Heavy Metals and Essential Elements in Association with Oxidative Stress in Women with Polycystic Ovary Syndrome—A Systematic Review
Abstract
:1. Introduction
1.1. PCOS and Chronic Inflammation
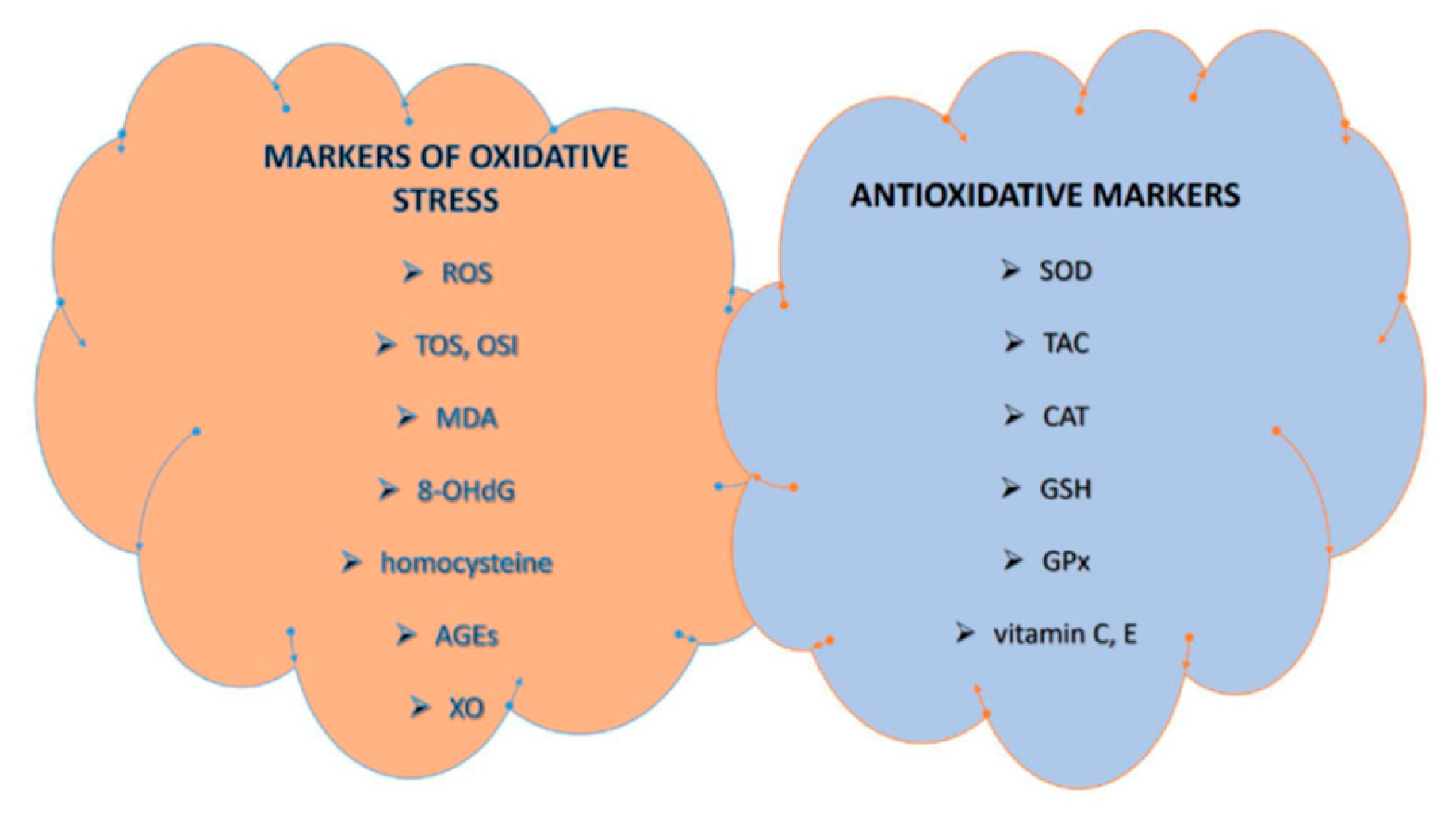
1.2. PCOS and Oxidative Stress
1.3. PCOS, Metal Exposure and Oxidative Stress
1.3.1. Heavy Metals
1.3.2. Essential Elements
2. Materials and Methods
2.1. Literature Identification
2.2. The Inclusion and Exclusion Criteria
2.3. Data Extraction
3. Results
3.1. Literature Search
3.2. Association of Heavy Metals and Essential Elements with Oxidative Stress in Women with PCOS
3.2.1. Heavy Metals and Oxidative Stress in Women with PCOS
3.2.2. Essential Elements and Oxidative Stress in Women with PCOS
4. Discussion
4.1. Heavy Metals and Oxidative Stress in Women with PCOS
4.2. Essential Elements and Oxidative Stress in Women with PCOS
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azziz, R.; Woods, K.S.; Reyna, R.; Key, T.J.; Knochenhauer, E.S.; Yildiz, B.O. The prevalence and features of the polycystic ovary syndrome in an unselected population. J. Clin. Endocrinol. Metab. 2004, 89, 2745–2749. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, R.; Sharma, S.; Bekir, J.; Conway, G.; Bailey, J.; Balen, A.H.; Prelevic, G. Prevalence of polycystic ovaries and polycystic ovary syndrome in lesbian women compared with heterosexual women. Fertil. Steril. 2004, 82, 1352–1357. [Google Scholar] [CrossRef]
- Murri, M.; Luque-Ramírez, M.; Insenser, M.; Ojeda-Ojeda, M.; Escobar-Morreale, H.F. Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): A systematic review and meta-analysis. Hum. Reprod. Update 2013, 19, 268–288. [Google Scholar] [CrossRef]
- Rudnicka, E.; Suchta, K.; Grymowicz, M.; Calik-Ksepka, A.; Smolarczyk, K.; Duszewska, A.M.; Smolarczyk, R.; Meczekalski, B. Chronic low grade inflammation in pathogenesis of PCOS. Int. J. Mol Sci. 2021, 22, 3789. [Google Scholar] [CrossRef]
- Abraham Gnanadass, S.; Divakar Prabhu, Y.; Valsala Gopalakrishnan, A. Association of metabolic and inflammatory markers with polycystic ovarian syndrome (PCOS): An update. Arch. Gynecol. Obstet. 2021, 303, 631–643. [Google Scholar] [CrossRef] [PubMed]
- Duleba, A.J.; Dokras, A. Is PCOS an inflammatory process? Fertil. Steril. 2012, 97, 7–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González, F.; Rote, N.S.; Minium, J.; Kirwan, J.P. Reactive oxygen species-induced oxidative stress in the development of insulin resistance and hyperandrogenism in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 336–340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, W.; Liu, C.; Yang, Q.; Zhou, Y.; Liu, M.; Shan, H. Oxidative stress and antioxidant imbalance in ovulation disorder in patients with polycystic ovary syndrome. Front. Nutr. 2022, 9, 1018674. [Google Scholar] [CrossRef]
- Sulaiman, M.A.; Al-Farsi, Y.M.; Al-Khaduri, M.M.; Saleh, J.; Waly, M.I. Polycystic ovarian syndrome is linked to increased oxidative stress in Omani women. Int. J. Womens Health 2018, 10, 763–771. [Google Scholar] [CrossRef] [Green Version]
- Lu, J.; Wang, Z.; Cao, J.; Chen, Y.; Dong, Y. A novel and compact review on the role of oxidative stress in female reproduction. Reprod. Biol. Endocrinol. 2018, 16, 80. [Google Scholar] [CrossRef] [Green Version]
- Nawrocka-Rutkowska, J.; Szydłowska, I.; Jakubowska, K.; Olszewska, M.; Chlubek, D.; Rył, A.; Szczuko, M.; Starczewski, A. Assessment of the parameters of oxidative stress depending on the metabolic and anthropometric status indicators in women with PCOS. Life 2022, 12, 225. [Google Scholar] [CrossRef]
- Zuo, T.; Zhu, M.; Xu, W. Roles of oxidative stress in polycystic ovary syndrome and cancers. Oxid. Med. Cell Longev. 2016, 2016, 8589318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uçkan, K.; Demir, H.; Turan, K.; Sarıkaya, E.; Demir, C. Role of oxidative stress in obese and nonobese PCOS patients. Int. J. Clin. Pract. 2022, 2022, 4579831. [Google Scholar] [CrossRef]
- Desai, V.; Prasad, N.R.; Manohar, S.M.; Sachan, A.; Narasimha, S.R.; Bitla, A.R. Oxidative stress in non-obese women with polycystic ovarian syndrome. J. Clin. Diagn. Res. 2014, 8, CC01–CC03. [Google Scholar] [CrossRef]
- Liang, J.; Gao, Y.; Feng, Z.; Zhang, B.; Na, Z.; Li, D. Reactive oxygen species and ovarian diseases: Antioxidant strategies. Redox Biol. 2023, 62, 102659. [Google Scholar] [CrossRef]
- Drejza, M.A.; Rylewicz, K.; Majcherek, E.; Gross-Tyrkin, K.; Mizgier, M.; Plagens-Rotman, K.; Wójcik, M.; Panecka-Mysza, K.; Pisarska-Krawczyk, M.; Kędzia, W.; et al. Markers of oxidative stress in obstetrics and gynaecology- a systematic literature review. Antioxidants 2022, 11, 1477. [Google Scholar] [CrossRef]
- Mohammadi, M. Oxidative stress and polycystic ovary syndrome: A brief review. Int. J. Prev. Med. 2019, 10, 86. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yu, Z.; Zhao, S.; Cheng, L.; Man, Y.; Gao, X.; Zhao, H. Oxidative stress markers in the follicular fluid of patients with polycystic ovary syndrome correlate with a decrease in embryo quality. J. Assist. Reprod. Genet. 2021, 38, 471–477. [Google Scholar] [CrossRef]
- Kurdoglu, Z.; Kurdoglu, M.; Demir, H.; Sahin, H.G. Serum trace elements and heavy metals in polycystic ovary syndrome. Hum. Exp. Toxicol. 2012, 31, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Obasi, C.N.; Frazzoli, C.; Orisakwe, O.E. Heavy metals and metalloids exposure and in vitro fertilization: Critical concerns in human reproductive medicine. Front. Reprod. Health 2022, 4, 1037379. [Google Scholar] [CrossRef]
- Padilla, M.A.; Elobeid, M.; Ruden, D.M.; Allison, D.B. An examination of the association of selected toxic metals with total and central obesity indices: NHANES 99-02. Int. J. Environ. Res. Public Health 2010, 7, 3332–3347. [Google Scholar] [CrossRef]
- Chen, Y.W.; Yang, C.Y.; Huang, C.F.; Hung, D.Z.; Leung, Y.M.; Liu, S.H. Heavy metals, islet function and diabetes development. Islets 2009, 1, 169–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, G.; Wang, L.; Guo, Z.; Sun, L.; Wang, L.; Wang, C.; Zuo, Z.; Qiu, H. Association of serum heavy metals and trace element concentrations with reproductive hormone levels and polycystic ovary syndrome in a Chinese population. Biol. Trace Elem. Res. 2015, 167, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Hong, X.; Ma, J.; Bu, Y.; Liu, R. Serum trace elements in patients with polycystic ovary syndrome: A systematic review and meta-analysis. Front. Endocrinol. 2020, 11, 572384. [Google Scholar] [CrossRef] [PubMed]
- Spritzer, P.M.; Lecke, S.B.; Fabris, V.C.; Ziegelmann, P.K.; Amaral, L. Blood trace element concentrations in polycystic ovary syndrome: Systematic review and meta-analysis. Biol. Trace Elem. Res. 2017, 175, 254–262. [Google Scholar] [CrossRef]
- Iavicoli, I.; Fontana, L.; Bergamaschi, A. The effects of metals as endocrine disruptors. J. Toxicol. Environ. Health B Crit. Rev. 2009, 12, 206–223. [Google Scholar] [CrossRef]
- Jackson, L.W.; Howards, P.P.; Wactawski-Wende, J.; Schisterman, E.F. The association between cadmium, lead and mercury blood levels and reproductive hormones among healthy, premenopausal women. Hum. Reprod. 2011, 26, 2887–2895. [Google Scholar] [CrossRef] [Green Version]
- da Costa, C.S.; Oliveira, T.F.; Freitas-Lima, L.C.; Padilha, A.S.; Krause, M.; Carneiro, M.T.W.D.; Salgado, B.S.; Graceli, J.B. Subacute cadmium exposure disrupts the hypothalamic-pituitary-gonadal axis, leading to polycystic ovarian syndrome and premature ovarian failure features in female rats. Environ. Pollut. 2021, 269, 116154. [Google Scholar] [CrossRef]
- Wu, M.M.; Chiou, H.Y.; Wang, T.W.; Hsueh, Y.M.; Wang, I.H.; Chen, C.J.; Lee, T.C. Association of blood arsenic levels with increased reactive oxidants and decreased antioxidant capacity in a human population of northeastern Taiwan. Environ. Health Perspect. 2001, 109, 1011–1017. [Google Scholar] [CrossRef]
- Roy, C.; Tremblay, P.Y.; Ayotte, P. Is mercury exposure causing diabetes, metabolic syndrome and insulin resistance? A systematic review of the literature. Environ. Res. 2017, 156, 747–760. [Google Scholar] [CrossRef]
- Sundar, S.; Chakravarty, J. Antimony toxicity. Int. J. Environ. Res. Public Health 2010, 7, 4267–4277. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, D.; Iavicoli, I.; Setini, A.; Marinaccio, A.; Perniconi, B.; Carelli, G.; Iavicoli, S. Genotoxic risk and oxidative DNA damage in workers exposed to antimony trioxide. Environ. Mol. Mutagen. 2002, 40, 184–189. [Google Scholar] [CrossRef]
- Belzile, N.; Chen, Y.W. Tellurium in the environment: A critical review focused on natural waters, soils, sediments and airborne particles. Appl. Geochem. 2015, 63, 83–92. [Google Scholar] [CrossRef]
- Cunha, R.L.; Gouvea, I.E.; Juliano, L. A glimpse on biological activities of tellurium compounds. An. Acad. Bras. Cienc. 2009, 81, 393–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, X.; Pan, W.; Zhu, Z.; Ye, X.; Li, C.; Zhou, J.; Liu, J. A case-control study of thallium exposure with the risk of premature ovarian insufficiency in women. Arch. Environ. Occup. Health 2022, 77, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Hanzel, C.E.; Verstraeten, S.V. Thallium induces hydrogen peroxide generation by impairing mitochondrial function. Toxicol. Appl. Pharmacol. 2006, 216, 485–492. [Google Scholar] [CrossRef]
- Friedova, N.; Pelclova, D.; Obertova, N.; Lach, K.; Kesslerova, K.; Kohout, P. Osmium absorption after osmium tetroxide skin and eye exposure. Basic Clin. Pharmacol. Toxicol. 2020, 127, 429–433. [Google Scholar] [CrossRef]
- Pieczyńska, J.; Grajeta, H. The role of selenium in human conception and pregnancy. J. Trace Elem. Med. Biol. 2015, 29, 31–38. [Google Scholar] [CrossRef]
- Lu, J.; Holmgren, A. Selenoproteins. J. Biol. Chem. 2009, 284, 723–727. [Google Scholar] [CrossRef] [Green Version]
- Jamilian, M.; Razavi, M.; Fakhrie Kashan, Z.; Ghandi, Y.; Bagherian, T.; Asemi, Z. Metabolic response to selenium supplementation in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Clin. Endocrinol. 2015, 82, 885–891. [Google Scholar] [CrossRef]
- ElObeid, T.; Awad, M.O.; Ganji, V.; Moawad, J. The Impact of mineral supplementation on polycystic ovarian syndrome. Metabolites 2022, 12, 338. [Google Scholar] [CrossRef]
- Babapour, M.; Mohammadi, H.; Kazemi, M.; Hadi, A.; Rezazadegan, M.; Askari, G. Associations between serum magnesium concentrations and polycystic ovary syndrome status: A systematic review and meta-analysis. Biol. Trace Elem. Res. 2021, 199, 1297–1305. [Google Scholar] [CrossRef] [PubMed]
- Kanafchian, M.; Mahjoub, S.; Esmaeilzadeh, S.; Rahsepar, M.; Mosapour, A. Status of serum selenium and zinc in patients with the polycystic ovary syndrome with and without insulin resistance. Middle East Fertil. Soc. J. 2017, 23, 241–245. [Google Scholar] [CrossRef]
- Bizoń, A.; Tchórz, A.; Madej, P.; Leśniewski, M.; Wójtowicz, M.; Piwowar, A.; Franik, G. The activity of superoxide dismutase, its relationship with the concentration of zinc and copper and the prevalence of rs2070424 superoxide dismutase gene in women with polycystic ovary syndrome-preliminary study. J. Clin. Med. 2022, 11, 2548. [Google Scholar] [CrossRef] [PubMed]
- Ebisch, I.M.; Thomas, C.M.; Peters, W.H.; Braat, D.D.; Steegers-Theunissen, R.P. The importance of folate, zinc and antioxidants in the pathogenesis and prevention of subfertility. Hum. Reprod. Update 2007, 13, 163–174. [Google Scholar] [CrossRef]
- Chakraborty, P.; Ghosh, S.; Goswami, S.K.; Kabir, S.N.; Chakravarty, B.; Jana, K. Altered trace mineral milieu might play an aetiological role in the pathogenesis of polycystic ovary syndrome. Biol. Trace Elem. Res. 2013, 152, 9–15. [Google Scholar] [CrossRef]
- Li, M.; Tang, Y.; Lin, C.; Huang, Q.; Lei, D.; Hu, Y. Serum macroelement and microelement concentrations in patients with polycystic ovary syndrome: A cross-sectional study. Biol. Trace Elem. Res. 2017, 176, 73–80. [Google Scholar] [CrossRef]
- Vincent, J.B. New evidence against chromium as an essential trace element. J. Nutr. 2017, 147, 2212–2219. [Google Scholar] [CrossRef] [Green Version]
- Jain, S.K.; Patel, P.; Rogier, K.; Jain, S.K. Trivalent chromium inhibits protein glycosylation and lipid peroxidation in high glucose-treated erythrocytes. Antioxid. Redox Signal. 2006, 8, 238–241. [Google Scholar] [CrossRef]
- Morvaridzadeh, M.; Estêvão, M.D.; Qorbani, M.; Heydari, H.; Hosseini, A.S.; Fazelian, S.; Belančić, A.; Persad, E.; Rezamand, G.; Heshmati, J. The effect of chromium intake on oxidative stress parameters: A systematic review and meta-analysis. J. Trace Elem. Med. Biol. 2022, 69, 126879. [Google Scholar] [CrossRef]
- Balali-Mood, M.; Naseri, K.; Tahergorabi, Z.; Khazdair, M.R.; Sadeghi, M. Toxic mechanisms of five heavy metals: Mercury, lead, chromium, cadmium, and arsenic. Front. Pharmacol. 2021, 12, 643972. [Google Scholar] [CrossRef] [PubMed]
- Ermak, G.; Davies, K.J. Calcium and oxidative stress: From cell signaling to cell death. Mol. Immunol. 2002, 38, 713–721. [Google Scholar] [CrossRef]
- Jain, S.K.; Micinski, D. Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes. Biochem. Biophys. Res. Commun. 2013, 437, 7–11. [Google Scholar] [CrossRef] [Green Version]
- Ayub, K.; Hallett, M.B. Ca2+ influx shutdown during neutrophil apoptosis: Importance and possible mechanism. Immunology 2004, 111, 8–12. [Google Scholar] [CrossRef]
- Köse, S.A.; Nazıroğlu, M. Selenium reduces oxidative stress and calcium entry through TRPV1 channels in the neutrophils of patients with polycystic ovary syndrome. Biol. Trace Elem. Res. 2014, 158, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Guler, I.; Himmetoglu, O.; Turp, A.; Erdem, A.; Erdem, M.; Onan, M.A.; Taskiran, C.; Taslipinar, M.Y.; Guner, H. Zinc and homocysteine levels in polycystic ovarian syndrome patients with insulin resistance. Biol. Trace Elem. Res. 2014, 158, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Foroozanfard, F.; Bahmani, F.; Talaee, R.; Monavari, M.; Asemi, Z. Effects of zinc supplementation on endocrine outcomes in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Biol. Trace Elem. Res. 2016, 170, 271–278. [Google Scholar] [CrossRef]
- Jamilian, M.; Bahmani, F.; Siavashani, M.A.; Mazloomi, M.; Asemi, Z.; Esmaillzadeh, A. The effects of chromium supplementation on endocrine profiles, biomarkers of inflammation, and oxidative stress in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Biol. Trace Elem. Res. 2016, 172, 72–78. [Google Scholar] [CrossRef]
- Razavi, M.; Jamilian, M.; Kashan, Z.F.; Heidar, Z.; Mohseni, M.; Ghandi, Y.; Bagherian, T.; Asemi, Z. Selenium supplementation and the effects on reproductive outcomes, biomarkers of inflammation, and oxidative stress in women with polycystic ovary syndrome. Horm. Metab. Res. 2016, 48, 185–190. [Google Scholar] [CrossRef]
- Razavi, M.; Jamilian, M.; Karamali, M.; Bahmani, F.; Aghadavod, E.; Asemi, Z. The effects of vitamin D-K-calcium co-supplementation on endocrine, inflammation, and oxidative stress biomarkers in vitamin D-deficient women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Horm. Metab. Res. 2016, 48, 446–451. [Google Scholar] [CrossRef]
- Özer, A.; Bakacak, M.; Kıran, H.; Ercan, Ö.; Köstü, B.; Kanat-Pektaş, M.; Kılınç, M.; Aslan, F. Increased oxidative stress is associated with insulin resistance and infertility in polycystic ovary syndrome. Ginekol. Pol. 2016, 87, 733–738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Afshar Ebrahimi, F.; Foroozanfard, F.; Aghadavod, E.; Bahmani, F.; Asemi, Z. The effects of magnesium and zinc co-supplementation on biomarkers of inflammation and oxidative stress, and gene expression related to inflammation in polycystic ovary syndrome: A randomized controlled clinical trial. Biol. Trace Elem. Res. 2018, 184, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Zadeh Modarres, S.; Amiri Siavashani, M.; Karimi, M.; Mafi, A.; Ostadmohammadi, V.; Asemi, Z. The Influences of chromium supplementation on glycemic control, markers of cardio-metabolic risk, and oxidative stress in infertile polycystic ovary syndrome women candidate for in vitro fertilization: A randomized, double-blind, placebo-controlled trial. Biol. Trace Elem. Res. 2018, 185, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Shokrpour, M.; Asemi, Z. The effects of magnesium and vitamin E co-supplementation on hormonal status and biomarkers of inflammation and oxidative stress in women with polycystic ovary syndrome. Biol. Trace Elem. Res. 2019, 191, 54–60. [Google Scholar] [CrossRef]
- Kanafchian, M.; Esmaeilzadeh, S.; Mahjoub, S.; Rahsepar, M.; Ghasemi, M. Status of serum copper, magnesium, and total antioxidant capacity in patients with polycystic ovary syndrome. Biol. Trace Elem. Res. 2020, 193, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Kirmizi, D.A.; Baser, E.; Turksoy, V.A.; Kara, M.; Yalvac, E.S.; Gocmen, A.Y. Are heavy metal exposure and trace element levels related to metabolic and endocrine problems in polycystic ovary syndrome? Biol. Trace Elem. Res. 2020, 198, 77–86. [Google Scholar] [CrossRef]
- Mousavi, R.; Alizadeh, M.; Asghari Jafarabadi, M.; Heidari, L.; Nikbakht, R.; Babaahmadi Rezaei, H.; Karandish, M. Effects of melatonin and/or magnesium supplementation on biomarkers of inflammation and oxidative stress in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Biol. Trace Elem. Res. 2022, 200, 1010–1019. [Google Scholar] [CrossRef]
- Abudawood, M.; Tabassum, H.; Alanazi, A.H.; Almusallam, F.; Aljaser, F.; Ali, M.N.; Alenzi, N.D.; Alanazi, S.T.; Alghamdi, M.A.; Altoum, G.H.; et al. Antioxidant status in relation to heavy metals induced oxidative stress in patients with polycystic ovarian syndrome (PCOS). Sci. Rep. 2021, 11, 22935. [Google Scholar] [CrossRef]
- Abudawood, M.; Alnuaim, L.; Tabassum, H.; Ghneim, H.K.; Alfhili, M.A.; Alanazi, S.T.; Alenzi, N.D.; Alsobaie, S. An insight into the impact of serum tellurium, thallium, osmium and antimony on the antioxidant/redox status of PCOS patients: A comprehensive study. Int. J. Mol. Sci. 2023, 24, 2596. [Google Scholar] [CrossRef]
- Pollack, A.Z.; Schisterman, E.F.; Goldman, L.R.; Mumford, S.L.; Albert, P.S.; Jones, R.L.; Wactawski-Wende, J. Cadmium, lead, and mercury in relation to reproductive hormones and anovulation in premenopausal women. Environ. Health Perspect. 2011, 119, 1156–1161. [Google Scholar] [CrossRef] [Green Version]
- Hilali, N.; Vural, M.; Camuzcuoglu, H.; Camuzcuoglu, A.; Aksoy, N. Increased prolidase activity and oxidative stress in PCOS. Clin. Endocrinol. 2013, 79, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Dinger, Y.; Akcay, T.; Erdem, T.; Ilker Saygili, E.; Gundogdu, S. DNA damage, DNA susceptibility to oxidation and glutathione level in women with polycystic ovary syndrome. Scand. J. Clin. Lab. Investig. 2005, 65, 721–728. [Google Scholar] [CrossRef]
- Zhang, D.; Luo, W.Y.; Liao, H.; Wang, C.F.; Sun, Y. The effects of oxidative stress to PCOS. Sichuan Da Xue Xue Bao Yi Xue Ban 2008, 39, 421–423. [Google Scholar]
- dos Santos, A.C.S.; Azevedo, G.D.; Lemos, T.M.A.M. The influence of oxidative stress in inflammatory process and insulin resistance in obese women with polycystic ovary syndrome. Transl. Biomed. 2016, 7, 4. [Google Scholar] [CrossRef]
- Kuşçu, N.K.; Var, A. Oxidative stress but not endothelial dysfunction exists in non-obese, young group of patients with polycystic ovary syndrome. Acta Obstet. Gynecol. Scand. 2009, 88, 612–617. [Google Scholar] [CrossRef]
- Talat, A.; Satyanarayana, P.; Anand, P. Association of superoxide dismutase level in women with polycystic ovary syndrome. J. Obstet. Gynaecol. India 2022, 72, 6–12. [Google Scholar] [CrossRef]
- Yilmaz, N.; Inal, H.A.; Gorkem, U.; Sargin Oruc, A.; Yilmaz, S.; Turkkani, A. Follicular fluid total antioxidant capacity levels in PCOS. J. Obstet. Gynaecol. 2016, 36, 654–657. [Google Scholar] [CrossRef] [PubMed]
- Menke, A.; Guallar, E.; Cowie, C.C. Metals in urine and diabetes in U.S. adults. Diabetes 2016, 65, 164–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.; Li, X.; Liu, X.; Dong, M.; Xiao, J.; Wang, J.; Zhou, M.; Wang, Y.; Ning, D.; Ma, W.; et al. Association between maternal antimony exposure and risk of gestational diabetes mellitus: A birth cohort study. Chemosphere 2020, 246, 125732. [Google Scholar] [CrossRef]
- Swaddiwudhipong, W.; Mahasakpan, P.; Limpatanachote, P.; Krintratun, S. Correlations of urinary cadmium with hypertension and diabetes in persons living in cadmium-contaminated villages in northwestern Thailand: A population study. Environ. Res. 2010, 110, 612–616. [Google Scholar] [CrossRef]
- Feng, W.; Cui, X.; Liu, B.; Liu, C.; Xiao, Y.; Lu, W.; Guo, H.; He, M.; Zhang, X.; Yuan, J.; et al. Association of urinary metal profiles with altered glucose levels and diabetes risk: A population-based study in China. PLoS ONE 2015, 10, e0123742. [Google Scholar] [CrossRef]
- Jiang, Q.; Zhang, F.; Han, L.; Zhu, B.; Liu, X. Serum copper level and polycystic ovarian syndrome: A meta-analysis. Gynecol. Obstet. Investig. 2021, 86, 239–246. [Google Scholar] [CrossRef]
- Yarali, H.; Yildirir, A.; Aybar, F.; Kabakçi, G.; Bükülmez, O.; Akgül, E.; Oto, A. Diastolic dysfunction and increased serum homocysteine concentrations may contribute to increased cardiovascular risk in patients with polycystic ovary syndrome. Fertil. Steril. 2001, 76, 511–516. [Google Scholar] [CrossRef]
- Roussel, A.M.; Kerkeni, A.; Zouari, N.; Mahjoub, S.; Matheau, J.M.; Anderson, R.A. Antioxidant effects of zinc supplementation in Tunisians with type 2 diabetes mellitus. J. Am. Coll. Nutr. 2003, 22, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Lux-Battistelli, C. Combination therapy with zinc gluconate and PUVA for alopecia areata totalis: An adjunctive but crucial role of zinc supplementation. Dermatol. Ther. 2015, 28, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Plonka, P.M.; Handjiski, B.; Popik, M.; Michalczyk, D.; Paus, R. Zinc as an ambivalent but potent modulator of murine hair growth in vivo- preliminary observations. Exp. Dermatol. 2005, 14, 844–853. [Google Scholar] [CrossRef]
- Jain, S.K.; Croad, J.L.; Velusamy, T.; Rains, J.L.; Bull, R. Chromium dinicocysteinate supplementation can lower blood glucose, CRP, MCP-1, ICAM-1, creatinine, apparently mediated by elevated blood vitamin C and adiponectin and inhibition of NFkappaB, Akt, and Glut-2 in livers of zucker diabetic fatty rats. Mol. Nutr. Food Res. 2010, 54, 1371–1380. [Google Scholar] [CrossRef] [Green Version]
- Sahin, N.; Akdemir, F.; Orhan, C.; Aslan, A.; Agca, C.A.; Gencoglu, H.; Ulas, M.; Tuzcu, M.; Viyaja, J.; Komorowskı, J.; et al. A novel nutritional supplement containing chromium picolinate, phosphatidylserine, docosahexaenoic acid, and boron activates the antioxidant pathway Nrf2/HO-1 and protects the brain against oxidative stress in high-fat-fed rats. Nutr. Neurosci. 2012, 15, 42–47. [Google Scholar] [CrossRef]
- Tian, Y.Y.; Zhang, L.Y.; Dong, B.; Cao, J.; Xue, J.X.; Gong, L.M. Effects of chromium methionine supplementation on growth performance, serum metabolites, endocrine parameters, antioxidant status, and immune traits in growing pigs. Biol. Trace Elem. Res. 2014, 162, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.K.; Kannan, K. Chromium chloride inhibits oxidative stress and TNF-alpha secretion caused by exposure to high glucose in cultured U937 monocytes. Biochem. Biophys. Res. Commun. 2001, 289, 687–691. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Asemi, Z. Chromium supplementation and the effects on metabolic status in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Ann. Nutr. Metab. 2015, 67, 42–48. [Google Scholar] [CrossRef]
- Chen, T.S.; Chen, Y.T.; Liu, C.H.; Sun, C.C.; Mao, F.C. Effect of chromium supplementation on element distribution in a mouse model of polycystic ovary syndrome. Biol. Trace Elem. Res. 2015, 168, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Chen, G.; Dong, Y.; Zhu, Y.; Chen, H. Chromium supplementation for adjuvant treatment of type 2 diabetes mellitus: Results from a pooled analysis. Mol. Nutr. Food Res. 2018, 62, 201700438. [Google Scholar] [CrossRef] [PubMed]
- Rabinovitz, H.; Friedensohn, A.; Leibovitz, A.; Gabay, G.; Rocas, C.; Habot, B. Effect of chromium supplementation on blood glucose and lipid levels in type 2 diabetes mellitus elderly patients. Int. J. Vitam. Nutr. Res. 2004, 74, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Wang, H.; Luo, G.; Niu, R.; Wang, J. Effect of dietary yeast chromium and L-carnitine on lipid metabolism of sheep. Biol. Trace Elem. Res. 2013, 155, 221–227. [Google Scholar] [CrossRef]
- Coskun, A.; Arikan, T.; Kilinc, M.; Arikan, D.C.; Ekerbiçer, H.Ç. Plasma selenium levels in Turkish women with polycystic ovary syndrome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 168, 183–186. [Google Scholar] [CrossRef]
- Mohammad Hosseinzadeh, F.; Hosseinzadeh-Attar, M.J.; Yekaninejad, M.S.; Rashidi, B. Effects of selenium supplementation on glucose homeostasis and free androgen index in women with polycystic ovary syndrome: A randomized, double blinded, placebo controlled clinical trial. J. Trace Elem. Med. Biol. 2016, 34, 56–61. [Google Scholar] [CrossRef]
- Muñoz, C.; Carson, A.F.; McCoy, M.A.; Dawson, L.E.; Irwin, D.; Gordon, A.W.; Kilpatrick, D.J. Effect of supplementation with barium selenate on the fertility, prolificacy and lambing performance of hill sheep. Vet. Rec. 2009, 164, 265–271. [Google Scholar] [CrossRef]
- Aréchiga, C.F.; Vázquez-Flores, S.; Ortíz, O.; Hernández-Cerón, J.; Porras, A.; McDowell, L.R.; Hansen, P.J. Effect of injection of beta-carotene or vitamin E and selenium on fertility of lactating dairy cows. Theriogenology 1998, 50, 65–76. [Google Scholar] [CrossRef]
- Özkaya, M.O.; Nazıroğlu, M.; Barak, C.; Berkkanoglu, M. Effects of multivitamin/mineral supplementation on trace element levels in serum and follicular fluid of women undergoing in vitro fertilization (IVF). Biol. Trace Elem. Res. 2011, 139, 1–9. [Google Scholar] [CrossRef]
- Pal, L.; Berry, A.; Coraluzzi, L.; Kustan, E.; Danton, C.; Shaw, J.; Taylor, H. Therapeutic implications of vitamin D and calcium in overweight women with polycystic ovary syndrome. Gynecol. Endocrinol. 2012, 28, 965–968. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Firouzabadi, R.D.; Aflatoonian, A.; Modarresi, S.; Sekhavat, L.; Mohammad Taheri, S. Therapeutic effects of calcium & vitamin D supplementation in women with PCOS. Complement. Ther. Clin. Pract. 2012, 18, 85–88. [Google Scholar] [CrossRef]
- Asemi, Z.; Karamali, M.; Esmaillzadeh, A. Effects of calcium-vitamin D co-supplementation on glycaemic control, inflammation and oxidative stress in gestational diabetes: A randomised placebo-controlled trial. Diabetologia 2014, 57, 1798–1806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simental-Mendia, L.E.; Sahebkar, A.; Rodriguez-Moran, M.; Zambrano-Galvan, G.; Guerrero-Romero, F. Effect of magnesium supplementation on plasma C-reactive protein concentrations: A systematic review and meta-analysis of randomized controlled trials. Curr. Pharm. Des. 2017, 23, 4678–4686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roman, A.; Desai, N.; Rochelson, B.; Gupta, M.; Solanki, M.; Xue, X.; Chatterjee, P.K.; Metz, C.N. Maternal magnesium supplementation reduces intrauterine growth restriction and suppresses inflammation in a rat model. Am. J. Obstet. Gynecol. 2013, 208, 383.e1. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L.J.; Galioto, A.; Ferlisi, A.; Cani, C.; Malfa, L.; Pineo, A.; Busardo’, A.; Paolisso, G. Role of magnesium in insulin action, diabetes and cardio-metabolic syndrome X. Mol. Asp. Med. 2003, 24, 39–52. [Google Scholar] [CrossRef]
- Sharifi, F.; Mazloomi, S.; Hajihosseini, R.; Mazloomzadeh, S. Serum magnesium concentrations in polycystic ovary syndrome and its association with insulin resistance. Gynecol. Endocrinol. 2012, 28, 7–11. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]


| Study, Year, (Country) | Study Design | Participants (No. of Women) | Sample Type | Exposure | Main Conclusions |
|---|---|---|---|---|---|
| Köse et al. (2014), Turkey [55] | Case–control study | 20: 10 with PCOS (mean age: 24.0 ± 5.5), 10 controls (mean age: 27.8 ± 6.9) | Peripheral whole blood sample | Se |
|
| Guler et al. (2014), Turkey [56] | Prospective study | 86: 53 with PCOS (mean age: 25.4 ± 6.7), 33 controls (mean age: 28 ± 5.9) | Overnight fasting venous blood sample | Zn |
|
| Jamilian et al. (2015), Iran [57] | Randomized, double-blind, placebo-controlled study | 48 with PCOS aged 18–40 | Fasting blood sample | Zn |
|
| Jamilian et al. (2015), Iran [58] | Randomized, double-blind, placebo-controlled study | 60 with PCOS aged 18–40 | Fasting blood sample | Cr |
|
| Razavi et al. (2016), Iran [59] | Randomized, double-blind, placebo-controlled study | 64 with PCOS aged 18–40 | Fasting blood sample | Se |
|
| Razavi et al. (2016), Iran [60] | Randomized, double-blind, placebo-controlled study | 60 vitamin D deficient with PCOS aged 18–40 | Fasting blood sample | Ca |
|
| Özer et al. (2016), Turkey [61] | Descriptive study | 124 aged 20–30: 71 with PCOS, 53 controls | Venous blood sample | Zn, Cu |
|
| Ebrahimi et al. (2017), Iran [62] | Randomized double-blind, placebo-controlled tri-al | 60 with PCOS aged 18–40 | Fasting blood sample | Mg, Zn |
|
| Jamilian et al. (2018), Iran [63] | Randomized, double-blind, placebo-controlled study | 40 infertile with PCOS, candidate for IVF, aged 18–40 | Fasting blood sample | Cr |
|
| Shokrpour et al. (2019), Iran [64] | Randomized, double-blind, placebo-controlled study | 60 with PCOS aged 18–40 | Fasting blood sample | Mg |
|
| Kanafchian et al. (2019), Iran [65] | Case–control study | 150 aged 20–40: 60 with PCOS, 90 controls | Fasting venous blood | Cu, Mg, Ca |
|
| Kirmizi et al. (2020), Turkey [66] | Case–control study | 154: 84 with PCOS (aged 22–36), 70 controls (aged 21–39) | Blood sample | As, Cr, Cd, Sb, Hg, Pb, Cu, Zn |
|
| Mousavi et al. (2021), Iran [67] | Randomized, double-blind, placebo-controlled study | 84 with PCOS aged 18–40 | Blood sample | Mg |
|
| Abudawood (2021), Saudi Arabia [68] | Prospective study | 106 aged 19–35: 56 with PCOS, 50 controls | Blood serum | As, Cd, Pb, Hg |
|
| Abudawood (2023), Saudi Arabia [69] | Case–control study | 106: 50 with PCOS (mean age: 30.41 ± 6.8), 56 controls (mean age: 29.16 ± 6.2) | Blood serum | Te, Tl, Sb, Os |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Srnovršnik, T.; Virant-Klun, I.; Pinter, B. Heavy Metals and Essential Elements in Association with Oxidative Stress in Women with Polycystic Ovary Syndrome—A Systematic Review. Antioxidants 2023, 12, 1398. https://doi.org/10.3390/antiox12071398
Srnovršnik T, Virant-Klun I, Pinter B. Heavy Metals and Essential Elements in Association with Oxidative Stress in Women with Polycystic Ovary Syndrome—A Systematic Review. Antioxidants. 2023; 12(7):1398. https://doi.org/10.3390/antiox12071398
Chicago/Turabian StyleSrnovršnik, Tinkara, Irma Virant-Klun, and Bojana Pinter. 2023. "Heavy Metals and Essential Elements in Association with Oxidative Stress in Women with Polycystic Ovary Syndrome—A Systematic Review" Antioxidants 12, no. 7: 1398. https://doi.org/10.3390/antiox12071398





