Abstract
Cardiovascular disease (CVD) remains the leading cause of death globally, with unhealthy lifestyles today greatly increasing the risk. Over the decades, scientific investigation has been carried out on reactive oxygen species (ROS) and their resultant oxidative stress based on their changes made on biological targets such as lipids, proteins, and DNA. Since the existing clinical studies with antioxidants failed to provide relevant findings on CVD prediction, the focus has shifted towards recognition of oxidised targets as biomarkers to predict prognosis and response to accurate treatment. The identification of redox markers could help clinicians in providing risk stratification for CVD events beyond the traditional prognostic and diagnostic targets. This review will focus on how oxidant-related parameters can be applied as biomarkers for CVD based on recent clinical evidence.
1. Introduction
Cardiovascular disease (CVD) represents an immense burden on health services globally. Every year, CVD contributes to nearly 44% of mortality compared to other non-communicable diseases (WHO, 2021) [1], with the major contributor—ischemic heart disease—giving a prevalence of 126.5 million people [2]. The health statistics reports present that 92.1 million people live with at least one form of CVD in the United States [3]. Comorbidity conditions such as hyperlipidaemia, hypertension, and hyperglycaemia are common in CVD patients which further accelerate the disease progression [4]. There remains growing concern focused on improving the cardiovascular risk stratification and the need for novel biomarkers to provide early diagnosis.
Oxidative stress is assumed to play a pivotal role in cardiac remodelling and is responsible for the promotion and propagation of CVD [5]. Recent research concerning its pathophysiology and development focuses on the breakdown of normal homeostatic systems resulting in oxidative stress. It occurs with the imbalance between the reactive oxygen or nitrogen species (ROS/RNS) and the body’s antioxidant defence systems [6]. The overproduction of ROS may surpass the cellular antioxidant capacity and perturb the equilibrium [7]. These may subsequently induce protein and lipid peroxidation along with DNA mutagenesis that may cause deleterious effects [8]. In addition to eliciting direct cellular damage, oxidative stress also stimulates mitochondrial dysfunction and promotes free radicals’ formation that only exacerbates the disease burden [9].
To date, the precise mechanism by which pro- and anti-oxidative factors influence CVD manifestation and contribute their complications are not fully elucidated [9]. However, in eliciting direct cellular damage, oxidative stress was reported to stimulate mitochondrial dysfunction, dyslipidaemia, and genetic predispositions, and promotes free radicals’ formation that only exacerbates the disease burden [10].
Many clinical and experimental studies provide a comprehensive understanding on antioxidant approaches, such as vitamins C and E to be used concurrently with guideline-recommended drug treatment, but these antioxidants mostly show discouraging results in cardiovascular prognosis [4,11]. There is emerging evidence suggesting that CVDs are associated with or even provoked by oxidised targets. Both animal models and patients with heart failure (HF) constantly showed increased oxidative stress throughout their onset and disease progression [5]. This fact is also well supported by ROS-sensitive pro-hypertrophic and remodelling signalling cascades in the setting of cardiac hypertrophy [8]. Despite the recognition of oxidant biomarkers with their convenience to be used and affordable, available information regarding their prognostic relevance is still limited [10].
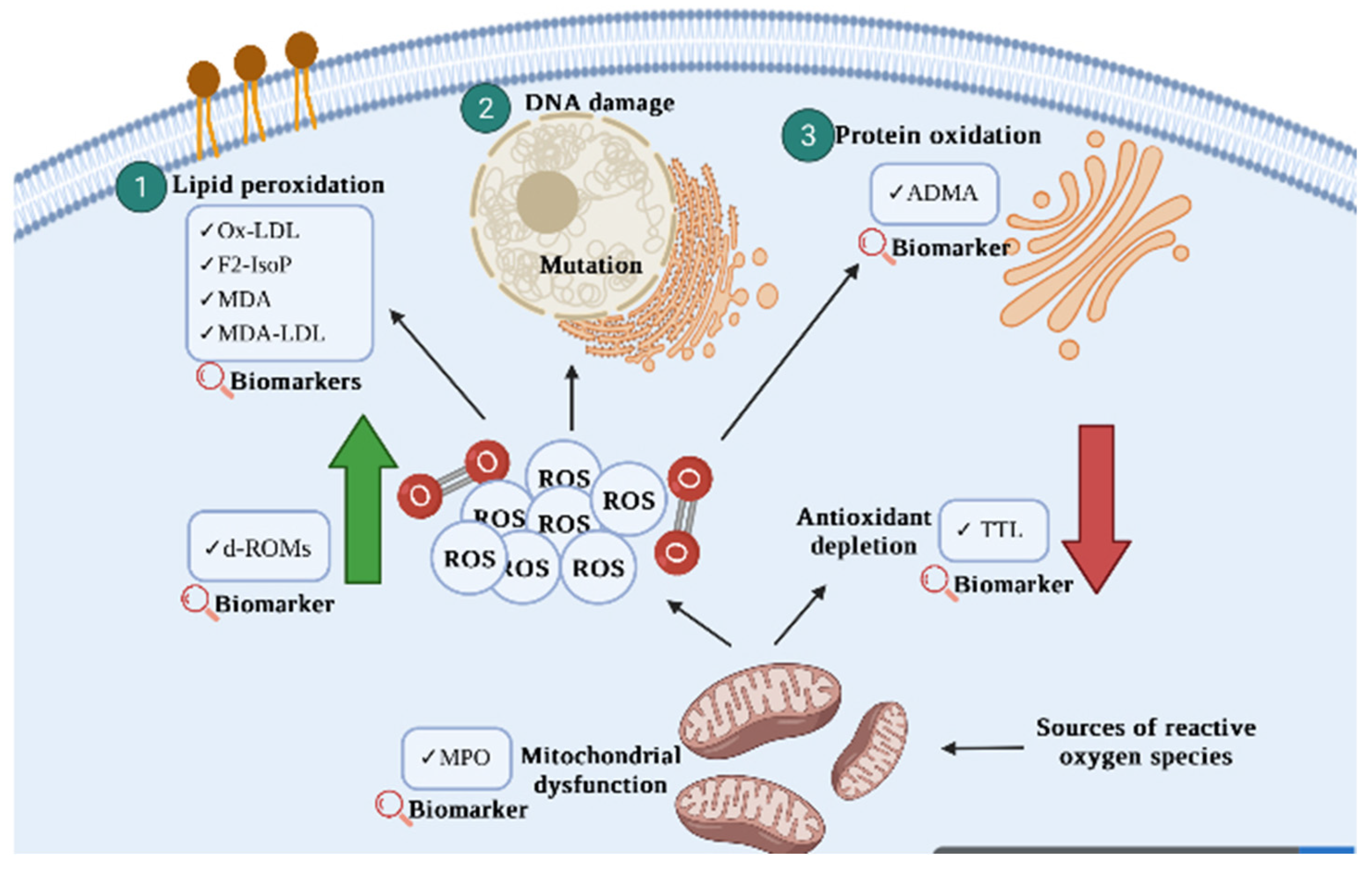
Nevertheless, the nature of ROS/RNS that are available in the body and specifically target CVD fulfil the essential requirement of a biomarker. The application of oxidant targets with prognostic values may be applied to reflect the disease risk on individuals and potentially be used in precision medicine shortly [4]. In this review, we aim to recapitulate the current knowledge regarding oxidant related parameters so as to estimate their effectiveness as a biomarker for the development and progression of CVD. Figure 1 represents oxidative stress-related biomarkers for cardiovascular disease.
Figure 1.
A schematic representation of oxidative stress-related biomarkers for cardiovascular disease that were discussed in the current review. Oxidative stress occurs when there is an imbalance of ROS and antioxidants. The generation of uncontrollable ROS may subsequently induce DNA damage, protein oxidation, and lipid peroxidation, which contribute to the progression and development of CVD.
2. Oxidant Biomarkers in the Diagnosis and Prognosis of CVD
2.1. Myeloperoxidase (MPO)
The primary source of oxidative stress is myeloperoxidase (MPO), a member of the family of heme peroxidases in human vasculature that is primarily secreted by neutrophils and macrophages [12]. Uncontrollable overexpression of MPO is associated with poor cardiovascular outcomes and an increased risk of cardiovascular-related mortality [13]. Mainly, MPO has contributed to the development of plaques in the artery wall with the production of ROS [14]. During the early onset of CVD, neutrophils and macrophages will be activated to synthesise MPO and produce 3-chlorotyrosine (3-Cl-Tyr) and 3-nitrotyrosine (3-NO-Tyr), the by-products that have been widely implicated in the development of atherosclerotic lesions. Both reactive oxidant products could stimulate protease cascades and induce plaque rupture [15]. Over the decades, MPO has been suggested to be used as a powerful diagnostic and prognostic marker for a wide variety of CVD conditions, such as acute myocardial infarction (AMI), coronary artery disease (CAD), and congestive HF [16].
High-density lipoprotein (HDL) is a primary target for oxidative modification in CAD patients [17]. Recent reviews highlighted the ability of MPO in inducing changes and impairing HDL, which resulted in a loss of cardioprotective effect and initiation of pro-inflammatory processes [12,18]. Both 3-Cl-Tyr and 3-NO-Tyr have been shown to impair the ATP-binding cassette transporter (ABCA1)-dependent cholesterol efflux activity which causes excessive cholesterol accumulation in arteries and activates foam cell formation [19,20]. However, a different research finding was demonstrated by Wang and colleagues (2018). The HDL isolated from aortic lesions in CAD patients contains high levels of 3-Cl-Tyr and 3-NO-Tyr. Despite HDL 3-NO-Tyr being identified as the best predictive marker associated with CAD, HDL 3-NO-Tyr did not correlate with 3-Cl-Tyr in MPO plasma, suggesting that the functional 3-NO-Tyr was derived from other RNS instead of MPO action. More studies on MPO-modified HDL are required to explore the association with cardiovascular outcomes before MPO could be used as a target to boost HDL function and provide clinical benefit to patients.
In an attempt to identify AMI in patients presenting angina, Omran and colleagues (2018) have investigated the diagnostic efficiency of plasma MPO levels alone or in combination with creatine kinase (CK)-MB and Troponin I (cTnI) within the first 6 h of disease onset [21]. MPO was found to be the most efficient marker in detecting AMI patients. Interestingly, the combination of MPO, CK-MB, and cTnI was able to provide a sensitivity of 91% and a specificity of 76% in detecting AMI compared to each marker alone. Similar finding was seen in Calmarza and colleagues (2018), whereby the plasma MPO levels significantly increased in ACS patients compared to those with stable angina and yielded its best result at the 6th hour after hospital administration [22].
In the setting of adult male participants with hypertension, Charkiewicz and colleagues (2021) showed high levels of MPO in hypertension men compared to the control groups without the disease [23]. The elevated MPO may induce oxidative stress and trigger endothelial dysfunction which results in increased blood pressure.
Zhang and colleagues (2022) highlighted the association of MPO with inflammatory responses [24]. Several inflammatory markers, such as c-reactive protein, fibrinogen, and neutrophil counts, were significantly increased with the elevation of MPO levels. Further analysis showed that MPO could provide a higher prognostic value in patients > 65 years and NT-proBNP level > 1000 pg/mL, suggesting its role in predicting the occurrence of major adverse cardiovascular events (MACEs) in patients with acute non-ST-segment elevation myocardial infarction (NSTEMI). There was also a positive correlation between MPO and global registry of coronary artery events (GRACE) scores in which high levels of MPO were classified as high-risk groups based on GRACE scores. This subsequently improved the risk classification of NSTEMI and aided in therapeutic approaches.
2.2. ox-LDL
Low-density lipoprotein (LDL) is routinely used for cardiovascular risk assessment clinically with high levels indicating greater risk of CVD [25]. In the presence of hydrogen peroxidase, MPO can induce oxidative modification on LDL and release oxidised LDL (ox-LDL) [18]. While the normal LDL only specified one type of receptor, ox-LDL had a higher affinity towards several receptors that greatly aided with its uptake to macrophages and endothelial cells. Together with other underlying metabolic syndromes, ox-LDL further accelerates its deposition in arteries and triggers plaque formation.
Large prospective cohort studies have demonstrated the association of elevated plasma ox-LDL with adverse cardiovascular events [26]. A positive correlation was seen in ox-LDL with the increased severity of CAD [27]. Likewise, Zhao and colleagues (2018) summarised the predictive values of CAD severity by employing six different LDL-related parameters [28]. All of them were raised with increasing severity of CAD, but ox-LDL showed the highest predictive value and was independently associated with CAD severity.
Another experiment performed by Zhao and colleagues (2018) investigated the relationship between ox-LDL and early-onset CAD based on a follow-up study on 1217 untreated patients with angina [29]. Higher levels of ox-LDL were associated with patients with very early CAD (VECAD) compared to the control group. The plasma levels of ox-LDL were independently associated with VECAD, suggesting that ox-LDL could be used as a prognostic predictor for VECAD to aid in disease management.
2.3. F2-Isoprostanes (F2-lsoP)
F2-isoprostanes (F2-IsoP) are circulating in bodily fluids, such as serum and urine [30]. Elevated levels of F2-IsoP can be observed in animal models of oxidant injury and human disease defined by elevated ROS. There is increasing evidence focusing on the association of increased F2-IsoP with CVD risk factors, such as hypercholesterolemia, diabetes mellitus, and cigarette smoking, but limited research linking this biomarker to clinical outcomes [27]. Anderson and colleagues (2018) demonstrated an elevation of F2-IsoP metabolite in individuals with incident hypertension [31]. The ability of F2-IsoP in promoting vasoconstriction and inflammation further supports their potential involvement in the development of hypertension.
In a large community-based study conducted by Castro-Diehl and colleagues (2021), urinary F2-IsoP was significantly associated with all causes of mortality, especially in fatal coronary heart disease (CHD) [32]. A similar finding was seen in another large German cohort study performed by Xuan and colleagues (2018) [33]. Urinary F2-IsoP was associated with fatal stroke and older (age ≥ 60 years) obese individuals in all CVD mortality. The ability of F2-IsoP to retain its stability in urine allowed it to assess oxidative stress status in vivo accurately.
2.4. Asymmetric Dimethylarginine (ADMA)
Asymmetric dimethylarginine (ADMA) competes with L-arginine to the same binding site of nitric oxide synthase and this affects the oxidative stress process [34]. Cordts and colleagues (2019) suggested that high levels of ADMA in the circulation may reduce nitric oxide production and impaired myocardial relaxation in patients with hypertrophic cardiomyopathy (HCM) [35]. A high concentration of ADMA was also associated with increasing severity of diastolic dysfunction, the early manifestation of HCM. Similarly, Charkiewicz and colleagues supported the association of increased ADMA in hypertension men with endothelial dysfunction [23].
In a meta-analysis conducted by Ye and colleagues (2021), CAD patients had an approximately two-fold increased risk of all causes of mortality and MACEs with the elevation of plasma ADMA [36]. This suggests that ADMA could be a marker to predict deaths and cardiovascular-related outcomes in CAD patients. A similar finding was demonstrated by Xu and colleagues (2019) in which ADMA independently predicted recurrent cardiovascular events in patients with stable CHD after one year of follow-up [37]. Another study by Appel and colleagues (2020) reported that patients with elevated ADMA were at risk of major cardiovascular complications before their non-cardiac operation [34].
2.5. Total Thiol (TTL)
Total thiol (TTL) appears early in CVD onset and represents the redox control status of vascular systems [38]. An application of this assay in a pooled case-control study by Xuan and colleagues (2019) showed that increased TTL was associated with incident stroke but only restricted to stroke events that happen in mid-life, ages ranging from 45 to 60 years. Further analysis revealed the association of TTL with fatal MI risk. However, Erdoğan and colleagues (2020) highlighted a different finding in which higher levels of TTL were shown in the control group than in the ascending aortic dilatation (AAD) group [39]. Lower TTL appears to confer a higher risk for AAD development and independently predicts the diameter of ascending aortic.
2.6. Derivatives of Reactive Oxygen Metabolites (d-ROMs)
Derivatives of reactive oxidative metabolites (d-ROMs) are a newly discovered marker of ROS and are good in reflecting ROS production of a biological target. Xuan and colleagues (2019) demonstrated an increased level of d-ROMs in the incidence of MI and stroke, but the results were only significant in the male subjects. d-ROMs were also associated with fatal MI risk [38]. Considering a weak correlation between d-ROMs and TTL, researchers proposed the use of a d-ROMs-to-TTL ratio, which provides stronger results compared to the individual markers alone. The d-ROMs-to-TTL ratio was significantly associated with the onset of major cardiovascular events, but this association did not retain when diseases and CRP for the outcome were included.
Nishihara and colleagues (2021) performed an 8-year follow-up cohort study and revealed the usage of d-ROMs in providing prognostic value for risk classification on non-ischemic heart failure (NIHF) [40]. Higher levels of d-ROMs increased the risk of HF-related events.
2.7. Malondialdehyde (MDA)
Nitric oxide contributes to oxidative stress by regulating lipid peroxidation and produces MDA as an end-product under physiological conditions [23]. Romuk and colleagues (2019) observed an elevation of MDA with the mortality prediction in chronic HF patients. The risk of mortality and the combined endpoint of death in the research subjects were increased two-fold in the presence of high MDA [41].
Recent novel findings by Boarescu and colleagues (2022) showed the importance of prevalent cardiovascular risk factors with MDA. Hypertension, lipid imbalance, and diabetes mellitus were associated with a slight increase in the concentration of MDA [42]. Similarly, Charkiewicz and colleagues (2021) demonstrated the increase of MDA in male subjects with hypertension. Taken together, these results suggest the role of oxidative stress in vascular endothelial dysfunction and raise the possibility of patients developing cardiovascular complications.
2.8. Malondialdehyde-Modified Low-Density Lipoprotein (MDA-LDL)
Malondialdehyde-modified low-density lipoprotein (MDA-LDL) is similar to ox-LDL and represents one of the major products of lipid peroxidation [43]. Research conducted by Amioka and colleagues (2019) revealed the association of high MDA-LDL levels with AMI compared to those with unstable angina. MDA-LDL was able to reflect the presence of vulnerable plaque and independently predict adverse cardiovascular events in ACS patients with successful non-surgical percutaneous coronary intervention (PCI). Not only that, the highest MDA-LDL group was associated with the early onset of ACS. This suggests that the young generation with ACS has poor lipid balance and high oxidative stress. Overall, MDA-LDL could be used as a potent predictor of cardiovascular outcomes and aid in stratifying ACS and AMI patients accordingly. Figure 1 represents oxidative stress-related biomarkers for cardiovascular disease, and studies appraised in this review are summarised in Table 1.

Table 1.
Summary of studies performed on oxidative stress biomarkers with cardiovascular disease.
3. Molecular Mechanisms of Pro- and Antioxidant towards CVD
Excessive pro-oxidant generation and a reduction in endogenous antioxidant status are associated with cardiovascular diseases, including mitochondrial dysfunction, dyslipidaemia, and genetic predisposition, i.e., autosome recessive hypercholesterolemia [46,47,48].
Intracellular ROS are formed as a by-product of electron transfer and are produced mainly by the mitochondrial respiratory chain. The principal generators of ROS within the respiratory chain are complexes I (NADH: ubiquinone oxidoreductase) and III (ubiquinol: cytochrome c oxidoreductase) [49]. To control the oxidative stress caused by mitochondrial ROS, it uses a complex network of ROS scavenging systems that act together to alleviate the stress. Superoxide dismutases (SODs) convert the highly reactive superoxide radical into hydrogen peroxide, which is then detoxified by GSH-PX and the PRX/Trx systems. Dyslipidaemia is defined as an elevated fasting and postprandial plasmatic concentration of total triglycerides and free fatty acids, with high levels of low-density lipoproteins (LDL) and low levels of high-density lipoproteins (HDL) [50]. Overproduction of reactive oxygen species has been linked to lipid metabolism disorders and is demonstrated to impact the antioxidant state of several organs and lipoprotein levels [51]. Increased superoxide production has been observed in hypercholesterolemic animal models. An increased NADPH oxidase activity is commonly seen as the principal source of superoxide [52,53]. Increased NOX4 transcript levels in hypercholesterolemic animal models are also observed due to transcriptional, posttranscriptional, or epigenetic NOX4 expression regulation [54].
Familial hypercholesterolemia (FH) is an autosomal dominant genetic disorder caused by loss of function, which results in the repression of protein synthesis, causing an extremely high level of low-density lipoprotein cholesterol (LDL-C) leads to atherosclerotic cardiovascular disease [55,56]. In FH patients, oxidative stress is a major factor in the onset and development of atherosclerosis. It is reported that hypercholesterolemia causes the production of superoxide radicals, which inhibits the activity of endothelial nitric oxide synthase (eNOS), lowering NO bioavailability as an antioxidant resulting in an inflammatory response in the artery wall [57,58].
4. Clinical Significance of Oxidative Stress Parameters Associated with CVD
Biomarker development for prognostic or predictive of CVD is critical for the evolution of treatment options [59]. Several effective research attempts have been conducted to determine the efficacy of various oxidative stress biomarkers. Antioxidants such as thiol are being investigated as a tool for avoiding oxidative stress in cells. It is reported that thiols transform into reversible disulphide structures during oxidative stress and are then reduced back to thiol groups when the oxidative stress is removed. A study by Stoppa-Vaucher and colleagues (2012) investigating teenagers with essential hypertension reported higher disulphide levels indicating increased oxidative stress [60]. In addition, another study comparing the body mass index of matched controls showed that children with hypertension had a worse antioxidative capability due to considerable glutathione depletion [61]. Adipokines such as the Interleukins are also reported as an oxidative biomarker for determining CVD risk [62,63,64]. Type 1 diabetes mellitus is reported as the major risk factor for accelerated atherosclerosis and vascular problems [65]. This data highlights the importance of proper inflammatory monitoring towards efficient interventions. Novel biomarkers, such as urine-tocopherol, a vitamin E metabolite, are being researched as they are considerably higher in children with type 1 diabetes [66].
5. Insights into ROS Detection Technology
The detection of reactive oxygen species (ROS) has attracted interest in academic, medical, and industrial settings, particularly in elucidating its pathological mechanism and diagnosis [67]. To date, there are no universal methods for detecting ROS directly and consistently; the electron spin resonance (ESR) [68,69], mass spectrometry (MS) [70], spectrophotometry [71,72], high-performance liquid chromatography (HPLC) [73], fluorescence spectroscopy [74], and electrochemical techniques have been elucidated as an effective technique. Recent advancements in screening technologies enabled the development and enhancements of these technologies. A recent study by Jiang and colleagues (2022) developed a high-throughput fluorescent sensors to detect H2O2 in live cancer cells [75]. Another recent study by Miripour and colleagues (2022) detected the presence of ROS/H2O2 in the peripheral blood of cancer patients using a real-time electrochemical test [76]. The researchers successfully identified ROS/H2O2 levels, indicating that these techniques could possibly use for detecting of ROS in CVD.
6. Challenges and Limitations in Targeting Oxidative Stress and CVD Biomarker
Oxidative stress contributed to the progression of various CVD, but controversy flared up with the application of antioxidant therapies in human clinical trials [77]. The effectiveness of antioxidants is generally influenced by the involvement of specific oxidants in disease pathology [78]. Mostly, oxidative stress plays a secondary role in disease causation, and, hence, targeting oxidative stress may not be entirely beneficial to disease progression. The short lifespan of ROS remains the main challenge and makes them difficult to measure accurately [79]. While approaches using the molecule that emits fluorescence such as dihydroethidium (DHE) and MitoSOX have been developed to detect ROS, their sensitivity and specificity results were discouraging since these molecules also appear in other non-specific redox reactions [46]. More novel approaches or validation studies with large human clinical trials focusing on current existing oxidant biomarkers are highly anticipated in breaking through the seemingly dead-end situation.
7. Conclusions
ROS represents a pivotal function in the cardiovascular system, but overproduction of ROS may exceed the capacity of the antioxidant defence systems, causing oxidative stress and inducing adverse cardiovascular outcomes. Despite the emerging attention on oxidant biomarkers as crucial adjuncts in diagnostic and prognostic usage, there is still a long way for their validation in clinical application. More work is required in large clinical trials to demonstrate the value of oxidant markers in addition to the established models of cardiovascular risk prediction. This study presenting oxidant biomarkers potential may guide future efforts for early cardiovascular diagnosis and provide clinical benefit for patients. Future research should focus on the identification of improved biomarkers that integrate the functionality of these biomarkers into a standardised clinical chemistry test.
Author Contributions
Conceptualisation, M.S. and K.S.L.; data curation, A.S.-Y.K.; writing—original draft preparation, A.S.-Y.K. and C.-W.H.; writing—review and editing, M.S., S.H.E.L. and J.Y.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 13 April 2022).
- Dai, H.; Much, A.A.; Maor, E.; Asher, E.; Younis, A.; Xu, Y.; Lu, Y.; Liu, X.; Shu, J.; Bragazzi, N.L. Global, regional, and national burden of ischaemic heart disease and its attributable risk factors, 1990–2017: Results from the Global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 8, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.M.; Maltagliati, A.J. Nrf2 at the heart of oxidative stress and cardiac protection. Physiol. Genom. 2018, 50, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Daiber, A.; Hahad, O.; Andreadou, I.; Steven, S.; Daub, S.; Münzel, T. Redox-related biomarkers in human cardiovascular disease-classical footprints and beyond. Redox Biol. 2021, 42, 101875. [Google Scholar] [CrossRef] [PubMed]
- Tsutsui, H.; Kinugawa, S.; Matsushima, S. Oxidative stress and heart failure. Am. J. Physiol. Heart Circ. Physiol. 2011, 301, H2181–H2190. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, M.I.; Romano, M.; Basarali, M.K.; Elzagallaai, A.; Karaman, M.; Demir, Z.; Demir, M.F.; Akcay, F.; Seyrek, M.; Haksever, N.; et al. The Effect of Corrected Inflammation, Oxidative Stress and Endothelial Dysfunction on Fmd Levels in Patients with Selected Chronic Diseases: A Quasi-Experimental Study. Sci. Rep. 2020, 10, 9018. [Google Scholar] [CrossRef] [PubMed]
- Sies, H.; Berndt, C.; Jones, D.P. Oxidative Stress. Annu. Rev. Biochem. 2017, 86, 715–748. [Google Scholar] [CrossRef]
- Ramachandra, C.J.A.; Cong, S.; Chan, X.; Yap, E.P.; Yu, F.; Hausenloy, D.J. Oxidative stress in cardiac hypertrophy: From molecular mechanisms to novel therapeutic targets. Free Radic. Biol. Med. 2021, 166, 297–312. [Google Scholar] [CrossRef]
- Mangge, H.; Becker, K.; Fuchs, D.; Gostner, J.M. Antioxidants, inflammation and cardiovascular disease. World J. Cardiol. 2014, 6, 462–477. [Google Scholar] [CrossRef]
- Aimo, A.; Castiglione, V.; Borrelli, C.; Saccaro, L.F.; Franzini, M.; Masi, S.; Emdin, M.; Giannoni, A. Oxidative stress and inflammation in the evolution of heart failure: From pathophysiology to therapeutic strategies. Eur. J. Prev. Cardiol. 2020, 27, 494–510. [Google Scholar] [CrossRef]
- Schmidt, H.H.; Stocker, R.; Vollbracht, C.; Paulsen, G.; Riley, D.; Daiber, A.; Cuadrado, A. Antioxidants in Translational Medicine. Antioxid. Redox Signal. 2015, 23, 1130–1143. [Google Scholar] [CrossRef]
- Mathew, A.V.; Li, L.; Byun, J.; Guo, Y.; Michailidis, G.; Jaiswal, M.; Chen, Y.E.; Pop-Busui, R.; Pennathur, S. Therapeutic Lifestyle Changes Improve HDL Function by Inhibiting Myeloperoxidase-Mediated Oxidation in Patients with Metabolic Syndrome. Diabetes Care 2018, 41, 2431–2437. [Google Scholar] [CrossRef] [PubMed]
- Ramachandra, C.J.A.; Kp, M.M.J.; Chua, J.; Hernandez-Resendiz, S.; Liehn, E.A.; Knöll, R.; Gan, L.-M.; Michaëlsson, E.; Jonsson, M.K.B.; Ryden-Markinhuhta, K.; et al. Inhibiting cardiac myeloperoxidase alleviates the relaxation defect in hypertrophic cardiomyocytes. Cardiovasc. Res. 2022, 118, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Chuang, C.Y.; Vanichkitrungruang, S.; Hawkins, C.L.; Davies, M.J. Hypochlorous acid-modified extracellular matrix contributes to the behavioral switching of human coronary artery smooth muscle cells. Free Radic. Biol. Med. 2019, 134, 516–526. [Google Scholar] [CrossRef] [PubMed]
- Afshinnia, F.; Zeng, L.; Byun, J.; Gadegbeku, C.A.; Magnone, M.C.; Whatling, C.; Valastro, B.; Kretzler, M.; Pennathur, S.; Michigan Kidney Translational Core, C.I.G. Myeloperoxidase Levels and Its Product 3-Chlorotyrosine Predict Chronic Kidney Disease Severity and Associated Coronary Artery Disease. Am. J. Nephrol. 2017, 46, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.S.; Kim, H.B.; Szuchman-Sapir, A.; McMahon, A.; Dennis, J.M.; Witting, P.K. Neutrophils recruited to the myocardium after acute experimental myocardial infarct generate hypochlorous acid that oxidizes cardiac myoglobin. Arch. Biochem. Biophys. 2016, 612, 103–114. [Google Scholar] [CrossRef]
- Wang, G.; Mathew, A.V.; Yu, H.; Li, L.; He, L.; Gao, W.; Liu, X.; Guo, Y.; Byun, J.; Zhang, J.; et al. Myeloperoxidase mediated HDL oxidation and HDL proteome changes do not contribute to dysfunctional HDL in Chinese subjects with coronary artery disease. PLoS ONE 2018, 13, e0193782. [Google Scholar] [CrossRef]
- Premkumar, J.; Sampath, P.; Sanjay, R.; Chandrakala, A.; Rajagopal, D. Synthetic Guaiacol Derivatives as Promising Myeloperoxidase Inhibitors Targeting Atherosclerotic Cardiovascular Disease. ChemMedChem 2020, 15, 1187–1199. [Google Scholar] [CrossRef]
- Ramachandra, C.J.A.; Ja, K.; Chua, J.; Cong, S.; Shim, W.; Hausenloy, D.J. Myeloperoxidase As a Multifaceted Target for Cardiovascular Protection. Antioxid. Redox Signal. 2020, 32, 1135–1149. [Google Scholar] [CrossRef]
- Soubhye, J.; Van Antwerpen, P.; Dufrasne, F. A patent review of myeloperoxidase inhibitors for treating chronic inflammatory syndromes (focus on cardiovascular diseases, 2013–2019). Expert Opin. Ther. Pat. 2020, 30, 595–608. [Google Scholar] [CrossRef]
- Omran, M.M.; Zahran, F.M.; Kadry, M.; Belal, A.A.M.; Emran, T.M. Role of myeloperoxidase in early diagnosis of acute myocardial infarction in patients admitted with chest pain. J. Immunoass. Immunochem. 2018, 39, 337–347. [Google Scholar] [CrossRef]
- Calmarza, P.; Lapresta, C.; Martínez, M.; Lahoz, R.; Povar, J. Utility of myeloperoxidase in the differential diagnosis of acute coronary syndrome. Arch. Cardiol. México 2018, 88, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Charkiewicz, A.E.; Garley, M.; Ratajczak-Wrona, W.; Nowak, K.; Jabłońska, E.; Maślach, D.; Omeljaniuk, W.J. Profile of new vascular damage biomarkers in middle-aged men with arterial hypertension. Adv. Med. Sci. 2021, 66, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Wang, J.-X.; Wu, X.-Y.; Cui, Y.; Zou, Z.-H.; Liu, Y.; Gao, J. Correlation Analysis of Plasma Myeloperoxidase Level with Global Registry of Acute Coronary Events Score and Prognosis in Patients with Acute Non-ST-Segment Elevation Myocardial Infarction. Front. Med. 2022, 9, 828174. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Li, L.; Chen, W.; Xu, S.; Feng, X.; Zhang, L. Natural products: The role and mechanism in low-density lipoprotein oxidation and atherosclerosis. Phytother. Res. 2021, 35, 2945–2967. [Google Scholar] [CrossRef]
- Hartley, A.; Haskard, D.; Khamis, R. Oxidized LDL and anti-oxidized LDL antibodies in atherosclerosis—Novel insights and future directions in diagnosis and therapy. Trends Cardiovasc. Med. 2019, 29, 22–26. [Google Scholar] [CrossRef]
- Ho, E.; Karimi Galougahi, K.; Liu, C.-C.; Bhindi, R.; Figtree, G.A. Biological markers of oxidative stress: Applications to cardiovascular research and practice. Redox Biol. 2013, 1, 483–491. [Google Scholar] [CrossRef]
- Zhao, X.; Sun, D.; Xu, R.X.; Guo, Y.L.; Zhu, C.G.; Wu, N.Q.; Zhang, Y.; Li, S.; Gao, Y.; Liu, G.; et al. Low-density lipoprotein-associated variables and the severity of coronary artery disease: An untreated Chinese cohort study. Biomarkers 2018, 23, 647–653. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, H.W.; Xu, R.X.; Guo, Y.L.; Zhu, C.G.; Wu, N.Q.; Gao, Y.; Li, J.J. Oxidized-LDL is a useful marker for predicting the very early coronary artery disease and cardiovascular outcomes. Pers. Med. 2018, 15, 521–529. [Google Scholar] [CrossRef]
- Karimi Galougahi, K.; Antoniades, C.; Nicholls, S.J.; Channon, K.M.; Figtree, G.A. Redox biomarkers in cardiovascular medicine. Eur. Heart J. 2015, 36, 1576–1582. [Google Scholar] [CrossRef]
- Anderson, C.; Milne, G.L.; Park, Y.-M.M.; Sandler, D.P.; Nichols, H.B. Cardiovascular disease risk factors and oxidative stress among premenopausal women. Free Radic. Biol. Med. 2018, 115, 246–251. [Google Scholar] [CrossRef]
- Castro-Diehl, C.; Ehrbar, R.; Obas, V.; Oh, A.; Vasan, R.S.; Xanthakis, V. Biomarkers representing key aging-related biological pathways are associated with subclinical atherosclerosis and all-cause mortality: The Framingham Study. PLoS ONE 2021, 16, e0251308. [Google Scholar] [CrossRef] [PubMed]
- Xuan, Y.; Gào, X.; Holleczek, B.; Brenner, H.; Schöttker, B. Prediction of myocardial infarction, stroke and cardiovascular mortality with urinary biomarkers of oxidative stress: Results from a large cohort study. Int. J. Cardiol. 2018, 273, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Appel, D.; Böger, R.; Windolph, J.; Heinze, G.; Goetz, A.E.; Hannemann, J. Asymmetric dimethylarginine predicts perioperative cardiovascular complications in patients undergoing medium-to-high risk non-cardiac surgery. J. Int. Med. Res. 2020, 48, 300060520940450. [Google Scholar] [CrossRef] [PubMed]
- Cordts, K.; Seelig, D.; Lund, N.; Carrier, L.; Böger, R.H.; Avanesov, M.; Tahir, E.; Schwedhelm, E.; Patten, M. Association of Asymmetric Dimethylarginine and Diastolic Dysfunction in Patients with Hypertrophic Cardiomyopathy. Biomolecules 2019, 9, 277. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; Dai, Y.; Mao, H.; Zheng, W.; Zhang, J. Prognostic value of asymmetric dimethylarginine in patients with coronary artery disease: A meta-analysis. Nitric Oxide 2021, 109, 50–56. [Google Scholar] [CrossRef]
- Xu, H.; Chen, Z.; Shang, Q.H.; Gao, Z.Y.; Yu, C.A.; Shi, D.Z.; Chen, K.J. Asymmetric Dimethylarginine Predicts One-year Recurrent Cardiovascular Events: Potential Biomarker of “Toxin Syndrome” in Coronary Heart Disease. Chin. J. Integr. Med. 2019, 25, 327–333. [Google Scholar] [CrossRef]
- Xuan, Y.; Bobak, M.; Anusruti, A.; Jansen, E.; Pająk, A.; Tamosiunas, A.; Saum, K.U.; Holleczek, B.; Gao, X.; Brenner, H.; et al. Association of serum markers of oxidative stress with myocardial infarction and stroke: Pooled results from four large European cohort studies. Eur. J. Epidemiol. 2019, 34, 471–481. [Google Scholar] [CrossRef]
- Erdoğan, M.; Polat, M.; Çelik, M.C.; Öztürk, S.; Baştuğ, S.; Özbebek, Y.E.; Neşelioğlu, S.; Akçay, M. Oxidative stress parameters in patients with ascending aortic dilatation. Turk. J. Med. Sci. 2020, 50, 1323–1329. [Google Scholar] [CrossRef]
- Nishihara, T.; Yamamoto, E.; Sueta, D.; Fujisue, K.; Usuku, H.; Oike, F.; Takae, M.; Tabata, N.; Ito, M.; Yamanaga, K.; et al. Impact of Reactive Oxidative Metabolites Among New Categories of Nonischemic Heart Failure. J. Am. Heart Assoc. 2021, 10, e016765. [Google Scholar] [CrossRef]
- Romuk, E.; Wojciechowska, C.; Jacheć, W.; Zemła-Woszek, A.; Momot, A.; Buczkowska, M.; Rozentryt, P. Malondialdehyde and Uric Acid as Predictors of Adverse Outcome in Patients with Chronic Heart Failure. Oxidative Med. Cell. Longev. 2019, 2019, 9246138. [Google Scholar] [CrossRef]
- Boarescu, P.-M.; Boarescu, I.; Pop, R.M.; Roşian, Ş.H.; Bocșan, I.C.; Rus, V.; Mada, R.O.; Popa, I.D.; Neagu, N.; Bulboacă, A.E.; et al. Evaluation of Oxidative Stress Biomarkers, Pro-Inflammatory Cytokines, and Histological Changes in Experimental Hypertension, Dyslipidemia, and Type 1 Diabetes Mellitus. Int. J. Mol. Sci. 2022, 23, 1438. [Google Scholar] [CrossRef] [PubMed]
- Amioka, N.; Miyoshi, T.; Otsuka, H.; Yamada, D.; Takaishi, A.; Ueeda, M.; Hirohata, S.; Ito, H. Serum malondialdehyde-modified low-density lipoprotein levels on admission predict prognosis in patients with acute coronary syndrome undergoing percutaneous coronary intervention. J. Cardiol. 2019, 74, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Wang, X.C.; Luo, Z.D.; Hu, G.Q.; Ma, M.Q.; Liang, Y.; Xu, B.L.; Lin, X.H. LncRNA HOXA11-AS promotes vascular endothelial cell injury in atherosclerosis by regulating the miR-515-5p/ROCK1 axis. ESC Heart Fail. 2022. [Google Scholar] [CrossRef] [PubMed]
- Araujo, F.B.; Barbosa, D.S.; Hsin, C.Y.; Maranhão, R.C.; Abdalla, D.S. Evaluation of oxidative stress in patients with hyperlipidemia. Atherosclerosis 1995, 117, 61–71. [Google Scholar] [CrossRef]
- Biswas, S.K.; Lopes De Faria, J.B.; Biswas, S.K.; Lopes De Faria, J.B. Which comes first: Renal inflammation or oxidative stress in spontaneously hypertensive rats? Free Radic. Res. 2007, 41, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Bakker, S.J.; IJzerman, R.G.; Teerlink, T.; Westerhoff, H.V.; Gans, R.O.; Heine, R.J. Cytosolic triglycerides and oxidative stress in central obesity: The missing link between excessive atherosclerosis, endothelial dysfunction, and β-cell failure? Atherosclerosis 2000, 148, 17–21. [Google Scholar] [CrossRef]
- Peoples, J.N.; Saraf, A.; Ghazal, N.; Pham, T.T.; Kwong, J.Q. Mitochondrial dysfunction and oxidative stress in heart disease. Exp. Mol. Med. 2019, 51, 1–13. [Google Scholar] [CrossRef]
- Pellegrino, D. Antioxidants and Cardiovascular Risk Factors. Diseases 2016, 4, 11. [Google Scholar] [CrossRef]
- Singh, S.V.; Shrivastava, A.; Chaturvedi, U.; Singh, S.C.; Shanker, K.; Saxena, J.K.; Bhatia, G.; Pal, A. A mechanism-based pharmacological evaluation of efficacy of Flacourtia indica in management of dyslipidemia and oxidative stress in hyperlipidemic rats. J. Basic Clin. Physiol. Pharmacol. 2016, 27, 121–129. [Google Scholar] [CrossRef]
- Csont, T.; Bereczki, E.; Bencsik, P.; Fodor, G.; Görbe, A.; Zvara, Á.; Csonka, C.; Puskás, L.G.; Sántha, M.; Ferdinandy, P. Hypercholesterolemia increases myocardial oxidative and nitrosative stress thereby leading to cardiac dysfunction in apoB-100 transgenic mice. Cardiovasc. Res. 2007, 76, 100–109. [Google Scholar] [CrossRef]
- Varga, Z.V.; Kupai, K.; Szűcs, G.; Gáspár, R.; Pálóczi, J.; Faragó, N.; Zvara, Á.; Puskás, L.G.; Rázga, Z.; Tiszlavicz, L. MicroRNA-25-dependent up-regulation of NADPH oxidase 4 (NOX4) mediates hypercholesterolemia-induced oxidative/nitrative stress and subsequent dysfunction in the heart. J. Mol. Cell. Cardiol. 2013, 62, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Csonka, C.; Sárközy, M.; Pipicz, M.; Dux, L.; Csont, T. Modulation of Hypercholesterolemia-Induced Oxidative/Nitrative Stress in the Heart. Oxidative Med. Cell. Longev. 2016, 2016, 3863726. [Google Scholar] [CrossRef]
- Ganjali, S.; Keshavarz, R.; Hosseini, S.; Mansouri, A.; Mannarino, M.R.; Pirro, M.; Jamialahmadi, T.; Sahebkar, A. Evaluation of Oxidative Stress Status in Familial Hypercholesterolemia. J. Clin. Med. 2021, 10, 5867. [Google Scholar] [CrossRef]
- Petrulioniene, Z.; Gargalskaite, U.; Mikstiene, V.; Norvilas, R.; Skiauteryte, E.; Utkus, A. Autosomal recessive hypercholesterolemia: Case report. J. Clin. Lipidol. 2019, 13, 887–893. [Google Scholar] [CrossRef]
- Alamdari, D.H.; Ghayour-Mobarhan, M.; Tavallaie, S.; Parizadeh, M.R.; Moohebati, M.; Ghafoori, F.; Kazemi-Bajestani, S.M.R.; Paletas, K.; Pegiou, T.; Koliakos, G. Prooxidant–antioxidant balance as a new risk factor in patients with angiographically defined coronary artery disease. Clin. Biochem. 2008, 41, 375–380. [Google Scholar] [CrossRef]
- Stokes, K.Y.; Cooper, D.; Tailor, A.; Granger, D.N. Hypercholesterolemia promotes inflammation and microvascular dysfunction: Role of nitric oxide and superoxide. Free. Radic. Biol. Med. 2002, 33, 1026–1036. [Google Scholar] [CrossRef]
- Hertiš Petek, T.; Petek, T.; Močnik, M.; Marčun Varda, N. Systemic Inflammation, Oxidative Stress and Cardiovascular Health in Children and Adolescents: A Systematic Review. Antioxidants 2022, 11, 894. [Google Scholar] [CrossRef] [PubMed]
- Stoppa-Vaucher, S.; Dirlewanger, M.A.; Meier, C.A.; de Moerloose, P.; Reber, G.; Roux-Lombard, P.; Combescure, C.; Saudan, S.; Schwitzgebel, V.M. Inflammatory and prothrombotic states in obese children of European descent. Obesity 2012, 20, 1662–1668. [Google Scholar] [CrossRef] [PubMed]
- Śladowska-Kozłowska, J.; Litwin, M.; Niemirska, A.; Wierzbicka, A.; Roszczynko, M.; Szperl, M. Associations of the eNOS G894T gene polymorphism with target organ damage in children with newly diagnosed primary hypertension. Pediatr. Nephrol. 2015, 30, 2189–2197. [Google Scholar] [CrossRef][Green Version]
- Olza, J.; Aguilera, C.M.; Gil-Campos, M.; Leis, R.; Bueno, G.; Valle, M.; Cañete, R.; Tojo, R.; Moreno, L.A.; Gil, Á. A continuous metabolic syndrome score is associated with specific biomarkers of inflammation and CVD risk in prepubertal children. Ann. Nutr. Metab. 2015, 66, 72–79. [Google Scholar] [CrossRef]
- González-Jiménez, E.; Schmidt-Riovalle, J.; Sinausía, L.; Carmen Valenza, M.; Perona, J.S. Predictive value of ceruloplasmin for metabolic syndrome in adolescents. Biofactors 2016, 42, 163–170. [Google Scholar] [PubMed]
- Kelly, A.S.; Steinberger, J.; Kaiser, D.R.; Olson, T.P.; Bank, A.J.; Dengel, D.R. Oxidative stress and adverse adipokine profile characterize the metabolic syndrome in children. J. Cardiometab. Syndr. 2006, 1, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Seckin, D.; Ilhan, N.; Ilhan, N.; Ertugrul, S. Glycaemic control, markers of endothelial cell activation and oxidative stress in children with type 1 diabetes mellitus. Diabetes Res. Clin. Pract. 2006, 73, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Muller, D.P.; O’Riordan, S.M.; Bryan, S.; Dattani, M.T.; Hindmarsh, P.C.; Mills, K. Urinary conjugated α-tocopheronolactone—A biomarker of oxidative stress in children with type 1 diabetes. Free Radic. Biol. Med. 2013, 55, 54–62. [Google Scholar] [CrossRef][Green Version]
- Duanghathaipornsuk, S.; Farrell, E.J.; Alba-Rubio, A.C.; Zelenay, P.; Kim, D.-S. Detection Technologies for Reactive Oxygen Species: Fluorescence and Electrochemical Methods and Their Applications. Biosensors 2021, 11, 30. [Google Scholar] [CrossRef]
- He, W.; Liu, Y.; Wamer, W.G.; Yin, J.-J. Electron spin resonance spectroscopy for the study of nanomaterial-mediated generation of reactive oxygen species. J. Food Drug Anal. 2014, 22, 49–63. [Google Scholar] [CrossRef]
- Utsumi, H.; Yasukawa, K.; Soeda, T.; Yamada, K.-I.; Shigemi, R.; Yao, T.; Tsuneyoshi, M. Noninvasive mapping of reactive oxygen species by in vivo electron spin resonance spectroscopy in indomethacin-induced gastric ulcers in rats. J. Pharmacol. Exp. Ther. 2006, 317, 228–235. [Google Scholar] [CrossRef]
- Barbin, L.E.; Saquy, P.C.; Guedes, D.F.C.; Sousa-Neto, M.D.; Estrela, C.; Pécora, J.D. Determination of para-chloroaniline and reactive oxygen species in chlorhexidine and chlorhexidine associated with calcium hydroxide. J. Endod. 2008, 34, 1508–1514. [Google Scholar] [CrossRef]
- Blaškovičová, J.; Sochr, J.; Koutsogiannis, A.; Diamantidou, D.; Kopel, P.; Adam, V.; Labuda, J. Detection of ROS Generated by UV-C Irradiation of CdS Quantum Dots and their Effect on Damage to Chromosomal and Plasmid DNA. Electroanalysis 2018, 30, 698–704. [Google Scholar] [CrossRef]
- Martínez, S.R.; Miana, G.E.; Albesa, I.; Mazzieri, M.R.; Becerra, M.C. Evaluation of antibacterial activity and reactive species generation of n-benzenesulfonyl derivatives of heterocycles. Chem. Pharm. Bull. 2016, 64, 135–141. [Google Scholar] [CrossRef]
- Kalyanaraman, B.; Cheng, G.; Hardy, M.; Ouari, O.; Bennett, B.; Zielonka, J. Teaching the basics of reactive oxygen species and their relevance to cancer biology: Mitochondrial reactive oxygen species detection, redox signaling, and targeted therapies. Redox Biol. 2018, 15, 347–362. [Google Scholar] [CrossRef] [PubMed]
- Wojtala, A.; Bonora, M.; Malinska, D.; Pinton, P.; Duszynski, J.; Wieckowski, M. Methods in Enzymology Conceptual Background and Bioenergetic/Mitochondrial Aspects of Oncometabolism; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Jiang, S.; Yang, J.; Ling, L.; Wang, S.; Ma, D. Supramolecular Fluorescent Probes for the Detection of Reactive Oxygen Species Discovered via High-Throughput Screening. Anal. Chem. 2022, 94, 5634–5641. [Google Scholar] [CrossRef] [PubMed]
- Miripour, Z.S.; Aminifar, M.; Akbari, M.E.; Abbasvandi, F.; Miraghaie, S.H.; Hoseinpour, P.; Javadi, M.R.; Dabbagh, N.; Mohajerzadeh, L.; Aghdam, M.K.; et al. Electrochemical measuring of reactive oxygen species levels in the blood to detect ratio of high-density neutrophils, suitable to alarm presence of cancer in suspicious cases. J. Pharm. Biomed. Anal. 2022, 209, 114488. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Kang, P.M. Oxidative Stress and Antioxidant Treatments in Cardiovascular Diseases. Antioxidants 2020, 9, 1292. [Google Scholar] [CrossRef] [PubMed]
- Forman, H.J.; Zhang, H. Targeting oxidative stress in disease: Promise and limitations of antioxidant therapy. Nat. Rev. Drug Discov. 2021, 20, 689–709. [Google Scholar] [CrossRef] [PubMed]
- Senoner, T.; Dichtl, W. Oxidative Stress in Cardiovascular Diseases: Still a Therapeutic Target? Nutrients 2019, 11, 2090. [Google Scholar] [CrossRef] [PubMed]
- Shields, H.J.; Traa, A.; Van Raamsdonk, J.M. Beneficial and Detrimental Effects of Reactive Oxygen Species on Lifespan: A Comprehensive Review of Comparative and Experimental Studies. Front. Cell Dev. Biol. 2021, 9, 628157. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).