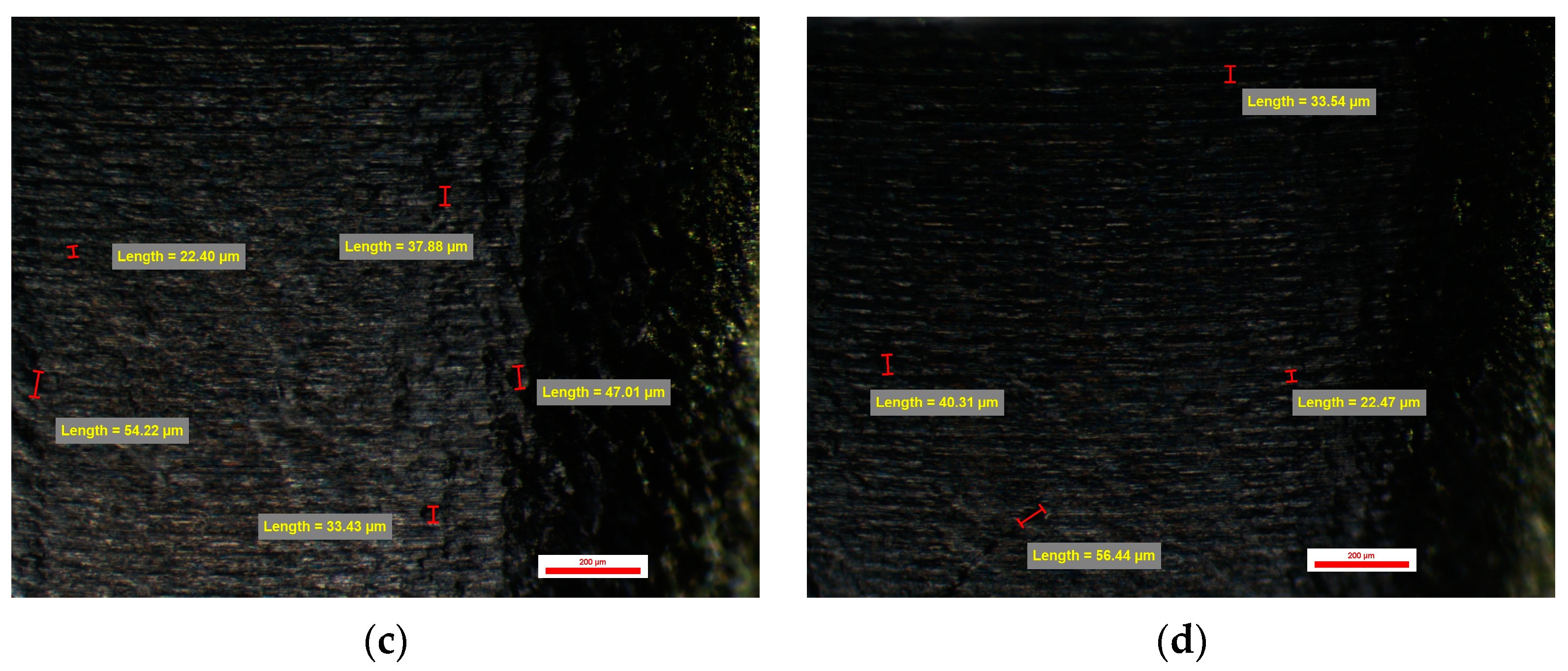
3.3.2. Surface Quality of the Emergence Profile of the Customized Dental Implant Abutments from Lot 4 (Study Group BS-YD2)
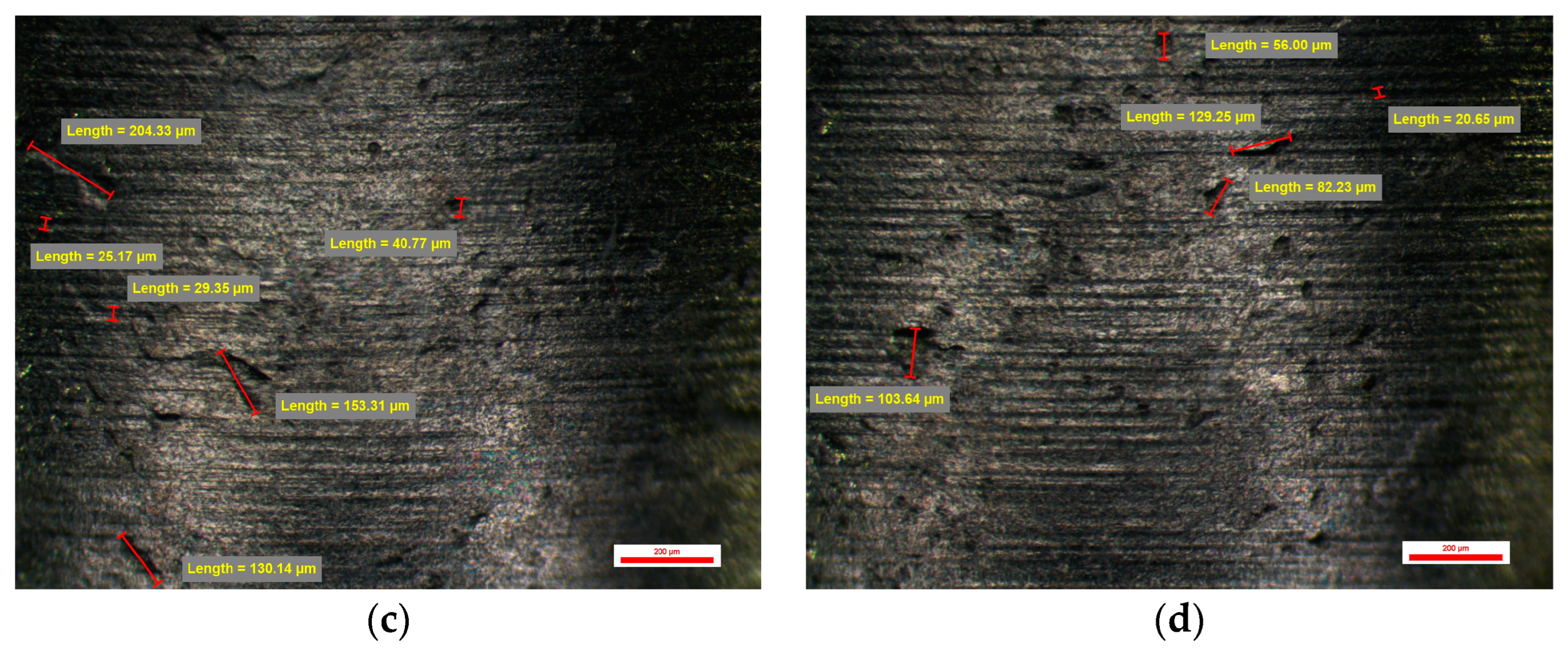
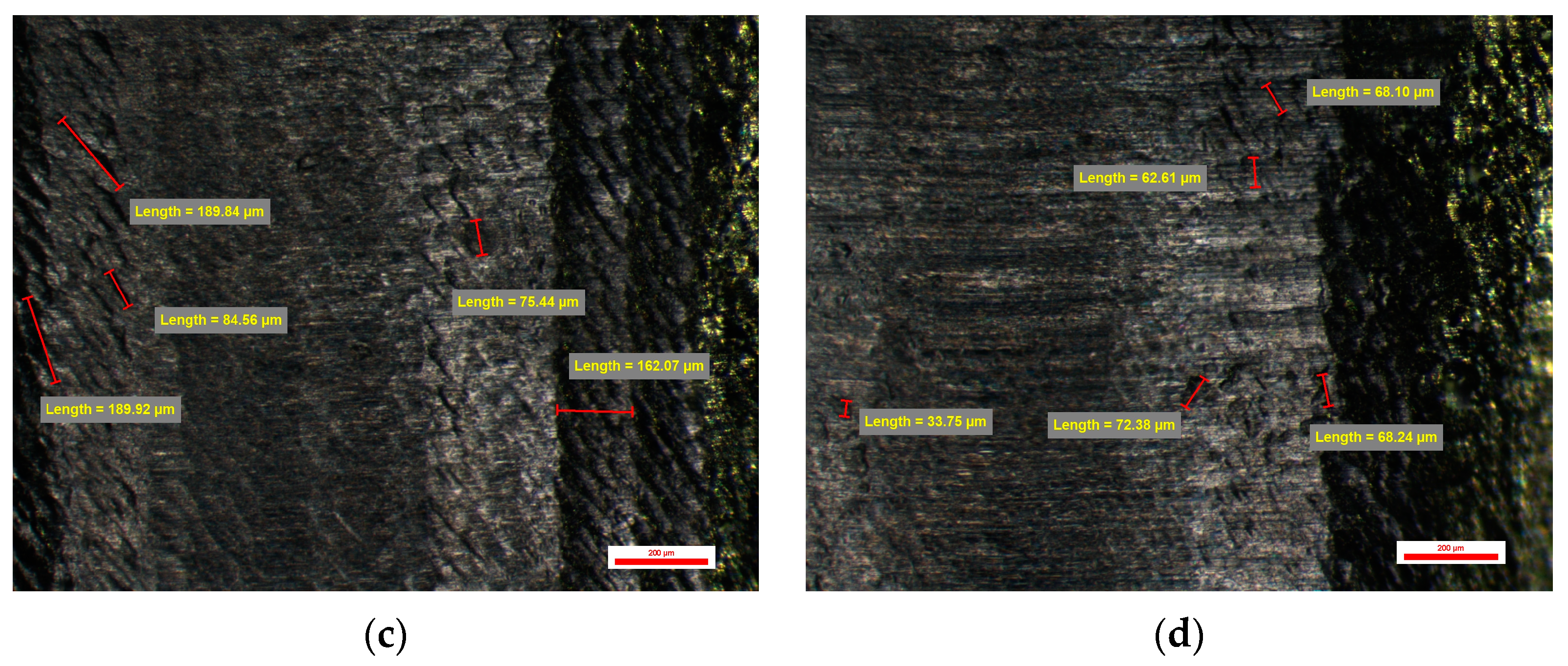
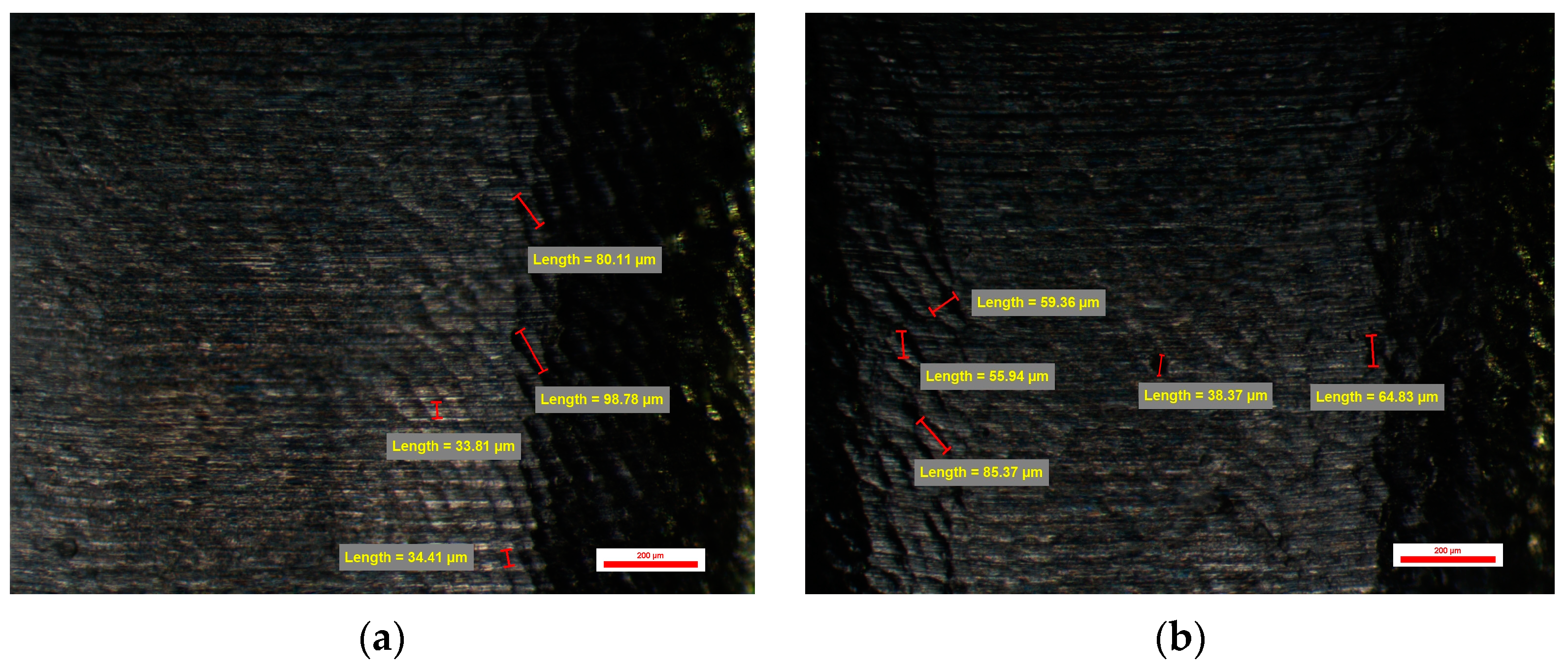
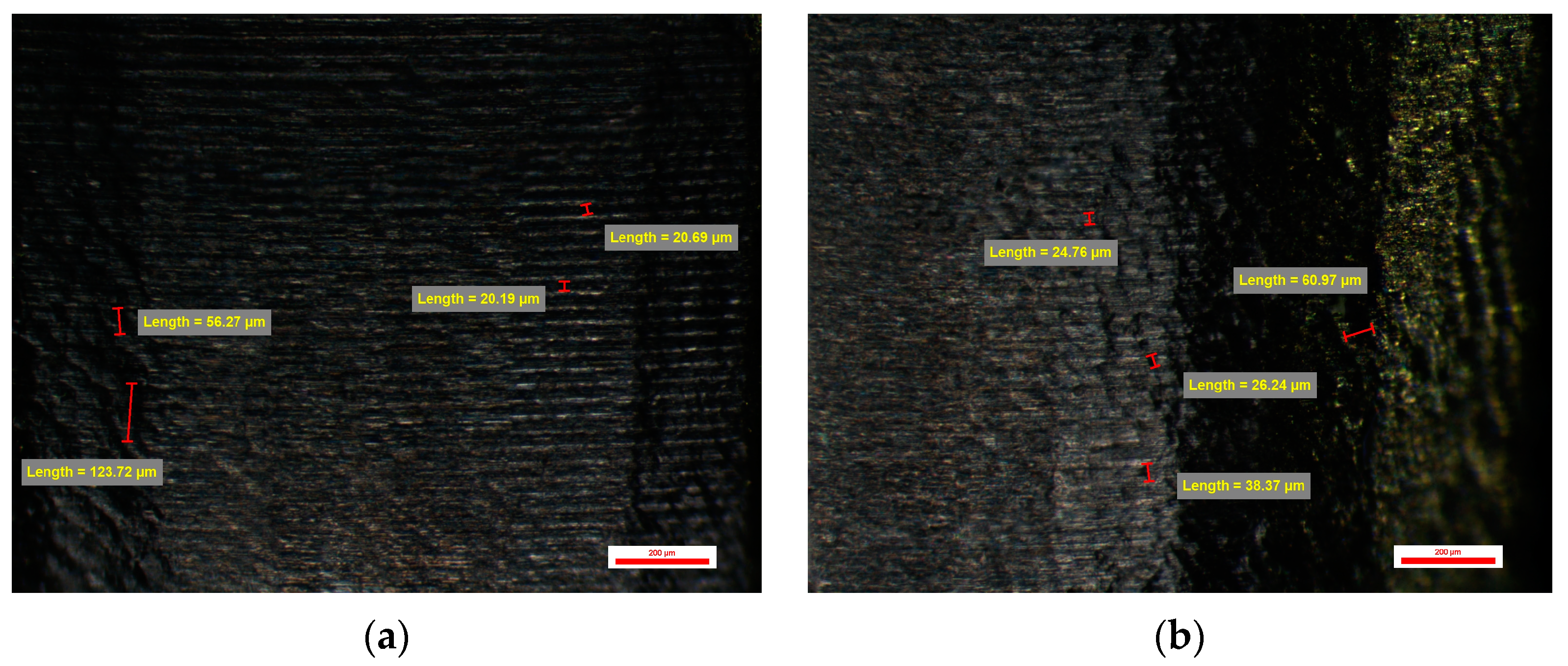
3.3.3. Surface Quality of the Emergence Profile of the Customized Dental Implant Abutments from Lot 5 (Study Group BS-YD3)
3.3.4. Surface Quality of the Emergence Profile of the Customized Dental Implant Abutments from Lot 6 (Study Group BS-YD4)
4. Discussion
5. Conclusions
- -
- The surface quality of the emergence profile of the non-industrial compatible CAD/CAM milled dental implant abutments represents a safe solution for customized prosthetics on the dental implant; the surface with horizontal micro-grooves observed in the original dental implant stock abutments is also found in the non-industrial milled abutments in the dental laboratory.
- -
- Obtaining a non-industrial-compatible CAD/CAM custom-milled dental implant abutment surface quality is possible in the dental laboratory if it is equipped with CAM software such as hyperDENT that allows the modification of the milling parameters so that the results can be improved to obtain the best results, but also the use of the most suitable milling tools, in our case Paragon Tools.
- -
- The use of specific Stepover (0.045 mm) and Feed Rate (600 mm/min) parameters during the milling process influences the surface roughness of the emergence profile for the customized dental implant abutments, making it possible to obtain a surface similar to the original;
- -
- The use of a higher resolution in milling abutments resulted in a smoother surface of the emergence profile compared to the original abutments.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ahmed, S.E.; Kalaignan, P.; Mohan, J. Evaluation of Microgap at the Implant-Abutment Interface with Premachined and Custom Cast Implant Abutments—An in vitro Study. J. Adv. Med. Dent. Sci. Res. 2019, 7, 23–32. [Google Scholar]
- Kim, S.; Choi, C.; Cha, Y.; Chang, J.S. The efficacy of convenient cleaning methods applicable for customized abutments: An in vitro study. BMC Oral Health 2021, 21, 78. [Google Scholar] [CrossRef] [PubMed]
- Femil Jilta, C.; Ravichandran, R.; Harsha Kumar, K.; Nair, V.V.; Janardanan, Z. Comparative evaluation of surface roughness of three different dental implant abutments using atomic force microscopy: An in vitro study. Int. J. Appl. Dent. Sci. 2020, 6, 643–647. [Google Scholar] [CrossRef]
- Sawase, T.; Wennerberg, A.; Hallgren, C.; Miyamoto, I.; Albrektsson, T. Atomic force microscopic study of commercially available implant abutments. Clin. Implant. Dent. Relat. Res. 1999, 1, 92–97. [Google Scholar] [CrossRef]
- Romanos, G.E. (Ed.) Front matter. In Saving Dental Implants; Wiley-Blackwell: Hoboken, NJ, USA, 2024; pp. 110–143. [Google Scholar]
- Morales, L.M.M.; Elias, C.N. Comparison of the Surface Roughness of Dental Implant Abutment and Tooth Root. Int. J. Dent. Diabetes Endocrinol. Oral Hyg. 2021, 3, 1–13. [Google Scholar]
- Nascimento, C.D.; Pita, M.S.; Fernandes, F.H.N.C.; Pedrazzi, V.; de Albuquerque Junior, R.F.; Ribeiro, R.F. Bacterial adhesion on the titanium and zirconia abutment surfaces. Clin. Oral Implant. Res. 2014, 25, 337–343. [Google Scholar] [CrossRef]
- Teughels, W.; Van Assche, N.; Sliepen, I.; Quirynen, M. Effect of material characteristics and/or surface topography on biofilm development. Clin. Oral Implant. Res. 2006, 17 (Suppl. S2), 68–81. [Google Scholar] [CrossRef]
- Quirynen, M.; Bollen, C.M. The influence of surface roughness and surface-free energy on supra- and subgingival plaque formation in man. A review of the literature. J. Clin. Periodontol. 1995, 22, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Munot, V.; Nayakar, R.; Patil, R. Effect of Surface Characteristics of Different Implant Abutment Materials on the Microbial Adhesion—An Invitro Study. J. Clin. Diagn. Res. 2021, 15, 10. [Google Scholar] [CrossRef]
- Mattheos, N.; Janda, M.; Acharya, A.; Pekarski, S.; Larsson, C. Impact of design elements of the implant supracrestal complex (ISC) on the risk of peri-implant mucositis and peri-implantitis: A critical review. Clin. Oral Implant. Res. 2021, 32 (Suppl. S21), 181–202. [Google Scholar] [CrossRef]
- Valente, N.; Wu, M.; Toti, P.; Derchi, G. Impact of Concave/Convergent vs Parallel/ Divergent Implant Transmucosal Profiles on Hard and Soft Peri-implant Tissues: A Systematic Review with Meta-Analyses. Int. J. Prosthodont. 2020, 33, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Siegenthaler, M.; Strauss, F.J.; Gamper, F.; Hämmerle, C.H.F.; Jung, R.E.; Thoma, D.S. Anterior implant restorations with a convex emergence profile increase the frequency of recession: 12-month results of a randomized controlled clinical trial. J. Clin. Periodontol. 2022, 49, 1145–1157. [Google Scholar] [CrossRef] [PubMed]
- Souza, A.; Alshihri, A.; Kämmerer, P.W.; Araújo, M.G.; Gallucci, G.O. Histological and micro-CT analysis of peri-implant soft and hard tissue healing on implants with different healing abutments configurations. Clin. Oral Implant. Res. 2018, 29, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Katafuchi, M.; Weinstein, B.F.; Leroux, B.G.; Chen, Y.W.; Daubert, D.M. Restoration contour is a risk indicator for peri-implantitis: A cross-sectional radiographic analysis. J. Clin. Periodontol. 2018, 45, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.; Koo, K.T.; Schwarz, F.; Ben Amara, H.; Și Heo, S.J. Association of prosthetic features and peri-implantitis: A cross-sectional study. J. Clin. Periodontol. 2020, 47, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Târtea, D.A.; Ionescu, M.; Manolea, H.O.; Mercuț, V.; Obădan, E.; Amărăscu, M.O.; Mărășescu, P.C.; Dăguci, L.; Popescu, S.M. Comparative Study of Dental Custom CAD-CAM Implant Abutments and Dental Implant Stock Abutments. J. Clin. Med. 2023, 12, 2128. [Google Scholar] [CrossRef]
- Târtea, D.A.; Popescu, S.M.; Manolea, H.O.; Ionescu, M.; Amărăscu, M.O.; Mărășescu, P.C.; Gîngu, O. Microscope evaluation of micro-gaps at Implant-Abutment connection. Rom. J. Oral Rehabil. 2024, 12, 411–423. [Google Scholar]
- Obădan, M.E.; Mitruț, I.; Ionescu, M.; Obădan, F.; Târtea, D.A.; Popescu, M.A.; Popescu, S.M.; Smarandache, A.M.; Manolea, H.O. Clinical Efficacy Analysis of the Personalization of Prosthetic Abutments in Implant Supported Restorations in Comparison to Available Standard Titanium Abutments. J. Pers. Med. 2023, 13, 1402. [Google Scholar] [CrossRef]
- Linkevicius, T.; Apse, P. Influence of abutment material on stability of peri-implant tissues: A systematic review. Int. J. Oral Maxillofac. Implant. 2008, 23, 449–456. [Google Scholar]
- Ferrari, M.; Cagidiaco, M.C.; Garcia-Godoy, F.; Goracci, C.; Cairo, F. Effect of different prosthetic abutments on peri-implant soft tissue. A randomized controlled clinical trial. Am. J. Dent. 2015, 28, 85–89. [Google Scholar]
- Chokaree, P.; Poovarodom, P.; Chaijareenont, P.; Yavirach, A.; Rungsiyakull, P. Biomaterials and Clinical Applications of Customized Healing Abutment-A Narrative Review. J. Funct. Biomater. 2022, 13, 291. [Google Scholar] [CrossRef] [PubMed]
- Chokaree, P.; Poovarodom, P.; Chaijareenont, P.; Rungsiyakull, P. Effect of Customized and Prefabricated Healing Abutments on Peri-Implant Soft Tissue and Bone in Immediate Implant Sites: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 886. [Google Scholar] [CrossRef] [PubMed]
- Desch, A.; Freifrau von Maltzahn, N.; Stumpp, N.; Dalton, M.; Yang, I.; Stiesch, M. Biofilm formation on zirconia and titanium over time-An in vivo model study. Clin. Oral Implant. Res. 2020, 31, 865–880. [Google Scholar] [CrossRef] [PubMed]
- Zeller, B.; Stöckli, S.; Zaugg, L.K.; Astasov-Frauenhoffer, M.; Hauser-Gerspach, I.; Waltimo, T.; Zitzmann, N.U. Biofilm formation on metal alloys, zirconia and polyetherketoneketone as implant materials in vivo. Clin. Oral Implant. Res. 2020, 31, 1078–1086. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, H.; Kern, J.S.; Kern, T.; Lautensack, J.; Conrads, G.; Wolfart, S. Early and mature biofilm on four different dental implant materials: An in vivo human study. Clin. Oral Implant. Res. 2020, 31, 1094–1104. [Google Scholar] [CrossRef] [PubMed]
- Del Rey, Y.C.; Parize, H.; Pedrazzi, V.; Cândido dos Reis, A.; do Nascimento, C. Clinical and in situ oral biofilm formation on dental implant abutment materials: A systematic review. Int. J. Oral Maxillofac. Implant. 2022, 37, 639–652. [Google Scholar] [CrossRef] [PubMed]
- Göthberg, C.; Gröndahl, K.; Omar, O.; Thomsen, P.; Slotte, C. Bone and soft tissue outcomes, risk factors, and complications of implant-supported prostheses: 5-Years RCT with different abutment types and loading protocols. Clin. Implant. Dent. Relat. Res. 2018, 20, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Wennerberg, A.; Sennerby, L.; Kultje, C.; Lekholm, U. Some soft tissue characteristics at implant abutments with different surface topography. A study in humans. J. Clin. Periodontol. 2003, 30, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Brunette, D.M.; Chehroudi, B. The effects of the surface topography of micromachined titanium substrata on cell behavior in vitro and in vivo. J. Biomech. Eng. 1999, 121, 49–57. [Google Scholar] [CrossRef]
- Weiner, S.; Simon, J.; Ehrenberg, D.S.; Zweig, B.; Ricci, J.L. The effects of laser microtextured collars upon crestal bone levels of dental implants. Implant. Dent. 2008, 17, 217–228. [Google Scholar] [CrossRef]
- Nevins, M.; Kim, D.M.; Jun, S.H.; Guze, K.; Schupbach, P.; Nevins, M.L. Histologic evidence of a connective tissue attachment to laser microgrooved abutments: A canine study. Int. J. Periodontics Restor. Dent. 2010, 30, 245–255. [Google Scholar]
- Shin, S.Y.; Han, D.H. Influence of a microgrooved collar design on soft and hard tissue healing of immediate implantation in fresh extraction sites in dogs. Clin. Oral Implant. Res. 2010, 21, 804–814. [Google Scholar] [CrossRef] [PubMed]
- Nevins, M.; Camelo, M.; Nevins, M.L.; Schupbach, P.; Kim, D.M. Reattachment of connective tissue fibers to a laser-microgrooved abutment surface. Int. J. Periodontics Restor. Dent. 2012, 32, e131–e134. [Google Scholar]
- Lee, H.J.; Lee, J.; Lee, J.T.; Hong, J.S.; Lim, B.S.; Park, H.J.; Kim, Y.K.; Kim, T.I. Microgrooves on titanium surface affect peri-implant cell adhesion and soft tissue sealing; an in vitro and in vivo study. J. Periodontal Implant. Sci. 2015, 45, 120–126. [Google Scholar] [CrossRef]
- Ketabi, M.; Deporter, D. The effects of laser microgrooves on hard and soft tissue attachment to implant collar surfaces: A literature review and interpretation. Int. J. Periodontics Restor. Dent. 2013, 33, e145–e152. [Google Scholar] [CrossRef]
- Geurs, N.C.; Geisinger, M.L.; Vassilopoulos, P.J.; O’Neal, S.J.; Haigh, S.J.; Reddy, M.S. Optimizing Connective Tissue Integration on Laser-Ablated Implant Abutments. Clin. Adv. Periodontics 2016, 6, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Ahamed, A.S.; Prakash, P.S.G.; Crena, J.; Victor, D.J.; Subramanian, S.; Appukuttan, D. The influence of laser-microgrooved implant and abutment surfaces on mean crestal bone levels and peri-implant soft tissue healing: A 3-year longitudinal randomized controlled clinical trial. Int. J. Implant. Dent. 2021, 7, 102. [Google Scholar] [CrossRef]
- blueSKY—The Bone Level Implant. Available online: https://www.bredent-implants.com/ (accessed on 29 May 2024).
- hyperDENT. Available online: https://www.follow-me-tech.com/hyperdent/ (accessed on 29 May 2024).
- Paragon. Available online: https://landings.paragon.tools/paragon_tools/ (accessed on 29 May 2024).
- Müller, F.; Al-Nawas, B.; Storelli, S.; Quirynen, M.; Hicklin, S.; Castro-Laza, J.; Bassetti, R.; Schimmel, M.; Roxolid Study Group. Small-diameter titanium grade IV and titanium-zirconium implants in edentulous mandibles: Five-year results from a double-blind, randomized controlled trial. BMC Oral Health 2015, 15, 123. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.H.; Kim, H.M.; Byun, J.H.; Kim, U.K.; Sung, I.Y.; Cho, Y.C.; Park, B.W. Stability of simultaneously placed dental implants with autologous bone grafts harvested from the iliac crest or intraoral jaw bone. BMC Oral Health 2015, 15, 172. [Google Scholar] [CrossRef]
- Degidi, M.; Artese, L.; Piattelli, A.; Scarano, A.; Shibli, J.A.; Piccirilli, M.; Perrotti, V.; Iezzi, G. Histological and immunohistochemical evaluation of the peri-implant soft tissues around machined and acid-etched titanium healing abutments: A prospective randomised study. Clin. Oral Investig. 2012, 16, 857–866. [Google Scholar] [CrossRef]
- Fröjd, V.; Linderbäck, P.; Wennerberg, A.; Chávez de Paz, L.; Svensäter, G.; Davies, J.R. Effect of nanoporous TiO2 coating and anodized Ca2+ modification of titanium surfaces on earlymicrobial biofilm formation. BMC Oral Health 2011, 11, 8. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, I.; Zitzmann, N.U.; Berglundh, T.; Linder, E.; Wennerberg, A.; Lindhe, J. The mucosal attachment to titanium implants with different surface characteristics: An experimental study in dogs. J. Clin. Periodontol. 2002, 29, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Kloss, F.R.; Steinmüller-Nethl, D.; Stigler, R.G.; Ennemoser, T.; Rasse, M.; Hächl, O. In vivo investigation on connective tissue healing to polished surfaces with different surface wettability. Clin. Oral Implant. Res. 2011, 22, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Gui, N.; Xu, W.; Myers, D.E.; Shukla, R.; Tang, H.P.; Qian, M. The effect of ordered and partially ordered surface topography on bone cell responses: A review. Biomater. Sci. 2018, 6, 250–264. [Google Scholar] [CrossRef] [PubMed]
- Rupp, F.; Liang, L.; Geis-Gerstorfer, J.; Scheideler, L.; Hüttig, F. Surface characteristics of dental implants: A review. Dent. Mater. 2018, 34, 40–57. [Google Scholar] [CrossRef] [PubMed]
- Rompen, E.; Domken, O.; Degidi, M.; Pontes, A.E.; Piattelli, A. The effect of material characteristics, of surface topography and of implants components and connections on soft tissue integration: A literature review. Clin. Oral. Implant. Res. 2006, 17, 55–67. [Google Scholar] [CrossRef] [PubMed]
- Chai, W.L.; Moharamzadeh, K.; Brook, I.M.; Van Noort, R. A review of histomorphometric analysis techniques for assessing implant-soft tissue interface. Biotech. Histochem. 2011, 86, 242–254. [Google Scholar] [CrossRef]
- Polishetty, A.; Goldberg, M.; Littlefair, G.; Puttaraju, M.; Patil, P.; Kalra, A. A Preliminary Assessment of Machinability of Titanium Alloy Ti 6AL 4V During thin Wall Machining Using Trochoidal Milling. Procedia Eng. 2014, 97, 357–364. [Google Scholar] [CrossRef]
- CleanImplant. Available online: https://www.cleanimplant.com/ (accessed on 29 May 2024).
- Albrektsson, T.; Canullo, L.; Cochran, D.; De Bruyn, H. “Peri-Implantitis”: A Complication of a Foreign Body or a Man-Made “Disease”. Facts and Fiction. Clin. Implant. Dent. Relat. Res. 2016, 18, 840–849. [Google Scholar] [CrossRef]






| Abutments | BS-YD1 | BS-YD2 | BS-YD3 | BS-YD4 |
|---|---|---|---|---|
| Stage 1 | ||||
| Spherical milling tool diameter (mm) | 1.5 | 1.5 | 1.5 | 1.5 |
| Stepover (mm) | 0.1 | 0.08 | 0.045 | 0.045 |
| Feed Rate (mm/min) | 1200 | 1200 | 600 | 600 |
| Resolution | low | low | low | high |
| Stage 2 | ||||
| Spherical milling tool diameter (mm) | 1 | 1 | 1 | 1 |
| Stepover (mm) | 0.08 | 0.045 | 0.045 | 0.045 |
| Feed Rate (mm/min) | 1200 | 1200 | 600 | 600 |
| Resolution | low | low | low | high |
| Parameter | BS-Exso (1) | BS-NM (2) | BS-YD1 (3) | BS-YD2 (4) | BS-YD3 (5) | BS-YD4 (6) | p * | Pairwise Comparisons ** |
|---|---|---|---|---|---|---|---|---|
| Total no of cavities | 53.00 | 56.00 | 39.00 | 39.00 | 57.00 | 57.00 | 0.017 | 3–6 |
| Min size | 20.33 | 22.51 | 53.75 | 24.87 | 23.62 | 22.56 | 0.003 | 1–3, 3–6 |
| Max size | 127.33 | 195.50 | 103.27 | 169.43 | 159.74 | 153.72 | 0.022 | 2–3 |
| Length variation | 88% | 88% | 46% | 87% | 86% | 85% | 0.004 | 1–3, 2–3 |
| Mean no of cavities | 13.25 | 14.00 | 9.75 | 9.75 | 14.25 | 14.25 | 0.017 | - |
| Mean Min size | 23.03 | 26.46 | 69.56 | 37.55 | 27.92 | 25.16 | <0.0005 | 1–3, 1–4, 3–6 |
| Mean Max size | 105.75 | 121.71 | 92.89 | 126.26 | 131.03 | 104.07 | 0.020 | - |
| Min variance | 9.87 | 20.57 | 159.99 | 46.76 | 15.72 | 8.30 | 0.021 | 1–3, 3–6 |
| Max variance | 270.93 | 1679.51 | 199.13 | 628.19 | 936.72 | 951.90 | 0.071 | - |
| Parameter | BS-Exso (1) | BS-NM (2) | BS-YD2 (4) | BS-YD3 (5) | BS-YD4 (6) | p * | Pairwise Comparisons ** |
|---|---|---|---|---|---|---|---|
| Total no of cavities | 53.00 | 56.00 | 39.00 | 57.00 | 57.00 | 0.146 | - |
| Min size | 20.33 | 22.51 | 24.87 | 23.62 | 22.56 | 0.066 | - |
| Max size | 127.33 | 195.50 | 169.43 | 159.74 | 153.72 | 0.057 | - |
| Length variation | 88% | 88% | 87% | 86% | 85% | 0.139 | - |
| Mean no of cavities | 13.25 | 14.00 | 9.75 | 14.25 | 14.25 | 0.146 | - |
| Mean Min size | 23.03 | 26.46 | 37.55 | 27.92 | 25.16 | 0.001 | 1–4, 4–6 |
| Mean Max size | 105.75 | 121.71 | 126.26 | 131.03 | 104.07 | 0.020 | - |
| Min variance | 9.87 | 20.57 | 46.76 | 15.72 | 8.30 | 0.518 | - |
| Max variance | 270.93 | 1679.51 | 628.19 | 936.72 | 951.90 | 0.114 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Târtea, D.A.; Manolea, H.O.; Ionescu, M.; Gîngu, O.; Amărăscu, M.O.; Popescu, A.M.; Mercuţ, V.; Popescu, S.M. A Microscopy Evaluation of Emergence Profile Surfaces of Dental Custom CAD-CAM Implant Abutments and Dental Implant Stock Abutments. J. Pers. Med. 2024, 14, 699. https://doi.org/10.3390/jpm14070699
Târtea DA, Manolea HO, Ionescu M, Gîngu O, Amărăscu MO, Popescu AM, Mercuţ V, Popescu SM. A Microscopy Evaluation of Emergence Profile Surfaces of Dental Custom CAD-CAM Implant Abutments and Dental Implant Stock Abutments. Journal of Personalized Medicine. 2024; 14(7):699. https://doi.org/10.3390/jpm14070699
Chicago/Turabian StyleTârtea, Daniel Adrian, Horia Octavian Manolea, Mihaela Ionescu, Oana Gîngu, Marina Olimpia Amărăscu, Adrian Marcel Popescu, Veronica Mercuţ, and Sanda Mihaela Popescu. 2024. "A Microscopy Evaluation of Emergence Profile Surfaces of Dental Custom CAD-CAM Implant Abutments and Dental Implant Stock Abutments" Journal of Personalized Medicine 14, no. 7: 699. https://doi.org/10.3390/jpm14070699
APA StyleTârtea, D. A., Manolea, H. O., Ionescu, M., Gîngu, O., Amărăscu, M. O., Popescu, A. M., Mercuţ, V., & Popescu, S. M. (2024). A Microscopy Evaluation of Emergence Profile Surfaces of Dental Custom CAD-CAM Implant Abutments and Dental Implant Stock Abutments. Journal of Personalized Medicine, 14(7), 699. https://doi.org/10.3390/jpm14070699








