Insulin–Mimetic Dihydroxanthyletin-Type Coumarins from Angelica decursiva with Protein Tyrosine Phosphatase 1B and α-Glucosidase Inhibitory Activities and Docking Studies of Their Molecular Mechanisms
Abstract
1. Introduction
2. Materials and Methods
2.1. General Experimental Procedures
2.2. Chemicals and Reagents
2.3. Plant Materials
2.4. Extraction, Fractionation, and Isolation
2.5. Assay for PTP1B Inhibitory Assay
2.6. α-Glucosidase Inhibitory Assay
2.7. Inhibition of ONOO−-Mediated Protein Tyrosine Nitration
2.8. Assay for ONOO− Scavenging Activity
2.9. Total ROS Generation Inhibitory Activity Assay
2.10. Measurement of Intracellular Reactive Oxygen Species Level
2.11. Kinetic Parameters of Coumarins in Lineweaver-Burk and Dixon Plots for Both PTP1B and α-Glucosidase Inhibition
2.12. Molecular Docking Simulation of PTP1B and α-Glucosidase Inhibition
2.13. Assay for Cell Viability
2.14. Induction of Insulin Resistant HepG2 Cells
2.15. 2-NBDG Glucose Uptake Assay
2.16. Cell Lysates Preparation and Analysis of Western Blot
2.17. Statistical Analysis
3. Results
3.1. Coumarins’ Activity in Inhibiting PTP1B and α-glucosidase
3.2. PTP1B and α-Glucosidase Inhibitory Enzyme Kinetics
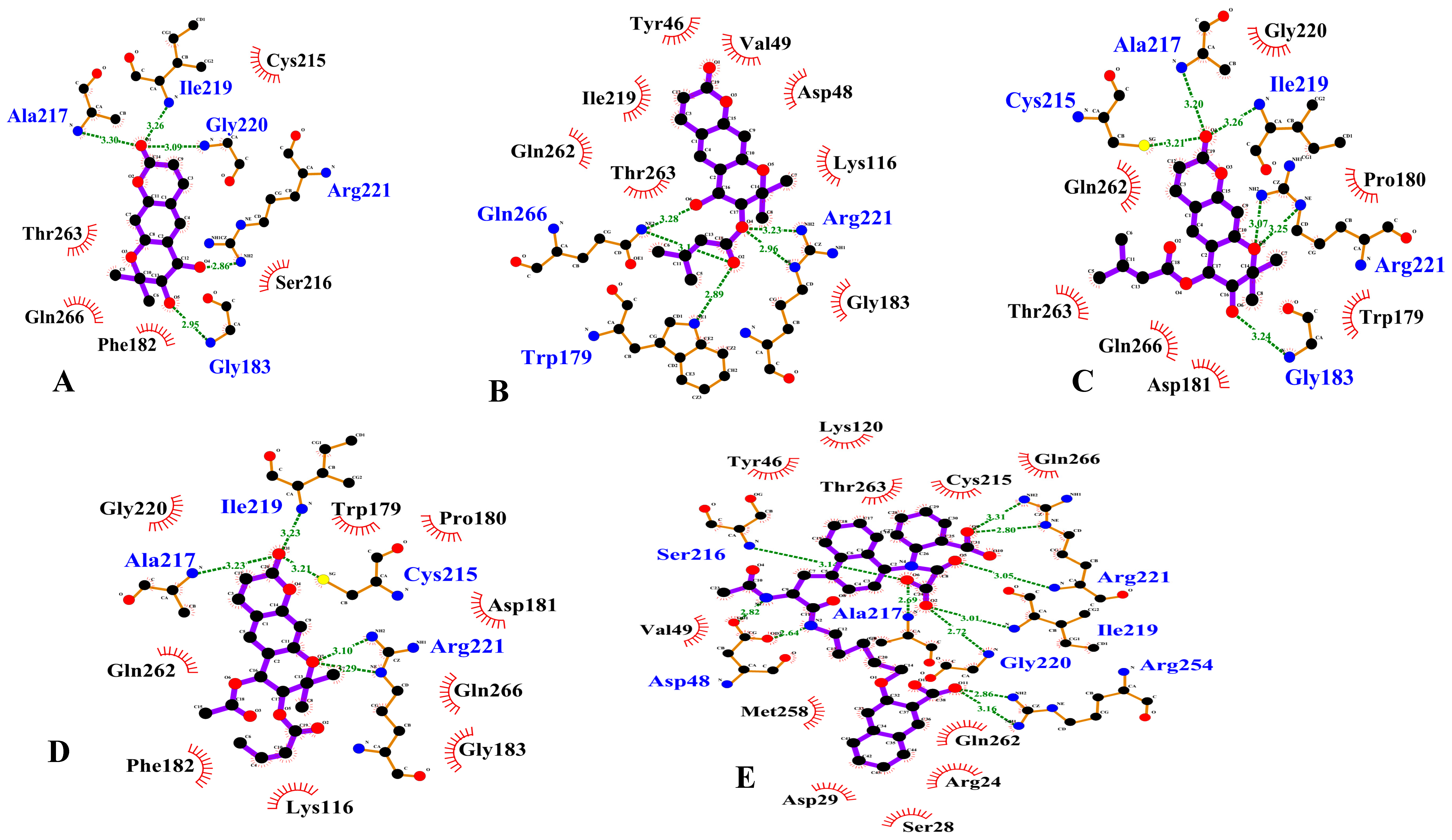
3.3. PTP1B Inhibition Molecular Docking Simulation
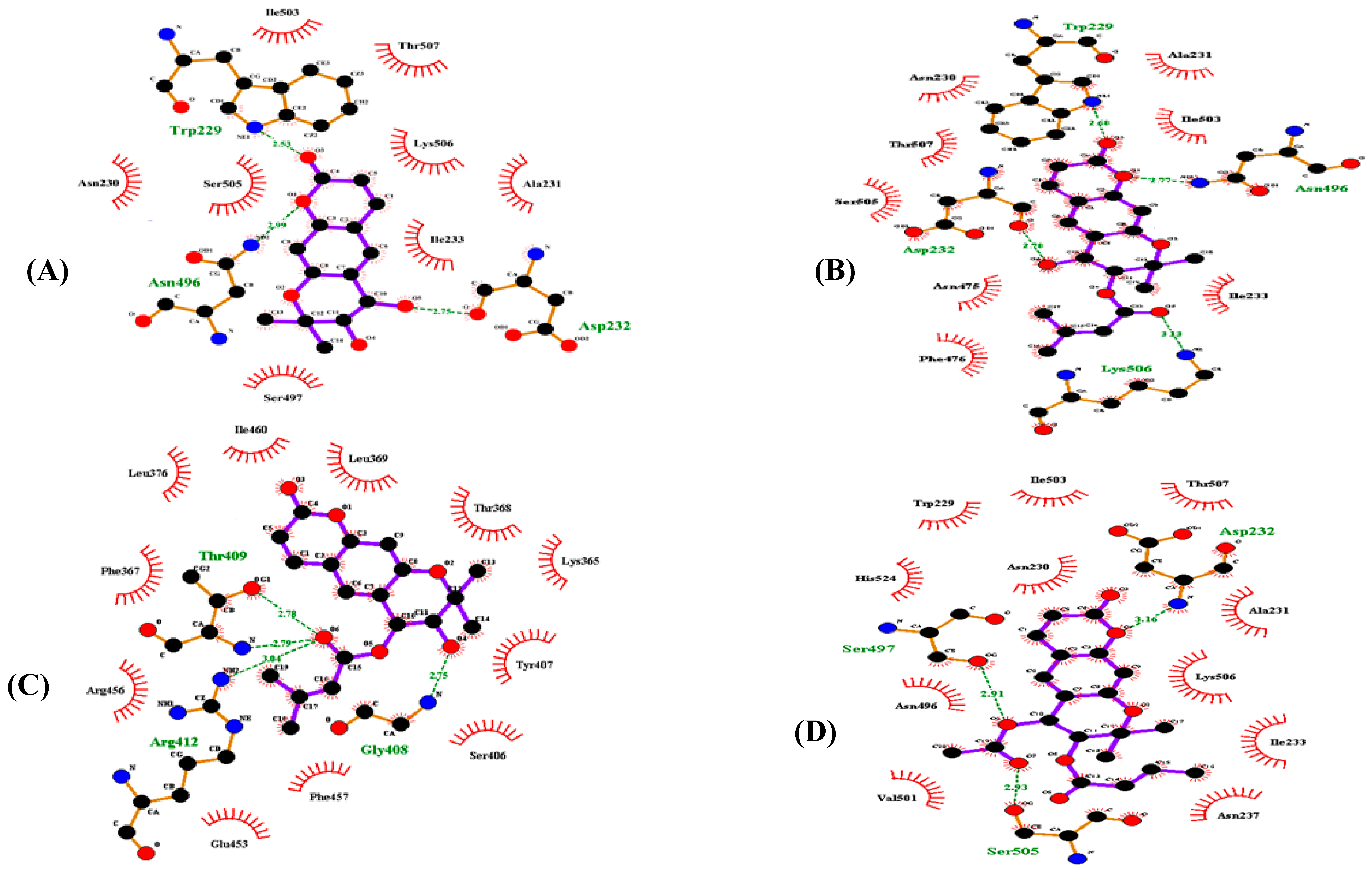
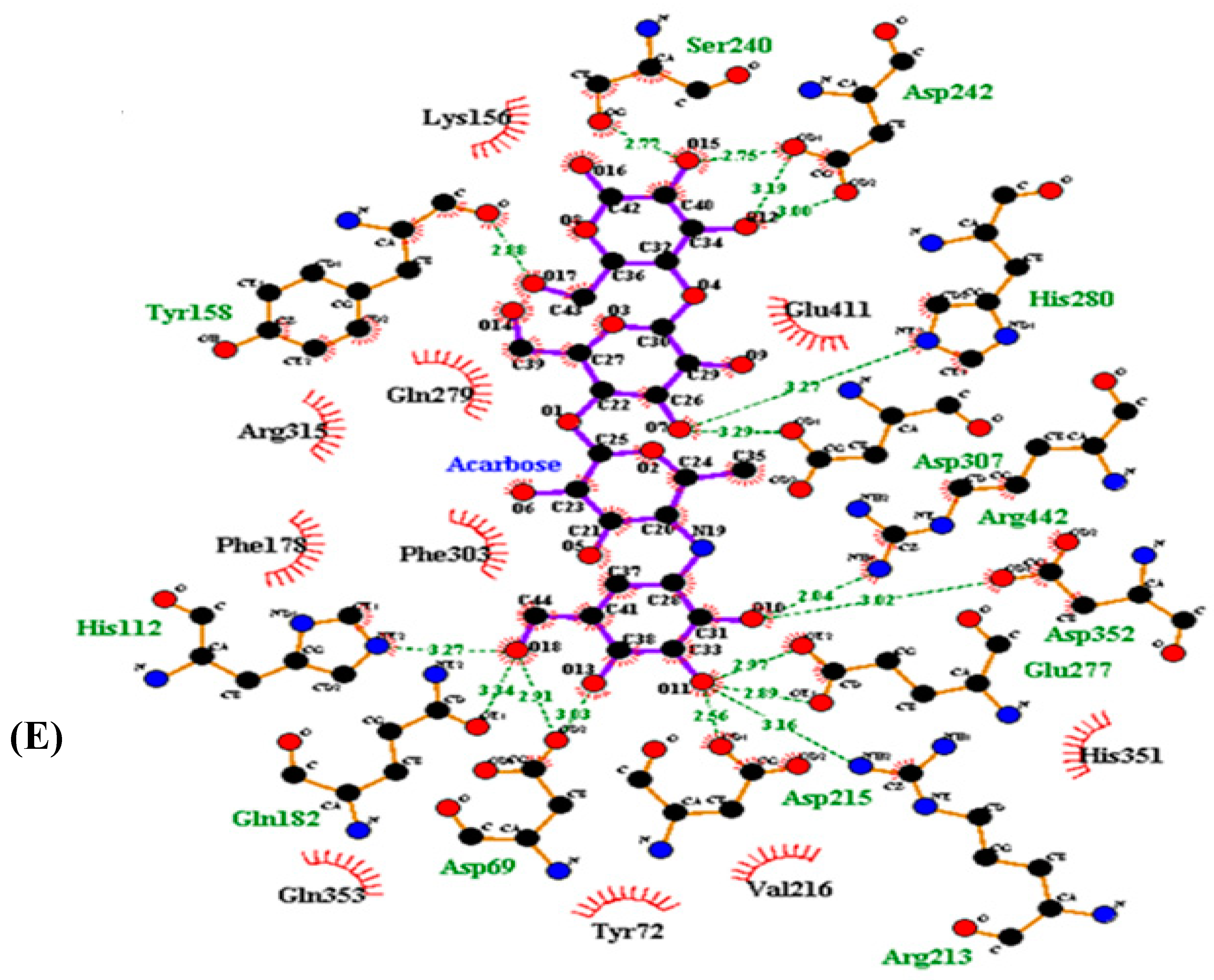
3.4. Molecular Docking Simulation of α-Glucosidase Inhibition
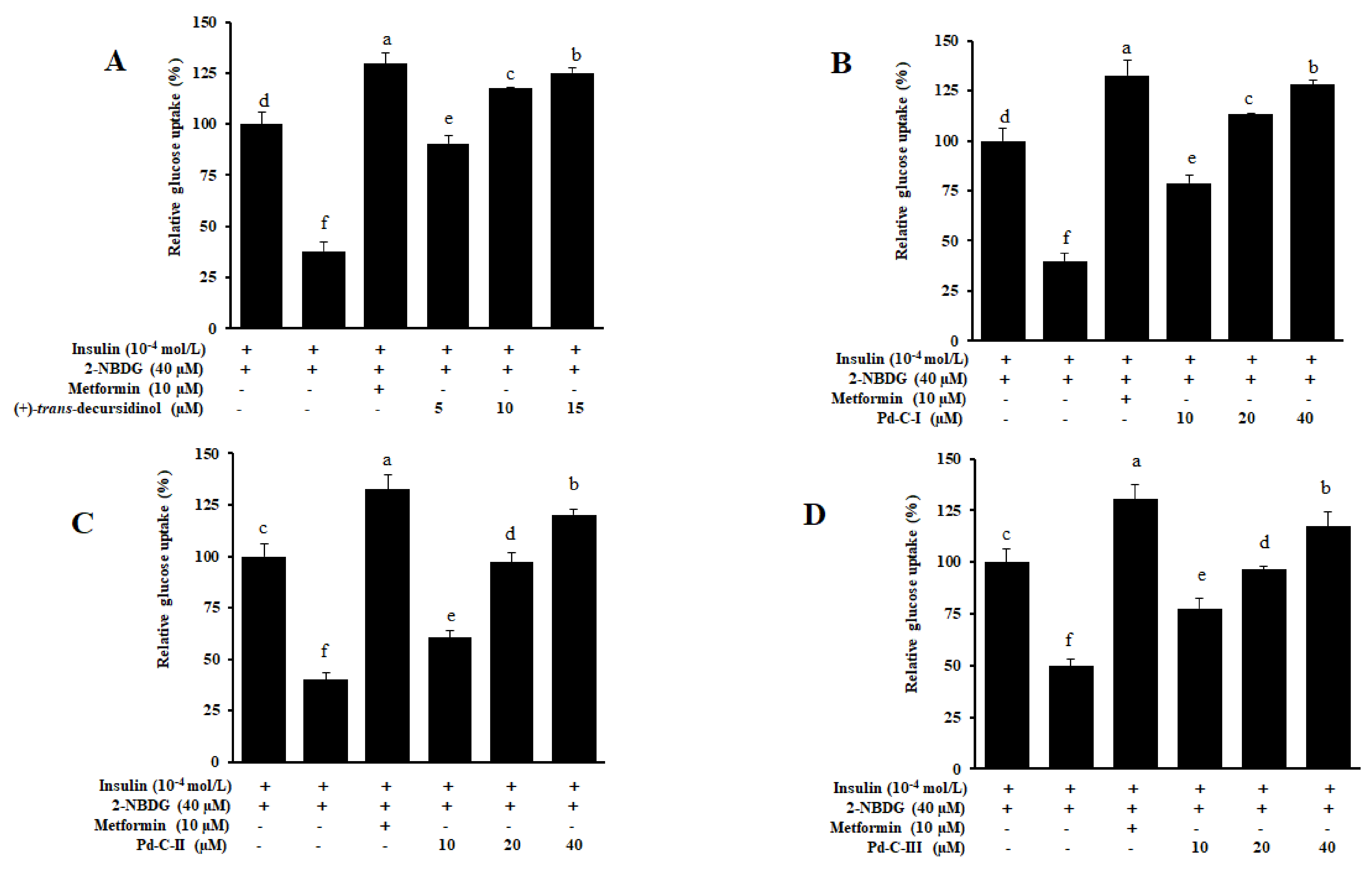
3.5. Coumarins’ Effect on Glucose Uptake in HepG2 Insulin-Resistant Cells
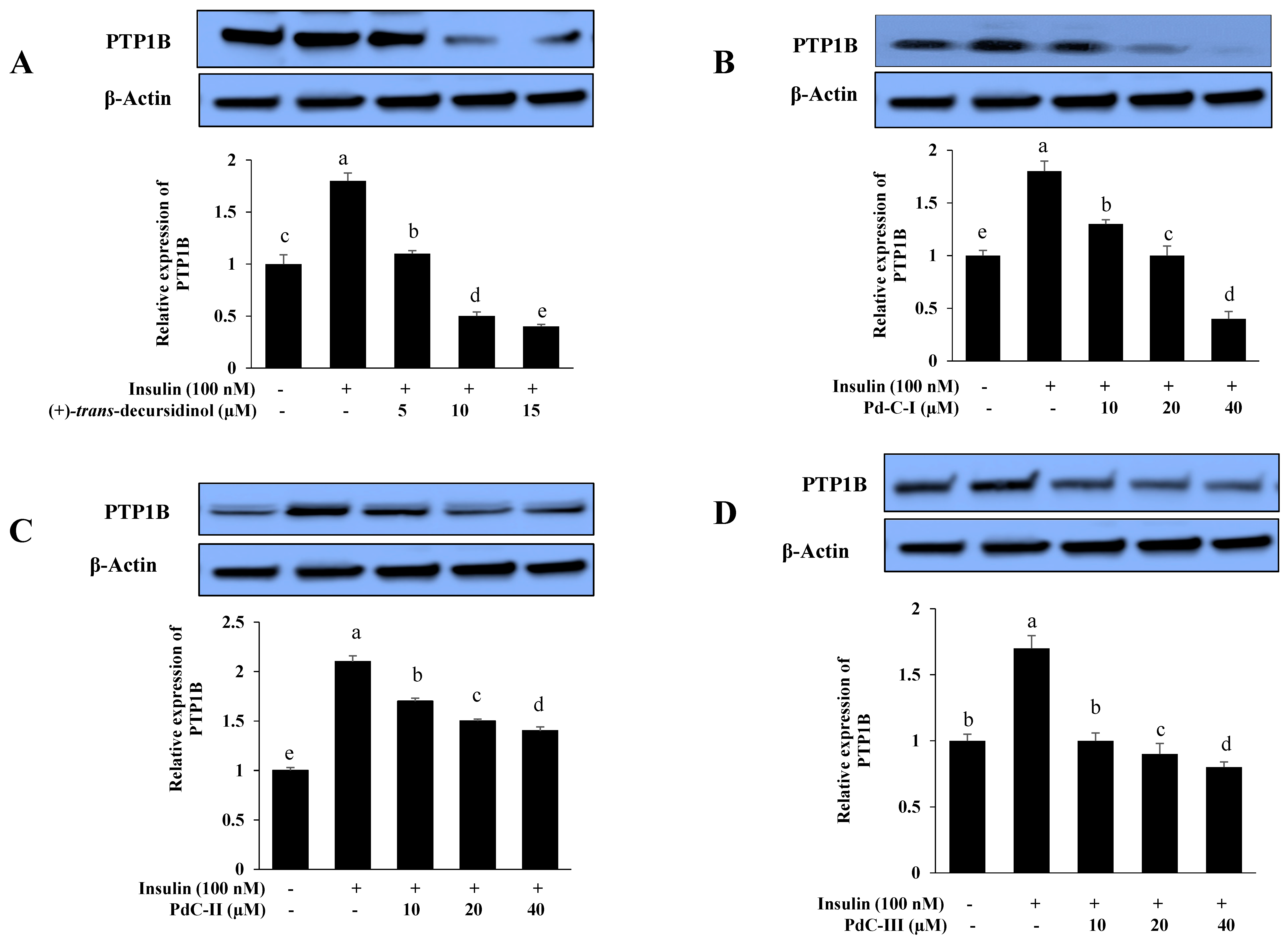
3.6. Effects on PTP1B Expression Level in Insulin-Resistant HepG2 Cells
3.7. The Coumarins’ Inhibitory Effect on ONOO−-Mediated Albumin Nitration
3.8. The Effect of Coumarins’ on the Levels of Intracellular ROS in t-BHP-Treated HepG2 Cells
3.9. The Coumarins’ Inhibitory Effect on ROS and ONOO−
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kong, W.; Wu, D.; Hu, N.; Li, N.; Dai, C.; Chen, X.; Suo, Y.; Li, G.; Wu, Y. Robust hybrid enzyme nanoreactor mediated plasmonic sensing strategy for ultrasensitive screening of anti-diabetic drug. Biosens. Bioelectron. 2018, 99, 653–659. [Google Scholar] [CrossRef]
- Fox, D.A.; Islam, N.; Sutherland, J.; Reimer, K.; Amed, S. Type 1 diabetes incidence and prevalence trends in a cohort of Canadian children and youth. Pediatr. Diabetes 2018, 19, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.A.; Ali, M.Y.; Bhakta, H.K.; Min, B.S.; Choi, J.S. Prunin is a highly potent flavonoid from Prunus davidiana stems that inhibits protein tyrosine phosphatase 1B and stimulates glucose uptake in insulin-resistant HepG2 cells. Arch. Pharm. Res. 2017, 40, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Lebovitz, H.E. Type 2 diabetes mellitus—Current therapies and the emergence of surgical options. Nat. Rev. Endocrinol. 2011, 7, 408. [Google Scholar] [CrossRef] [PubMed]
- Dang, F.; Jiang, Y.; Pan, R.; Zhou, Y.; Wu, S.; Wang, R.; Zhuang, K.; Zhang, W.; Li, T.; Man, C. Administration of Lactobacillus paracasei ameliorates type 2 diabetes in mice. Food Funct. 2018, 9, 3630–3639. [Google Scholar] [CrossRef]
- Paudel, P.; Yu, T.; Seong, S.H.; Kuk, E.B.; Jung, H.A.; Choi, J.S. Protein tyrosine phosphatase 1B inhibition and glucose uptake potentials of mulberrofuran G, albanol B, and kuwanon G from root bark of Morus alba L. in insulin resistant HepG2 cells: An in vitro and in silico study. Int. J. Mol. Sci. 2018, 19, 1542. [Google Scholar] [CrossRef]
- Johnson, T.O.; Ermolieff, J.; Jirousek, M.R. Protein tyrosine phosphatase 1B inhibitors for diabetes. Nat. Rev. Drug Discov. 2002, 1, 696–709. [Google Scholar] [CrossRef]
- Haque, A.; Andersen, J.N.; Salmeen, A.; Barford, D.; Tonks, N.K. Conformation-sensing antibodies stabilize the oxidized form of PTP1B and inhibit its phosphatase activity. Cell 2011, 147, 185–198. [Google Scholar] [CrossRef]
- Goldstein, B.J.; Bitter-Kowalczyk, A.; White, M.F.; Harbeck, M.J. Tyrosine dephosphorylation and deactivation of insulin receptor substrate-1 by protein tyrosine phosphatase 1B. Possible facilitation by the formation of a ternary complex with the GRB2 adaptor protein. Biol. Chem. 2000, 275, 4283–4289. [Google Scholar] [CrossRef]
- Elchebly, M.; Payette, P.; Michaliszyn, E.; Cromlish, W.; Collins, S.; Loy, A.L.; Normandin, D.; Cheng, A.; Himms-Hagen, J.; Chan, C.C.; et al. Increased insulin sensitivity and obesity resistance in mice lacking the protein tyrosine phosphatase-1B gene. Science 1999, 283, 1544–1548. [Google Scholar] [CrossRef]
- Klaman, L.D.; Boss, O.; Peroni, O.D.; Kim, J.K.; Martino, J.L.; Zabolotny, J.M.; Moghal, N.; Lubkin, M.; Kim, Y.B.; Sharpe, A.H.; et al. Increased energy expenditure, decreased adiposity, and tissue- specific insulin sensitivity in protein-tyrosine phosphatase1B-deficient mice. Mol. Cell. Biol. 2000, 20, 5479–5489. [Google Scholar] [CrossRef]
- Rasouli, H.; Hosseini-Ghazvini, S.M.B.; Adibi, H.; Khodarahmi, R. Differential α-amylase/α-glucosidase inhibitory activities of plant-derived phenolic compounds: A virtual screening perspective for the treatment of obesity and diabetes. Food Funct. 2017, 8, 1942–1954. [Google Scholar] [CrossRef]
- Han, L.; Fang, C.; Zhu, R.; Peng, Q.; Li, D.; Wang, M. Inhibitory effect of phloretin on α-glucosidase: Kinetics, interaction mechanism and molecular docking. Int. J. Biol. Macromol. 2017, 95, 520–527. [Google Scholar] [CrossRef]
- Lee, B.H.; Rose, D.R.; Lin, A.H.-M.; Quezada-Calvillo, R.; Nichols, B.L.; Hamaker, B.R. Contribution of the individual small intestinal α-glucosidases to digestion of unusual α-linked glycemic disaccharides. J. Agric. Food Chem. 2016, 64, 6487–6494. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.; Tang, B.; Stewart, A.J.; Tao, Y.; Shao, Y.; Cui, Y.; Yue, H.; Pei, J.; Liu, Z.; Mei, L.; et al. Erythritol attenuates postprandial blood glucose by inhibiting α-glucosidase. J. Agric. Food Chem. 2018, 66, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.L. Free radicals and tissue damage, mechanistic evidence from radiation studies. In Biochemical Mechanisms of Liver Injury; Academic Press: New York, NY, USA, 1998; pp. 123–125. [Google Scholar]
- Evans, J.L.; Goldfine, I.D.; Maddux, B.A.; Grodsky, G.M. Are oxidative stress activated signaling pathways mediators of insulin resistance and beta-cell dysfunction? Diabetes 2003, 52, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Drews, G.; Krippeit-Drews, P.; Dufer, M. Oxidative stress and beta-cell dysfunction. Pflugers Arch. 2010, 460, 703–718. [Google Scholar] [CrossRef]
- Bonnefont-Rousselot, D.; Bastard, J.P.; Jaudon, M.C.; Delattre, J. Consequences of the diabetic status on the oxidant/antioxidant balance. Diabetes Metab. 2000, 26, 163–176. [Google Scholar]
- Ceriello, A. Oxidative stress and diabetes-associated complications. Endocr. Pract. 2006, 12, 60–62. [Google Scholar] [CrossRef] [PubMed]
- Rains, J.L.; Jain, S.K. Oxidative stress, insulin signaling and diabetes. Free Radic. Biol. Med. 2011, 50, 567–575. [Google Scholar] [CrossRef]
- Ischiropoulos, H. Biological tyrosine nitration: A pathophysiological function of nitric oxide and reactive oxygen species. Arch. Biochem. Biophys. 1998, 356, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; Mercuri, F.; Quagliaro, L.; Assaloni, R.; Motz, E.; Tonutti, L.; Tabaga, C. Detection of nitrotyrosine in the diabetic plasma: Evidence of oxidative stress. Diabetologia 2001, 44, 834–838. [Google Scholar]
- Chi, Y.S.; Cheon, B.S.; Kim, H.P. Effect of wogonin, a plant flavone from Scutellaria radix, on the suppression of cyclooxygenase and the induction of inducible nitric oxide synthase in lipolpolysaccharide-treated RAW 264.7 cells. Biochem. Pharmacol. 2001, 61, 1195–1203. [Google Scholar] [PubMed]
- Kong, L.Y.; Li, Y.; Min, Z.D.; Li, X.; Zhu, T.R. Coumarins from Peucedanum praeruptorum. Phytochemistry 1996, 41, 1423–1426. [Google Scholar] [CrossRef]
- Yi, J.H.; Park, I.K.; Choi, K.S.; Shin, S.C.; Ahn, Y.J. Toxicity of medicinal plant extracts to Lycoriella ingenua (Diptera: Sciaridae) and Coboldia fuscipes (Diptera: Scatopsidae). J. Asia Pac. Entomol. 2008, 11, 221–223. [Google Scholar] [CrossRef]
- Zhao, D.; Islam, M.N.; Ahn, B.R.; Jung, H.A.; Kim, B.W.; Choi, J.S. In vitro antioxidant and anti-inflammatory activities of Angelica decursiva. Arch. Pharm. Res. 2012, 35, 179–192. [Google Scholar] [CrossRef]
- Ishita, I.J.; Islam, M.N.; Kim, Y.S.; Choi, R.J.; Sohn, H.S.; Jung, H.A.; Choi, J.S. Coumarins from Angelica decursiva inhibit lipopolysacharide-induced nitric oxide production in RAW 264.7 cells. Arch. Pharm. Res. 2016, 39, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.Y.; Jung, H.A.; Choi, J.S. Anti-diabetic and anti-Alzheimer’s disease activities of Angelica decursiva. Arch. Pharm. Res. 2015, 38, 2216–2227. [Google Scholar]
- Ali, M.Y.; Jannat, S.; Jung, H.A.; Choi, R.J.; Roy, A.; Choi, J.S. Anti-Alzheimer potential of coumarins from Angelica decursiva and Artemisia capillaris and structure-activity analysis. Asian Pac. J. Trop. Med. 2016, 9, 103–111. [Google Scholar] [CrossRef]
- Ali, M.Y.; Jannat, S.; Jung, H.A.; Jeong, H.O.; Chung, H.Y.; Choi, J.S. Coumarins from Angelica decursiva inhibit α-glucosidase activity and protein tyrosine phosphatase 1B. Chem. Biol. Interact. 2016, 252, 93–101. [Google Scholar] [CrossRef]
- Ali, M.Y.; Seong, S.H.; Reddy, M.R.; Seo, S.Y.; Choi, J.S.; Jung, H.A. Kinetics and molecular docking studies of 6-formyl umbelliferone isolated from Angelica decursiva as an inhibitor of cholinesterase and BACE1. Molecules 2017, 22, 1604. [Google Scholar] [CrossRef]
- Ali, M.Y.; Seong, S.H.; Jung, H.A.; Jannat, S.; Choi, J.S. Kinetics and molecular docking of dihydroxanthyletin-type coumarins from Angelica decursiva that inhibit cholinesterase and BACE1. Arch. Pharm. Res. 2018, 41, 753–764. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.Y.; Jung, H.A.; Jannat, S.; Choi, J.S. Dihydroxanthyletin-type coumarins from Angelica decursiva that inhibits the formation of advanced glycation end products and human recombinant aldose reductase. Arch. Pharm. Res. 2018, 41, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.Y.; Seong, S.H.; Jung, H.A.; Choi, J.S. Ethanobotany, phytochemistry, and pharmacology of Angelica decursiva Fr. et Sav. Nat. Prod. Sci. 2019, 25, 181–199. [Google Scholar] [CrossRef]
- Ali, M.Y.; Seong, S.H.; Jung, H.A.; Choi, J.S. Angiotensin-I-converting enzyme inhibitory activity of coumarins from Angelica decursiva. Molecules 2019, 24, 3937. [Google Scholar] [CrossRef]
- Chen, Y.C.; Chen, P.Y.; Wu, C.C.; Tsai, I.L.; Chen, I.S. Chemical constituents and anti-platelet aggregation activity from the root of Peucedanum formosanum. J. Food Drug Anal. 2008, 16, 15–25. [Google Scholar]
- Sarkhail, P. Traditional uses phytochemistry and pharmacological properties of the genus Peucedanum: A review. J. Ethnopharmacol. 2014, 156, 235–270. [Google Scholar] [CrossRef]
- Ahn, K.S.; Sim, W.S.; Lee, I.K.; Seu, Y.B.; Kim, I.H. Decursinol angelate: A cytotoxic and protein kinase C activating agent from the root of Angelica gigas. Planta Med. 1997, 63, 360–361. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Lee, S.; Jin, J.L.; Yun-Choi, H.S. Platelet antiaggregatory effects of coumarins from the roots of Angelica genuflexa and Angelica gigas. Arch. Pharm. Res. 2003, 26, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Jeon, S.J.; Jung, H.A.; Lee, H.E.; Park, S.J.; Lee, Y.; Lee, Y.; Ko, S.Y.; Kim, B.; Choi, J.S.; et al. Nodakenin enhances cognitive function and adult hippocampal neurogenesis in mice. Neurochem. Res. 2015, 40, 1438–1447. [Google Scholar] [CrossRef]
- Kang, S.Y.; Lee, K.Y.; Sung, S.H.; Kim, Y.C. Four new neuroprotective dihydropyranocoumarins from Angelica gigas. J. Nat. Prod. 2005, 68, 56–59. [Google Scholar] [CrossRef]
- Kim, D.H.; Kim, D.Y.; Kim, Y.C.; Jung, J.W.; Lee, S.J.; Yoon, B.H.; Cheong, J.H.; Kim, Y.S.; Kang, S.S.; Ko, K.H.; et al. Nodakenin, a coumarin compound, ameliorates scopolamine-induced memory disruption in mice. Life Sci. 2007, 80, 1944–1950. [Google Scholar] [CrossRef]
- Islam, M.N.; Choi, R.J.; Jin, S.E.; Kim, Y.S.; Ahn, B.R.; Zhao, D.; Jung, H.A.; Choi, J.S. Mechanism of anti-inflammatory activity of umbelliferone 6-carboxylic acid isolated from Angelica decursiva. J. Ethnopharmacol. 2012, 144, 175–181. [Google Scholar] [CrossRef]
- Sakakibara, I.; Okuyama, T.; Shibata, S. Studies on coumarins of a Chinese drug “Qian-Hu”. Planta Med. 1982, 44, 199–203. [Google Scholar] [CrossRef]
- Kooy, N.W.; Royall, J.A.; Ischiropoulos, H.; Beckman, J.S. Peroxynitrite-mediated oxidation of dihydrorhodamine 123. Free Radic. Biol. Med. 1994, 2, 149–156. [Google Scholar] [CrossRef]
- Lebel, C.P.; Bondy, S.C. Sensitive and rapid quantitation of oxygen reactive species formation in rat synaptosome. Neurochem. Int. 1990, 17, 435–440. [Google Scholar] [CrossRef]
- Lineweaver, H.; Burk, D. The determination of enzyme dissociation constants. J. Am. Chem. Soc. 1934, 56, 658–666. [Google Scholar] [CrossRef]
- Dixon, M. The determination of enzyme inhibitor constant. Biochem. J. 1953, 55, 170–171. [Google Scholar] [CrossRef]
- Cornish-Bowden, A. A simple graphical method for determining the inhibition constants of mixed, uncompetitive and non- competitive inhibitors. Biochem. J. 1974, 137, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Wiesmann, C.; Barr, K.J.; Kung, J.; Zhu, J.; Erlanson, D.A.; Shen, W.; Fahr, B.J.; Zhong, M.; Taylor, L.; Randal, M.; et al. Allosteric inhibition of protein tyrosine phosphatase 1B. Nat. Struct. Mol. Biol. 2004, 11, 730–737. [Google Scholar] [CrossRef]
- Ali, M.Y.; Kim, D.H.; Seong, S.H.; Kim, H.R.; Jung, H.A.; Choi, J.S. α-Glucosidase and protein tyrosine phosphatase 1B inhibitory activity of plastoquinones from marine brown alga Sargassum serratifolium. Mar. Drugs. 2017, 15, 368. [Google Scholar] [CrossRef]
- Verma, M.; Gupta, S.J.; Chaudhary, A.; Garg, V.K. Protein tyrosine phosphatase 1B inhibitors as antidiabetic agents –A brief review. Bioorganic Chem. 2017, 70, 267–283. [Google Scholar] [CrossRef]
- Wang, L.J.; Jiang, B.; Wu, N.; Wang, S.Y.; Shi, D.Y. Natural and semisynthetic protein tyrosine phosphatase 1B (PTP1B) inhibitors as anti-diabetic agents. RSC. Adv. 2015, 5, 48822–48834. [Google Scholar] [CrossRef]
- Israili, Z.H. Advances in the treatment of type 2 diabetes mellitus. Am. J. Ther. 2011, 18, 117–152. [Google Scholar] [CrossRef]
- Wu, X.; Hardy, V.E.; Joseph, J.I. Protein-tyrosine phosphatase activity in human adipocytes is strongly correlated with insulin- stimulated glucose uptake and is a target of insulin induced oxidative inhibition. Metabolism 2003, 52, 705–712. [Google Scholar] [CrossRef]
- Panzhinskiy, E.; Ren, J.; Nair, S. Pharmacological inhibition of protein tyrosine phosphatase 1B: A promising strategy for the treatment of obesity and type 2 diabetes mellitus. Curr. Med. Chem. 2013, 20, 2609–2625. [Google Scholar] [CrossRef] [PubMed]
- Derosa, G.; Maffioli, P. α-Glucosidase inhibitors and their use in clinical practice. Arch. Med. Sci. 2012, 8, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Barford, D.; Flint, A.J.; Tonks, N.K. Crystal structure of human protein tyrosine phosphatase 1B. Science 1994, 263, 1397–1404. [Google Scholar] [CrossRef] [PubMed]
- Shen, K.; Keng, Y.F.; Wu, L.; Guo, X.L.; Lawrence, D.S.; Zhang, Z.Y. Acquisition of a specific and potent PTP1B inhibitor from a novel combinatorial library and screening procedure. J. Biol. Chem. 2001, 276, 47311–47319. [Google Scholar] [CrossRef] [PubMed]
- Maeda, A.; Kai, K.; Ishii, M.; Ishii, T.; Akagawa, M. Safranal, a novel protein tyrosine phosphatase 1B inhibitor, activates insulin signaling in C2C12 myotubes and improves glucose tolerance in diabetic KK-Ay mice. Mol. Nutr. Food Res. 2014, 58, 1177–1189. [Google Scholar] [CrossRef]
- Takada, M.; Sumi, M.; Maeda, A.; Watanabe, F.; Kamiya, T.; Ishii, T.; Nakano, M.; Akagawa, M. Pyrroloquinoline quinone, a novel protein tyrosine phosphatase 1B inhibitor, activates insulin signaling in C2C12myotubes and improves impaired glucose tolerance in diabetic KK-Ay mice. Biochem. Biophys. Res. Commun. 2012, 428, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.Q.; Liu, T.; Chen, C.; Li, M.Y.; Wang, Z.Y.; Chen, R.S.; Wei, G.X.; Wang, X.Y.; Luo, D.Q. Fumosorinone, a novel PTP1B inhibitor, activates insulin signaling in insulin-resistance HepG2 cells and shows anti-diabetic effect in diabetic KKAy mice. Toxicol. Appl. Pharmacol. 2015, 285, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.A.; Kasum, C.M. Dietary flavonoids: Bioavailability, metabolic effects, and safety. Annu. Rev. Nutr. 2002, 22, 19–34. [Google Scholar] [CrossRef]
- Vitaglione, P.; Morisco, F.; Caporaso, N.; Fogliano, V. Dietary antioxidant compounds and liver health. Crit. Rev. Food Sci. Nutr. 2004, 44, 575–586. [Google Scholar] [CrossRef]
- Johansen, J.S.; Harris, A.K.; Rychly, D.J.; Ergu, A. Oxidative stress and the use of antioxidants in diabetes: Linking basic science to clinical practice. Cardiovasc. Diabetol. 2005, 4, 5. [Google Scholar] [CrossRef]
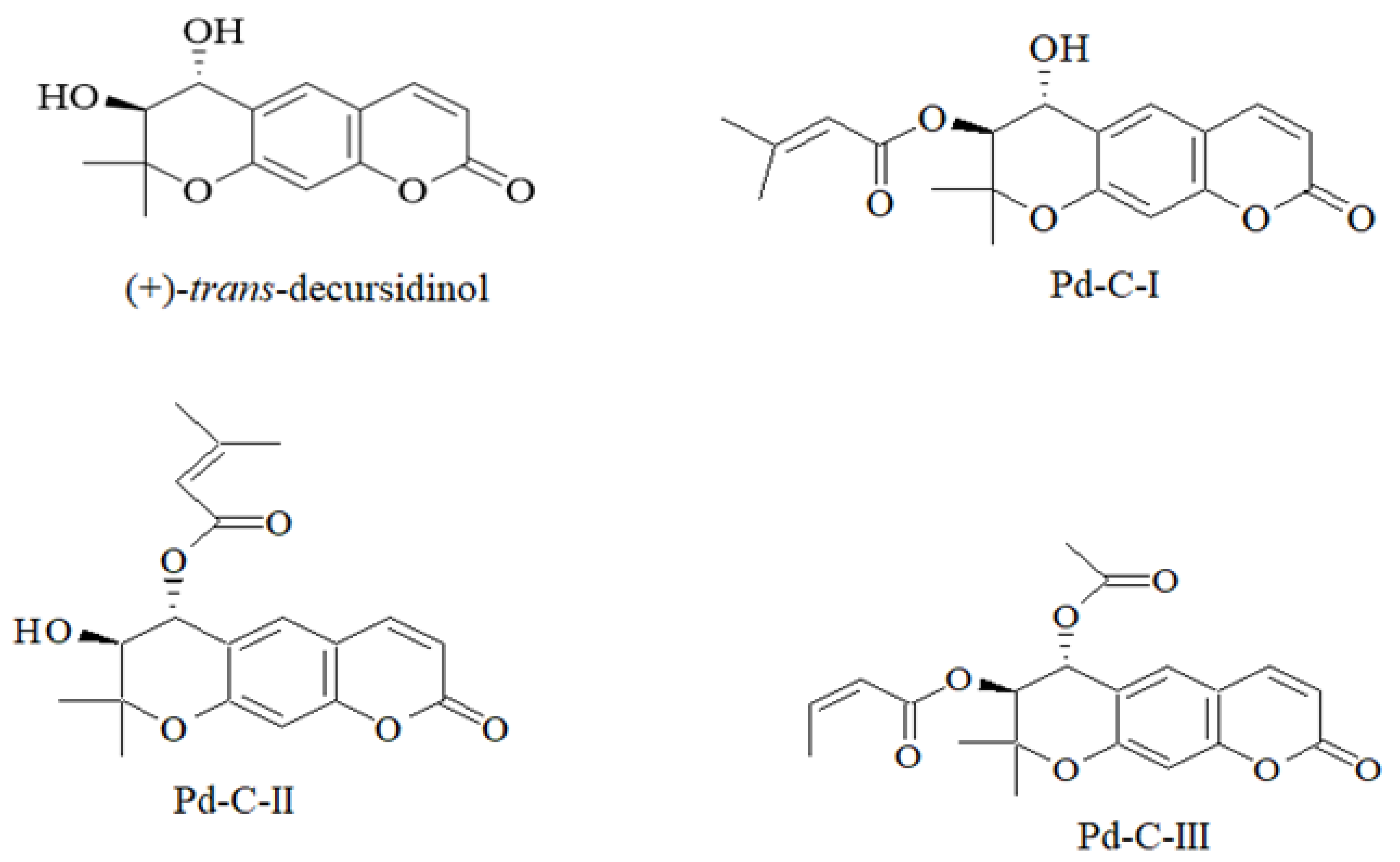


| Compounds | Protein Tyrosine Phosphatase 1B | α-Glucosidase | ||||
|---|---|---|---|---|---|---|
| IC50 (µM) a | Ki Value b | Inhibition Type c | IC50 (µM) a | Ki Value b | Inhibition Type c | |
| (+)-trans-decursidinol | 2.33 ± 0.07 | 2.84 | Competitive | 11.32 ± 0.56 | 16.02 | Competitive |
| Pd-C-I | 4.32 ± 0.12 | 6.21 | Competitive | 17.40 ± 0.33 | 22.98 | Mixed |
| Pd-C-II | 6.17 ± 0.31 | 9.72 | Competitive | 24.74 ± 0.89 | 30.83 | Mixed |
| Pd-C-III | 11.98 ± 0.43 | 16.04 | Mixed | 36.77 ± 1.04 | 55.59 | Noncompetitive |
| Ursolic acid d | 6.87 ± 0.19 | - | - | |||
| Acarbose e | 169.49 ± 3.25 | - | - | |||
| Compounds | Binding Energies (Kcal/mol) a | No. of H Bond b | H-bonding Interacting Residues c | Van der Waals Interacting Residues d |
|---|---|---|---|---|
| (+)-trans-decursidinol | −7.9 | 5 | Ala27, Ile219, Gly220, Arg221, Gly183 | Cys215, Gln266, Phe182, Thr263, Ser216 |
| Pd-C-I | −7.8 | 6 | Gln266, Arg221, Trp179 | Asp48, Gln262, Gly163, Ile219, Lys116, Thr263, Tyr46, Val49 |
| Pd-C-II | −7.5 | 6 | Cys215, Ala217, Ile219, Gly183, Arg221 | Asp181, Gln266, Gly220, Gln262, Pro180, Trp179, Thr263 |
| Pd-C-III | −7.7 | 5 | Ile219, Ala217, Cys215, Arg221 | Asp181, Gly183, Gln266, Gln262, Gly220, Lys116, Phe182, Pro180, Trp179 |
| Compound 23 | −11.23 | 11 | Asp48, Ala217, Arg221, Arg254, Gly220, Ile219, Ser216 | Arg24, Asp29, Cys215, Gln266, Gln262, Lys120, Met258, Ser28, Thr263, Tyr46, Val49 |
| Compounds. | Binding Energies (Kcal/mol) a | No. of H Bond b | H-bonding Interacting Residues c | Van der Waals Interacting Residues d |
|---|---|---|---|---|
| (+)-trans-decursidinol | −7.09 | 3 | Trp229, Ans496, Asp232 | Ile503, Thr507, Lys506, Ala231, Ile233, Ser497, Asn230, Ser505 |
| Pd-C-I | −8.09 | 4 | Trp229, Asp232, Ans496, Lys506 | Asn230, Ala231, Thr507, Ile503, Ser505, Asn475, Ile233, Phe476 |
| Pd-C-II | −7.6 | 4 | Thr409, Arg412, Gly408 | Ile460, Leu369, Thr368, Lys365, Tyr407, Ser406, Phe457, Glu453, Arg456, Phe367, Leu376 |
| Pd-C-III | −7.24 | 3 | Asp232, Ser497, Ser505 | Ile503, Thr507, Ala231, Lys506, Ile233, Asn237, Val501, Asn496, His524, Asn230, Trp229 |
| Acarbose | −10.20 | 17 | Arg442, Asp307, Asp215, Arg213, Asp352, Asp69, Asp242, His280, Tyr158, His112, Gln182, Glu277, Ser240, | Arg315, Gln353, His351, Glu411, Tyr72, Lys156, Gln279, Phe178, Phe303, Val216 |
| Test Sample | IC50 (µM) a | |
|---|---|---|
| ONOO− | ROS | |
| (+)-trans-decursidinol | 4.57 ± 0.21 | 9.77 ± 0.32 |
| Pd-C-I | 1.82 ± 0.44 | 6.32 ± 0.41 |
| Pd-C-II | 3.77 ± 0.15 | 10.76 ± 0.73 |
| Pd-C-III | 1.44 ± 0.22 | 9.69 ± 0.21 |
| l-Penicillamine b | 1.86 ± 0.11 | - |
| Trolox c | - | 3.29 ± 0.26 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, M.Y.; Jannat, S.; Jung, H.A.; Choi, J.S. Insulin–Mimetic Dihydroxanthyletin-Type Coumarins from Angelica decursiva with Protein Tyrosine Phosphatase 1B and α-Glucosidase Inhibitory Activities and Docking Studies of Their Molecular Mechanisms. Antioxidants 2021, 10, 292. https://doi.org/10.3390/antiox10020292
Ali MY, Jannat S, Jung HA, Choi JS. Insulin–Mimetic Dihydroxanthyletin-Type Coumarins from Angelica decursiva with Protein Tyrosine Phosphatase 1B and α-Glucosidase Inhibitory Activities and Docking Studies of Their Molecular Mechanisms. Antioxidants. 2021; 10(2):292. https://doi.org/10.3390/antiox10020292
Chicago/Turabian StyleAli, Md Yousof, Susoma Jannat, Hyun Ah Jung, and Jae Sue Choi. 2021. "Insulin–Mimetic Dihydroxanthyletin-Type Coumarins from Angelica decursiva with Protein Tyrosine Phosphatase 1B and α-Glucosidase Inhibitory Activities and Docking Studies of Their Molecular Mechanisms" Antioxidants 10, no. 2: 292. https://doi.org/10.3390/antiox10020292
APA StyleAli, M. Y., Jannat, S., Jung, H. A., & Choi, J. S. (2021). Insulin–Mimetic Dihydroxanthyletin-Type Coumarins from Angelica decursiva with Protein Tyrosine Phosphatase 1B and α-Glucosidase Inhibitory Activities and Docking Studies of Their Molecular Mechanisms. Antioxidants, 10(2), 292. https://doi.org/10.3390/antiox10020292






