Results of Tendon Transfers in Radial Nerve Palsies: A New Evaluation Protocol
Abstract
1. Introduction
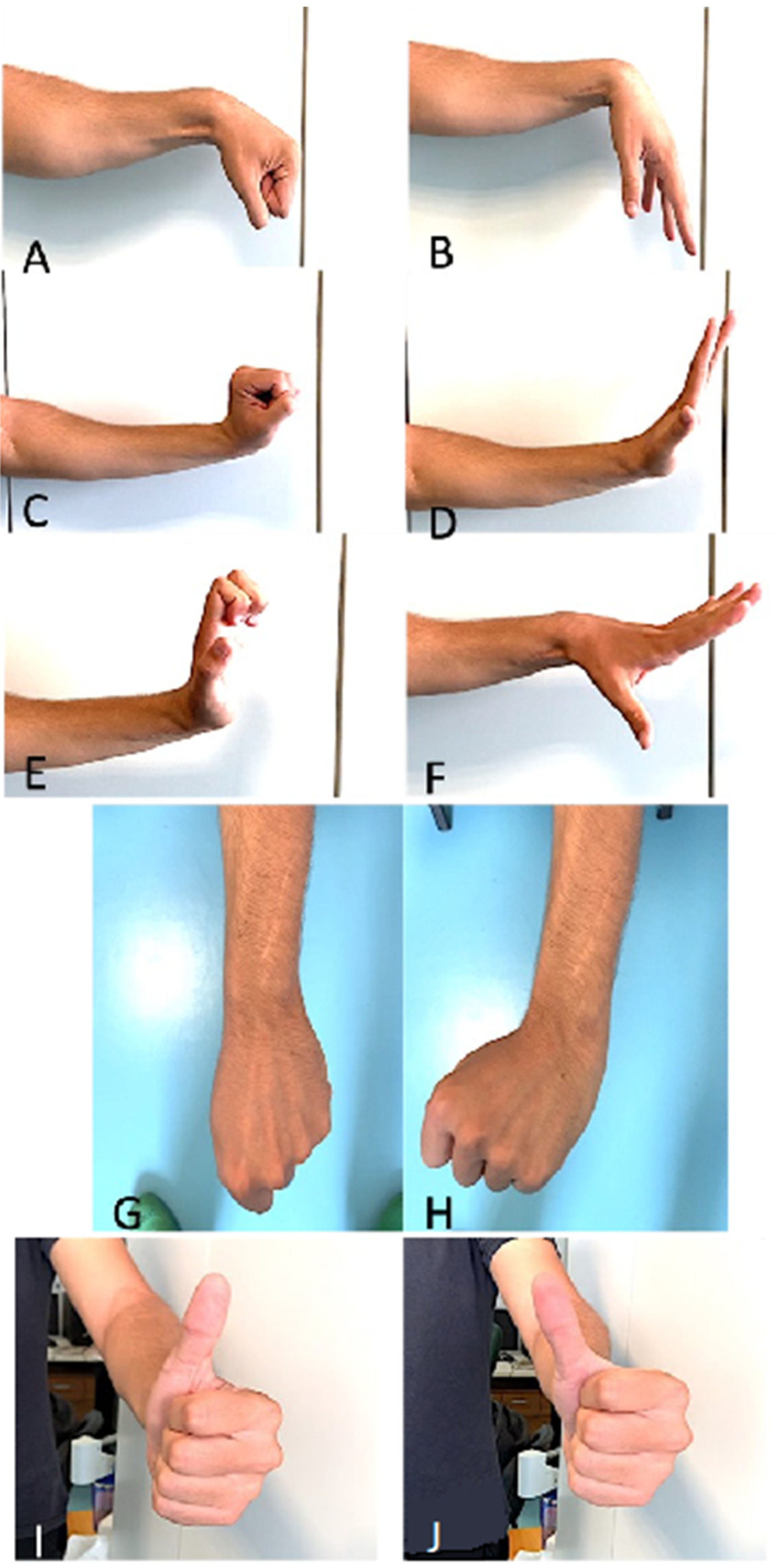
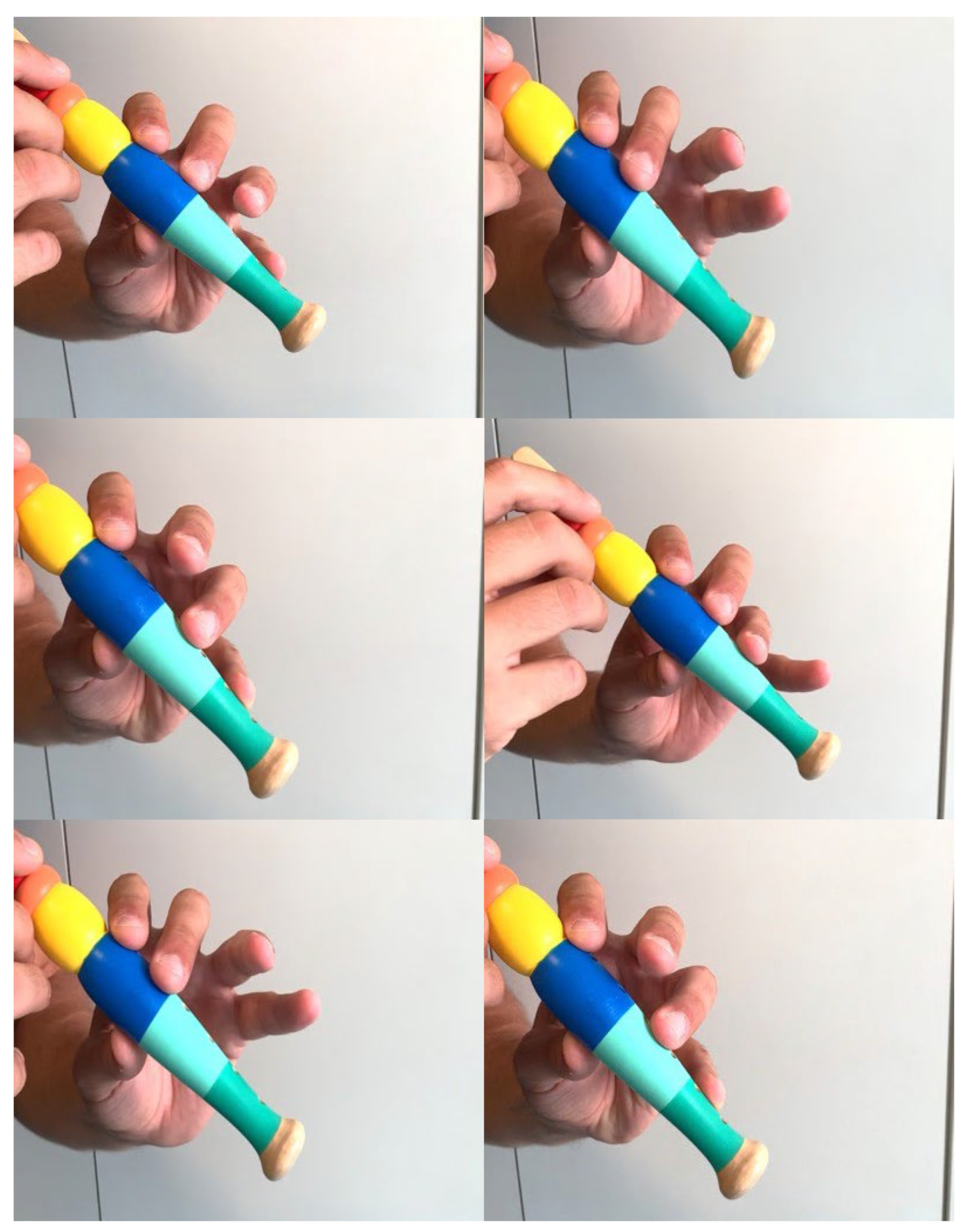
2. Materials and Methods
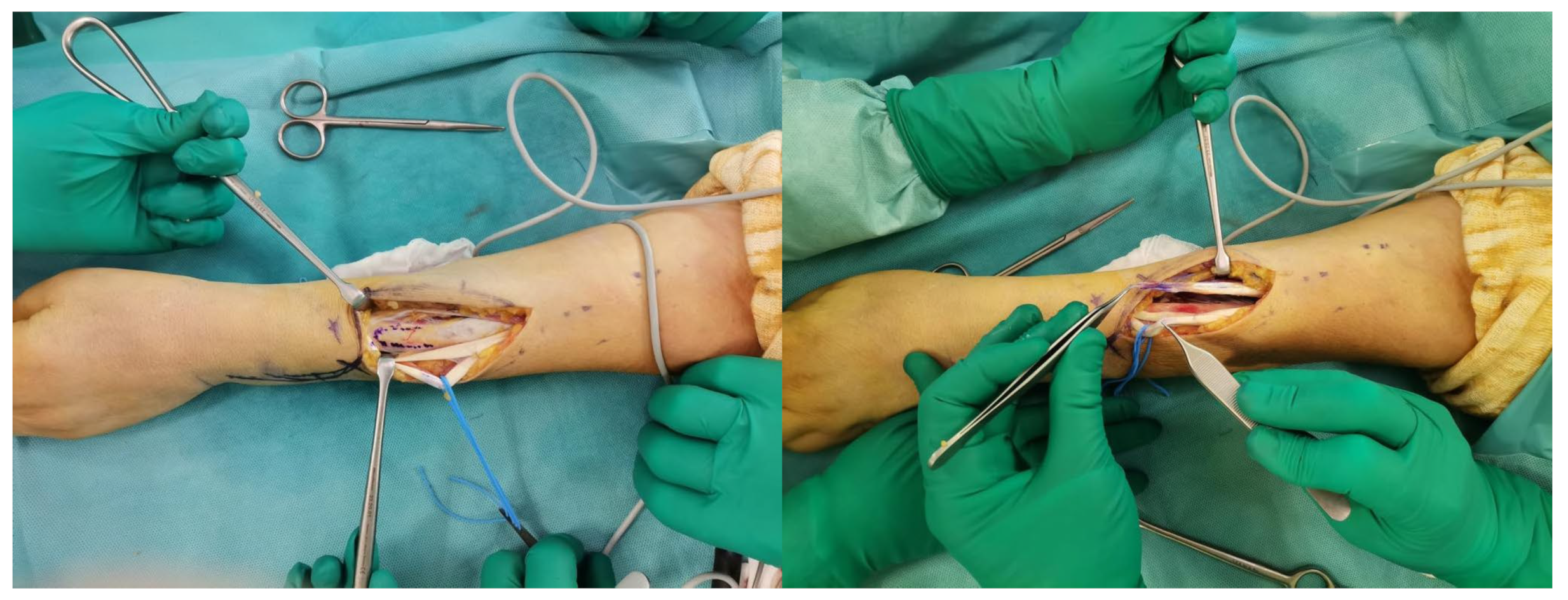
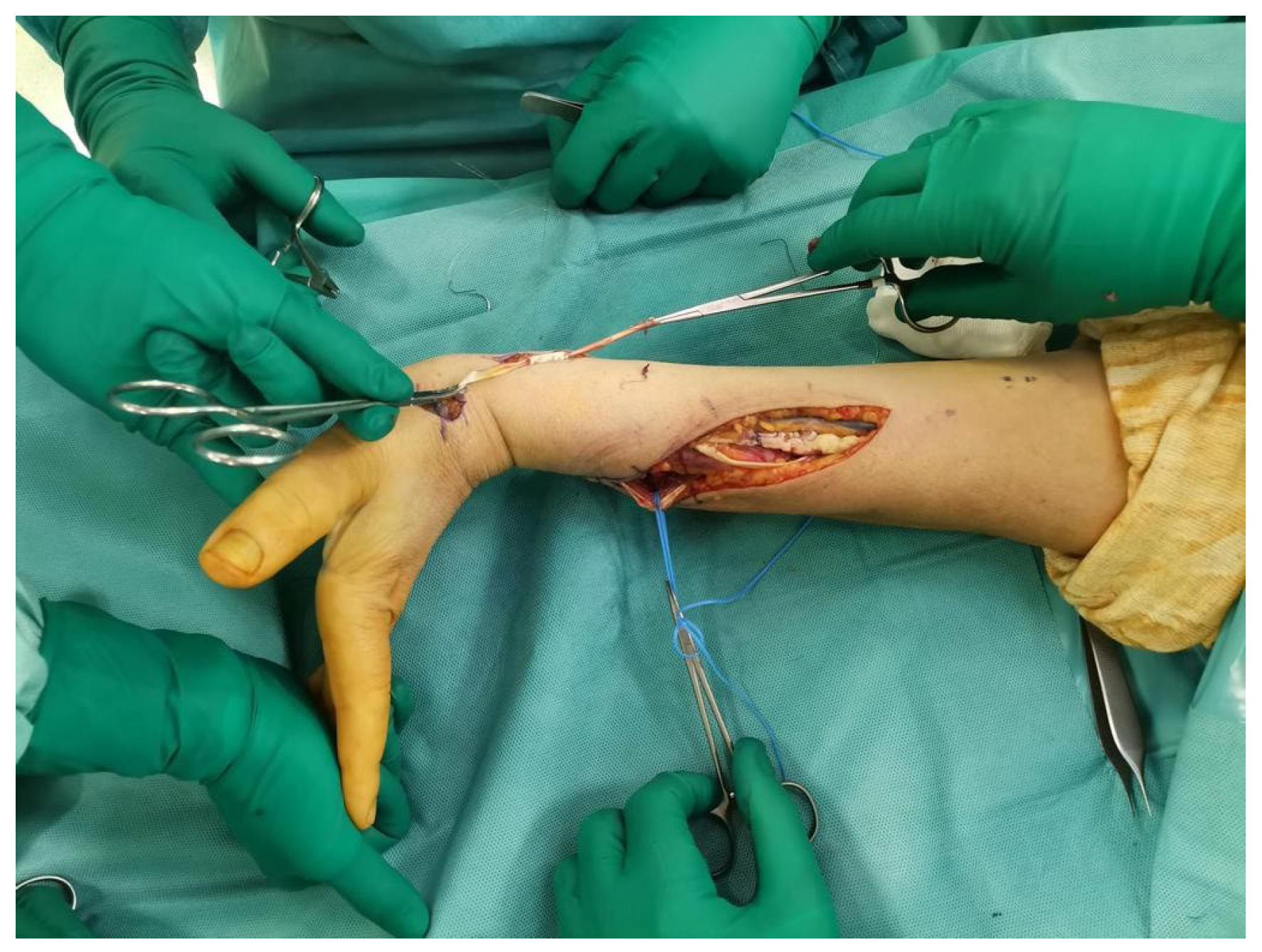
Surgical Technique
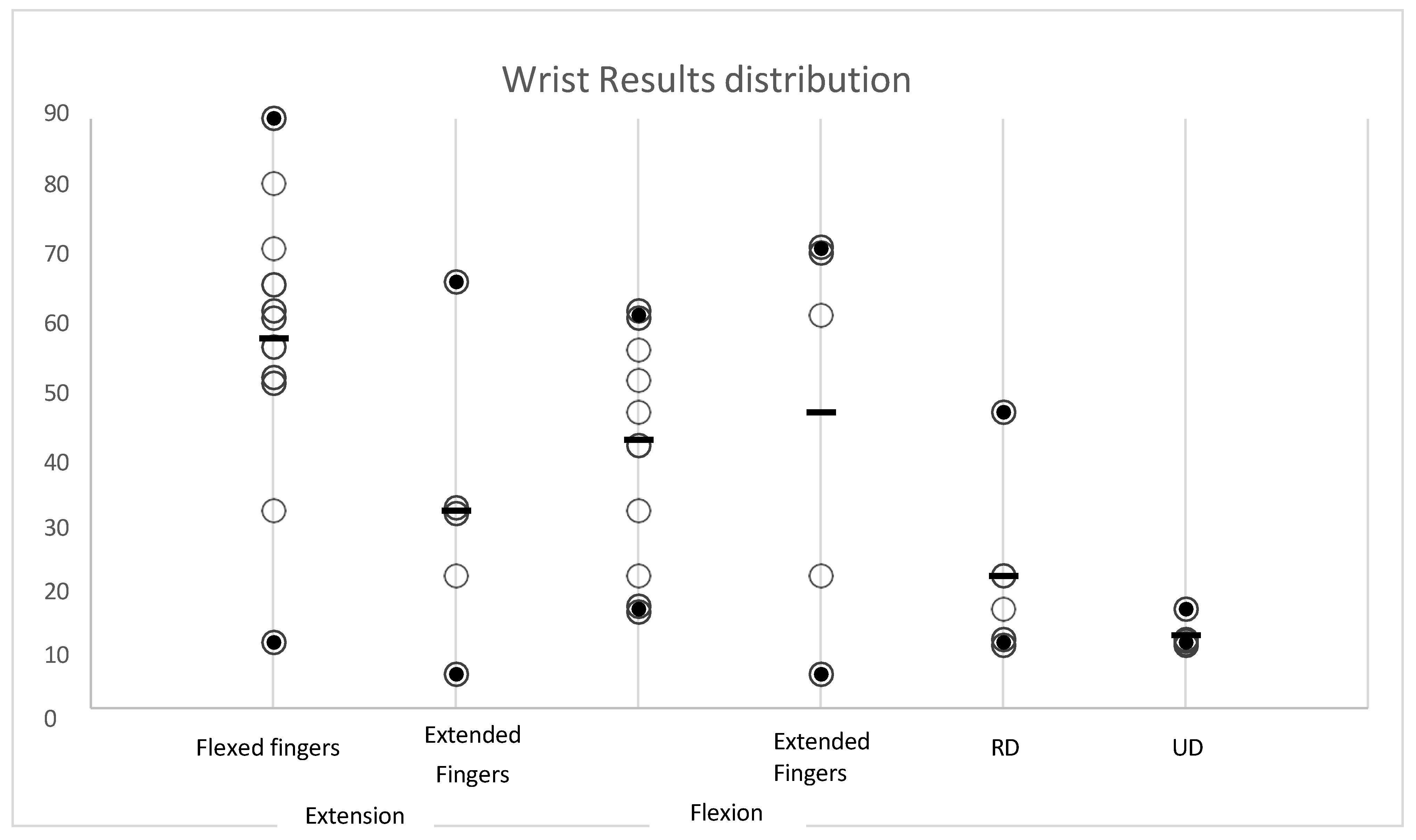
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ljungquist, K.L.; Martineau, P.; Allan, C. Radial nerve injuries. J. Hand Surg. Am. 2015, 40, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Mai, T.T.; Nguyen, V.Q.; Nguyễn, P.D. Treatment of irrecoverable radial nerve palsy using the modified merle d‘aubigné tendon transfer method. Orthop. Rev. 2024, 16, 94033. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheah, A.E.J.; Etcheson, J.; Yao, J. Radial Nerve Tendon Transfers. Hand Clin. 2016, 32, 323–338. [Google Scholar] [CrossRef]
- Kozin, S.H. Tendon transfers for radial and median nerve palsies. J. Hand Ther. 2005, 18, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Ratner, J.A.; Peljovich, A.; Kozin, S.H. Update on tendon transfers for peripheral nerve injuries. J. Hand Surg. Am. 2010, 35, 1371–1381. [Google Scholar] [CrossRef]
- Compton, J.; Owens, J.; Day, M.; Caldwell, L. Systematic Review of Tendon Transfer Versus Nerve Transfer for the Restoration of Wrist Extension in Isolated Traumatic Radial Nerve Palsy. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e001. [Google Scholar] [CrossRef]
- Moussavi, A.A.; Saied, A.; Karbalaeikhani, A. Outcome of tendon transfer for radial nerve paralysis: Comparison of three methods. Indian J. Orthop. 2011, 45, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Riordan, D.C. Tendon transfers in hand surgery. J. Hand Surg. Am. 1983, 8, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Colantoni Woodside, J.; Bindra, R.R. Rerouting extensor pollicis longus tendon transfer. J. Hand Surg. Am. 2015, 40, 822–825. [Google Scholar] [CrossRef]
- Pulvertaft, R.G. Suture materials and tendon junctures. Am. J. Surg. 1965, 109, 346–352. [Google Scholar] [CrossRef]
- Enye, L.A.; Saalu, L.C.; Osinubi, A.A. The Prevalence of Agenesis of Palmaris Longus Muscle amongst Students in Two Lagos-Based Medical Schools. Int. J. Morphol. 2010, 28, 849–854. [Google Scholar] [CrossRef]
- Sebastin, S.J.; Puhaindran, M.E.; Lim, A.Y.T.; Lim, I.J.; Bee, W.H. The prevalence of absence of the palmaris longus—A study in a Chinese population and a review of the literature. J. Hand Surg. Am. 2005, 30, 525–527. [Google Scholar] [CrossRef] [PubMed]
- Shao, Y.C.; Harwood, P.; Grotz, M.R.W. nUpper limb Radial nerve palsy associated with fractures of the shaft of the humerus A Systematic Review. J. Bone Jt. Surg. Br. Vol. 2005, 87, 1647–1652. [Google Scholar] [CrossRef] [PubMed]
- Schwab, T.R.; Stillhard, P.F.; Schibli, S.; Furrer, M.; Sommer, C. Radial nerve palsy in humeral shaft fractures with internal fixation: Analysis of management and outcome. Eur. J. Trauma Emerg. Surg. 2018, 44, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Chang, G.; Ilyas, A.M. Radial Nerve Palsy After Humeral Shaft Fractures: The Case for Early Exploration and a New Classification to Guide Treatment and Prognosis. Hand Clin. 2018, 34, 105–112. [Google Scholar] [CrossRef]
- Korompilias, A.V.; Lykissas, M.G.; Kostas-Agnantis, I.P.; Vekris, M.D.; Soucacos, P.N.; Beris, A.E. Approach to radial nerve palsy caused by humerus shaft fracture: Is primary exploration necessary? Injury 2013, 44, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Węgiel, A.; Karauda, P.; Zielinska, N.; Tubbs, R.S.; Olewnik, Ł. Radial nerve compression: Anatomical perspective and clinical consequences. Neurosurg. Rev. 2023, 46, 53. [Google Scholar] [CrossRef] [PubMed]
- Karabeg, R. New Functional Evaluation Scheme—Modality of the Results of Forearm Tendon Transfers Evaluation in Cases of Irreparable Radial Nerve Injury. Med. Arch. 2020, 74, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Karabeg, R. Assessment of the Forearm Tendon Transfer with Irreparable Radial Nerve Injuries Caused by War Projectiles. Med. Arch. 2019, 73, 415–420. [Google Scholar] [CrossRef]
- Sunderland, S. A classification of peripheral nerve injuries producing loss of function. Brain 1951, 74, 491–516. [Google Scholar] [CrossRef]
- Ropars, M.; Dréano, T.; Siret, P.; Belot, N.; Langlais, F. Long-term results of tendon transfers in radial and posterior interosseous nerve paralysis. J. Hand Surg. Br. 2006, 31, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Richards, R.R. Tendon transfers for failed nerve reconstruction. Clin. Plast. Surg. 2003, 30, 223–245. [Google Scholar] [CrossRef] [PubMed]
- Sammer, D.; Chung, K. Tendon Transfers Part I: Principles of Transfer and Transfers for Radial Nerve Palsy. Plast Reconstr. Surg. 2009, 123, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.F.; Machado, G.R. Tendon Transfers for Radial, Median, and Ulnar Nerve Injuries: Current Surgical Techniques. Clin Plast Surg. 2011, 38, 621–642. [Google Scholar] [CrossRef] [PubMed]
- Brand, P.W.; Beach, R.B.; Thompson, D.E. Relative tension and potential excursion of muscles in the forearm and hand. J. Hand Surg. Am. 1981, 6, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Burkhalter, W.E. Early tendon transfer in upper extremity peripheral nerve injury. Clin. Orthop. 1974, 104, 68–79. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhou, W.; Zhou, Q.; Yin, Y. Comparison of nerve versus tendon transfer for radial nerve palsy. Clin Neurol Neurosurg. 2024, 236, 108077. [Google Scholar] [CrossRef] [PubMed]
- Al-Qattan, M.M. Tendon transfer for radial nerve palsy: A single tendon to restore finger extension as well as thumb extension/radial abduction. J. Hand Surg. Eur. Vol. 2012, 37, 855–862. [Google Scholar] [CrossRef]
- Altintas, A.A.; Altintas, M.A.; Gazyakan, E.; Gohla, T.; Germann, G.; Sauerbier, M. Long-term results and the Disabilities of the Arm, Shoulder, and Hand score analysis after modified Brooks and D’Aubigne tendon transfer for radial nerve palsy. J. Hand Surg. Am. 2009, 34, 474–478. [Google Scholar] [CrossRef]
- Patterson, J.M.M.; Russo, S.A.; El-Haj, M.; Novak, C.B.; Mackinnon, S.E. Radial Nerve Palsy: Nerve Transfer Versus Tendon Transfer to Restore Function. Hand 2022, 17, 1082–1089. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Agrawal, N.K.; Gupta, M.K. Comprehensive Analysis of Zachary’s Modification of Jones Tendon Transfer in Isolated High Radial Nerve Palsy. J. Clin. Diagn. Res. 2021, 15, PC20–PC25. [Google Scholar] [CrossRef]
- Franke, F. Über die operative Behandlung der Radialisla€hmung nebst Bemer- kungen über die Sehnenüberpflanzungen bei spastischen Paresen. Arch. Klin. Chir. 1898, 57, 763. [Google Scholar]
- Lucich, E.A.; Fahrenkopf, M.P.; Kelpin, J.P.; Hall, T.C.; Do, V.H. Extensor Tendon Transfers for Radial Nerve Palsy Secondary to Humeral Shaft Fracture. Eplasty 2018, 18, ic18. [Google Scholar] [PubMed] [PubMed Central]
- Jain, N.S.; Barr, M.L.; Kim, D.; Jones, N.F. Tendon Transfers, Nerve Grafts, and Nerve Transfers for Isolated Radial Nerve Palsy: A Systematic Review and Analysis. Hand 2023, 19, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Bincaz, L.E.; Cherifi, H.; Alnot, J.Y. Les transferts palliatifs de réanimation de l’extension du poignet et des doigts. À propos de 14 transferts pour paralysie radiale et dix transferts pour lésion plexique. Chir. Main. 2002, 21, 13–22. [Google Scholar] [CrossRef]
- Zachary, R.B. Tendon transplantation for radial paralysis. Br. J. Surg. 1946, 33, 358–364. [Google Scholar] [CrossRef]
- Tajima, T. Tendon transfers in radial nerve palsy. In Tendon Surgery of the Hand; Hunter, J.M., Schneider, L.A., Mackin, E.J., Eds.; CV Mosby: Maryland Heights, MO, USA, 1987; pp. 432–438. [Google Scholar]



| Degrees | Value | Excellent | Good | Satisfactory | Poor | |
|---|---|---|---|---|---|---|
| WRIST (0°–90°) | ||||||
| Extension | Flexed fingers | ≥60° | 30–60° | 0–30° | <0° | |
| Extended fingers | ≥30° | 15–30° | 0–15° | <0° | ||
| Flexion | Flexed fingers | ≥30° | 15–30° | 0–15° | <0° | |
| Extended fingers | ≥60° | 30–60° | 0–30° | <0° | ||
| Radial Deviation | ≥20° | 10–20° | 0°–10° | Inability of DR | ||
| Ulnar Deviation | ≥20° | 10–20° | 0°–10° | Inability of DU | ||
| MP (90°–180°) | ||||||
| Extension | Flexed Wrist | ≥170° | 150–170° | 130–150° | <130° | |
| Neutral Wrist | ≥170° | 150–170° | 130–150° | <130° | ||
| Thumb (0°–90°) | ||||||
| Extension | TM | ≥70° | 45–70° | 30–45° | <30° | |
| MP | ≥70° | 45–70° | 30–45° | <30° | ||
| IP | ≥70° | 45–70° | 30–45° | <30° | ||
| Abduction | ≥70° | 45–70° | 30–45° | <30° | ||
| Flexion (Kapandji) | 9–10 | 8 | 7 | <7 | ||
| Test | Value | Range | ||||
| Flute test (Fingers Independence) | Yes–No | |||||
| Degree of personal satisfaction | 0–10 | |||||
| Time to back to work | Months | |||||
| Grip strength | Jamar (percentage compared to the healthy side) | |||||
| Dash score | (0–100) https://orthotoolkit.com/dash/ (accessed on 20 April 2024). | |||||
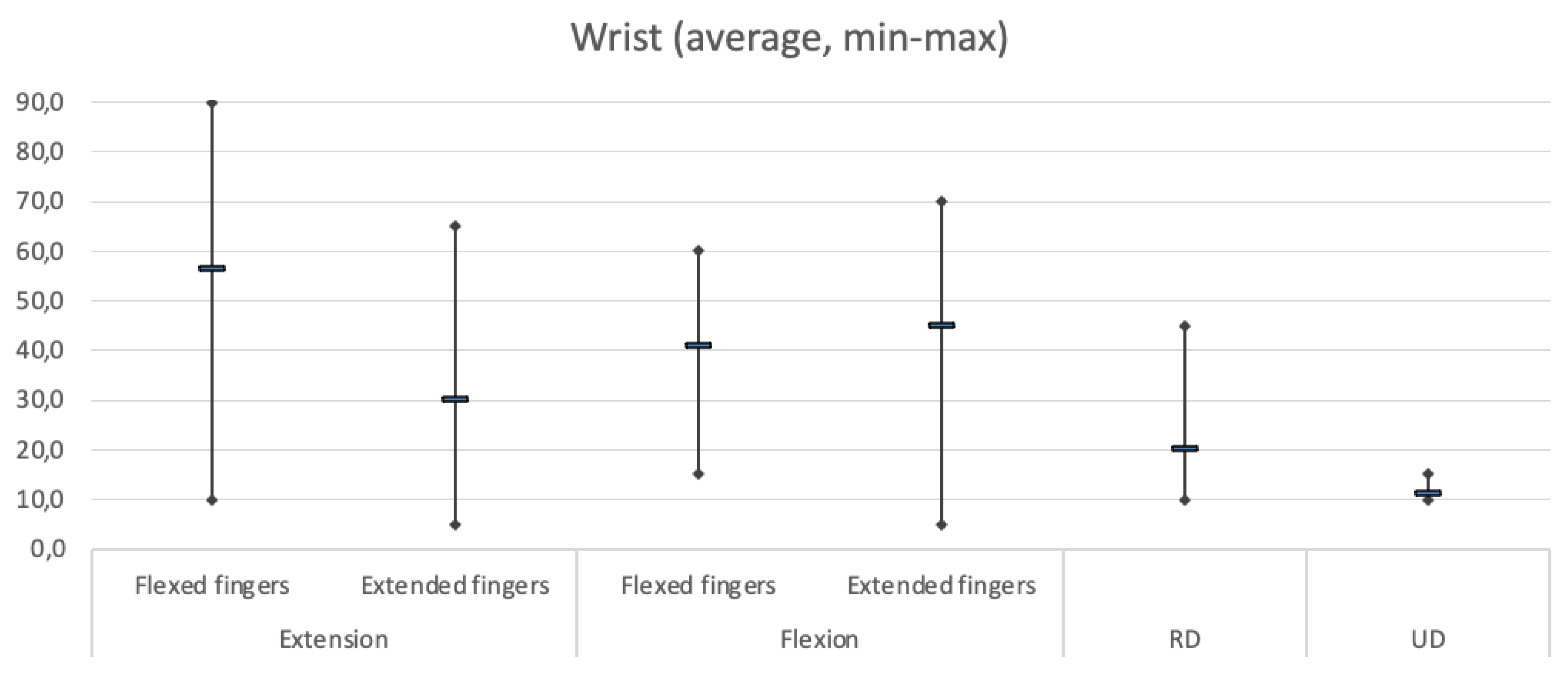
| Degrees | Average | Results | Std Dev | ||
|---|---|---|---|---|---|
| WRIST (0°–90°) | Min | Max | |||
| Extension | Flexed fingers | 56.3 | 10.0 | 90.0 | 22.1 |
| Extended fingers | 30.0 | 5.0 | 65.0 | 22.1 | |
| Flexion | Flexed fingers | 40.9 | 15.0 | 60.0 | 18.1 |
| Extended fingers | 45.0 | 5.0 | 70.0 | 30.4 | |
| Radial Deviation | 20.0 | 10.0 | 45.0 | 14.6 | |
| Ulnar Deviation | 11.0 | 10.0 | 15.0 | 2.2 | |
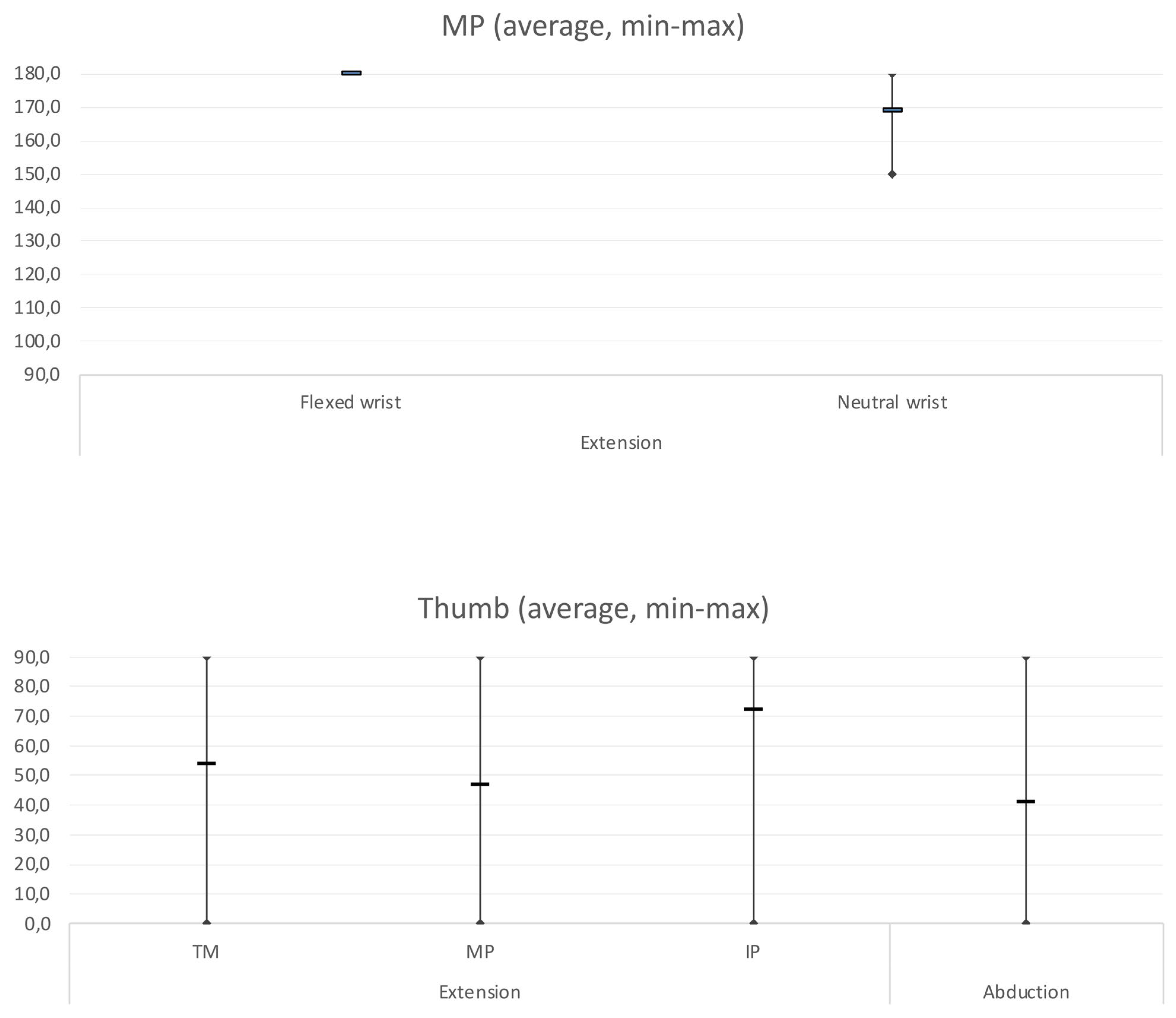
| MP (90°–180°) | |||||
| Extension | Flexed Wrist | 180.0 | 180.0 | 180.0 | 0.0 |
| Neutral Wrist | 169.1 | 150.0 | 180.0 | 11.6 | |
| Thumb (0°–90°) | |||||
| Extension | TM | 54.0 | 0.0 | 90.0 | 37.8 |
| MP | 47.0 | 0.0 | 90.0 | 42.7 | |
| IP | 72.0 | 0.0 | 90.0 | 37.9 | |
| Abduction | 41.0 | 0.0 | 90.0 | 32.5 | |
| Flexion (Kapandji) | 8.7 | 8.0 | 10.0 | 0.8 | |
| Test | |||||
| Degree of personal satisfaction | 9.4 | 9.0 | 10.0 | 0.5 | |
| Time to back to work | 7.3 | 4.0 | 12.0 | 4.2 | |
| Grip strength | 69.4% | 30.0% | 100.0% | 0.2 | |
| Dash score | 26.2 | 1.7 | 60.7 | 21.3 | |
| Degrees | Excellent | Good | Satisfactory | Poor | |
|---|---|---|---|---|---|
| WRIST (0°–90°) | |||||
| Extension | Flexed fingers | 54.5% | 36.4% | 9.1% | 0.0% |
| Extended fingers | 60.0% | 20.0% | 20.0% | 0.0% | |
| Flexion | Flexed fingers | 72.7% | 27.3% | 0.0% | 0.0% |
| Extended fingers | 60.0% | 0.0% | 40.0% | 0.0% | |
| Radial Deviation | 40.0% | 60.0% | 0.0% | 0.0% | |
| Ulnar Deviation | 0.0% | 100.0% | 0.0% | 0.0% | |
| MP (90°–180°) | |||||
| Extension | Flexed Wrist | 100.0% | 0.0% | 0.0% | 0.0% |
| Neutral Wrist | 54.5% | 45.5% | 0.0% | 0.0% | |
| Thumb (0°–90°) | |||||
| Extension | TM | 60.0% | 0.0% | 20.0% | 20.0% |
| MP | 40.0% | 20.0% | 0.0% | 40.0% | |
| IP | 80.0% | 0.0% | 0.0% | 20.0% | |
| Abduction | 20.0% | 20.0% | 40.0% | 20.0% | |
| Flexion (Kapandji) | 54.5% | 45.5% | 0.0% | 0.0% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reina, M.; Odella, S.; Magnani, M.; Locatelli, F.; Clemente, A.; Macrì, M.; Tos, P. Results of Tendon Transfers in Radial Nerve Palsies: A New Evaluation Protocol. J. Pers. Med. 2024, 14, 758. https://doi.org/10.3390/jpm14070758
Reina M, Odella S, Magnani M, Locatelli F, Clemente A, Macrì M, Tos P. Results of Tendon Transfers in Radial Nerve Palsies: A New Evaluation Protocol. Journal of Personalized Medicine. 2024; 14(7):758. https://doi.org/10.3390/jpm14070758
Chicago/Turabian StyleReina, Micaela, Simonetta Odella, Mauro Magnani, Francesco Locatelli, Alice Clemente, Martina Macrì, and Pierluigi Tos. 2024. "Results of Tendon Transfers in Radial Nerve Palsies: A New Evaluation Protocol" Journal of Personalized Medicine 14, no. 7: 758. https://doi.org/10.3390/jpm14070758
APA StyleReina, M., Odella, S., Magnani, M., Locatelli, F., Clemente, A., Macrì, M., & Tos, P. (2024). Results of Tendon Transfers in Radial Nerve Palsies: A New Evaluation Protocol. Journal of Personalized Medicine, 14(7), 758. https://doi.org/10.3390/jpm14070758






