Reduced Clavicle Length Indicates the Severity of Scapular Misalignment in Obstetric Brachial Plexus Lesions
Abstract
1. Introduction
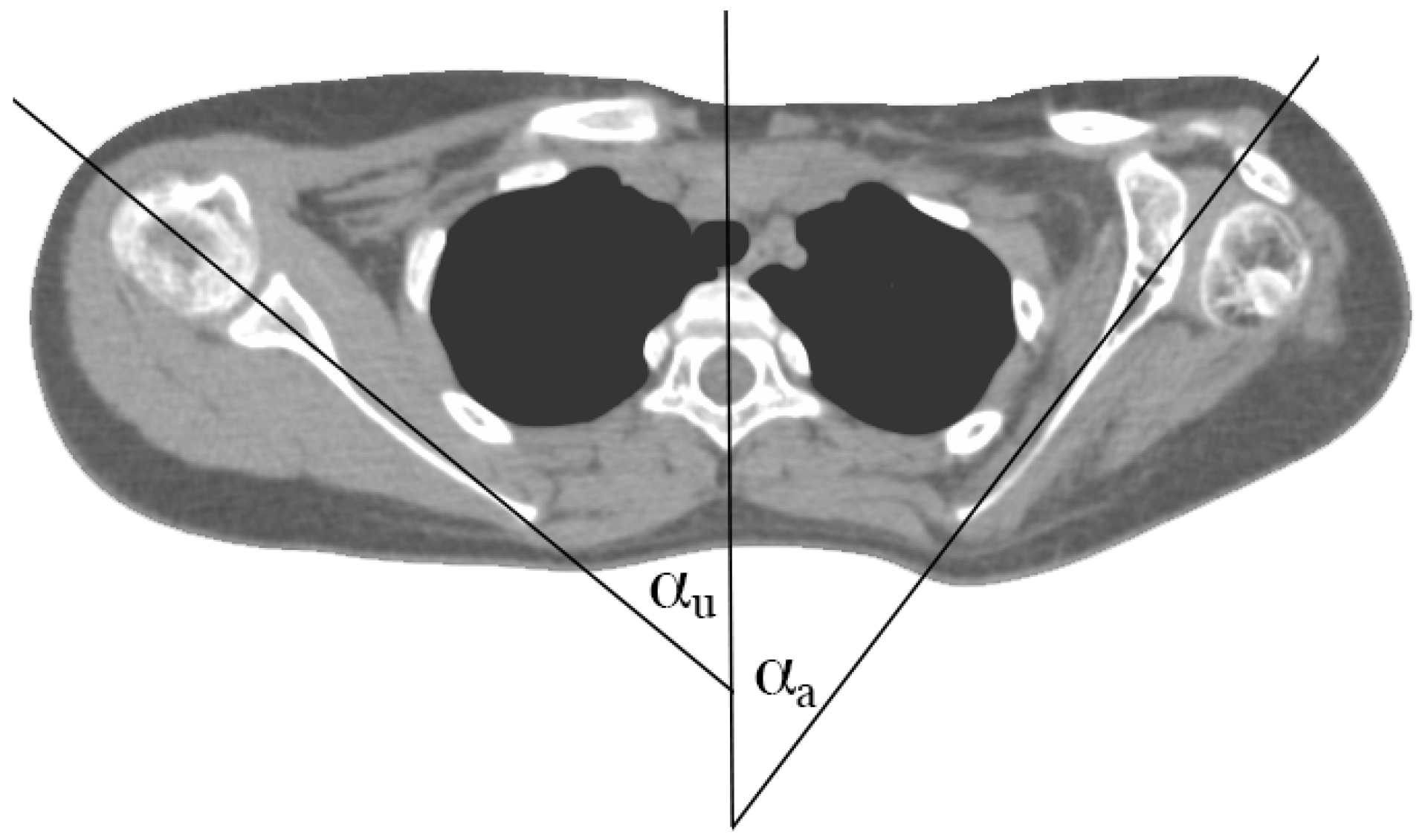
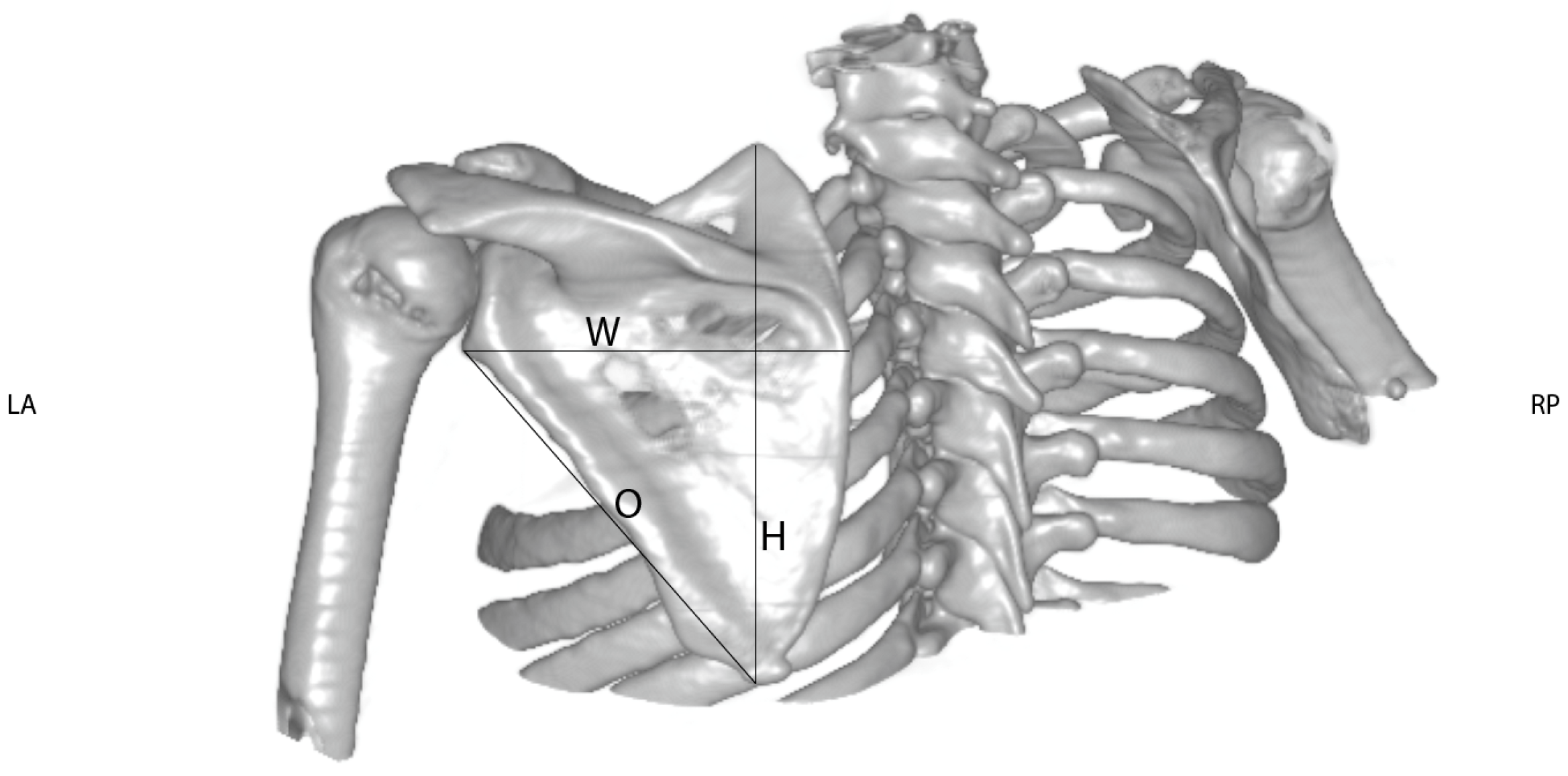
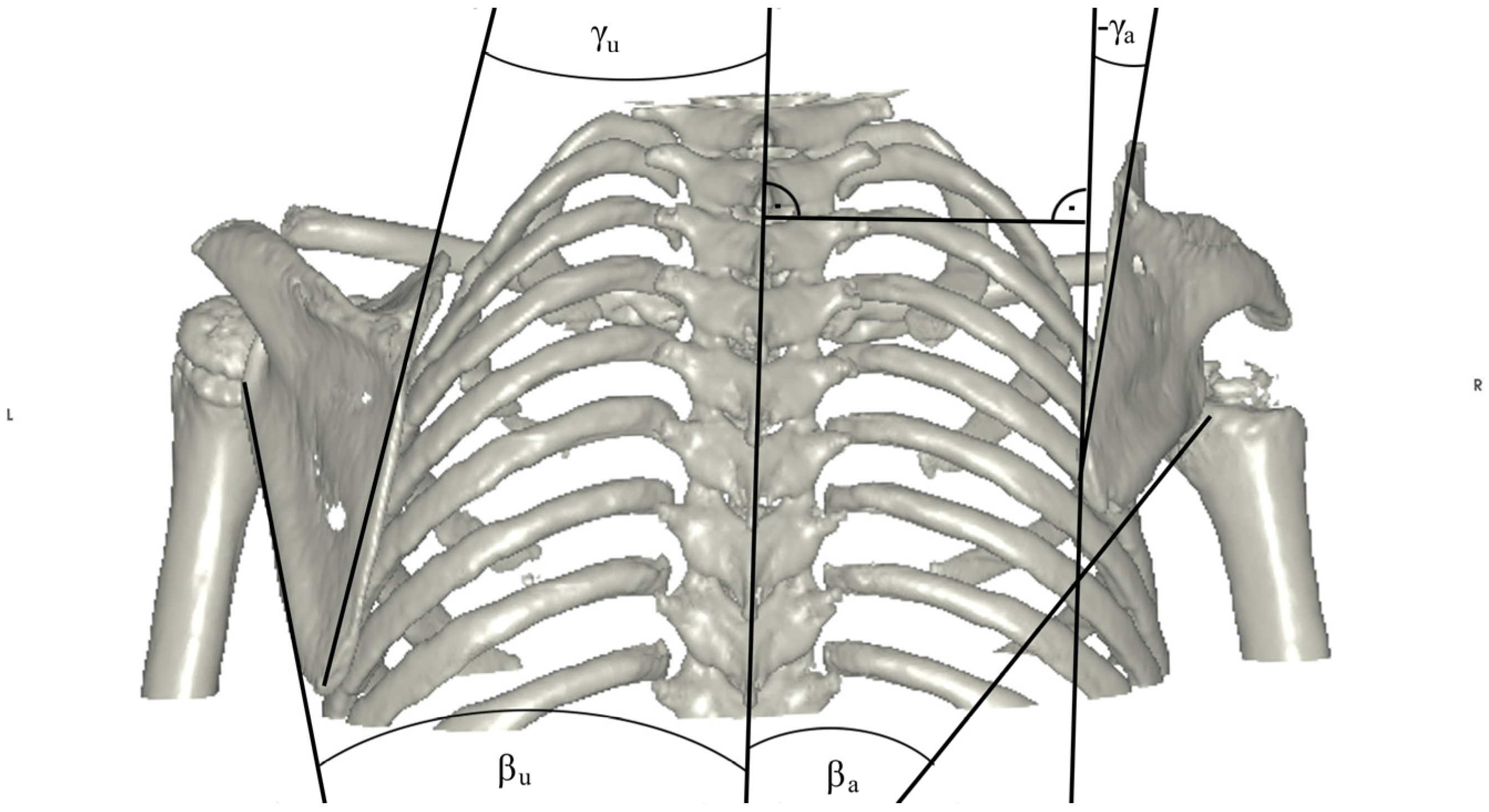
2. Materials and Methods
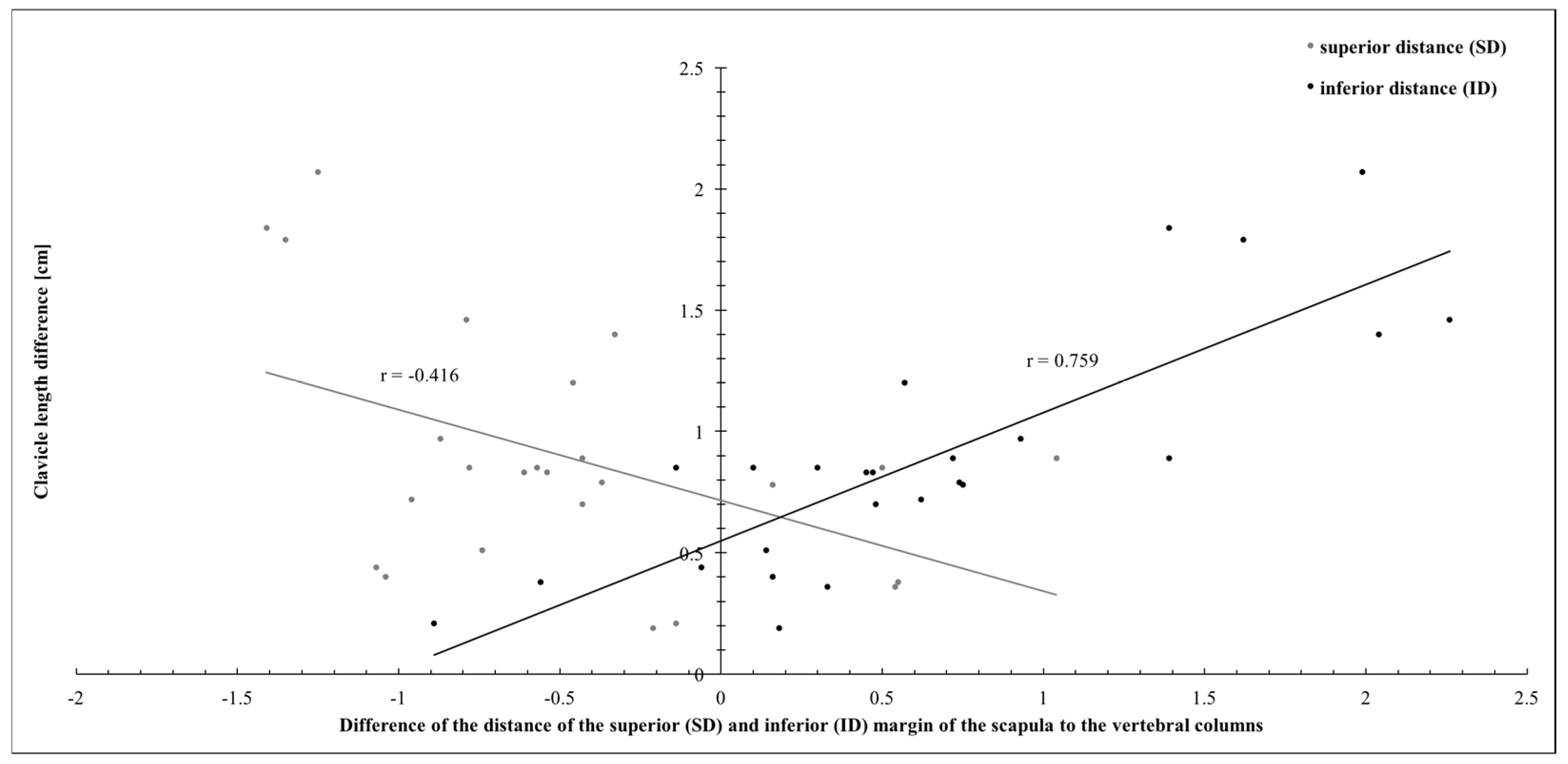
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Greenhill, D.A.; Lukavsky, R.; Tomlinson-Hansen, S.; Kozin, S.H.; Zlotolow, D.A. Relationships between 3 Classification Systems in Brachial Plexus Birth Palsy. J. Pediatr. Orthop. 2017, 37, 374–380. [Google Scholar] [CrossRef]
- Lalka, A.; Gralla, J.; Sibbel, S.E. Brachial Plexus Birth Injury: Epidemiology and Birth Weight Impact on Risk Factors. J. Pediatr. Orthop. 2020, 40, e460–e465. [Google Scholar] [CrossRef] [PubMed]
- DeFrancesco, C.J.; Shah, D.K.; Rogers, B.H.; Shah, A.S. The Epidemiology of Brachial Plexus Birth Palsy in the United States: Declining Incidence and Evolving Risk Factors. J. Pediatr. Orthop. 2019, 39, e134–e140. [Google Scholar] [CrossRef]
- Greenhill, D.A.; Smith, W.R.; Ramsey, F.V.; Kozin, S.H.; Zlotolow, D.A. Double Versus Single Tendon Transfers to Improve Shoulder Function in Brachial Plexus Birth Palsy. J. Pediatr. Orthop. 2019, 39, 328–334. [Google Scholar] [CrossRef]
- Leshikar, H.B.; Bauer, A.S.; Lightdale-Miric, N.; Molitor, F.; Waters, P.M. Clavicle Fracture Is Not Predictive of the Need for Microsurgery in Brachial Plexus Birth Palsy. J. Pediatr. Orthop. 2018, 38, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Bahm, J.; Schäfer, B. Microsurgical Reconstruction of Obstetric Brachial Plexus Palsy: Ongoing Challenges and Future Directions. J. Hand Surg. 2023, 48, 368–372. [Google Scholar] [CrossRef] [PubMed]
- van Gelein Vitringa, V.M.; van Royen, B.J.; van der Sluijs, J.A. Scapular Deformity in Obstetric Brachial Plexus Palsy and the Hueter-Volkmann Law; a Retrospective Study. BMC Musculoskelet. Disord. 2013, 14, 107. [Google Scholar] [CrossRef]
- Frich, L.H.; Schmidt, P.H.; Torfing, T. Glenoid Morphology in Obstetrical Brachial Plexus Lesion: A Three-Dimensional Computed Tomography Study. J. Shoulder Elb. Surg. 2017, 26, 1374–1382. [Google Scholar] [CrossRef]
- Pearl, M.L.; Edgerton, B.W. Glenoid Deformity Secondary to Brachial Plexus Birth Palsy. J. Bone Jt. Surg. 1998, 80, 659–667. [Google Scholar] [CrossRef]
- Abzug, J.M.; Wyrick-Glover, T.O.; Case, A.L.; Zlotolow, D.A.; Kozin, S.H. Loss of Midline Function in Brachial Plexus Birth Palsy Patients. J. Pediatr. Orthop. 2019, 39, e232–e235. [Google Scholar] [CrossRef]
- Russo, S.A.; Kozin, S.H.; Zlotolow, D.A.; Nicholson, K.F.; Richards, J.G. Motion Necessary to Achieve Mallet Internal Rotation Positions in Children With Brachial Plexus Birth Palsy. J. Pediatr. Orthop. 2019, 39, 14–21. [Google Scholar] [CrossRef]
- Pollock, A.N.; Reed, M.H. Shoulder Deformities from Obstetrical Brachial Plexus Paralysis. Skelet. Radiol. 1989, 18, 295–297. [Google Scholar] [CrossRef]
- Dixit, N.N.; McFarland, D.C.; Saul, K.R. Computational Analysis of Glenohumeral Joint Growth and Morphology Following a Brachial Plexus Birth Injury. J. Biomech. 2019, 86, 48–54. [Google Scholar] [CrossRef]
- Gladstein, A.Z.; Sachleben, B.; Ho, E.S.; Anthony, A.; Clarke, H.M.; Hopyan, S. Forearm Pronation Osteotomy for Supination Contracture Secondary to Obstetrical Brachial Plexus Palsy: A Retrospective Cohort Study. J. Pediatr. Orthop. 2017, 37, e357–e363. [Google Scholar] [CrossRef]
- Lahiji, F.A.; Tahririan, M.A.; Karami, M.; Madadi, F.; Emami, M.; Maleki, A. Transfer of Pectoralis Major to Subscapularis in the Management of Brachial Plexus Birth Palsy Sequels. J. Pediatr. Orthop. 2017, 37, 305–310. [Google Scholar] [CrossRef]
- DeDeugd, C.M.; Shin, A.Y.; Shaughnessy, W.J. Derotational Pronation-Producing Osteotomy of the Radius and Biceps Tendon Rerouting for Supination Contractures in Neonatal Brachial Plexus Palsy Patients: A Review of 20 Cases. J. Pediatr. Orthop. 2019, 39, e366–e372. [Google Scholar] [CrossRef]
- Pillen, S.; van Alfen, N. Skeletal Muscle Ultrasound. Neurol. Res. 2011, 33, 1016–1024. [Google Scholar] [CrossRef]
- Jit, I.; Kulkarni, M. Times of Appearance and Fusion of Epiphysis at the Medial End of the Clavicle. Indian J. Med. Res. 1976, 64, 773–782. [Google Scholar]
- Georgieff, M.K.; Bernbaum, J.C. Abnormal Shoulder Girdle Muscle Tone in Premature Infants during Their First 18 Months of Life. Pediatrics 1986, 77, 664–669. [Google Scholar] [CrossRef] [PubMed]
- Monfort, K.; Case-Smith, J. The Effects of a Neonatal Positioner on Scapular Rotation. Am. J. Occup. Ther. 1997, 51, 378–384. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alberti, E.J.; Pichorim, S.F.; Brawerman, A. An Obstetric Brachial Plexus Lesion Rehabilitation Platform. Res. Biomed. Eng. 2019, 35, 167–172. [Google Scholar] [CrossRef]
- Sibbel, S.E.; Bauer, A.S.; James, M.A. Late Reconstruction of Brachial Plexus Birth Palsy. J. Pediatr. Orthop. 2014, 34, S57–S62. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.; Laor, T.; Carr, P.; Zbojniewicz, A.; Cornwall, R. The Effect of Scapular Position on Magnetic Resonance Imaging Measurements of Glenohumeral Dysplasia Caused by Neonatal Brachial Plexus Palsy. J. Hand Surg. 2017, 42, 1030.e1–1030.e11. [Google Scholar] [CrossRef]
- Narakas, A.O. Obstetrical brachial plexus injuries. In The Paralysed Hand; Churchill Livingstone: Edinburgh, Scotland, 1987; pp. 116–135. [Google Scholar]
- Waters, P.M.; Smith, G.R.; Jaramillo, D. Glenohumeral Deformity Secondary to Brachial Plexus Birth Palsy. J. Bone Jt. Surg. 1998, 80, 668–677. [Google Scholar] [CrossRef]
- Bahm, J. Upper Limb Multifactorial Movement Analysis in Brachial Plexus Birth Injury. J. Brachial Plex. Peripher. Nerve Inj. 2016, 11, e1–e9. [Google Scholar] [CrossRef][Green Version]
- Chung, K.; Yang, L.; McGillicuddy, J. Practical Management of Pediatric and Adult Brachial Plexus Palsies E-Book; Elsevier Health Scieces: Amsterdam, The Netherlands, 2011. [Google Scholar]
- Ogden, J.A.; Phillips, S.B. Radiology of Postnatal Skeletal Development. VII. The Scapula. Skelet. Radiol. 1983, 9, 157–169. [Google Scholar] [CrossRef]
- Ogden, J.A.; Conlogue, G.J.; Bronson, M.L. Radiology of Postnatal Skeletal Development. III. The Clavicle. Skelet. Radiol. 1979, 4, 196–203. [Google Scholar] [CrossRef]




| # | Clavicle Length [cm] | Sagittal Orientation of the Scapula [°] | Dimensions of the Scapula [cm] | Distance of the Superior and Inferior Margins to the Vertebral Column [cm] | Angles of the Medial and Lateral Borders of the Scapula to the Vertebral Column [°] | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Width | Height | Oblique | Superior Margin | Inferior Margin | Medial Border | Lateral Border | ||||||||||||
| Healthy | Affected | Healthy | Affected | Healthy | Affected | Healthy | Affected | Healthy | Affected | Healthy | Affected | Healthy | Affected | Healthy | Affected | Healthy | Affected | |
| 1 | 14.29 | 13.44 | 40.55 | 25.93 | 11.58 | 10.14 | 14.67 | 12.87 | 12.06 | 7.99 | 6.21 | 6.99 | 10.47 | 10.61 | 13.80 | 16.94 | 19.21 | 21.69 |
| 2 | 8.14 | 7.36 | 40.45 | 32.19 | 6.98 | 6.13 | 7.89 | 7.52 | 6.56 | 5.12 | 4.54 | 4.38 | 7.32 | 6.57 | 16.67 | 8.10 | 24.49 | 31.92 |
| 3 | 10.31 | 9.95 | 41.33 | 22.05 | 9.55 | 9.09 | 10.68 | 10.00 | 9.48 | 7.26 | 7.25 | 6.71 | 9.99 | 9.66 | 15.49 | 14.73 | 12.80 | 14.58 |
| 4 | 9.84 | 9.01 | 40.40 | 32.97 | 9.01 | 8.39 | 9.72 | 9.19 | 7.49 | 6.43 | 5.20 | 5.74 | 7.99 | 7.54 | 25.74 | 25.05 | 24.47 | 17.94 |
| 5 | 6.49 | 6.28 | 40.34 | 23.85 | 5.69 | 5.43 | 6.37 | 6.29 | 5.20 | 3.79 | 5.22 | 5.36 | 6.00 | 6.89 | 27.78 | 24.78 | 20.47 | 20.11 |
| 6 | 8.90 | 8.05 | 47.51 | 41.32 | 7.27 | 6.76 | 8.57 | 9.21 | 7.18 | 5.81 | 4.24 | 3.74 | 8.15 | 8.05 | 21.37 | 26.42 | 11.01 | 3.88 |
| 7 | 11.13 | 10.73 | 44.43 | 28.91 | 10.55 | 8.75 | 11.58 | 11.25 | 9.96 | 9.25 | 6.32 | 7.36 | 8.23 | 8.07 | 5.45 | 6.89 | 40.73 | 41.78 |
| 8 | 8.46 | 7.76 | 21.81 | 16.83 | 8.03 | 7.29 | 9.59 | 8.94 | 7.24 | 5.89 | 7.54 | 7.97 | 8.96 | 8.48 | 11.94 | 9.30 | 24.04 | 37.34 |
| 9 | 12.50 | 11.53 | 46.55 | 52.84 | 12.18 | 11.17 | 13.82 | 12.80 | 11.28 | 9.75 | 6.70 | 7.57 | 9.47 | 8.54 | 13.59 | 19.71 | 23.34 | 29.18 |
| 10 | 11.06 | 10.17 | 41.54 | 41.67 | 11.16 | 10.81 | 11.58 | 11.24 | 9.95 | 8.82 | 6.96 | 5.92 | 10.51 | 9.12 | 17.82 | 23.47 | 8.86 | 17.19 |
| 11 | 10.02 | 9.64 | 41.07 | 35.00 | 8.25 | 7.64 | 10.08 | 10.40 | 8.28 | 7.07 | 5.61 | 5.06 | 8.86 | 9.42 | 15.61 | 16.37 | 16.22 | 17.09 |
| 12 | 14.67 | 12.88 | 37.78 | 44.39 | 13.39 | 12.70 | 14.87 | 13.35 | 14.56 | 11.42 | 7.79 | 9.14 | 11.45 | 9.83 | 13.98 | 23.13 | 8.78 | 23.23 |
| 13 | 11.53 | 11.09 | 41.48 | 33.03 | 10.20 | 9.25 | 12.38 | 11.40 | 11.09 | 9.84 | 6.07 | 7.14 | 10.56 | 10.62 | 20.22 | 14.72 | 16.62 | 16.23 |
| 14 | 9.21 | 8.38 | 47.10 | 35.64 | 7.75 | 7.65 | 9.14 | 8.06 | 7.46 | 5.76 | 5.87 | 6.48 | 8.06 | 7.59 | 14.10 | 17.11 | 24.37 | 27.54 |
| 15 | 11.70 | 10.50 | 49.37 | 37.53 | 9.80 | 8.90 | 11.67 | 10.95 | 9.38 | 8.61 | 8.49 | 8.95 | 8.53 | 7.96 | 10.03 | 19.73 | 33.37 | 35.89 |
| 16 | 14.66 | 13.94 | 61.71 | 39.88 | 11.16 | 10.73 | 16.92 | 16.14 | 14.69 | 13.32 | 8.54 | 9.50 | 11.12 | 10.50 | 6.34 | 8.49 | 23.85 | 30.20 |
| 17 | 11.01 | 10.50 | 53.59 | 48.44 | 8.31 | 8.35 | 11.38 | 9.99 | 10.74 | 7.40 | 7.67 | 8.41 | 8.07 | 7.93 | 10.19 | 10.71 | 28.08 | 34.21 |
| 18 | 11.23 | 9.83 | 40.87 | 52.36 | 10.50 | 8.96 | 12.40 | 11.52 | 11.42 | 8.44 | 6.59 | 6.92 | 10.55 | 8.51 | 14.91 | 26.17 | 14.19 | 20.89 |
| 19 | 14.28 | 12.82 | 39.54 | 43.60 | 12.90 | 12.29 | 15.57 | 12.24 | 13.74 | 10.93 | 8.73 | 9.52 | 10.51 | 8.25 | 8.92 | 18.97 | 29.61 | 39.24 |
| 20 | 7.66 | 6.81 | 41.11 | 36.20 | 6.32 | 5.69 | 8.82 | 8.13 | 6.39 | 5.40 | 5.53 | 6.10 | 7.08 | 6.78 | 17.74 | 20.55 | 17.98 | 24.85 |
| 21 | 12.01 | 9.94 | 46.48 | 32.47 | 9.54 | 9.14 | 12.55 | 11.35 | 10.77 | 8.61 | 7.26 | 8.51 | 9.04 | 7.05 | 11.37 | 24.97 | 26.82 | 63.77 |
| 22 | 8.82 | 8.63 | 35.28 | 31.09 | 8.73 | 7.81 | 10.31 | 10.01 | 8.24 | 7.56 | 5.88 | 6.09 | 7.70 | 7.52 | 12.91 | 10.66 | 29.29 | 19.99 |
| 23 | 12.54 | 11.75 | 38.88 | 34.78 | 10.01 | 9.83 | 12.84 | 12.69 | 11.38 | 10.73 | 8.63 | 9.00 | 9.44 | 8.70 | 0.33 | 4.83 | 20.38 | 24.00 |
| 24 | 12.38 | 10.54 | 43.43 | 35.19 | 9.48 | 9.20 | 12.69 | 11.65 | 12.36 | 8.98 | 7.16 | 8.57 | 9.07 | 7.68 | 13.23 | 21.51 | 23.62 | 34.47 |
| 25 | 11.79 | 10.90 | 48.73 | 36.97 | 10.98 | 10.20 | 12.36 | 11.14 | 10.56 | 7.79 | 5.46 | 5.89 | 7.64 | 6.92 | 12.15 | 18.75 | 39.62 | 46.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosenauer, R.; Nógrádi, A.; Quadlbauer, S.; Schmidhammer, M.; Schmidhammer, R.; Tsolakidis, S. Reduced Clavicle Length Indicates the Severity of Scapular Misalignment in Obstetric Brachial Plexus Lesions. J. Pers. Med. 2024, 14, 846. https://doi.org/10.3390/jpm14080846
Rosenauer R, Nógrádi A, Quadlbauer S, Schmidhammer M, Schmidhammer R, Tsolakidis S. Reduced Clavicle Length Indicates the Severity of Scapular Misalignment in Obstetric Brachial Plexus Lesions. Journal of Personalized Medicine. 2024; 14(8):846. https://doi.org/10.3390/jpm14080846
Chicago/Turabian StyleRosenauer, Rudolf, Antal Nógrádi, Stefan Quadlbauer, Markus Schmidhammer, Robert Schmidhammer, and Savas Tsolakidis. 2024. "Reduced Clavicle Length Indicates the Severity of Scapular Misalignment in Obstetric Brachial Plexus Lesions" Journal of Personalized Medicine 14, no. 8: 846. https://doi.org/10.3390/jpm14080846
APA StyleRosenauer, R., Nógrádi, A., Quadlbauer, S., Schmidhammer, M., Schmidhammer, R., & Tsolakidis, S. (2024). Reduced Clavicle Length Indicates the Severity of Scapular Misalignment in Obstetric Brachial Plexus Lesions. Journal of Personalized Medicine, 14(8), 846. https://doi.org/10.3390/jpm14080846






