Abstract
Health professionals are regarded as important sources of information and guidance for healthy living. Knowing health determinants and risks, and invested with credibility in society, many struggle with their own human limits to apply these principles. A cross-sectional study was conducted among advanced medical students to assess their attitude towards recreational cannabis consumption, intention to use it, and their opinion of its legal status. Secondary objectives were to explore the relation of these primary outcomes to: (a) potentially addictive habits (such as smoking and drinking); (b) individuals’ disturbances in self-organization (DSOs), defined in the ICD-11 as pervasive chronic effects of traumatic experiences or stressful events. An anonymous online questionnaire active in November 2022 collected data from 171 medical students, of which almost 56% were in favor of recreational cannabis legalization. In a logistic regression analysis, each additional point of own consumption intention (on a scale from 1 to 5) was found to increase the odds of a positive opinion of legalization by three times, when controlling for gender, age, smoking, drinking, onset age of smoking, and DSO: OR = 2.918, 95%CI (1.893–4.497). In conclusion, health professionals’ personal beliefs and practices regarding substance use have a significant subjective component.
Keywords:
cannabis; poly-substance use; healthcare professionals; young adults; CUIQ; ITQ; DSO; complex PTSD 1. Introduction
Consumption of recreational cannabis is illegal in Romania and even its medical use is controversial [1,2,3], despite the fact that new policies regarding recreational cannabis are being implemented around the world employing measures that aim for better information rather than punitive actions [2,4,5]. Moreover, prospective studies aimed at advancing the understanding of medical mechanisms and social implications are funded [6,7,8]. On the other hand, there are European countries, such as Romania, where simple possession is punishable with the possibility of imprisonment [2]. Although some medical benefits of cannabinoids are widely accepted [8,9,10,11,12], the negative consequences of tetrahydrocannabinol use and addiction are also acknowledged and include: cognitive impairment [13,14,15,16], predisposition towards developing schizophrenia-related psychosis [15,17,18,19], and mania [15,20]. Regardless of these recognized high risks, the drug’s consumption has been on the rise worldwide since the mid-2000s, in spite of a previous decrease in the 1990s [5,15]. Perceived availability and medical control or simply physicians’ professional stress might be behind medical doctors using cannabis [11,21,22,23]. Young doctors and medical students experience higher levels of stress, are more vulnerable in crises and emergency situations, and are therefore at higher risk of poly-substance consumption, both legal and illegal [21,23,24,25,26].
Recreational use of cannabis is influenced by many factors, such as cigarette smoking, which was linked to both recreational use and cannabis addiction [27]. The two are seen as having a reciprocal causal relationship [28,29,30,31], with smoking paving the way to cannabis consumption, and cannabis leading to tobacco abuse. Risky behavior associated with poly-substance use (such as drinking, smoking, and drug use) has been acknowledged among adolescents [32] and also in older adults [33,34]. Drinking and simultaneous use of cannabis increases health risks and potentiates risky behaviors like driving under the influence [35] and alcohol abuse [36].
Diagnoses of post-traumatic stress disorder (PTSD) and complex post-traumatic stress disorder (CPTSD) have been recently included in the International Classification of Diseases 11th edition (ICD-11) [37]. Disturbances in self-organization (DSOs) are related to CPTSD; they encompass affective dysregulation, negative self-concept, and disturbances in relationships associated with impairment in functioning [37,38,39,40,41,42]. DSOs can be unspecific when separately presented (i.e., rather than a cluster) and are not necessarily associated with the core cluster of PTSD symptoms (namely, re-experiencing the traumatic event in the present, avoidance of traumatic reminders, and a persistent sense of current threat that reflects various forms of arousal) [37,38,39,40,41,42]. DSOs can even overlap with symptoms from other disorders, such as: affective dysregulation and self-concept evaluated at extremes in borderline personality disorder [43,44], guilt and shame in depression [45], or natural and non-pathological processes in unusual contexts [46]. In the ICD-11 taxonomy, DSOs are linked to trauma exposure (or complex trauma) [38,47], which has been suggested to be associated with addictive behaviors [28,48,49], self-medication [50,51], or substance use disorders (SUDs) [52,53,54].
One’s own view on the recreational use of cannabis depends on many factors. Medical students represent a unique demographic with both professional knowledge and possible personal experiences concerning cannabis consumption, which may in turn be reflected in the professional advice and guidance they provide. Young health professionals who used cannabis tended to be better informed about its benefits and also more inclined to be in favor of the legalization of medical cannabis [22,55,56]. In general, people are more likely to have a positive attitude towards recreational cannabis after being exposed to patients’ narratives about medical cannabis and its benefits [57]. Overall, physicians have heterogeneous opinions of the balance of positive effects and potential addiction risks of medical and recreational cannabis and might be influenced by non-medical factors [56,58,59]. In summary, health professionals’ unhealthy attitudes and behaviors, such as substance use, could be a way of coping with their own stress, disturbances and limitations, and could subsequently impact on their professional opinions or decisions.
We conducted a cross-sectional study among medical students in their final stage of the undergraduate program, with the main objective of assessing the attitude towards recreational cannabis consumption, intention to use, opinion of cannabis’s legal status, and potential differences between genders. The secondary objectives were to explore the relation of these primary outcomes to: (a) potentially addictive habits (such as smoking and drinking); and (b) individuals’ disturbances in self-organization (DSOs) due to previous traumatic experiences or stressful events, i.e., as part of coping strategy.
2. Participants and Methods
2.1. Study Design and Participants
An anonymous, voluntary online survey (called CannabisTim) was active in November 2022 to collect the data in two language versions: Romanian (RO) and English (EN). In order to specifically target advanced medical students, the online questionnaire was distributed through the existing database of e-mail addresses of students in their final year and the recipients were requested to recruit only fellow students. Comprehensive information regarding the study aims and instruments was provided to the respondents. The first page of the questionnaire included a declaration of consent, which participants had to accept before filling out the questionnaire, so informed consent was obtained from all subjects involved in the study. The necessary time to answer the full online form was estimated to be 20–30 min. Due to the sensitive information the questionnaire sought, we decided not to send e-mail reminders (no e-mail tracking was carried out). Although it entailed a possible decrease in the response rate, this approach ensured more authenticity of the data. The survey was closed after five consecutive days with no answer.
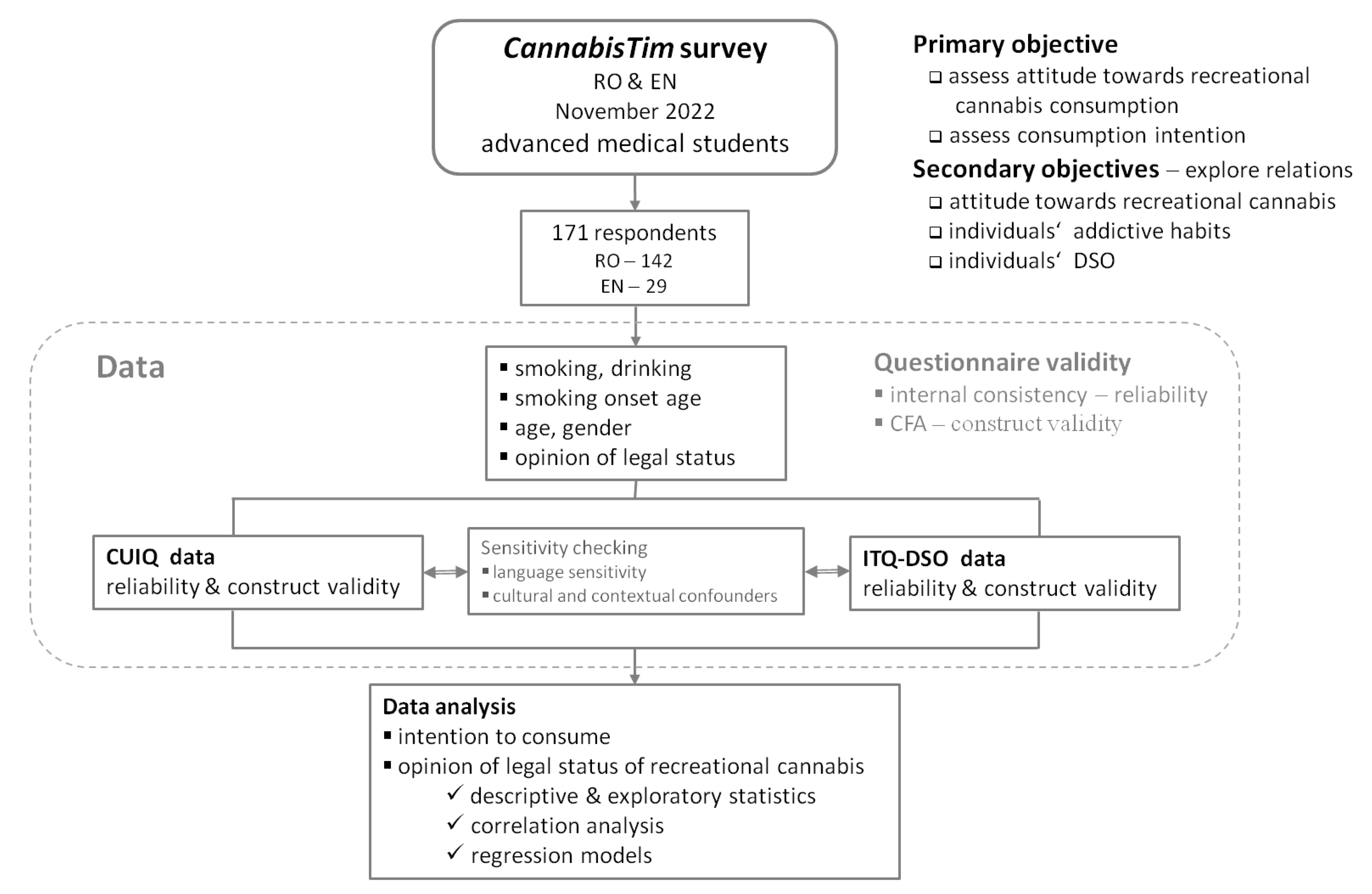
The project’s questionnaire is available in full in the Supplementary Materials. It included: Cannabis Use Intention Questionnaire (CUIQ), International Trauma Questionnaire—DSO (ITQ-DSO), International Trauma Exposure Measure (ITEM), and personal preferences/opinions/habits and socio-demographic questions. Figure 1 presents the study flow diagram, illustrating the distinct investigation stages.
Figure 1.
Study flow diagram. The acronyms stand for: CFA, confirmatory factor analysis; CUIQ, Cannabis Use Intention Questionnaire; ITQ-DSO, International Trauma Questionnaire—Disturbances in Self-Organization.
2.2. Instruments for Data Collection
2.2.1. CUIQ: Cannabis Use Intention Questionnaire
The questionnaire was developed within the CAPPYC European project (https://cappyc.eu/en/; accessed on 8 February 2024). It was built based on the theory of planned behavior and assesses attitude towards cannabis use and intention to use as being influenced by three components: (a) attitude toward the behavior; (b) subjective norm; (c) perceived behavioral control [60]. Specifically for cannabis use, the CUIQ authors developed and validated a questionnaire with four sub-scales: attitudes toward cannabis consumption, subjective norm, self-efficacy to abstinence, and cannabis use intention [60].
CUIQ was created for teenage/adolescent populations and there have been no reported results in educated young adults. We were specifically interested in students at the end, or in the advanced stage, of the undergraduate medical program.
The Romanian version of the questionnaire was validated within the CAPPYC project; an English version developed by the CUIQ authors is also available on the project’s website and we employed both versions.
2.2.2. ITQ-DSO: International Trauma Questionnaire—Disturbances in Self-Organization
The ITQ self-assessment was created to align with the guiding principles of the ICD-11, as outlined by the World Health Organization. Its design aims to optimize clinical usefulness and ensure overall relevance by focusing on the core symptoms of each disorder [40]. The ITQ serves as a valuable tool for screening symptoms of PTSD and complex PTSD (CPTSD) and is accessible to all interested individuals via the following link: https://www.traumameasuresglobal.com/itq (accessed on 8 February 2024). CPTSD encapsulates disturbances in self-organization (DSOs), which focus on healthy self-regulation as a mechanism of adaptation; they encompass the wide-ranging functional impairments and long-term impact of traumatic experiences on educational, relational, vocational, or health problems.
DSOs comprise three domains; they were defined by Dr. Marylene Cloitre [38,40] and were included in the sixth chapter of the ICD-11. They reframe the trauma based on the person’s strengths and long-term surviving efforts: affect dysregulation, negative self-concept, and disturbances in relationships (https://www.complextrauma.org; accessed on 8 February 2024).
As there had been no reports of ITQ applied in the Romanian population, the procedure of translation followed by back-translation was applied to ensure the accuracy of the underlying meaning and equivalency in possible interpretations for RO and EN versions of the survey.
2.2.3. ITEM: International Trauma Exposure Measure
In addition to collecting DSO data, the CannabisTim survey included the International Trauma Exposure Measure (ITEM), a checklist designed to capture traumatic life events and their associated characteristics consistent with the definition of a traumatic event in the ICD-11. The ITEM questionnaire evaluates exposure to potentially traumatic life events throughout various developmental stages (childhood, adolescence, and adulthood), the frequency of exposure to the most distressing traumatic event, and the primary emotion linked to that event. While ITEM gathers qualitative information that could support the interpretation of DSO data, such an investigation was not pursued in the present quantitative analysis.
ITEM is accessible to the research and clinical communities without requiring prior authorization via the following link: https://www.traumameasuresglobal.com/item (accessed on 8 February 2024). For this project, the same translation and adaptation procedure was applied to ITEM as that used for the ITQ.
2.3. Data Analysis
2.3.1. Questionnaire Validity
Internal consistency was assessed based on Cronbach’s alpha (the value was calculated for the entire scales and for each sub-scale corresponding to the latent variables reported by the scales’ developers). Values of Cronbach’s alpha greater than 0.8 were considered to indicate good internal consistency, but smaller actual values entailed no consequences on possible discharge of scales or sub-scales. Reported values for some original CUIQ sub-scales were smaller than 0.8 [60].
Regarding the construct validity of each questionnaire or scale, confirmatory factor analysis (CFA) was conducted to verify the structural models initially presented by the developers. The goodness of fit indices for the CFA models and their respective [threshold values] were as follows: the model chi-square test and resultant p-value [<0.05]; comparative fit index (CFI) [>0.90]; root mean square error of approximation (RMSEA) [<0.1]; standardized root mean square residual (SRMR) [<0.08] [61,62].
Both CUIQ and ITQ-DSO have been reported to have unidimensional and second-order models [40,60,63]. In the current construct validation process, all reported models were taken into account and subsequently compared based on their fit statistics and the Akaike information criterion (AIC). To assess the statistical significance of changes in AIC values and select the simplest model, Vuong’s closeness test, based on likelihood ratio, was employed.
To ensure the consistency of multiple comparisons across the questionnaires or their sub-scales, min–max scaling in the [0, 1] range was further carried out. When applied, this re-scaling is explicitly reported in the results.
2.3.2. Statistical Analysis
Descriptive statistics encompassed the observed frequency counts and percentages for categorical variables and the sample’s mean and standard deviation (SD) for numerical variables, regardless of their distribution. The normality of numerical variables was assessed using the Kolmogorov–Smirnov statistical test. Additionally, for certain scale scores treated as rank variables, the median (interquartile range) with Tukey’s hinges was provided.
Univariate non-parametric statistical tests were utilized to compare the distribution of numerical data across two or multiple groups, as appropriate (employing either the Mann–Whitney U or Kruskal–Wallis test, respectively). The chi-square statistical test (either asymptotic or Monte Carlo simulation with 10,000 samples) was employed to evaluate the statistical significance of associations between categorical variables.
Covariance between various scale scores was explored using two-by-two non-parametric Spearman correlation. This analysis was also utilized to scrutinize and confirm the hypothesized convergent and discriminant validity of the questionnaires or scales in the surveyed population, mirroring the approach of the original questionnaires.
To quantify the contribution of individuals’ habits, preferences, and vulnerabilities to one’s view on legalization of recreational cannabis, a multivariable logistic regression model was applied; the strength of predictors’ contribution to the opinion was quantified based on odds ratio (OR) values.
The statistical analysis was conducted at a 95% level of confidence and 5% level of statistical significance, except for CFA (when other values are explicitly specified). All reported probability values were two-tailed.
Data analysis was performed with the statistical software IBM SPSS v. 20 and R v. 4.0.5 packages (including “lavaan” v. 0.6–11 and “nonnest2” v. 0.5–5).
3. Results
3.1. Study Participants, Descriptive Statistics
Answers were collected from 171 medical students: 142 RO respondents + 29 EN respondents. The target groups were approximately 600 RO + 180 EN, so the rates of response were estimated to be 23.67% and 16.1% for the RO and EN groups, respectively. Table 1 presents the descriptive statistics for the respondents’ characteristics. The two groups were similar, except for their age distribution and declared drinking habits. The full dataset of 171 records was considered in further analysis to meet the study objectives.

Table 1.
Study participants: descriptive and exploratory statistics.
Smoking and drinking were strongly and significantly correlated (i.e., a Spearman R-coefficient close to 0.75). Although the relation of these habits (namely, smoking and drinking) with an early onset of smoking was more than twice as weak, they both were significantly correlated with early smoking onset.
More than half of respondents were of the opinion that recreational cannabis should be legalized on similar terms to alcohol and tobacco.
3.2. CUIQ Scale Validity
The analysis was conducted for all 171 respondents and separately for the 142 respondents of the RO data subset (these latter results are presented in the Supplementary Materials, Table S1a,b). The results were equivalent, confirming the full dataset’s consistency, with no indication of cultural confounders.
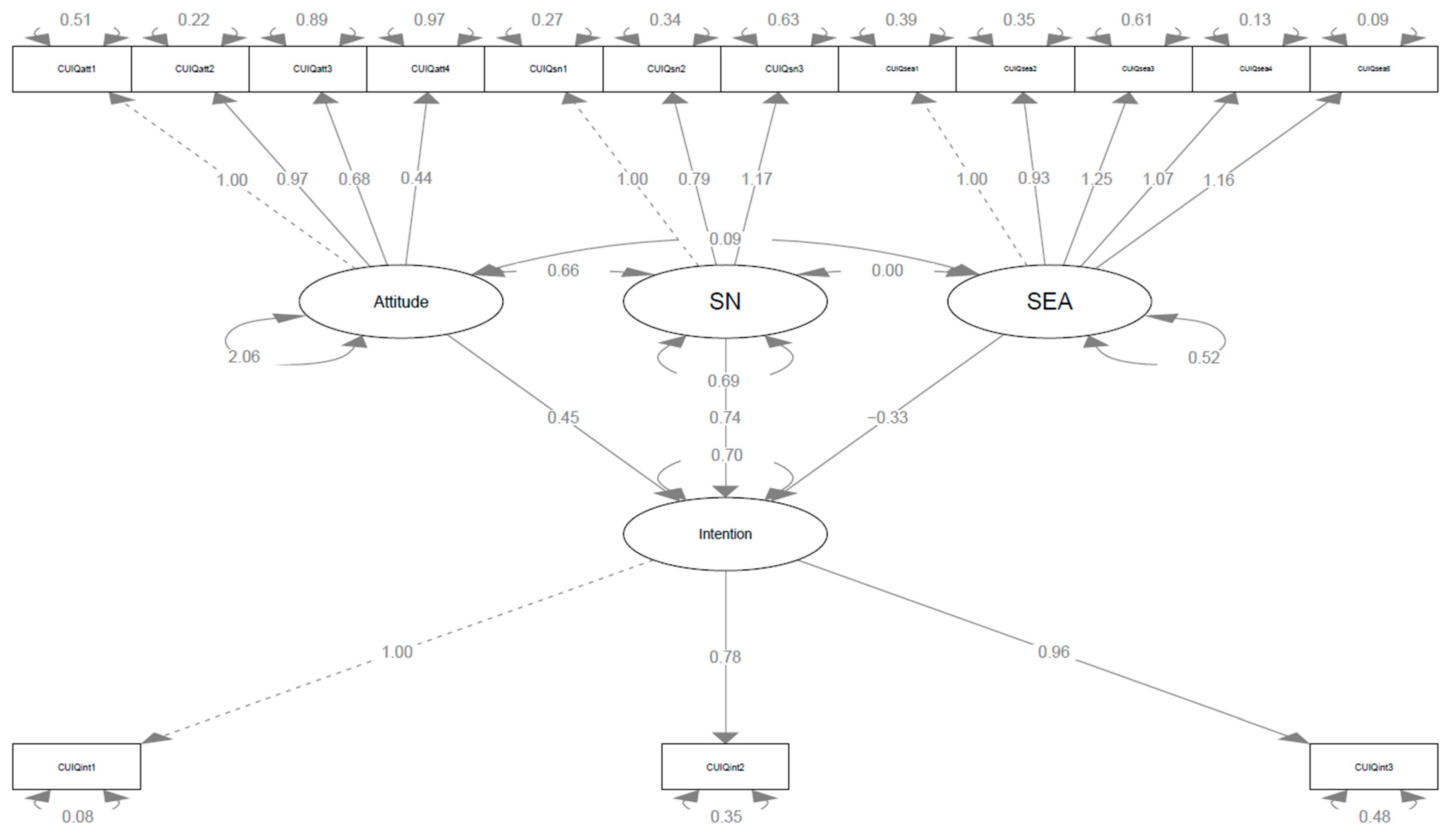
Table 2 shows the good internal consistency of the CUIQ scale for the dataset and Table 3 presents the CFA based on four latent factors: attitude, subjective norm (SN), self-efficacy to abstinence (SEA), and intention. Figure 2 presents the path diagram of this model; the underlying factor structure of the theoretical model proposed by the CUIQ developers to assess the intention of cannabis use was confirmed. The complete 171-record dataset was considered in subsequent analysis (see the diagram in Figure 1).

Table 2.
Internal consistency of CUIQ and CUIQ sub-scales (N = 171 data observations).

Table 3.
Confirmatory factor analysis (CFA) analysis for CUIQ scale based on the four factors originally identified: attitudes, subjective norm (SN), self-efficacy to abstinence (SEA), intention. (N = 171 data observations).
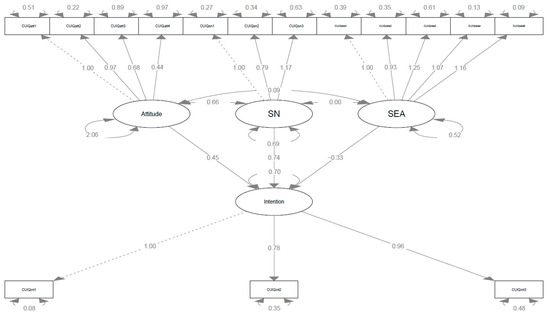
Figure 2.
Second-order four-factor CFA model for the CUIQ scale (N = 171). Latent variables (factors) are in ovals and manifest variables (indicators) are in rectangles. Arrows from each factor to corresponding indicators show the factor loadings with the first indicator’s loading set to 1 (reference by default). Arrows from the factors defined as predictors of intention to use in the CUIQ model (i.e., attitude, SN, and SEA) show the regression coefficients. Double arrows within and between factors indicate the residual variance and covariance, respectively. The values relevant to the present investigation are explicitly shown in Table 3. Abbreviations: CFA, confirmatory factor analysis; SEA, self-efficacy to abstinence; SN, subjective norm.
The covariance of the CUIQ model’s latent variables (factors) showed that attitude and SN were significantly interdependent, and they both significantly contributed to the intention to use (regressions in Table 3). SEA showed a highly significant negative contribution to the intention to use (regressions in Table 3); on the other hand, there seems to be no relation between SEA and SN or attitude (covariances in Table 3).
For each sub-scale, the scores were further rescaled over the range [0, 1]. Table 4 shows the CUIQ descriptive statistics for the 171 respondents, according to the three reported genders. There were no differences except for SEA, for which the female respondents outperformed the other two gender groups. Consistently, the declared intention to consumption was higher among these latter respondents, but the small difference between genders did not reach statistical significance.

Table 4.
CUIQ descriptive statistics across the three genders (for each variable, scores were rescaled in the range [0, 1]).
3.3. DSO Scale Validity
Similarly to CUIQ, the DSO scale validation was conducted for all 171 respondents and for the RO subset of data (these subset’s results are presented in the Supplementary Materials, Table S2a,b). The results were equivalent, confirming the complete DSO dataset’s consistency, therefore the complete 171-record dataset was considered in subsequent analysis, as shown in Figure 1.
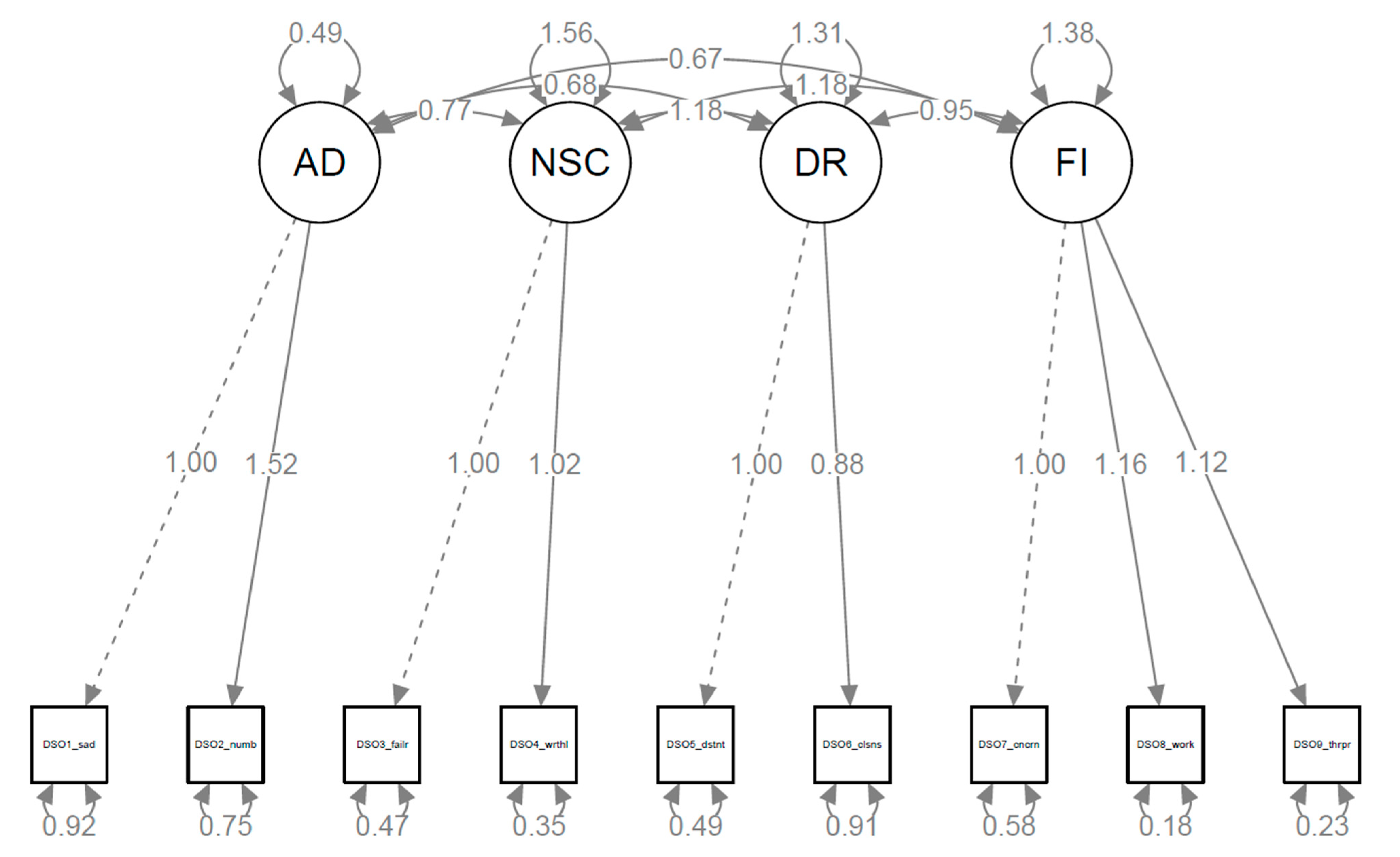
Table 5 shows the internal consistency of DSO data and Table 6 presents the CFA based on a first-order model and four latent factors: affect dysregulation (AD), negative self-concept (NSC), disturbances in relationships (DR), functional impairment (FI). Figure 3 presents the path diagram of this model. A second-order model was also tested, but it showed no significant improvement compared to this first-order model (decision based on Vuong’s test, p-value = 0.5). All covariance coefficients were highly significant (covariances in Table 6).

Table 5.
Internal consistency of DSO and DSO sub-scales (N = 171 data observations).

Table 6.
Confirmatory factor analysis (CFA) analysis for DSO scale based on the four factors originally identified: affect dysregulation (AD), negative self-concept (NSC), disturbances in relationships (DR), functional impairment (FI). (N = 171 data observations).
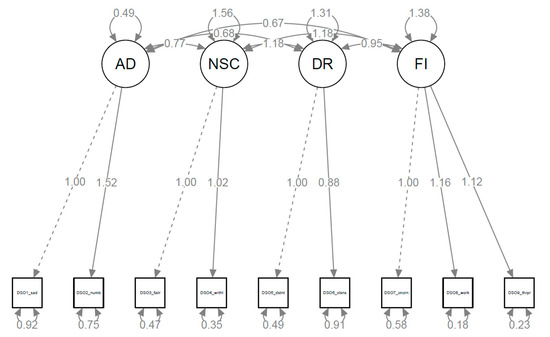
Figure 3.
First-order four-factor CFA model for DSO scale (N = 171). Latent variables (factors) are in ovals and manifest variables (indicators) are in squares. Arrows from each factor to corresponding indicators show the factor loadings with the first indicator’s loading set to 1 (reference by default). Double arrows within and between factors indicate the residual variance and covariance, respectively. The values relevant to the present investigation are explicitly shown in Table 6. Abbreviations: AD, affect dysregulation; CFA, confirmatory factor analysis; DR, disturbances in relationships; FI, functional impairment; NSC, negative self-concept.
For each latent variable (factor), the scores were further rescaled over the range [0, 1]. Table 7 shows the descriptive statistics for each DSO-related variable among the 171 respondents, according to the three genders. For all four disturbances, the male respondents were less affected compared to the other two genders, but the DR differences were only marginally significant.

Table 7.
DSO descriptive statistics across the three genders (for each variable, scores were rescaled in the range [0, 1]).
The ITEM questionnaire did not reveal any significant traumatic event among the 171 respondents and did not contribute to interpretation of the quantitative analysis.
3.4. Perspective and Opinion of Legal Status of Recreational Cannabis
The relationship between intention to use recreational cannabis and potentially addictive habits related to consumption of legal substances (such as tobacco or alcohol) was further investigated. Additionally, the relationship to individuals’ DSO-Intention was explored.
Table 8 synthesizes the results of two-by-two Spearman correlation analysis. The correlation of consumption intention with age (over the limited range of participants’ age), DSO-DR, and DSO-FI was weak and insignificant.

Table 8.
Two-by-two Spearman correlation between the CUIQ-Intention and participants’ age, habits (namely, smoking, drinking, and early smoking onset), and the DSO scores (N = 171 data observations).
On the other hand, weak but highly significant correlation was found with the habits (namely smoking, drinking alcohol, and early onset of smoking), DSO-AD, and DSO-NSC.
Moreover, when asked about their opinion of legalizing the consumption of recreational cannabis, 56% of the medical students stated it should be legalized on similar terms to alcohol and tobacco (see Table 1).
Table 9 presents the results of the logistic regression analysis, with respondents’ own intention to consume cannabis in recreational settings as an independent predictor in the regression model. When controlling for gender, age, smoking, drinking alcohol, early smoking onset, DSO-AD, DSO-NSC, DSO-DR, DSO-FI, and group (RO or EN), each additional point of intention on a scale from 1 to 5 increases the chance of a positive opinion of the legalization by almost three times: OR = 2.918, 95%CI (1.893–4.497). Although the model explains less than 40% of the opinion of the legal status of cannabis (Nagelkerke R-square = 0.368), the medical students’ own intention to consume proved to be a significant predictor.

Table 9.
Logistic regression model of opinion of legalization of recreational cannabis as predicted by respondent’s intention to use (N = 171 data observations). CUIQ-Intention is a rank variable with values between 1 and 5. Exp (B) is equivalent to the odds ratio (OR), a measure of a relationship’s strength between the predictor and the binary outcome.
4. Discussion
This anonymous survey examined advanced medical students’ attitudes toward recreational cannabis, intention to consume, and opinion of its legal status. All these were investigated in relation to smoking and drinking habits, and also possible connections with disturbances in self-organization were sought. For collecting these data, the study questionnaire employed the CUIQ and ITQ-DSO scales, used for the first time in this particular population. CFA confirmed their construct validity. Female respondents were more vulnerable to DSO but more efficient in their abstinence regarding the cannabis consumption. Such variables as drinking, smoking, and DSO were found to be correlated with intention to use recreational cannabis. All significant correlations were weak to moderate, thus suggesting a high degree of variability among respondents; to account for this variability, these variables were included as controlling factors in the logistic regression model. Intention to consume cannabis proved to be a significant independent predictor for the opinion of the legal status of recreational cannabis, but intention did not differ between the genders.
Cannabis consumption is controversial and implies several risks even when used for medical reasons, mostly because there is no scientifically robust evidence base compared to other pharmaco-therapies employed as treatments [64]. The political factors linked to cannabis’s legal status are also controversial; while some countries decided that legalization would be rather beneficial, some are still reserved (Romania included). Public health policies and programs are driven by the societal perception of risk [65,66], but there is a steady increase in recreational cannabis use in spite of the growing evidence of risks [67,68,69]. Although data are still scarce on this topic, some articles have tried to address the sensitive issue of drug use among medical doctors [11,21,22,70]. Cannabis consumption among young medical doctors and students is acknowledged to be higher compared to older professionals [21,23,24,25,26,71]. Stress is an important factor for cannabis use [72] and some medical specialties might be prone to chronic stress and burnout; in addition, certain situations (like the recent challenges of the COVID-19 pandemic) in already vulnerable groups could simply tilt the delicate balance in the wrong direction [23,25,73]. The medical knowledge that comes with medical education does not seem to deter the use of recreational cannabis or cannabis in general. The significant connection between thoughts that recreational cannabis should be legalized and one’s intention to use appears to support the previous literature findings that medical education is not in all circumstances sufficiently protective.
In this context, the time frame of our study after the COVID-19 pandemic is of particular importance: the participants were already enrolled in the undergraduate medical program during the pandemic, when emotional effects of isolation, professional confusion, and perceived danger augmented existing vulnerabilities and decreased their mental health resilience [25,74]. Additionally, the increase in cannabis use among adults was linked to pandemic-related measures and effects, such as self-isolation or feelings of boredom, depression, and anxiety [75,76]. At early stages of a professional career, keeping a sustainable balance between sound knowledge and evidence-based practice on the one hand and aspiration for novelty and progress on the other hand takes its toll on the mental health resilience of young healthcare professionals and medical schools should address this issue [56]. Our study brings novel data on current attitudes and opinions of advanced medical students, with subsequent effects on their effectiveness as healthy lifestyle promoters.
PTSD or CPTSD combined with SUD as a comorbidity is often encountered [52,53,54,77,78]. The burden of this association is high and decreases the efficacy of SUD treatment; clinical presentations are often accompanied by additional risks like suicidality and impaired functioning [79,80] or multiple vulnerability factors [81,82]. Female populations are more likely to develop PTSD after trauma exposure [83,84], while male populations more often seek help for SUD [85,86,87]. Growing evidence shows the need for tailored approaches to women [88,89]. It is probable that societal cultures with higher acceptability of substance use in men rather than women have an additionally protective influence for women against SUD, but gender equity and career challenges put increasing pressure on women, as well [89,90]. In line with previous reports, our study also found women as more vulnerable to DSO but more efficient in their abstinence from cannabis consumption.
We investigated advanced medical students who were professionally functional and accomplished, so our research design avoided any biased train of thought such as trauma exposure—PTSD—SUD. Our questionnaire included only the DSO section of ITQ, namely the more subtle criteria for CPTSD in the ICD-11. Although the DSO cluster of symptoms is also found in other mental disorders such as borderline personality disorder, depression, anxiety, and others, the exposure to trauma was not explicitly stated.
Addictive behaviors may be interconnected and can influence each other. Cannabis was considered a gateway to stronger and more dangerous drugs but this view has been challenged [91,92]; exposure to alcohol and tobacco have also been reported in a two-way relationship [27,28,29,30,31,32,33,34]. The preventive measures for SUD are similar to those aimed at early exposure to trauma, encompassing multiple socio-economic factors.
In the medical profession, exposure to stress in the workplace is high and an adaptive trajectory should be cultivated in the educational process. Some degree of stress can be beneficial and resilience to stress generates healthy adaptation and builds future resilience, but exposure to traumatic experiences creates vulnerability and decreases professional effectiveness. On the other hand, motivations, causes, and consequences of cannabis use should be regarded in their social and cultural contexts. Actors such as peers, family, and media may shape medical students’ views and intention of cannabis consumption in recreational contexts, with subsequent opinions and professional advice.
Limitations
Firstly, this study collected anonymous self-reported data, with no objective confirmation and no control of respondents’ background. The relatively wide variation in declared age (i.e., over a five-year range) might also entail variation in level of education. This shortcoming would combine with the common method bias, leading to spurious associations on the one hand and underestimated effect sizes on the other hand. The survey questionnaire was designed to limit the shared variance and to control the method biases by alternating the scale and factual questions. Comprehensive professional information regarding the study aims and the scales employed for data collection was also provided throughout the questionnaire in order to gain the participants’ trust and professional commitment. In addition, the medical students initially contacted were requested to further share the survey only with their peers.
Secondly, the questionnaire was distributed in two language versions (namely RO and EN). Although we made every effort to ensure the data validity and consistency across the entire dataset, we acknowledge that most of the EN answers came from international students; respondents’ various cultural and religious inheritances might have generated imbalance in both gender distribution and self-reported habits (such as drinking). Therefore, the correlations including drinking habits might have been underestimated as a consequence of such confounding factors.
Thirdly, the ITQ-DSO sub-scale of affect dysregulation had a moderate internal consistency (Cronbach’s alpha = 0.622), which would imply some uncertainty with subsequent effects of diminishing the correlation size and loss in statistical significance. This effect would especially impact the weakly correlated factors with spurious confounders.
Fourthly, the cross-sectional design brings inherent limitations concerning any causal inference. The logistic regression model we applied to formalize the relationship between the intention to consume and opinion on legal status of recreational cannabis employed marginal rather than model-free estimands. However, our results would provide useful background for future longitudinal multivariate analyses regarding recreational cannabis consumption and disturbances in self-organization among medical professionals. The effect sizes we identified in our exploratory analysis are valuable data for controlling the statistical power in future longitudinal studies.
5. Conclusions
Half of advanced medical students thought recreational cannabis should be legalized in a similar manner to tobacco and alcohol. There were no gender differences in respondents’ own intention to use cannabis.
Our investigation substantiated the evidence for the hypothesized relationship of medical students’ views on the legal status of cannabis consumption as being dependent on their own intention to use, which in turn was found to be associated with their own vulnerabilities. Prevention policies and health promotion programs should acknowledge these possible vulnerabilities of health professionals involved in such programs, while medical education and residency training should actively target them.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/soc14040052/s1, Supplement S1: CannabisTim questionnaire (PDF file); Supplement S2: Tables S1–S3 (PDF file).
Author Contributions
Conceptualization, A.-L.P., S.C.T. and D.L.; methodology, A.-L.P., S.C.T. and D.L.; software, L.M.-B., B.M., M.G.M. and D.L.; validation, A.-L.P., S.C.T., L.M.-B., B.M., M.G.M., C.C.V., A.P. and D.L.; formal analysis, A.-L.P. and D.L.; data curation, L.M.-B., B.M. and M.G.M.; writing—original draft preparation, A.-L.P., S.C.T. and D.L.; writing—review and editing, A.-L.P., S.C.T., C.C.V., A.P. and D.L.; supervision, D.L.; project administration, D.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee for Scientific Research of Victor Babes University of Medicine and Pharmacy, Timisoara, Romania (ID code 50; 21 October 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on “figshare” under CC BY 4.0 license: https://figshare.com/articles/dataset/CannabisTim-Nov2022/23703780. (DOI 10.6084/m9.figshare.23703780.v1).
Acknowledgments
We express our gratitude to Silvia Loica-Mersa of Stanford University School of Medicine for her most kind support in translating the ITQ and ITEM questionnaires and further valuable recommendations. We also gratefully acknowledge the openness and support of survey respondents. The publication costs were supported by “Victor Babes” University of Medicine and Pharmacy, Timisoara.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CFA | Confirmatory Factor Analysis |
| CPTSD | Complex Post-Traumatic Stress Disorder |
| CUIQ | Cannabis Use Intention Questionnaire |
| DSOs | Disturbances in Self-Organization |
| ICD-11 | International Classification of Diseases 11th Revision |
| ITEM | International Trauma Exposure Measure |
| ITQ | International Trauma Questionnaire |
| PTSD | Post-Traumatic Stress Disorder |
| SUD | Substance Use Disorder |
References
- Iovu, M.-B.; Breaz, M.A. The Prevalence and Burden of Mental and Substance Use Disorders in Romania: Findings from the Global Burden of Disease Study 2016. Psychiatr. Danub. 2019, 31, 457–464. [Google Scholar] [CrossRef] [PubMed]
- EMCDDA Penalties for Drug Law Offences in Europe at a Glance. Available online: https://www.emcdda.europa.eu/publications/topic-overviews/content/drug-law-penalties-at-a-glance_en (accessed on 17 July 2023).
- BBC News Teenage Cannabis Use Rises in Europe—EU Espad Survey. Available online: https://www.bbc.com/news/world-europe-37419072 (accessed on 25 July 2023).
- Englund, A.; Freeman, T.P.; Murray, R.M.; McGuire, P. Can We Make Cannabis Safer? Lancet Psychiatry 2017, 4, 643–648. [Google Scholar] [CrossRef]
- EMCDDA European Drug Report 2023: Trends and Developments. Available online: https://www.emcdda.europa.eu/publications/european-drug-report/2023_en (accessed on 17 July 2023).
- Harris, S. Largest Ever Study into the Effects of Cannabis on the Brain. Medscape UK 2022. Available online: https://www.medscape.co.uk/viewarticle/largest-ever-study-effects-cannabis-brain-2022a10022e1 (accessed on 8 February 2024).
- Hines, L.A.; Jones, H.J.; Hickman, M.; Lynskey, M.; Howe, L.D.; Zammit, S.; Heron, J. Adverse Childhood Experiences and Adolescent Cannabis Use Trajectories: Findings from a Longitudinal UK Birth Cohort. Lancet Public Health 2023, 8, e442–e452. [Google Scholar] [CrossRef] [PubMed]
- Gräfe, E.L.; Reid, H.M.O.; Shkolnikov, I.; Conway, K.; Kit, A.; Acosta, C.; Christie, B.R. Women Are Taking the Hit: Examining the Unique Consequences of Cannabis Use across the Female Lifespan. Front. Neuroendocr. 2023, 70, 101076. [Google Scholar] [CrossRef]
- Whiting, P.F.; Wolff, R.F.; Deshpande, S.; Di Nisio, M.; Duffy, S.; Hernandez, A.V.; Keurentjes, J.C.; Lang, S.; Misso, K.; Ryder, S.; et al. Cannabinoids for Medical Use. JAMA 2015, 313, 2456–2473. [Google Scholar] [CrossRef]
- Bedard-Gilligan, M.; Lehinger, E.; Cornell-Maier, S.; Holloway, A.; Zoellner, L. Effects of Cannabis on PTSD Recovery: Review of the Literature and Clinical Insights. Curr. Addict. Rep. 2022, 9, 203–216. [Google Scholar] [CrossRef]
- Weisman, J.M.; Rodríguez, M. A Systematic Review of Medical Students’ and Professionals’ Attitudes and Knowledge Regarding Medical Cannabis. J. Cannabis Res. 2021, 3, 47. [Google Scholar] [CrossRef] [PubMed]
- Hill, K.P. Medical Marijuana for Treatment of Chronic Pain and Other Medical and Psychiatric Problems. JAMA 2015, 313, 2474–2483. [Google Scholar] [CrossRef]
- Figueiredo, P.R.; Tolomeo, S.; Steele, J.D.; Baldacchino, A. Neurocognitive Consequences of Chronic Cannabis Use: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2020, 108, 358–369. [Google Scholar] [CrossRef]
- Grant, I.; Gonzalez, R.; Carey, C.L.; Natarajan, L.; Wolfson, T. Non-Acute (Residual) Neurocognitive Effects of Cannabis Use: A Meta-Analytic Study. J. Int. Neuropsychol. Soc. 2003, 9, 679–689. [Google Scholar] [CrossRef]
- Campeny, E.; López-Pelayo, H.; Nutt, D.; Blithikioti, C.; Oliveras, C.; Nuño, L.; Maldonado, R.; Florez, G.; Arias, F.; Fernández-Artamendi, S.; et al. The Blind Men and the Elephant: Systematic Review of Systematic Reviews of Cannabis Use Related Health Harms. Eur. Neuropsychopharmacol. 2020, 33, 1–35. [Google Scholar] [CrossRef] [PubMed]
- Sultan, R.S.; Zhang, A.W.; Olfson, M.; Kwizera, M.H.; Levin, F.R. Nondisordered Cannabis Use Among US Adolescents. JAMA Netw. Open 2023, 6, e2311294. [Google Scholar] [CrossRef] [PubMed]
- Van Os, J.; Linscott, R.J.; Myin-Germeys, I.; Delespaul, P.; Krabbendam, L. A Systematic Review and Meta-Analysis of the Psychosis Continuum: Evidence for a Psychosis Proneness–Persistence–Impairment Model of Psychotic Disorder. Psychol. Med. 2009, 39, 179–195. [Google Scholar] [CrossRef]
- Large, M.; Sharma, S.; Compton, M.T.; Slade, T.; Nielssen, O. Cannabis Use and Earlier Onset of Psychosis. Arch. Gen. Psychiatry 2011, 68, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Smit, F.; Bolier, L.; Cuijpers, P. Cannabis Use and the Risk of Later Schizophrenia: A Review. Addiction 2004, 99, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, M.; Winsper, C.; Marwaha, S.; Gilbert, E.; Broome, M.; Singh, S.P. Cannabis Use and Mania Symptoms: A Systematic Review and Meta-Analysis. J Affect Disord 2015, 171, 39–47. [Google Scholar] [CrossRef]
- Naillon, P.-L.; Flaudias, V.; Brousse, G.; Laporte, C.; Baker, J.S.; Brusseau, V.; Comptour, A.; Zak, M.; Bouillon-Minois, J.-B.; Dutheil, F. Cannabis Use in Physicians: A Systematic Review and Meta-Analysis. Medicines 2023, 10, 29. [Google Scholar] [CrossRef]
- Papazisis, G.; Siafis, S.; Tsakiridis, I.; Koulas, I.; Dagklis, T.; Kouvelas, D. Prevalence of Cannabis Use Among Medical Students: A Systematic Review and Meta-Analysis. Subst. Abus. Res. Treat. 2018, 12, 117822181880597. [Google Scholar] [CrossRef]
- Dutheil, F.; Aubert, C.; Pereira, B.; Dambrun, M.; Moustafa, F.; Mermillod, M.; Baker, J.S.; Trousselard, M.; Lesage, F.-X.; Navel, V. Suicide among Physicians and Health-Care Workers: A Systematic Review and Meta-Analysis. PLoS ONE 2019, 14, e0226361. [Google Scholar] [CrossRef]
- Tyssen, R.; Vaglum, P. Mental Health Problems among Young Doctors: An Updated Review of Prospective Studies. Harv. Rev. Psychiatry 2002, 10, 154–165. [Google Scholar] [CrossRef]
- Bredicean, C.; Tamasan, S.C.; Lungeanu, D.; Giurgi-Oncu, C.; Stoica, I.-P.; Panfil, A.-L.; Vasilian, C.; Secosan, I.; Ursoniu, S.; Patrascu, R. Burnout Toll on Empathy Would Mediate the Missing Professional Support in the COVID-19 Outbreak. Risk Manag. Healthc. Policy 2021, 14, 2231–2244. [Google Scholar] [CrossRef] [PubMed]
- Murkar, A.; Kendzerska, T.; Shlik, J.; Quilty, L.; Saad, M.; Robillard, R. Increased Cannabis Intake during the COVID-19 Pandemic Is Associated with Worsening of Depression Symptoms in People with PTSD. BMC Psychiatry 2022, 22, 554. [Google Scholar] [CrossRef] [PubMed]
- Hindocha, C.; Shaban, N.D.C.; Freeman, T.P.; Das, R.K.; Gale, G.; Schafer, G.; Falconer, C.J.; Morgan, C.J.A.; Curran, H.V. Associations between Cigarette Smoking and Cannabis Dependence: A Longitudinal Study of Young Cannabis Users in the United Kingdom. Drug Alcohol. Depend. 2015, 148, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Badiani, A.; Boden, J.M.; De Pirro, S.; Fergusson, D.M.; Horwood, L.J.; Harold, G.T. Tobacco Smoking and Cannabis Use in a Longitudinal Birth Cohort: Evidence of Reciprocal Causal Relationships. Drug Alcohol. Depend. 2015, 150, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Cohn, A.M.; Elmasry, H. First Use of Cannabis Compared to First Use of Alcohol and Tobacco: Associations with Single and Poly-Substance Use Behavior. Drug Alcohol. Depend. 2023, 248, 109904. [Google Scholar] [CrossRef] [PubMed]
- Midanik, L.T.; Tam, T.W.; Weisner, C. Concurrent and Simultaneous Drug and Alcohol Use: Results of the 2000 National Alcohol Survey. Drug Alcohol. Depend. 2007, 90, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Levy, S.; Brogna, M.; Minegishi, M.; Subramaniam, G.; McCormack, J.; Kline, M.; Menzin, E.; Allende-Richter, S.; Fuller, A.; Lewis, M.; et al. Assessment of Screening Tools to Identify Substance Use Disorders Among Adolescents. JAMA Netw. Open 2023, 6, e2314422. [Google Scholar] [CrossRef] [PubMed]
- Faeh, D.; Viswanathan, B.; Chiolero, A.; Warren, W.; Bovet, P. Clustering of Smoking, Alcohol Drinking and Cannabis Use in Adolescents in a Rapidly Developing Country. BMC Public Health 2006, 6, 169. [Google Scholar] [CrossRef]
- Al-Rousan, T.; Moore, A.A.; Han, B.H.; Ko, R.; Palamar, J.J. Trends in Binge Drinking Prevalence among Older U.S. Men and Women, 2015 to 2019. J. Am. Geriatr. Soc. 2022, 70, 812–819. [Google Scholar] [CrossRef]
- Kepner, W.E.; Han, B.H.; Nguyen, D.; Han, S.S.; Lopez, F.A.; Palamar, J.J. Past-Month Binge Drinking and Cannabis Use among Middle-Aged and Older Adults in the United States, 2015–2019. Alcohol 2023, 107, 32–37. [Google Scholar] [CrossRef]
- Terry-McElrath, Y.M.; O’Malley, P.M.; Johnston, L.D. Alcohol and Marijuana Use Patterns Associated With Unsafe Driving Among U.S. High School Seniors: High Use Frequency, Concurrent Use, and Simultaneous Use. J. Stud. Alcohol. Drugs 2014, 75, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Stinson, F.S.; Ruan, W.J.; Pickering, R.; Grant, B.F. Cannabis Use Disorders in the USA: Prevalence, Correlates and Co-Morbidity. Psychol. Med. 2006, 36, 1447–1460. [Google Scholar] [CrossRef] [PubMed]
- WHO International Classification of Diseases 11th Revision. The Global Standard for Diagnostic Health Information. Available online: https://icd.who.int/en (accessed on 17 July 2023).
- Cloitre, M. ICD-11 Complex Post-Traumatic Stress Disorder: Simplifying Diagnosis in Trauma Populations. Br. J. Psychiatry 2020, 216, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Kazlauskas, E.; Zelviene, P.; Daniunaite, I.; Hyland, P.; Kvedaraite, M.; Shevlin, M.; Cloitre, M. The Structure of ICD-11 PTSD and Complex PTSD in Adolescents Exposed to Potentially Traumatic Experiences. J. Affect. Disord. 2020, 265, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Cloitre, M.; Shevlin, M.; Brewin, C.R.; Bisson, J.I.; Roberts, N.P.; Maercker, A.; Karatzias, T.; Hyland, P. The International Trauma Questionnaire: Development of a Self-Report Measure of ICD-11 PTSD and Complex PTSD. Acta Psychiatr. Scand. 2018, 138, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Redican, E.; Nolan, E.; Hyland, P.; Cloitre, M.; McBride, O.; Karatzias, T.; Murphy, J.; Shevlin, M. A Systematic Literature Review of Factor Analytic and Mixture Models of ICD-11 PTSD and CPTSD Using the International Trauma Questionnaire. J. Anxiety Disord. 2021, 79, 102381. [Google Scholar] [CrossRef] [PubMed]
- Spinazzola, J.; Wilson, K.M.; Pressley, J. The Foundation Trust Complex Trauma: What Is It and How Does It Affect People? Available online: https://www.complextrauma.org/complex-trauma/complex-trauma-what-is-it-and-how-does-it-affect-people/ (accessed on 17 July 2023).
- Daros, A.R.; Williams, G.E. A Meta-Analysis and Systematic Review of Emotion-Regulation Strategies in Borderline Personality Disorder. Harv. Rev. Psychiatry 2019, 27, 217–232. [Google Scholar] [CrossRef] [PubMed]
- Vater, A.; Schröder-Abé, M.; Weißgerber, S.; Roepke, S.; Schütz, A. Self-Concept Structure and Borderline Personality Disorder: Evidence for Negative Compartmentalization. J. Behav. Ther. Exp. Psychiatry 2015, 46, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Thibodeau, R.; Jorgensen, R.S. Shame, Guilt, and Depressive Symptoms: A Meta-Analytic Review. Psychol. Bull. 2011, 137, 68–96. [Google Scholar] [CrossRef]
- Nickerson, A.; Bryant, R.A.; Schnyder, U.; Schick, M.; Mueller, J.; Morina, N. Emotion Dysregulation Mediates the Relationship between Trauma Exposure, Post-Migration Living Difficulties and Psychological Outcomes in Traumatized Refugees. J. Affect. Disord. 2015, 173, 185–192. [Google Scholar] [CrossRef]
- Cloitre, M.; Garvert, D.W.; Weiss, B.; Carlson, E.B.; Bryant, R.A. Distinguishing PTSD, Complex PTSD, and Borderline Personality Disorder: A Latent Class Analysis. Eur. J. Psychotraumatology 2014, 5, 25097. [Google Scholar] [CrossRef] [PubMed]
- Levin, Y.; Lev Bar-Or, R.; Forer, R.; Vaserman, M.; Kor, A.; Lev-Ran, S. The Association between Type of Trauma, Level of Exposure and Addiction. Addict. Behav. 2021, 118, 106889. [Google Scholar] [CrossRef] [PubMed]
- Lotzin, A.; Haupt, L.; von Schönfels, J.; Wingenfeld, K.; Schäfer, I. Profiles of Childhood Trauma in Patients with Alcohol Dependence and Their Associations with Addiction-Related Problems. Alcohol. Clin. Exp. Res. 2016, 40, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Khantzian, E.J. The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harv. Rev. Psychiatry 1997, 4, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Volpicelli, J.; Balaraman, G.; Hahn, J.; Wallace, H.; Bux, D. The Role of Uncontrollable Trauma in the Development of PTSD and Alcohol Addiction. Alcohol. Res. Health 1999, 23, 256–262. [Google Scholar] [PubMed]
- Roberts, N.P.; Roberts, P.A.; Jones, N.; Bisson, J.I. Psychological Interventions for Post-Traumatic Stress Disorder and Comorbid Substance Use Disorder: A Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2015, 38, 25–38. [Google Scholar] [CrossRef]
- Schäfer, I.; Langeland, W.; Hissbach, J.; Luedecke, C.; Ohlmeier, M.D.; Chodzinski, C.; Kemper, U.; Keiper, P.; Wedekind, D.; Havemann-Reinecke, U. Childhood Trauma and Dissociation in Patients with Alcohol Dependence, Drug Dependence, or Both—A Multi-Center Study. Drug Alcohol. Depend. 2010, 109, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, M.; Mezey, G.; Chapman, M.; Wheeler, M.; Drummond, C.; Baldacchino, A. Co-Morbid Post-Traumatic Stress Disorder in a Substance Misusing Clinical Population. Drug Alcohol. Depend. 2005, 77, 251–258. [Google Scholar] [CrossRef]
- Paut Kusturica, M.; Tomas, A.; Sabo, A.; Tomić, Z.; Horvat, O. Medical Cannabis: Knowledge and Attitudes of Prospective Doctors in Serbia. Saudi Pharm. J. 2019, 27, 320–325. [Google Scholar] [CrossRef]
- Brown, T.; Berman, S.; McDaniel, K.; Radford, C.; Mehta, P.; Potter, J.; Hirsh, D.A. Trauma-Informed Medical Education (TIME): Advancing Curricular Content and Educational Context. Acad. Med. 2021, 96, 661–667. [Google Scholar] [CrossRef]
- Sznitman, S.R.; Lewis, N. Examining Effects of Medical Cannabis Narratives on Beliefs, Attitudes, and Intentions Related to Recreational Cannabis: A Web-Based Randomized Experiment. Drug Alcohol. Depend. 2018, 185, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Zolotov, Y.; Vulfsons, S.; Sznitman, S. Predicting Physicians’ Intentions to Recommend Medical Cannabis. J. Pain. Symptom Manag. 2019, 58, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Zolotov, Y.; Vulfsons, S.; Zarhin, D.; Sznitman, S. Medical Cannabis: An Oxymoron? Physicians’ Perceptions of Medical Cannabis. Int. J. Drug Policy 2018, 57, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Morell-Gomis, R.; Moriano, J.A.; Laguía, A.; Dias, P.; Lloret, D. Adolescents Cannabis Use Intention: Validating a Theory of Planned Behavior Questionnaire in Four European Countries. J. Subst. Use 2019, 24, 66–72. [Google Scholar] [CrossRef]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Kenny, D.A., Little, T.D., Eds.; The Guilford Press: New York, NY, USA, 2016; ISBN 978-1-4625-2334-4. [Google Scholar]
- Gelezelyte, O.; Roberts, N.P.; Kvedaraite, M.; Bisson, J.I.; Brewin, C.R.; Cloitre, M.; Kairyte, A.; Karatzias, T.; Shevlin, M.; Kazlauskas, E. Validation of the International Trauma Interview (ITI) for the Clinical Assessment of ICD-11 Posttraumatic Stress Disorder (PTSD) and Complex PTSD (CPTSD) in a Lithuanian Sample. Eur. J. Psychotraumatology 2022, 13, 2037905. [Google Scholar] [CrossRef] [PubMed]
- MacCallum, C.A.; Lo, L.A.; Boivin, M. “Is Medical Cannabis Safe for My Patients?” A Practical Review of Cannabis Safety Considerations. Eur. J. Intern. Med. 2021, 89, 10–18. [Google Scholar] [CrossRef]
- Wickens, C.M.; McDonald, A.J.; Stoduto, G.; Di Ciano, P.; Hamilton, H.A.; Elton-Marshall, T.; Nigatu, Y.T.; Mann, R.E. Risk Perceptions of Driving under the Influence of Cannabis: Comparing Medical and Non-Medical Cannabis Users. Transp. Res. Part. F Traffic Psychol. Behav. 2023, 95, 36–45. [Google Scholar] [CrossRef]
- Hochbaum, G.M. Research Relating to Health Education. Health Educ. Monogr. 1960, 1, 10–21. [Google Scholar] [CrossRef]
- Chambers, J.; Keyhani, S.; Ling, P.M.; Hoggatt, K.J.; Hasin, D.; Nguyen, N.; Woods, A.; Ryder, A.; Cohen, B.E. Perceptions of Safety of Daily Cannabis vs Tobacco Smoking and Secondhand Smoke Exposure, 2017–2021. JAMA Netw. Open 2023, 6, e2328691. [Google Scholar] [CrossRef]
- Hammond, D.; Wadsworth, E.; Reid, J.L.; Burkhalter, R. Prevalence and Modes of Cannabis Use among Youth in Canada, England, and the US, 2017 to 2019. Drug Alcohol. Depend. 2021, 219, 108505. [Google Scholar] [CrossRef] [PubMed]
- Hasin, D.; Walsh, C. Trends over Time in Adult Cannabis Use: A Review of Recent Findings. Curr. Opin. Psychol. 2021, 38, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Rose, G.L.; Brown, R.E. The Impaired Anesthesiologist: Not Just about Drugs and Alcohol Anymore. J. Clin. Anesth. 2010, 22, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Kory, W.P.; Crandall, L.A. Nonmedical Drug Use Patterns among Medical Students. Int. J. Addict. 1984, 19, 871–884. [Google Scholar] [CrossRef] [PubMed]
- Glodosky, N.C.; Cuttler, C. Motives Matter: Cannabis Use Motives Moderate the Associations between Stress and Negative Affect. Addict. Behav. 2020, 102, 106188. [Google Scholar] [CrossRef] [PubMed]
- Besson, A.; Tarpin, A.; Flaudias, V.; Brousse, G.; Laporte, C.; Benson, A.; Navel, V.; Bouillon-Minois, J.-B.; Dutheil, F. Smoking Prevalence among Physicians: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 13328. [Google Scholar] [CrossRef] [PubMed]
- Panfil, A.-L.; Lungeanu, D.; Tamasan, S.; Bredicean, C.; Papava, I.; Smirnova, D.; Fountoulakis, K.N. Suicidality Related to the COVID-19 Lockdown in Romania: Structural Equation Modeling. Front. Psychiatry 2022, 13, 818712. [Google Scholar] [CrossRef] [PubMed]
- Bartel, S.J.; Sherry, S.B.; Stewart, S.H. Self-Isolation: A Significant Contributor to Cannabis Use during the COVID-19 Pandemic. Subst. Abus. 2020, 41, 409–412. [Google Scholar] [CrossRef]
- Chong, W.W.-Y.; Acar, Z.I.; West, M.L.; Wong, F. A Scoping Review on the Medical and Recreational Use of Cannabis During the COVID-19 Pandemic. Cannabis Cannabinoid Res. 2022, 7, 591–602. [Google Scholar] [CrossRef]
- Gielen, N.; Havermans, R.C.; Tekelenburg, M.; Jansen, A. Prevalence of Post-Traumatic Stress Disorder among Patients with Substance Use Disorder: It Is Higher than Clinicians Think It Is. Eur. J. Psychotraumatology 2012, 3, 17734. [Google Scholar] [CrossRef]
- Simpson, T.L.; Goldberg, S.B.; Louden, D.K.N.; Blakey, S.M.; Hawn, S.E.; Lott, A.; Browne, K.C.; Lehavot, K.; Kaysen, D. Efficacy and Acceptability of Interventions for Co-Occurring PTSD and SUD: A Meta-Analysis. J. Anxiety Disord. 2021, 84, 102490. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.N.; Le Foll, B.; Imtiaz, S.; Rehm, J. The Effect of Post-Traumatic Stress Disorder on the Risk of Developing Prescription Opioid Use Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. Drug Alcohol. Depend. 2017, 179, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Sells, J.R.; Waters, A.J.; Schwandt, M.L.; Kwako, L.E.; Heilig, M.; George, D.T.; Ramchandani, V.A. Characterization of Comorbid PTSD in Treatment-Seeking Alcohol Dependent Inpatients: Severity and Personality Trait Differences. Drug Alcohol. Depend. 2016, 163, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.J.; Stout, R.L.; Mueller, T. Substance Use Disorder and Posttraumatic Stress Disorder Comorbidity: Addiction and Psychiatric Treatment Rates. Psychol. Addict. Behav. 1999, 13, 115–122. [Google Scholar] [CrossRef]
- Torchalla, I.; Nosen, L.; Rostam, H.; Allen, P. Integrated Treatment Programs for Individuals with Concurrent Substance Use Disorders and Trauma Experiences: A Systematic Review and Meta-Analysis. J. Subst. Abuse Treat. 2012, 42, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Breslau, N.; Kessler, R.C.; Chilcoat, H.D.; Schultz, L.R.; Davis, G.C.; Andreski, P. Trauma and Posttraumatic Stress Disorder in the Community. Arch. Gen. Psychiatry 1998, 55, 626. [Google Scholar] [CrossRef] [PubMed]
- Gluck, R.L.; Hartzell, G.E.; Dixon, H.D.; Michopoulos, V.; Powers, A.; Stevens, J.S.; Fani, N.; Carter, S.; Schwartz, A.C.; Jovanovic, T.; et al. Trauma Exposure and Stress-Related Disorders in a Large, Urban, Predominantly African-American, Female Sample. Arch. Womens Ment. Health 2021, 24, 893–901. [Google Scholar] [CrossRef]
- Messer, T.; Lammers, G.; Müller-Siecheneder, F.; Schmidt, R.-F.; Latifi, S. Substance Abuse in Patients with Bipolar Disorder: A Systematic Review and Meta-Analysis. Psychiatry Res. 2017, 253, 338–350. [Google Scholar] [CrossRef] [PubMed]
- Brady, T.M.; Ashley, O.S. Women in Substance Abuse Treatment: Results From the Alcohol and Drug Services Study (ADSS); National Clearinghouse for Alcohol and Drug Information: Rockville, MD, USA, 2005. [Google Scholar]
- Tuchman, E. Women and Addiction: The Importance of Gender Issues in Substance Abuse Research. J. Addict. Dis. 2010, 29, 127–138. [Google Scholar] [CrossRef]
- Ait-Daoud, N.; Blevins, D.; Khanna, S.; Sharma, S.; Holstege, C.P.; Amin, P. Women and Addiction: An Update. Med. Clin. N. Am. 2019, 103, 699–711. [Google Scholar] [CrossRef] [PubMed]
- Young, A.M.; Morales, M.; McCabe, S.E.; Boyd, C.J.; Darcy, H.; BOYD, C.J. Drinking Like a Guy: Frequent Binge Drinking Among Undergraduate Women. Subst. Use Misuse 2005, 40, 241–267. [Google Scholar] [CrossRef] [PubMed]
- Tomsen, S. A TOP NIGHT: Social Protest, Masculinity and the Culture of Drinking Violence. Br. J. Criminol. 1997, 37, 90–102. [Google Scholar] [CrossRef]
- Jorgensen, C.; Wells, J. Is Marijuana Really a Gateway Drug? A Nationally Representative Test of the Marijuana Gateway Hypothesis Using a Propensity Score Matching Design. J. Exp. Criminol. 2022, 18, 497–514. [Google Scholar] [CrossRef]
- Smart, R.; Pacula, R.L. Early Evidence of the Impact of Cannabis Legalization on Cannabis Use, Cannabis Use Disorder, and the Use of Other Substances: Findings from State Policy Evaluations. Am. J. Drug Alcohol. Abuse 2019, 45, 644–663. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).