Insurance Types and All-Cause Mortality in Korean Cancer Patients: A Nationwide Population-Based Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
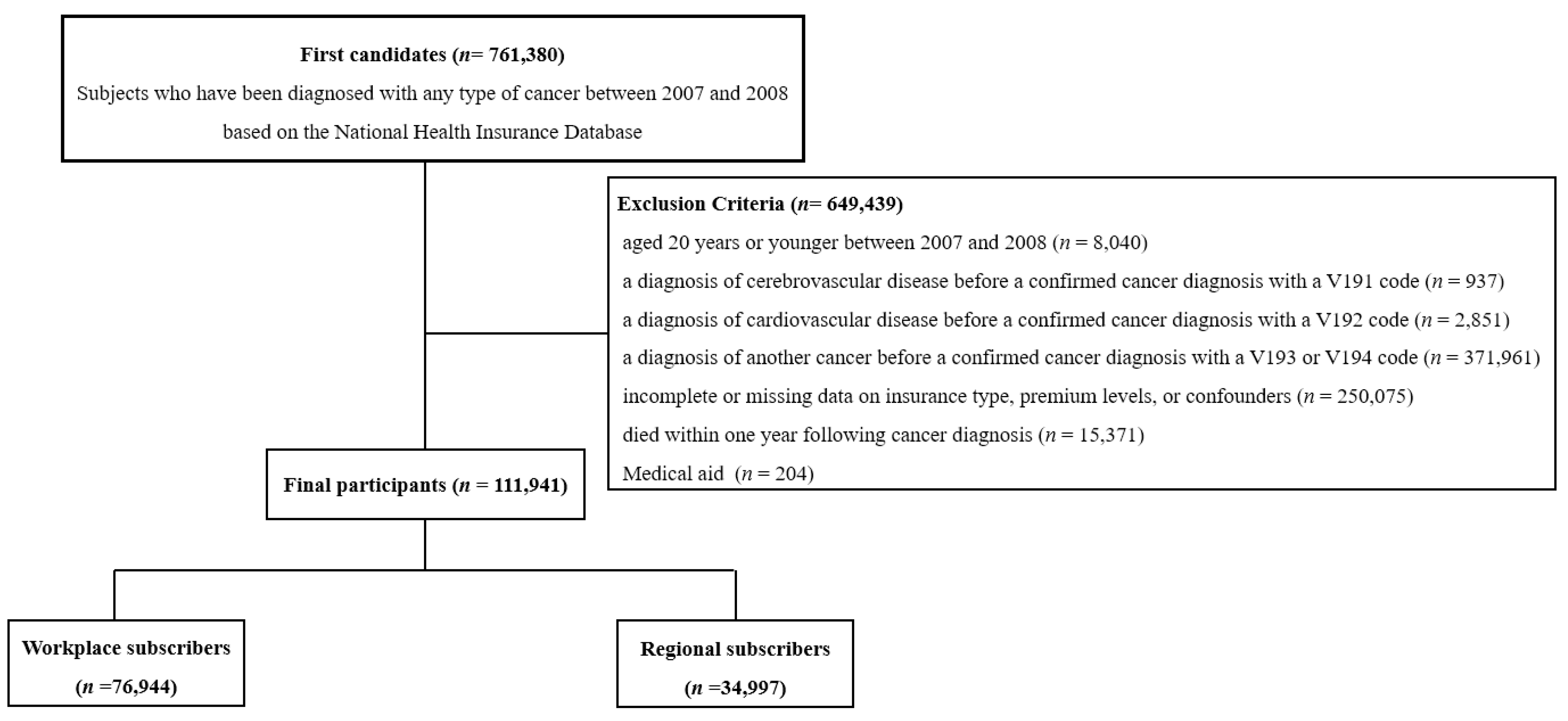
2.2. Study Subjects
2.3. Definitions of Insurance Types, Malignancy, and Confounders
2.4. Statistical Analysis
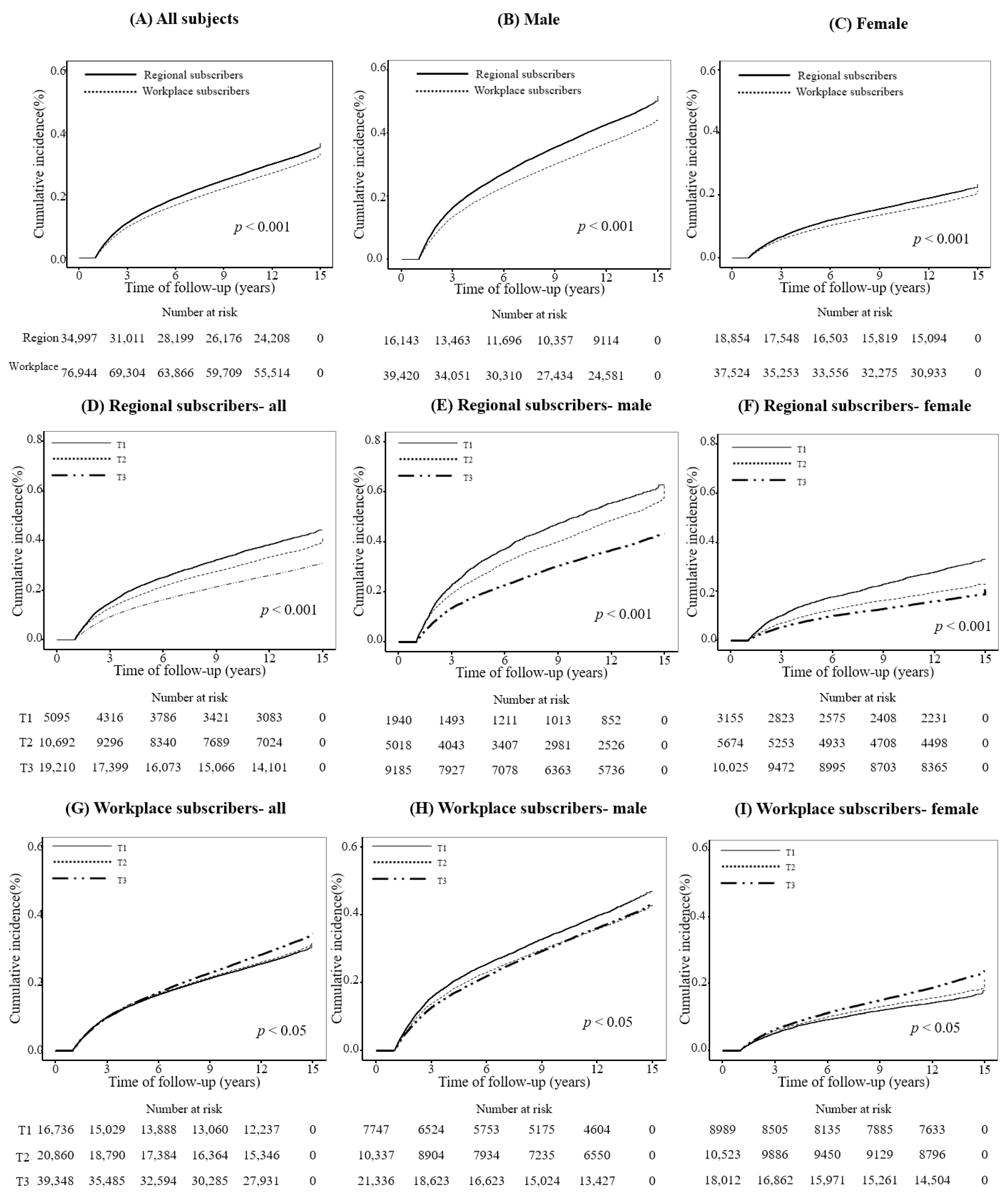
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Statistics Korea. Causes of Death Statistics. Available online: https://kostat.go.kr/menu.es?mid=a20205010000 (accessed on 10 October 2023).
- Hastings, K.G.; Boothroyd, D.B.; Kapphahn, K.; Hu, J.; Rehkopf, D.H.; Cullen, M.R.; Palaniappan, L. Socioeconomic Differences in the Epidemiologic Transition From Heart Disease to Cancer as the Leading Cause of Death in the United States, 2003 to 2015: An Observational Study. Ann. Intern. Med. 2018, 169, 836–844. [Google Scholar] [CrossRef]
- Heron, M.; Anderson, R.N. Changes in the Leading Cause of Death: Recent Patterns in Heart Disease and Cancer Mortality. NCHS Data Brief 2016, 254, 1–8. [Google Scholar]
- Kang, H.T. Current Status of the National Health Screening Programs in South Korea. Korean J. Fam. Med. 2022, 43, 168–173. [Google Scholar] [CrossRef]
- Suh, M.; Song, S.; Cho, H.N.; Park, B.; Jun, J.K.; Choi, E.; Kim, Y.; Choi, K.S. Trends in Participation Rates for the National Cancer Screening Program in Korea, 2002–2012. Cancer Res. Treat. 2017, 49, 798–806. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.J.; Won, Y.J.; Lee, J.J.; Jung, K.W.; Kim, H.J.; Kong, H.J.; Im, J.S.; Seo, H.G. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2019. Cancer Res. Treat. 2022, 54, 330–344. [Google Scholar] [CrossRef] [PubMed]
- WHO. Total Population with Household Expenditures on Health Greater than 10% of Total Household Expenditure or Income. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/total-population-with-household-expenditures-on-health-greater-than-10-of-total-household-expenditure-or-income-(sdg-3-8-2)-(-) (accessed on 1 August 2024).
- Quatromoni, J.; Jones, R. Inequalities in socio-economic status and invasive procedures for coronary heart disease: A comparison between the USA and the UK. Int. J. Clin. Pract. 2008, 62, 1910–1919. [Google Scholar] [CrossRef]
- Alves Soares Ferreira, N.; Melo Figueiredo de Carvalho, S.; Engrácia Valenti, V.; Pinheiro Bezerra, I.M.; Melo Teixeira Batista, H.; de Abreu, L.C.; Matos, L.L.; Adami, F. Treatment delays among women with breast cancer in a low socio-economic status region in Brazil. BMC Womens Health 2017, 17, 13. [Google Scholar] [CrossRef]
- Kim, M.J.; Lee, H.; Kim, E.H.; Cho, M.H.; Shin, D.W.; Yun, J.M.; Shin, J.H. Disparity in Health Screening and Health Utilization according to Economic Status. Korean J. Fam. Med. 2017, 38, 220–225. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef]
- Simsek, H.; Doganay, S.; Budak, R.; Ucku, R. Relationship of socioeconomic status with health behaviors and self-perceived health in the elderly: A community-based study, Turkey. Geriatr. Gerontol. Int. 2014, 14, 960–968. [Google Scholar] [CrossRef]
- Moorin, R.E.; Holman, C.D. The effects of socioeconomic status, accessibility to services and patient type on hospital use in Western Australia: A retrospective cohort study of patients with homogenous health status. BMC Health Serv. Res. 2006, 6, 74. [Google Scholar] [CrossRef] [PubMed]
- Noh, E.; Khang, Y.H. Occupational inequalities in mortality in Korea using nationally representative mortality follow-up data from the late 2000s and after. Epidemiol. Health 2022, 44, e2022038. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.; Song, Y.M.; Kim, T.H.; Cho, S.I. Socio-economic status and the risk of liver cancer mortality: A prospective study in Korean men. Public Health 2008, 122, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.T.; Ju, Y.W.; Kim, Y.A.; Kim, J.; Oh, S.; Jung, J.; Chai, Y.J.; Choi, I.S.; Oh, S.W. Prognostic influence of Korean public medical insurance system on breast cancer patients. Ann. Surg. Treat. Res. 2019, 96, 58–69. [Google Scholar] [CrossRef]
- Fowler, H.; Belot, A.; Njagi, E.N.; Luque-Fernandez, M.A.; Maringe, C.; Quaresma, M.; Kajiwara, M.; Rachet, B. Persistent inequalities in 90-day colon cancer mortality: An English cohort study. Br. J. Cancer 2017, 117, 1396–1404. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.; Shin, D.W.; Lee, J.; Hwang, J.H.; Yoo, J.E.; Ko, H.; Song, Y.-M. Association between perception of care coordination and health outcomes in Korean cancer survivors. Health Qual. Life Outcomes 2020, 18, 21. [Google Scholar] [CrossRef] [PubMed]
- Pollock, A.M.; Vickers, N. Breast, lung and colorectal cancer incidence and survival in South Thames Region, 1987–1992: The effect of social deprivation. J. Public Health 1997, 19, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Kim, J.; Jeong, J.H.; Lee, J.K.; Chin, D.K.; Chung, C.K.; Lee, S.H.; Lee, J.Y. Prevalence and Incidence of Osteoporosis and Osteoporotic Vertebral Fracture in Korea: Nationwide Epidemiological Study Focusing on Differences in Socioeconomic Status. Spine 2016, 41, 328–336. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Kieszak, S.M.; Flanders, W.D.; Kosinski, A.S.; Shipp, C.C.; Karp, H. A comparison of the Charlson comorbidity index derived from medical record data and administrative billing data. J. Clin. Epidemiol. 1999, 52, 137–142. [Google Scholar] [CrossRef]
- Levy, A.R.; Tamblyn, R.M.; Fitchett, D.; McLeod, P.J.; Hanley, J.A. Coding accuracy of hospital discharge data for elderly survivors of myocardial infarction. Can. J. Cardiol. 1999, 15, 1277–1282. [Google Scholar] [PubMed]
- Quan, H.; Parsons, G.A.; Ghali, W.A. Validity of information on comorbidity derived rom ICD-9-CCM administrative data. Med. Care 2002, 40, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Chayo, I.; Uribe Perez, C.J.; De Vries, E.; Pinheiro, P.S. The impact of health insurance affiliation and socioeconomic status on cervical cancer survival in Bucaramanga, Colombia. Cancer Epidemiol. 2023, 85, 102375. [Google Scholar] [CrossRef] [PubMed]
- Gomez, S.L.; Chirikova, E.; McGuire, V.; Collin, L.J.; Dempsey, L.; Inamdar, P.P.; Lawson-Michod, K.; Peters, E.S.; Kushi, L.H.; Kavecansky, J.; et al. Role of neighborhood context in ovarian cancer survival disparities: Current research and future directions. Am. J. Obstet. Gynecol. 2023, 229, 366–376.e8. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Jang, S.; Lee, G.; Chang, Y.J. Disparities in Cancer-Related Avoidable Mortality by the Level of Area Deprivation in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 7856. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kang, H.T. Association between Socioeconomic Status and Cancer Screening in Koreans over 40 Years in Age Based on the 2010-2012 Korean National Health and Nutrition Examination Survey. Korean J. Fam. Med. 2016, 37, 287–292. [Google Scholar] [CrossRef]
- Oake, J.D.; Harasemiw, O.; Tangri, N.; Ferguson, T.W.; Saranchuk, J.W.; Bansal, R.K.; Drachenberg, D.E.; Nayak, J.G. The Association between Income Status and Treatment Selection for Prostate Cancer in a Universal Health Care System: A Population-Based Analysis. J. Urol. 2021, 206, 1204–1211. [Google Scholar] [CrossRef]
| Male | p-Value | Female | p-Value | |||
|---|---|---|---|---|---|---|
| Regional Subscribers | Workplace Subscribers | Regional Subscribers | Workplace Subscribers | |||
| Number | 16,143 | 39,420 | 18,854 | 37,524 | ||
| Age at cancer diagnosis, year | 63.6 ± 10.4 | 61.3 ± 12.2 | <0.001 | 57.6 ± 10.6 | 56.1 ± 12.5 | <0.001 |
| Body mass index, kg/m2 | 23.6 ± 3.0 | 23.6 ± 3.0 | 0.066 | 24.0 ± 3.3 | 23.6 ± 3.2 | <0.001 |
| Smoking status, N (%) | <0.001 | <0.001 | ||||
| Never | 8269 (51.2) | 20,855 (52.9) | 17,935 (95.1) | 36,534 (97.4) | ||
| Former | 3007 (18.6) | 7843 (19.9) | 263 (1.4) | 421 (1.1) | ||
| Current | 4867 (30.1) | 10,722 (27.2) | 656 (3.5) | 569 (1.5) | ||
| Alcohol consumption, N (%) | <0.001 | <0.001 | ||||
| Mild | 8451 (52.3) | 20,224 (51.3) | 15,721 (83.4) | 31,654 (84.4) | ||
| Moderate | 4461 (27.6) | 13,059 (33.1) | 2740 (14.5) | 5502 (14.7) | ||
| Heavy | 3231 (20.0) | 6137 (15.6) | 393 (2.1) | 368 (0.98) | ||
| Physical activity, N (%) | <0.001 | <0.001 | ||||
| Rare | 8292 (51.4) | 18,001 (45.7) | 10,436 (55.4) | 20,220 (53.9) | ||
| Moderate | 5403 (33.5) | 16,027 (40.7) | 6144 (32.6) | 13,190 (35.2) | ||
| Regular | 2448 (15.2) | 5392 (13.7) | 2274 (12.1) | 4114 (11.0) | ||
| Charlson comorbidity index, N (%) | <0.001 | 0.007 | ||||
| 0 | 3154 (19.5) | 8898 (22.6) | 5263 (27.9) | 10,870 (29.0) | ||
| 1 | 6314 (39.1) | 15,704 (39.8) | 7853 (41.7) | 15,645 (41.7) | ||
| ≥2 | 6675 (41.3) | 14.818 (37.6) | 5738 (30.4) | 11,009 (29.3) | ||
| Household income level, N (%) | <0.001 | <0.001 | ||||
| Lowest | 1940 (12.0) | 7747 (19.7) | 3155 (16.7) | 10,870 (29.0) | ||
| Middle | 5018 (31.1) | 10,337 (26.2) | 5674 (30.1) | 15,645 (41.7) | ||
| Highest | 9185 (56.9) | 21,336 (54.1) | 10,025 (53.2) | 11,009 (29.3) | ||
| Male | Regional Subscribers (n = 16,143) | p-Value | Workplace Subscribers (n = 39,420) | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | |||
| Number | 1940 | 5018 | 9185 | 7747 | 10,337 | 21,336 | ||
| Age at cancer diagnosis, year | 65.9 ± 11.4 | 63.8 ± 11.0 | 63.1 ± 9.9 | <0.001 | 62.0 ± 10.0 | 59.8 ± 12.0 | 61.8 ± 12.9 | <0.001 |
| Body mass index, kg/m2 | 23.2 ± 3.2 | 23.4 ± 3.1 | 23.8 ± 2.9 | <0.001 | 23.6 ± 3.0 | 23.6 ± 3.0 | 23.6 ± 2.9 | 0.534 |
| Smoking status, N (%) | <0.001 | <0.001 | ||||||
| Never | 932 (48.0) | 2462 (49.1) | 4875 (53.1) | 3915 (50.5) | 5166 (50.0) | 11,774 (55.2) | ||
| Former | 327 (16.9) | 832 (16.6) | 1848 (20.1) | 1315 (17.0) | 1947 (18.8) | 4581 (21.5) | ||
| Current | 681 (35.1) | 1724 (34.4) | 2462 (26.8) | 2517 (32.5) | 3224 (31.2) | 4981 (23.3) | ||
| Alcohol consumption, N (%) | <0.001 | <0.001 | ||||||
| Mild | 1074 (55.4) | 2691 (53.6) | 4686 (51.0) | 3932 (50.8) | 5126 (49.6) | 11,166 (52.3) | ||
| Moderate | 494 (25.5) | 1256 (25.0) | 2711 (29.5) | 2464 (31.8) | 3392 (32.8) | 7203 (33.8) | ||
| Heavy | 372 (19.2) | 1071 (21.3) | 1788 (19.5) | 1351 (17.4) | 1819 (17.6) | 2967 (13.9) | ||
| Physical activity, N (%) | <0.001 | <0.001 | ||||||
| Rare | 1135 (58.5) | 2879 (57.4) | 4278 (46.6) | 3791 (48.9) | 5005 (48.4) | 9205 (43.1) | ||
| Moderate | 544 (28.0) | 1462 (29.1) | 3397 (37.0) | 2983 (38.5) | 3985 (38.6) | 9059 (42.5) | ||
| Regular | 261 (13.5) | 677 (13.5) | 1510 (16.4) | 973 (12.6) | 1347 (13.0) | 3072 (14.4) | ||
| Charlson comorbidity index, N (%) | <0.001 | 0.074 | ||||||
| 0 | 368 (19.0) | 925 (18.4) | 1861 (20.3) | 1687 (21.8) | 2288 (221) | 4923 (23.1) | ||
| 1 | 719 (37.1) | 1927 (38.4) | 3668 (39.9) | 3093 (39.9) | 4183 (40.5) | 8428 (39.5) | ||
| ≥ 2 | 853 (44.0) | 2166 (43.2) | 3656 (39.8) | 2967 (38.3) | 3866 (37.4) | 7985 (37.4) | ||
| Female | Regional Subscribers (n = 18,854) | p-Value | Workplace Subscribers (n = 37,524) | p-Value | ||||
| T1 | T2 | T3 | T1 | T2 | T3 | |||
| Number | 3155 | 5674 | 10,025 | 8989 | 10,523 | 18,012 | ||
| Age at cancer diagnosis, year | 60.5 ± 12.4 | 57.2 ± 10.7 | 56.9 ± 9.7 | <0.001 | 53.6 ± 11.1 | 54.1 ± 12.6 | 58.6 ± 12.6 | <0.001 |
| Body mass index, kg/m2 | 23.9 ± 3.4 | 24.0 ± 3.4 | 24.0 ± 3.2 | 0.573 | 23.7 ± 3.2 | 23.7 ± 3.3 | 24.5 ± 3.2 | <0.001 |
| Smoking status, N (%) | <0.001 | <0.001 | ||||||
| Never | 2855 (90.5) | 5345 (94.2) | 9735 (97.1) | 8710 (96.9) | 10,195 (96.9) | 17,629 (97.9) | ||
| Former | 68 (2.2) | 91 (1.6) | 104 (1.0) | 111 (1.2) | 140 (1.3) | 170 (0.9) | ||
| Current | 232 (7.4) | 238 (4.2) | 186 (1.9) | 168 (1.9) | 188 (1.8) | 213 (1.2) | ||
| Alcohol consumption, N (%) | <0.001 | <0.001 | ||||||
| Mild | 2599 (82.4) | 4688 (82.6) | 8434 (84.1) | 7255 (80.7) | 8672 (82.4) | 15,727 (87.3) | ||
| Moderate | 460 (14.6) | 851 (15.0) | 1429 (14.3) | 1619 (18.0) | 1730 (16.4) | 2153 (12.0) | ||
| Heavy | 96 (3.0) | 135 (2.4) | 1629 (1.6) | 115 (1.3) | 121 (1.2) | 132 (0.7) | ||
| Physical activity, N (%) | <0.001 | <0.001 | ||||||
| Rare | 1986 (62.9) | 3358 (59.2) | 5092 (50.8) | 5063 (56.3) | 5913 (56.2) | 9244 (51.3) | ||
| Moderate | 846 (26.8) | 1649 (29.1) | 3649 (36.4) | 3030 (33.7) | 3537 (33.6) | 6623 (36.8) | ||
| Regular | 323 (10.2) | 667 (11.8) | 1284 (12.8) | 896 (10.0) | 1073 (10.2) | 2145 (11.9) | ||
| Charlson comorbidity index, N (%) | 0.002 | <0.001 | ||||||
| 0 | 828 (26.4) | 1539 (27.1) | 2896 (28.9) | 2729 (30.4) | 3162 (30.0) | 4979 (27.6) | ||
| 1 | 1296 (41.1) | 2375 (41.9) | 4182 (41.7) | 3845 (42.8) | 4363 (41.5) | 7437 (41.3) | ||
| ≥2 | 1031 (32.7) | 1760 (31.0) | 2947 (29.4) | 2415 (26.9) | 2998 (28.5) | 5596 (31.1) | ||
| All | Male | Female | ||||
|---|---|---|---|---|---|---|
| Regional Subscribers | Workplace Subscribers | Regional Subscribers | Workplace Subscribers | Regional Subscribers | Workplace Subscribers | |
| Model 1 | 1 | 0.891 (0.872–0.911) | 1 | 0.826 (0.804–0.849) | 1 | 0.880 (0.847–0.915) |
| Model 2 | 1 | 0.946 (0.925–0.967) | 1 | 0.919 (0.894–0.945) | 1 | 0.929 (0.893–0.966) |
| Model 3 | 1 | 0.940 (0.919–0.961) | 1 | 0.922 (0.897–0.948) | 1 | 0.925 (0.890–0.962) |
| Regional Subscribers | Workplace Subscribers | ||||||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | ||
| Male | Model 1 | 1 | 0.835 (0.770–0.895) | 0.572 (0.536–0.611) | 1 | 0.874 (0.830–0.915) | 0.881 (0.847–0.917) |
| Model 2 | 1 | 0.925 (0.863–0.991) | 0.700 (0.654–0.748) | 1 | 0.950 (0.908–0.994) | 0.871 (0.867–0.907) | |
| Model 3 | 1 | 0.925 (0.864–0.992) | 0.730 (0.682–0.781) | 1 | 0.950 (0.907–0.994) | 0.880 (0.846–0.916) | |
| Female | Model 1 | 1 | 0.655 (0.603–0.713) | 0.529 (0.489–0.571) | 1 | 1.098 (1.025–1.177) | 1.387 (1.306–1.474) |
| Model 2 | 1 | 0.876 (0.805–0.953) | 0.774 (0.715–0.839) | 1 | 0.993 (0.926–1.064) | 0.898 (0.844–0.956) | |
| Model 3 | 1 | 0.874 (0.803–0.952) | 0.777 (0.717–0.841) | 1 | 0.986 (0.920–1.057) | 0.883 (0.830–0.940) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, J.; Bae, Y.-J.; Kang, H.-T. Insurance Types and All-Cause Mortality in Korean Cancer Patients: A Nationwide Population-Based Cohort Study. J. Pers. Med. 2024, 14, 861. https://doi.org/10.3390/jpm14080861
Shin J, Bae Y-J, Kang H-T. Insurance Types and All-Cause Mortality in Korean Cancer Patients: A Nationwide Population-Based Cohort Study. Journal of Personalized Medicine. 2024; 14(8):861. https://doi.org/10.3390/jpm14080861
Chicago/Turabian StyleShin, Jinyoung, Yoon-Jong Bae, and Hee-Taik Kang. 2024. "Insurance Types and All-Cause Mortality in Korean Cancer Patients: A Nationwide Population-Based Cohort Study" Journal of Personalized Medicine 14, no. 8: 861. https://doi.org/10.3390/jpm14080861
APA StyleShin, J., Bae, Y.-J., & Kang, H.-T. (2024). Insurance Types and All-Cause Mortality in Korean Cancer Patients: A Nationwide Population-Based Cohort Study. Journal of Personalized Medicine, 14(8), 861. https://doi.org/10.3390/jpm14080861






