The Evidence for Perioperative Anesthetic Techniques in the Prevention of New-Onset or Recurrent Complex Regional Pain Syndrome in Hand Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Scoping Review
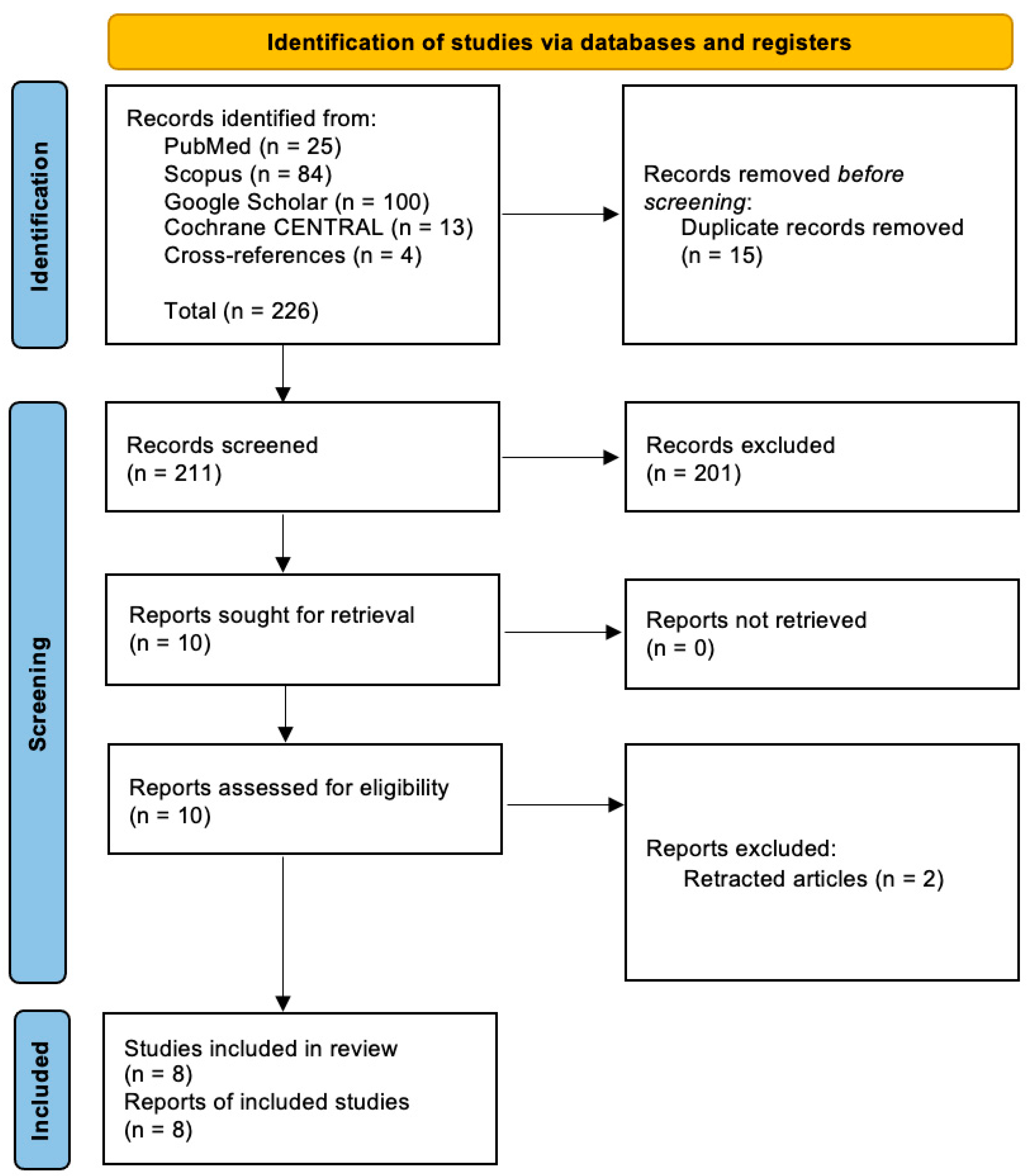
2.2. Literature Search and Selection
2.3. Data Management and Extraction
2.4. Assessment of Studies and Their Quality of Evidence
3. Results
3.1. Included Articles
3.2. Identified Techniques
3.3. Incidence of CRPS Based on Various Anesthetic Techniques
3.4. Risk of Bias Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ratti, C.; Nordio, A.; Resmini, G.; Murena, L. Post-traumatic complex regional pain syndrome: Clinical features and epidemiology. Clin. Cases Min. Bone Metab. 2015, 12, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, M.C.; Cashin, A.G.; Wand, B.M.; Smart, K.M.; Berryman, C.; Marston, L.; Moseley, G.L.; McAuley, J.H.; O’Connell, N.E. Interventions for treating pain and disability in adults with complex regional pain syndrome—An overview of systematic reviews. Cochrane Database Syst. Rev. 2023, 6. [Google Scholar] [CrossRef]
- Saed, A.; Neal-Smith, G.; Fernquest, S.; Bourget-Murray, J.; Wood, A. Management of complex regional pain syndrome in trauma and orthopaedic surgery—A systematic review. Br. Med. Bull. 2023, 146, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Harden, N.R.; Bruehl, S.; Perez, R.; Birklein, F.; Marinus, J.; Maihofner, C.; Lubenow, T.; Buvanendran, A.; Mackey, S.; Graciosa, J.; et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for Complex Regional Pain Syndrome. Pain 2010, 150, 268–274. [Google Scholar] [CrossRef]
- da Costa, V.V.; de Oliveira, S.B.; Fernandes, M.d.C.B.; Saraiva, R.Â. Incidence of Regional Pain Syndrome after Carpal Tunnel Release. Is there a Correlation with the Anesthetic Technique? Braz. J. Anesthesiol. 2011, 61, 425–433. [Google Scholar] [CrossRef]
- Gschwind, C.; Fricker, R.; Lacher, G.; Jung, M. Does Peri-Operative Guanethidine Prevent Reflex Sympathetic Dystrophy? J. Hand Surg. 1995, 20, 773–775. [Google Scholar] [CrossRef]
- Goh, E.L.; Chidambaram, S.; Ma, D. Complex regional pain syndrome: A recent update. Burn. Trauma 2017, 5, 2. [Google Scholar] [CrossRef]
- Ackerman, W.E.; Ahmad, M. Recurrent Postoperative CRPS I in Patients With Abnormal Preoperative Sympathetic Function. J. Hand Surg. 2008, 33, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Rocco, A.G. Comment on: Abnormal contralateral pain responses from an intradermal injection of phenylephrine in a subset of patients with complex regional pain syndrome (CRPS), Mailis-Gagnon and Bennet. Pain 2005, 115, 213–214. [Google Scholar] [CrossRef]
- Seth, I.; Bulloch, G.; Seth, N.; Siu, A.; Clayton, S.; Lower, K.; Roshan, S.; Nara, N. Effect of Perioperative Vitamin C on the Incidence of Complex Regional Pain Syndrome: A Systematic Review and Meta-Analysis. J. Foot Ankle Surg. 2022, 61, 748–754. [Google Scholar] [CrossRef]
- Droog, W.; Walbeehm, E.T.; Konijn, J.B.; Lucas, B.M.J.; Coert, J.H.; Stolker, R.J.; Galvin, E.M. A Systematic Review on Long-Term Postsurgical Pain Outcomes; What Is the Effect of Upper Extremity Regional Anesthesia? Anesth. Analg. 2023, 137, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef] [PubMed]
- Ramos, P.R.; Sakata, R.K.; Ribeiro, H.C.; Bonfanti, A.; Ferraro, L. A prospective, comparative study of the analgesic effect between the WALANT technique and local anesthesia associated with sedation for hand surgery. Acta Cir. Bras. 2023, 38, e384323. [Google Scholar] [CrossRef] [PubMed]
- Far-Riera, A.M.; Perez-Uribarri, C.; Serrano, M.J.E.; González, J.M.R. Impact of WALANT Hand Surgery in a Secondary Care Hospital in Spain. Benefits to the Patient and the Health System. J. Hand Surg. Glob. Online 2023, 5, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Jerome, J.T.J. Wide-awake local anesthesia no tourniquet and dexamethasone (WALANT-D) for modified Camitz opponens plasty in severe carpal tunnel syndrome—A retrospective study of 30 cases. J. Clin. Orthop. Trauma 2023, 43, 102228. [Google Scholar] [CrossRef] [PubMed]
- Jerome, J.T.J. Wide-awake local anesthesia No tourniquet (WALANT) for reconstruction of flexor pollicis longus ruptures following volar plate fixation of distal radius fractures—A Case series. J. Orthop. Rep. 2023, 2, 100162. [Google Scholar] [CrossRef]
- Lichtman, D.M.; Florio, R.L.; Mack, G.R. Carpal tunnel release under local anesthesia: Evaluation of the outpatient procedure. J. Hand Surg. 1979, 4, 544–546. [Google Scholar] [CrossRef]
- Reuben, S.S.; Rosenthal, E.A.; Steinberg, R.B. Surgery on the affected upper extremity of patients with a history of complex regional pain syndrome: A retrospective study of 100 patients. J. Hand Surg. 2000, 25, 1147–1151. [Google Scholar] [CrossRef]
- Katz, M.M.; Hungerford, D.S. Reflex sympathetic dystrophy affecting the knee. J. Bone Jt. Surg. Br. Vol. 1987, 69, 797–803. [Google Scholar] [CrossRef] [PubMed]
All the following statements must be met:
| ||
| No. | Category | Signs/Symptoms |
| 1 | Sensory | Hyperalgesia (to pinprick) and/or allodynia (pain to light touch, deep somatic pressure, or joint movement). |
| 2 | Vasomotor | Temperature asymmetry, skin changes, and/or skin color asymmetry. |
| 3 | Sudomotor/edema | Edema, sweating changes, and/or sweating asymmetry. |
| 4 | Motor/trophic | Decreased range of motion, motor dysfunction (weakness, tremor, dystonia), and/or trophic changes (hair, skin, and nails). |
| Anesthetic Technique | Author(s) | No. of Patients | Follow-Up Period | Procedure(s) | Percentage of Females (%) | Mean Torniquet Time (min) | Phase of Administration | Anesthetic Agent | Incidence of CRPS (%) |
|---|---|---|---|---|---|---|---|---|---|
| New-Onset CRPS | |||||||||
| WALANT | Ramos et al., 2023 [15] | 28 | 1 month | Carpal tunnel release/De Quervain’s tenosynovitis/synovial cyst/finger cyst/trigger finger | 75.0 | NA | Pre-incisional | 9 mL of 1% lidocaine with 1:100,000 adrenaline, made up to 10 mL with 8.4% sodium bicarbonate | Zero |
| Far-Riera et al., 2023 [16] | 150 (prospective study) | 1 month | Carpal tunnel release/trigger finger | 69.0 | NA | 1% lidocaine with 1:100,000 adrenaline | Zero | ||
| 580 (retrospective study) | 2–21 months (mean: 12 months) | Carpal tunnel release/trigger finger | 65.0 | NA | 0.3% (two cases) | ||||
| Jerome, 2023a [17] | 7 | 12–19 months (mean: 16.5 months) | Reconstruction of flexor pollicis longus ruptures following volar plate fixation of distal radius fractures. | 14.3 | NA | 10 mL of 1% lidocaine with 1:100,000 adrenaline | Zero | ||
| WALANT with dexamethasone | Jerome, 2023b [18] | 27 | 10–14 months (mean: 12.5 months) | Carmitz opponensplasty for carpal tunnel syndrome | 81.5 | NA | 10 mL of 1% lidocaine with 1:100,000 adrenaline and 8 mg of dexamethasone | Zero | |
| Local anesthesia with sedation | Ramos et al., 2023 [15] | 28 | 1 month | Carpal tunnel release/De Quervain’s tenosynovitis/synovial cyst/finger cyst/trigger finger | 85.7 | NR | 10 mL of 1% lidocaine only | Zero | |
| Local anesthesia with torniquet | Lichtman, Florio and Mack, 1979 [19] | 100 | 6 months | Carpal tunnel release | NR | 16.0 ^ | 10 mL of 1% lidocaine only | 5.0 | |
| IVRB with lidocaine alone | Da Costa et al., 2011 [5] | 90 | 6 months | Carpal tunnel release | 96.0 | 44.0 ± 9.4 | 40 mL of 0.5% lidocaine only | 4.1 | |
| IVRB with lidocaine and clonidine | Da Costa et al., 2011 [5] | 67 | 6 months | Carpal tunnel release | 96.0 | 44.9 ± 10.7 | 40 mL of 0.5% lidocaine with clonidine 1 µg/kg | 4.1 | |
| IVRB with guanethidine and axillary plexus block | Gschwind et al., 1995 [6] | 39 | 8 weeks | Fasciectomy for Dupuytren’s contracture | 10.3 | 82.0 ^ | 20 mL of fluid containing 20 mg of guanethidine only | 12.8 | |
| Axillary plexus block | Far-Riera et al., 2023 [16] | 150 | 1 month | Carpal tunnel release/trigger finger | 69.0 | NR | NR | Zero | |
| Da Costa et al., 2011 [5] | 71 | 6 months | Carpal tunnel release | 96.0 | 16.0 ± 8.4 | 30 mL of 2% lidocaine with 1:200,000 adrenaline | 11.3 | ||
| Gschwind et al., 1995 [6] | 32 | 8 weeks | Fasciectomy for Dupuytren’s contracture | 18.8 | 70.0 ^ | Not reported | 6.3 | ||
| Recurrent CRPS | |||||||||
| IVRB with lidocaine + SGB with bupivacaine | Reuben, Rosenthal and Steinberg, 2000 [20] | 50 | 3 months | Upper extremity procedure including carpal tunnel release, tenolysis, tendon release, capsulotomy, arthrodesis and neuroma excision. Performed in those with a history of CRPS. | 74.0 | 45.0 ± 18.0 | Pre-incisional | 40 mL of 0.5% lidocaine (IVRB) and 10 mL of 0.25% bupivacaine (SGB) | 10.0 |
| IVRB with lidocaine | 50 | 82.0 | 40.0 ± 16.0 | Immediately postoperative | 40 mL of 0.5% lidocaine only | 72.0 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chua, M.; Ratnagandhi, A.; Seth, I.; Lim, B.; Cevik, J.; Rozen, W.M. The Evidence for Perioperative Anesthetic Techniques in the Prevention of New-Onset or Recurrent Complex Regional Pain Syndrome in Hand Surgery. J. Pers. Med. 2024, 14, 825. https://doi.org/10.3390/jpm14080825
Chua M, Ratnagandhi A, Seth I, Lim B, Cevik J, Rozen WM. The Evidence for Perioperative Anesthetic Techniques in the Prevention of New-Onset or Recurrent Complex Regional Pain Syndrome in Hand Surgery. Journal of Personalized Medicine. 2024; 14(8):825. https://doi.org/10.3390/jpm14080825
Chicago/Turabian StyleChua, Marcel, Avinassh Ratnagandhi, Ishith Seth, Bryan Lim, Jevan Cevik, and Warren M. Rozen. 2024. "The Evidence for Perioperative Anesthetic Techniques in the Prevention of New-Onset or Recurrent Complex Regional Pain Syndrome in Hand Surgery" Journal of Personalized Medicine 14, no. 8: 825. https://doi.org/10.3390/jpm14080825
APA StyleChua, M., Ratnagandhi, A., Seth, I., Lim, B., Cevik, J., & Rozen, W. M. (2024). The Evidence for Perioperative Anesthetic Techniques in the Prevention of New-Onset or Recurrent Complex Regional Pain Syndrome in Hand Surgery. Journal of Personalized Medicine, 14(8), 825. https://doi.org/10.3390/jpm14080825








