Maternal Health Phone Line: Saving Women in Papua New Guinea
Abstract
:1. Introduction
1.1. Project Establishment
1.2. Phone Calls Received
| Month | First Calls (New Obstetric Cases) | First Calls (New Non-Obstetric Cases) | Total Number of New Cases | Follow-Up Calls | Total Number Of All Calls |
|---|---|---|---|---|---|
| November 2012 | 17 | 2 | 19 | 49 | 68 |
| December 2012 | 19 | 6 | 25 | 53 | 78 |
| January 2013 | 27 | 2 | 29 | 22 | 51 |
| February 2013 | 14 | 2 | 16 | 35 | 51 |
| March 2013 | 27 | 5 | 32 | 51 | 83 |
| April 2013 | 14 | 2 | 16 | 25 | 41 |
| May 2013 | 10 | 4 | 14 | 17 | 31 |
| Total | 128 | 23 | 151 | 252 | 403 |
2. Literature
2.1. Maternal Health in PNG
2.2. Health Communication in PNG
2.3. Mobile Phones and Healthcare
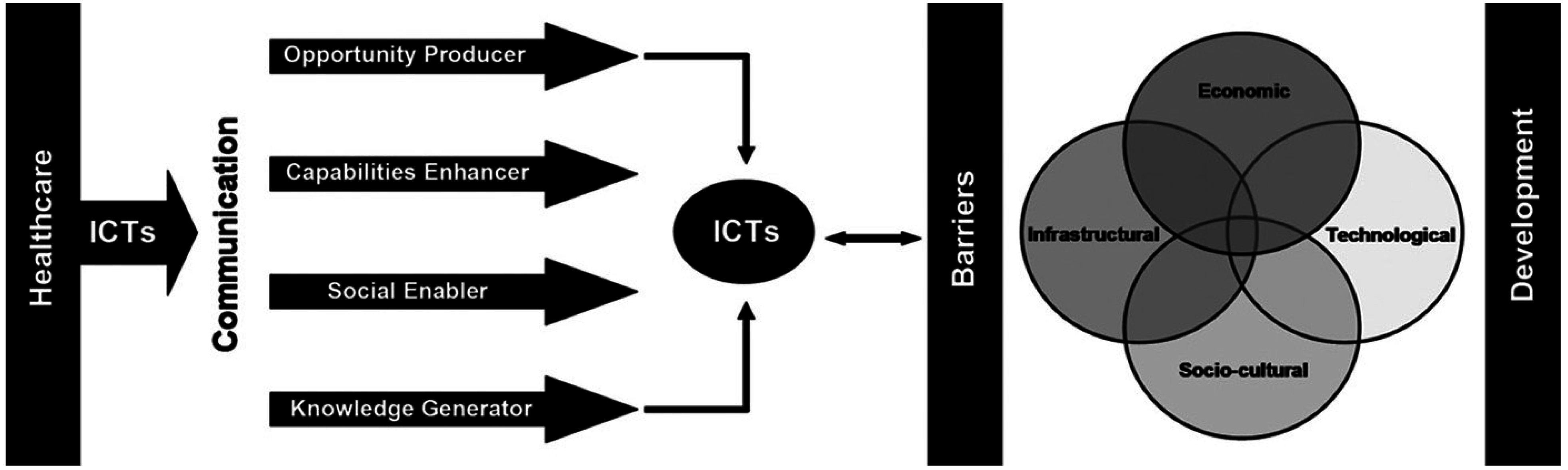
2.4. ICT4H Model
2.5. Three Stages of Delay

3. Research Design
3.1. Research Questions
3.2. Research Methods and Data Analysis
| Type of Interviewee | Number of Interviews |
|---|---|
| Rural health worker, based at health centre | 25 |
| Rural health worker, based at aid post | 3 |
| Labour ward staff member, round 1, 2012 | 5 |
| Labour ward staff member, round 2, 2013 | 5 |
| Mother | 2 |
| Community leader | 2 |
| Total | 42 |
4. Results in Relation to Theoretical Models
4.1. Findings in Relation to ICT4H Model
“Now we also have phones that we can be able to communicate out. But the only problem is sometimes phones too they don’t have units (mobile phone credit). Out here in the remote (areas), we find it difficult to find a unit. When we have a unit available, then we can be able to communicate out. And that’s when if we can be able to manage what we can then but like if we need the extra advice from the what (colleagues elsewhere), that’s the difficulties we are facing.”
“The project is very good. Before, I saw a mother die in front of me, because of no communication. Today, anywhere I can call, and it’s free. I don’t need to spend any money and it’s very good. I’m really happy and I thank the Australian government for this initiative to help people, especially those of us serving the remote, rural majority out here. They’re lowly educated, they do not have much money also, services are far away and we are the ones, we attend to them.”
“With the phone coming up, you realise that we are all very happy, because now we can have calls straight coming into the ward and we can answer to their calls, especially their needing help, because we see the difficulty of the whole, you know, process of getting, I mean the whole process of communicating, for a patient, for an obstetric emergency.”
“Straight after we got this information about the free-call to the labour ward, I had this retained placenta. And I went. For three days, this mother was, you know, placenta was retained, and when I went to the clinic site, straight away from there I talked to the labour ward staff and I got advice on what to do. Had I not, you know, if this project was not here and I didn’t have any means to communicate, we could have lost this mother because she was already septicaemic. And so I find it very helpful. It’s very good. From anywhere, any point, I could seek advice. Very isolated or what, I could seek advice and I can help the patients.”
4.2. Findings in Relation to Three Stages of Delay

“There are numerous number of them, for example, we have one girl, … she was at her about third trimester, I mean almost to deliver and then she got sick, not knowing that (her) mother … died from preeclampsia toxemia, nobody knew that she was a preeclampsia toxemia, she was undiagnosed preeclampsia toxemia, so when she had that high sudden fever and then her heart started to go faster she just passed away, here no one knew, she just slept and died, it was preeclampsia toxemia. But to them the parents, they said, not this one, they pwakau (poisoned), her already, they poison her or gave her something and she is like that, so to us is poor negligence or poor misdiagnose or other things but to them, village community is not that, it’s that thing, Poison. (…) Even, death that happens in the health centre has a traditional cause of death more than the physical illness itself, so in one other sense is that there is a need for awareness and health education in a sense that everyone must know that every deceased has a pathological cause or other socio-economical factor involve in it. Otherwise, this people will not understand yet.”
“I responded to a case this morning. Upon advice that the clinician should use oxytocin but it was out of stock. The patient was transported to the next health facility in order to execute the advice given. We here at the hospital have everything but I feel responsible when giving advice and the prescribed drug is unavailable. Every call we receive from rural health facilities, the patient becomes our patient and responsibility.”
5. Discussion
5.1. Practical Implications of Research
5.2. Theoretical Implications of Research
5.3. Limitations of Research
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fifer, D. Comment. Australian Volunteers International Magazine, Winter 2010. [Google Scholar]
- Giris, J.; Rynkiewich, T.; Dick Kapinias, I.; Winfrey, P. Emerging Issues for Women and Children in Papua New Guinea; Melanesian Institute: Goroka, Papua New Guinea, 2005. [Google Scholar]
- Ministerial Forum. Schedule to the Papua New Guinea—Australia Partnership for Development, Priority Outcome 2: Health and HIV/AIDS; Government of Papua New Guinea and the Government of Australia: Port Moresby, Papua New Guinea, 2011.
- Papua New Guinea Medium Term Development Plan 2011–2015; Department of National Planning and Monitoring: Port Moresby, Papua New Guinea, 2010.
- Papua New Guinea Development Strategic Plan 2010–2030; Department of National Planning and Monitoring: Port Moresby, Papua New Guinea, 2010.
- Kirby, B. Maternal Deaths in PNG. OG Mag. Aust. 2011, 13, 57–59. [Google Scholar]
- The World Bank. PNG Health Workforce Crisis: A Call to Action; The World Bank: Port Moresby, Papua New Guinea, 2011. [Google Scholar]
- Ministerial Taskforce on Maternal Health in Papua New Guinea, Report; National Department of Health: Port Moresby, Papua New Guinea, 2009.
- National Health Plan 2011–2020; Government of Papua New Guinea: Port Moresby, Papua New Guinea, 2010; Volume 2.
- Chib, A.; Lwin, M.O.; Ang, J.; Lin, H.; Santoso, F. Midwives and mobiles: Using ICTs to improve healthcare in Aceh Besar, Indonesia. Asian J. Commun. 2008, 18, 348–364. [Google Scholar] [CrossRef]
- Milne Bay Provincial Health Capacity Diagnostic Assessment, Draft Report; Papua New Guinea National Department of Health and AusAID: Port Moresby, Papua New Guinea, 2011.
- Erbs, A. NDoH National Health Services Radio Network Review: Options to Strengthen and Support Rural and Remote Communications in the Health Sector for PNG; JTA International: Port Moresby, Papua New Guinea, 2012. [Google Scholar]
- Weigel, G. Part 1: ICT4D today—Enhancing knowledge and people-centred communication for development and poverty reduction. In ICT4D—Connecting People for a Better World: Lessons, Innovations and Perspectives of Information and Communication Technologies in Development; Weigel, G., Waldburger, D., Eds.; Swiss Agency for Development and Cooperation, and the Global Knowledge Partnership: Berne, Switzerland, 2004; pp. 15–42. [Google Scholar]
- Chib, A. The promise and peril of mHealth in developing countries. Mob. Media Commun. 2013, 1, 69–75. [Google Scholar] [CrossRef]
- Akter, S.; Ray, P.; D’Ambra, J. Continuance of mHealth services at the bottom of the pyramid: The roles of service quality and trust. Electron. Mark. 2013, 23, 29–47. [Google Scholar] [CrossRef]
- Sherry, J.M.; Ratzan, S.C. Measurement and evaluation outcomes for mHealth communication: Don’t we have an app for that? J. Health Commun. 2012, 17, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, K.; Duplaga, M.; Ingram, D. Information Technology Solutions for Healthcare; Springer: London, UK, 2006. [Google Scholar]
- Watson, A.H.A. ‘We would have saved her life’: Mobile Telephony in an Island Village in Papua New Guinea. Ejournalist 2010, 10, 106–127. [Google Scholar]
- Watson, A.H.A.; Queensland University of Technology, Brisbane, Australia. The mobile phone: The new communication drum of Papua New Guinea. Unpublished data. 2011. [Google Scholar]
- Kelly, T.; Minges, M. Executive Summary. In Maximising Mobile: Information and Communications for Development; The World Bank: Washington, DC, USA, 2012; pp. 3–7. [Google Scholar]
- Huq, N.L.; Koehlmoos, T.L.P.; Azmi, A.J.; Quaiyum, M.; Mahmud, A.; Hossain, S. Use of mobile phone: Communication barriers in maternal and neonatal emergencies in rural Bangladesh. Int. J. Sociol. Anthropol. 2012, 4, 226–237. [Google Scholar] [CrossRef]
- Chib, A.; Phuong, T.K.; Si, C.W.; Hway, N.S. Enabling informal digital guanxi for rural doctors in Shaanxi, China. Chin. J. Commun. 2013, 6, 62–80. [Google Scholar] [CrossRef]
- Chib, A.; Cheong, Y.J.; Lee, L.C.L.; Ng, C.H.C.; Tan, C.K.; Vlv, K. The Hope of Mobile Phones in Indian Rural Healthcare. J. Health Inform. Dev. Ctries 2012, 6, 406–421. [Google Scholar]
- Chib, A.; Chen, V.H.-H. Midwives with mobiles: A dialectical perspective on gender arising from technology introduction in rural Indonesia. New Media Soc. 2011, 13, 486–501. [Google Scholar] [CrossRef]
- Thaddeus, S.; Maine, D. Too far to walk: Maternal mortality in context. Soc. Sci. Med. 1994, 38, 1091–1110. [Google Scholar] [CrossRef] [PubMed]
- Kirby, B. Too Far to Travel: Maternal Mortality in Milne Bay Province: Beyond the Numbers; unpublished: Port Moresby, Papua New Guinea, 2010. [Google Scholar]
- Gabrysch, S.; Campbell, O. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 2009, 9, e34. [Google Scholar] [CrossRef]
- Stekelenburg, J.; Kyanamina, S.; Mukelabai, M.; Wolffers, I.; van Roosmalen, J. Waiting too long: Low use of maternal health services in Kalabo, Zambia. Trop. Med. Int. Health 2004, 9, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Knight, H.E.; Self, A.; Kennedy, S.H. Why are women dying when they reach hospital on time? A systematic review of the “third delay”. PLOS ONE 2013, 8. [Google Scholar] [CrossRef]
- Kura, S.; Vince, J.; Crouch-Chivers, P. Male Involvement in Sexual and Reproductive Health in the Mendi District, Southern Highlands Province of Papua New Guinea. In Proceedings of the 49th PNG Annual Medical Symposium, Lae, Papua New Guinea, 3 September 2013.
- Reilly, B. State functioning and state failure in the South Pacific. Aust. J. Int. Aff. 2004, 58, 479–493. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watson, A.H.A.; Sabumei, G.; Mola, G.; Iedema, R. Maternal Health Phone Line: Saving Women in Papua New Guinea. J. Pers. Med. 2015, 5, 120-139. https://doi.org/10.3390/jpm5020120
Watson AHA, Sabumei G, Mola G, Iedema R. Maternal Health Phone Line: Saving Women in Papua New Guinea. Journal of Personalized Medicine. 2015; 5(2):120-139. https://doi.org/10.3390/jpm5020120
Chicago/Turabian StyleWatson, Amanda H.A., Gaius Sabumei, Glen Mola, and Rick Iedema. 2015. "Maternal Health Phone Line: Saving Women in Papua New Guinea" Journal of Personalized Medicine 5, no. 2: 120-139. https://doi.org/10.3390/jpm5020120





