Implications of Exposure to Air Pollution on Male Reproduction: The Role of Oxidative Stress
Abstract
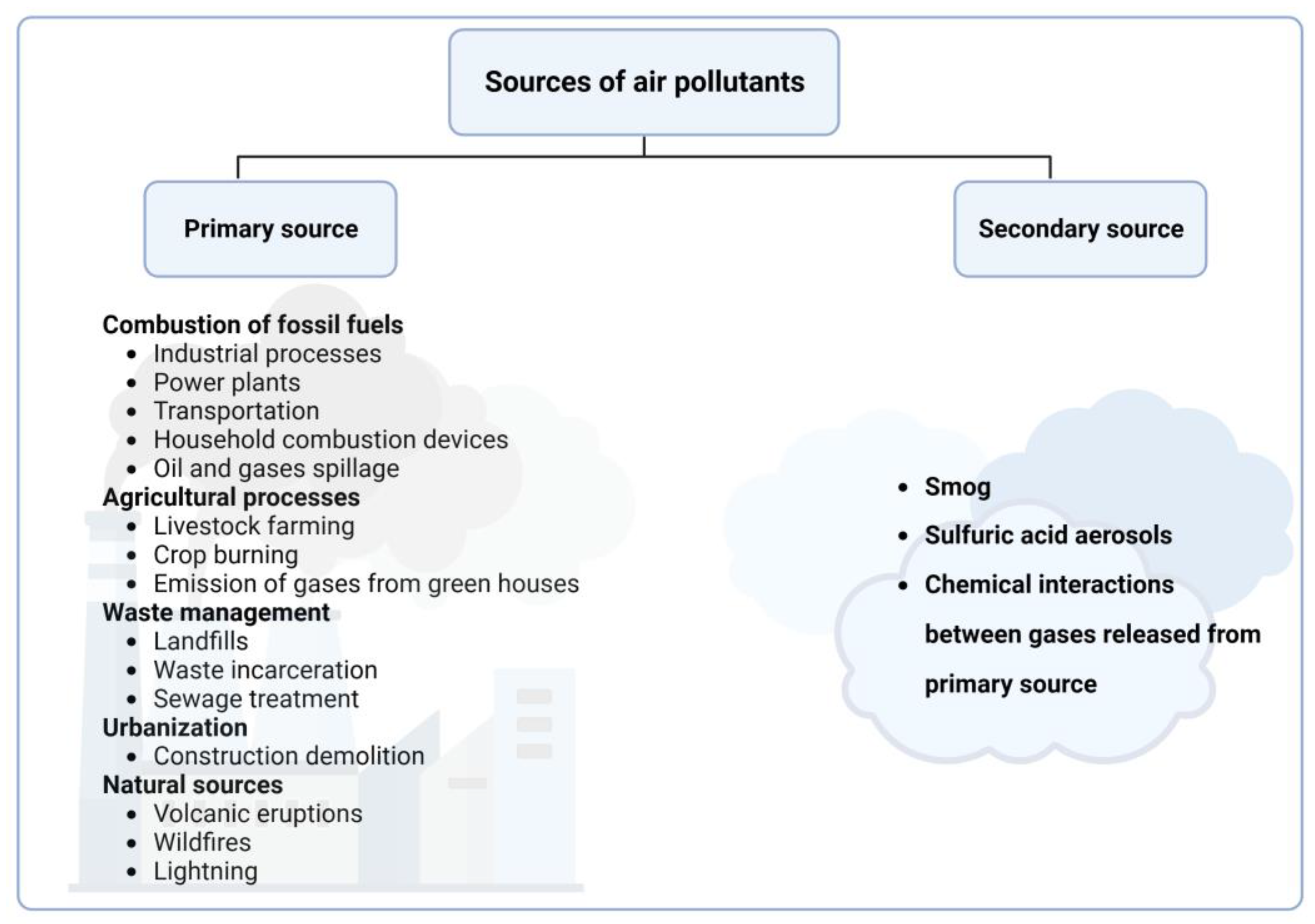
:1. Introduction
2. Search Methods
3. Implications of Exposure to Air Pollution on Male Reproductive Parameters
3.1. Evidence of the Effects of Air Pollution on Male Reproductive Parameters: Animal Studies
Basic and Advanced Parameters
3.2. Evidence of the Effects of Air Pollution on Male Reproductive Parameters: Human Studies
3.2.1. Basic Parameters
| Reference | Type of Study Design | Country | Sample Size | Pollutants | Study Outcome |
|---|---|---|---|---|---|
| [46] | Cohort Study/Cross-sectional study | Czech Republic | 54 | PM1O, SO2, NO2, CO, O3, Benzene, Benzo[a]pyrene | ○ No significant association between air pollutants and sperm parameters was observed during the winter and summer months ○ Sperm kinetic parameters such as STR, VAP, VSL and LIN, and DSL were significantly reduced during the spring and autumn months |
| [68] | Prospective cohort study | China | 15,112 | PM2.5, PM1O | ○ Exposure to PM2.5 and PM1O significantly decreased sperm concentration, total sperm count, total motility, progressive motility, total motile sperm count, and progressively motile sperm count, during the entire spermatogenesis period |
| [69] | Longitudinal study | China | 15,112 | PM2.5, CO, SO2, NO2, O3 | ○ Exposure to ambient SO2 was negatively associated with all semen quality parameters except for the progressive motility ○ There was also a linear and non-linear dose–response association between SO2 and sperm motility |
| [70] | Retrospective cohort study | China | 1168 | PM2.5, PM1O, CO, SO2, NO2, O3 | ○ PM2.5 and PM1O were shown to significantly decrease sperm count ○ A negative association between all air pollutants and sperm parameters was observed ○ O3 significantly reduced motility in the late stage of sperm development |
| [71] | Cross-sectional study/Comparative study | China | 1346 | PM1O, SO2, NO2 | ○ Exposure to these pollutants adversely affected sperm morphology sperm motility and sperm kinematics (VCL and VSL) |
| [72] | Retrospective cohort study | United States of America | 1699 | PM2.5 | ○ Negative correlation was observed between PM2.5 and motility after 2 and 3 months of exposure to pollutants |
| [76] | Retrospective study and longitudinal study | China | 686 | PM2.5, PM1O, CO, SO2, NO2, O3 | ○ Exposure to PM2.5, PM1O, and CO negatively affected sperm concentration and the concentration of progressively motile spermatozoa |
| [77] | Prospective cohort study | China | 3940 | PM2.5, PM1O, CO, SO2, NO2 | ○ There was a decrease in total motility, progressive motility, and sperm morphology following exposures to all pollutants tested ○ The SO2-induced effects were mostly on sperm morphology |
| [78] | Retrospective cohort study/Cross-sectional study | Poland | 327 | PM2.5, PM1O, CO, SO2, NOx | ○ Exposure to pollutants significantly altered sperm morphology |
| [79] | Retrospective cohort study | Italy | 406 | PM2.5, PM1O | ○ PM2.5 was positively associated with total sperm count ○ PM10 was positively associated with both semen volume and percentage of normal sperm morphology |
| [80] | Prospective | China | 1759 | SO2, NO2, CO, O3 | ○ After 90 days of exposure to the pollutants, reported observations included the following: ○ Decreased sperm concentration ○ Reduced sperm count ○ Reduced total motile sperm count ○ Reduce total and progressive motility ○ SO2 had the most adverse effect on semen quality |
| [81] | Prospective | China | 72,917 | PM2.5, PM1O, CO, SO2, NO2, O3 | ○ Following exposure to the pollutants for 30 days, there was as significant decrease in serum sex hormone levels (follicle-stimulating hormone, luteinizing hormone, estradiol, prolactin, especially testosterone) |
| [82] | Observational | Czech Republic | 2585 parental pairs | SO2 | ○ Exposure to SO2 for 4 months before conception until 2 years after delivery led to the following: ○ Decreased fecundity ○ Increased sperm abnormalities |
| [75] | Population-based case–control study | 4371 male infants | Maternal exposure to SO2, PM10, NO2 | ○ Maternal exposure to SO2 during the 3 months before and the first and second months after conception increased the risk of hypospadias in male offspring | |
| [83] | Observational | Taiwan | 282 male patients with primary infertility | SO2, NOx, O3 | ○ Exposure to NO2 and SO2 was negatively associated with the seminal parameters (sperm count and concentration) and decreased testicular volume |
| [84] | Prospective | Human Sperm Bank | 1515 | PM2.5, PM1O, CO, SO2, NO2, O3 | ○ Exposure to the different pollutants over 90 days resulted in decreased progressive and total motility ○ Adversely affected sperm concentration and total sperm number |
| [85] | Prospective | China | 1069 | PM10, NO2, SO2, O3 | ○ Exposure to these air pollutants at varying spermatogenesis stages adversely affected spermatogenesis ○ PM10 was associated with declined sperm concentration, reduced sperm count, reduced total and progressive motility, and reduced sperm concentration ○ SO2 induced a decrease in progressive and total motility ○ NO2 and O3 were not associated with the sperm quality parameters measured |
| [86] | Prospective | USA | 5134 | PM10, NO2, SO2, O3 | ○ Exposure to the different air pollutants resulted in a significant negative correlation between O3 levels (at 0–9, 10–14, and 70–90 days before donation) and sperm concentration, which was maintained after correction for the donor’s birth date, age at donation, temperature, and seasonality ○ Exposure to ambient O3 levels adversely affected semen quality, while no other pollutant was significantly associated with sperm quality outcomes |
| [87] | Cross-observational | China | 1852 | SO2 | ○ Exposure to SO2 and NO2 for 90 days significantly decreased sperm concentration, sperm count, and progressive motility ○ There was no association between exposure to SO2 and NO2 and semen volume |
3.2.2. Advanced Parameters
4. Implications of Air Pollution on Male Sexual Health
5. Effects of Air Pollution on Reproductive Outcomes
6. Mechanisms through Which Air Pollutants Affect Sperm Parameters
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carlsen, E.; Giwercman, A.; Keiding, N.; Skakkebaek, N.E. Evidence for decreasing quality of semen during past 50 years. Br. Med. J. 1992, 305, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Swan, S.H.; Elkin, E.P.; Fenster, L. The question of declining sperm density revisited: An analysis of 101 studies published 1934–1996. Environ. Health Perspect. 2000, 108, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Levine, H.; Jørgensen, N.; Martino-Andrade, A.; Mendiola, J.; Weksler-Derri, D.; Mindlis, I.; Pinotti, R.; Swan, S.H. Temporal trends in sperm count: A systematic review and meta-regression analysis. Hum. Reprod. Update 2017, 23, 646–659. [Google Scholar] [CrossRef] [PubMed]
- Hunt, P.A.; Sathyanarayana, S.; Fowler, P.A.; Trasande, L. Female reproductive disorders, diseases, and costs of exposure to endocrine disrupting chemicals in the European Union. J. Clin. Endocrinol. Metab. 2016, 101, 1562–1570. [Google Scholar] [CrossRef] [PubMed]
- Skakkebaek, N.E.; Rajpert-De Meyts, E.; Buck Louis, G.M.; Toppari, J.; Andersson, A.-M.; Eisenberg, M.L.; Jensen, T.K.; Jørgensen, N.; Swan, S.H.; Sapra, K.J.; et al. Male Reproductive Disorders and Fertility Trends: Influences of Environment and Genetic Susceptibility. Physiol. Rev. 2016, 96, 55–97. [Google Scholar] [CrossRef]
- Jensen, T.K.; Jacobsen, R.; Christensen, K.; Nielsen, N.C.; Bostofte, E. Good semen quality and life expectancy: A cohort study of 43,277 men. Am. J. Epidemiol. 2009, 170, 559–565. [Google Scholar] [CrossRef]
- Gollenberg, A.L.; Liu, F.; Brazil, C.; Drobnis, E.Z.; Guzick, D.; Overstreet, J.W.; Redmon, J.B.; Sparks, A.; Wang, C.; Swan, S.H. Semen quality in fertile men in relation to psychosocial stress. Fertil. Steril. 2010, 93, 1104–1111. [Google Scholar] [CrossRef]
- Sharma, R.; Harlev, A.; Agarwal, A.; Esteves, S.C. Cigarette Smoking and Semen Quality: A New Meta-analysis Examining the Effect of the 2010 World Health Organization Laboratory Methods for the Examination of Human Semen. Eur. Urol. 2016, 70, 635–645. [Google Scholar] [CrossRef]
- Sermondade, N.; Faure, C.; Fezeu, L.; Shayeb, A.G.; Bonde, J.P.; Jensen, T.K.; Van Wely, M.; Cao, J.; Martini, A.C.; Eskandar, M.; et al. BMI in relation to sperm count: An updated systematic review and collaborative meta-analysis. Hum. Reprod. Update 2013, 19, 221–231. [Google Scholar] [CrossRef]
- Durairajanayagam, D. Lifestyle causes of male infertility. Arab. J. Urol. 2018, 16, 10–20. [Google Scholar] [CrossRef]
- Bloom, M.S.; Whitcomb, B.W.; Chen, Z.; Ye, A.; Kannan, K.; Buck Louis, G.M. Associations between urinary phthalate concentrations and semen quality parameters in a general population. Hum. Reprod. 2015, 30, 2645–2657. [Google Scholar] [CrossRef] [PubMed]
- Gore, A.C.; Chappell, V.A.; Fenton, S.E.; Flaws, J.A.; Nadal, A.; Prins, G.S.; Toppari, J.; Zoeller, R.T. EDC-2: The Endocrine Society’s Second Scientific Statement on Endocrine-Disrupting Chemicals. Endocr. Rev. 2015, 36, 1–150. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.-H.; Gaskins, A.J.; Williams, P.L.; Mendiola, J.; Jørgensen, N.; Levine, H.; Hauser, R.; Swan, S.H.; Chavarro, J.E. Intake of Fruits and Vegetables with Low-to-Moderate Pesticide Residues Is Positively Associated with Semen-Quality Parameters among Young Healthy Men. J. Nutr. 2016, 146, 1084–1092. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.H.; Zhang, A.D.; Shi, Z.D.; Wang, L.G.; Qiu, Y. Changes in levels of seminal nitric oxide synthase, macrophage migration inhibitory factor, sperm DNA integrity and caspase-3 in fertile men after scrotal heat stress. PLoS ONE 2015, 10, e0141320. [Google Scholar] [CrossRef] [PubMed]
- Najafi, T.F.; Roudsari, R.L.; Namvar, F.; Ghanbarabadi, V.G.; Talasaz, Z.H.; Esmaeli, M. Air Pollution and Quality of Sperm: A Meta-Analysis. Iran. Red. Crescent Med. J. 2015, 17, 26930. [Google Scholar] [CrossRef]
- World Health Organization Air Pollution. Available online: https://www.who.int/health-topics/air-pollution#tab=tab_1 (accessed on 11 July 2023).
- Soppelsa, M.E.; Lozano-Gracia, N.; Xu, L.C. The Effects of Pollution and Business Environment on Firm Productivity in Africa; World Bank: Washington, DC, USA, 2019. [Google Scholar] [CrossRef]
- World Bank Group, T. The Global Health Cost of PM2.5 Air Pollution: A Case for Action Beyond 2021; World Bank: Washington, DC, USA, 2022. [Google Scholar] [CrossRef]
- WHO. Human Health Effects of Polycyclic Aromatic Hydrocarbons as Ambient Air Pollutants; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Phillips, K.P.; Tanphaichitr, N. Human exposure to endocrine disrupters and semen quality. J. Toxicol. Environ. Heal. Part. B Crit. Rev. 2008, 11, 188–220. [Google Scholar] [CrossRef]
- Jbaily, A.; Zhou, X.; Liu, J.; Lee, T.-H.; Kamareddine, L.; Verguet, S.; Dominici, F. Air pollution exposure disparities across US population and income groups. Nature 2022, 601, 228–233. [Google Scholar] [CrossRef]
- WHO. WHO Guidelines for Indoor Air Quality: Selected Pollutants; Chapter 5. Nitrogen Dioxide; WHO: Geneva, Switzerland, 2010; pp. 201–248. [Google Scholar]
- Pérez Velasco, R.; Jarosi, D. Update of the WHO global air quality guidelines: Systematic reviews-An introduction. Environ. Int. 2022, 170, 160–4120. [Google Scholar] [CrossRef]
- Zheng, X.-Y.; Orellano, P.; Lin, H.-L.; Jiang, M.; Guan, W.-J. Short-term exposure to ozone, nitrogen dioxide, and sulphur dioxide and emergency department visits and hospital admissions due to asthma: A systematic review and meta-analysis. Environ. Int. 2021, 150, 106435. [Google Scholar] [CrossRef]
- Orellano, P.; Reynoso, J.; Quaranta, N.; Bardach, A.; Ciapponi, A. Short-term exposure to particulate matter (PM 10 and PM 2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: Systematic review and meta-analysis. Environ. Int. 2020, 142, 105876. [Google Scholar] [CrossRef]
- Huangfu, P.; Atkinson, R. Long-term exposure to NO2 and O3 and all-cause and respiratory mortality: A systematic review and meta-analysis. Environ. Int. 2020, 144, 105998. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.K.; Spath, N.; Miller, M.R.; Mills, N.L.; Shah, A.S.V. Short-term exposure to carbon monoxide and myocardial infarction: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105901. [Google Scholar] [CrossRef] [PubMed]
- Orellano, P.; Reynoso, J.; Quaranta, N. NC-ND license Short-term exposure to sulphur dioxide (SO2) and all-cause and respiratory mortality: A systematic review and meta-analysis. Environ. Int. 2021, 150, 106434. [Google Scholar] [CrossRef] [PubMed]
- Pénard-Morand, C.; Annesi-Maesano, I. Air Pollution: From sources of emissions to health effects. Breathe 2004, 1, 109–119. [Google Scholar] [CrossRef]
- IARC. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Outdoor Air Pollution; IARC: Lyopn, France, 2015; Volume 109, ISBN 9789283201755. [Google Scholar]
- Sierra-Vargas, M.P.; Teran, L.M. Air pollution: Impact and prevention. Respirology 2012, 17, 1031–1038. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef]
- Pryor, J.T.; Cowley, L.O.; Simonds, S.E. The Physiological Effects of Air Pollution: Particulate Matter, Physiology and Disease. Front. Public Health 2022, 10, 882569. [Google Scholar] [CrossRef]
- Chen, T.M.; Gokhale, J.; Shofer, S.; Kuschner, W.G. Outdoor air pollution: Nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am. J. Med. Sci. 2007, 333, 249–256. [Google Scholar] [CrossRef]
- Wang, J.; Li, J.; Ye, J.; Zhao, J.; Wu, Y.; Hu, J.; Liu, D.; Nie, D.; Shen, F.; Huang, X.; et al. Fast sulfate formation from oxidation of SO2 by NO2 and HONO observed in Beijing haze. Nat. Commun. 2020, 11, 1–7. [Google Scholar] [CrossRef]
- Thompson, J.E. Airborne Particulate Matter: Human Exposure and Health Effects. J. Occup. Environ. Med. 2018, 60, 392–423. [Google Scholar] [CrossRef]
- WHO. WHO Laboratory Manual for the Examination and Processing of Human Semen, 6th ed.; WHO: Geneva, Switzerland, 2021; Volume V. [Google Scholar]
- Radwan, M.; Dziewirska, E.; Radwan, P.; Jakubowski, L.; Hanke, W.; Jurewicz, J. Air Pollution and Human Sperm Sex Ratio. Am. J. Mens. Health 2018, 12, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Bergamo, P.; Volpe, M.G.; Lorenzetti, S.; Mantovani, A.; Notari, T.; Cocca, E.; Cerullo, S.; Di Stasio, M.; Cerino, P.; Montano, L. Human semen as an early, sensitive biomarker of highly polluted living environment in healthy men: A pilot biomonitoring study on trace elements in blood and semen and their relationship with sperm quality and RedOx status. Reprod. Toxicol. 2016, 66, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chang, H.C.; Liao, C.H.; Chiang, B.J.; Chang, Y.K. The impact of the fine ambient particle on infertile male’s sperm quality. Urol. Sci. 2019, 30, 177. [Google Scholar] [CrossRef]
- Hansen, C.; Luben, T.J.; Sacks, J.D.; Olshan, A.; Jeffay, S.; Strader, L.; Perreault, S.D. The effect of ambient air pollution on sperm quality. Environ. Health Perspect. 2010, 118, 203–209. [Google Scholar] [CrossRef]
- Pizzol, D.; Foresta, C.; Garolla, A.; Demurtas, J.; Trott, M.; Bertoldo, A.; Smith, L. Pollutants and sperm quality: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. 2021, 28, 4095–4103. [Google Scholar] [CrossRef]
- Zhang, Y.; Wei, J.; Liu, C.; Cao, W.; Zhang, Z.; Li, Y.; Zeng, Q.; Sun, S. Association between ambient PM1 and semen quality: A cross-sectional study of 27,854 men in China. Environ. Int. 2023, 175, 107919. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Singh, A.K. Impact of environmental factors on human semen quality and male fertility: A narrative review. Environ. Sci. Eur. 2022, 34, 1–13. [Google Scholar] [CrossRef]
- Jurewicz, J.; Dziewirska, E.; Radwan, M.; Hanke, W. Air pollution from natural and anthropic sources and male fertility. Reprod. Biol. Endocrinol. 2018, 16, 109. [Google Scholar] [CrossRef]
- Rubes, J.; Sipek, J.; Kopecka, V.; Musilova, P.; Vozdova, M. Semen quality and sperm DNA integrity in city policemen exposed to polluted air in an urban industrial agglomeration. Int. J. Hyg. Environ. Health 2021, 237, 113835. [Google Scholar] [CrossRef] [PubMed]
- Rubes, J.; Selevan, S.G.; Evenson, D.P.; Zudova, D.; Vozdova, M.; Zudova, Z.; Robbins, W.A.; Perreault, S.D. Episodic air pollution is associated with increased DNA fragmentation in human sperm without other changes in semen quality. Hum. Reprod. 2005, 20, 2776–2783. [Google Scholar] [CrossRef]
- Vecoli, C.; Montano, L.; Borghini, A.; Notari, T.; Guglielmino, A.; Mercuri, A.; Turchi, S.; Andreassi, M.G. Effects of highly polluted environment on sperm telomere length: A pilot study. Int. J. Mol. Sci. 2017, 18, 1703. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Zhang, B.; Liu, B.; Wu, M.; Zhang, L.; Wang, L.; Xu, S.; Cao, Z.; Wang, Y. Effects of maternal exposure to ambient air pollution on newborn telomere length. Environ. Int. 2019, 128, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Šabović, I.; Cosci, I.; De Toni, L.; Ferramosca, A.; Stornaiuolo, M.; Di Nisio, A.; Dall’Acqua, S.; Garolla, A.; Foresta, C. Perfluoro-octanoic acid impairs sperm motility through the alteration of plasma membrane. J. Endocrinol. Invest. 2020, 43, 641–652. [Google Scholar] [CrossRef] [PubMed]
- Sipinen, V.; Laubenthal, J.; Baumgartner, A.; Cemeli, E.; Linschooten, J.O.; Godschalk, R.W.L.; Van Schooten, F.J.; Anderson, D.; Brunborg, G. In vitro evaluation of baseline and induced DNA damage in human sperm exposed to benzo[a]pyrene or its metabolite benzo[a]pyrene-7,8-diol-9,10-epoxide, using the comet assay. Mutagenesis 2010, 25, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Ning Cao, X.; Ju Shen, L.; De Wu, S.; Yan, C.; Zhou, Y.; Xiong, G.; Cai Wang, Y.; Liu, Y.; Liu, B.; Liang Tang, X.; et al. Urban fine particulate matter exposure causes male reproductive injury through destroying blood-testis barrier (BTB) integrity. Toxicol. Lett. 2017, 266, 1–12. [Google Scholar] [CrossRef]
- Qiu, L.; Chen, M.; Wang, X.; Qin, X.; Chen, S.; Qian, Y.; Liu, Z.; Cao, Q.; Ying, Z. Exposure to Concentrated Ambient PM2.5 Compromises Spermatogenesis in a Mouse Model: Role of Suppression of Hypothalamus-Pituitary-Gonads Axis. Toxicol. Sci. 2018, 162, 318–326. [Google Scholar] [CrossRef]
- Cao, X.N.; Yan, C.; Liu, D.Y.; Peng, J.P.; Chen, J.J.; Zhou, Y.; Long, C.L.; He, D.W.; Lin, T.; Shen, L.J.; et al. Fine particulate matter leads to reproductive impairment in male rats by overexpressing phosphatidylinositol 3-kinase (PI3K)/protein kinase B (Akt) signaling pathway. Toxicol. Lett. 2015, 237, 181–190. [Google Scholar] [CrossRef]
- Liu, J.; Ren, L.; Wei, J.; Zhang, J.; Zhu, Y.; Li, X.; Jing, L.; Duan, J.; Zhou, X.; Sun, Z. Fine particle matter disrupts the blood–testis barrier by activating TGF-β3/p38 MAPK pathway and decreasing testosterone secretion in rat. Environ. Toxicol. 2018, 33, 711–719. [Google Scholar] [CrossRef]
- Yang, W.; Xu, Y.; Pan, H.; Tian, F.; Wang, Y.; Xia, M.; Hu, J.; Yang, M.; Tao, S.; Sun, S.; et al. Chronic exposure to diesel exhaust particulate matter impairs meiotic progression during spermatogenesis in a mouse model. Ecotoxicol. Environ. Saf. 2020, 202, 110881. [Google Scholar] [CrossRef]
- Zhou, L.; Su, X.; Li, B.; Chu, C.; Sun, H.; Zhang, N.; Han, B.; Li, C.; Zou, B.; Niu, Y.; et al. PM2.5 exposure impairs sperm quality through testicular damage dependent on NALP3 inflammasome and miR-183/96/182 cluster targeting FOXO1 in mouse. Ecotoxicol. Environ. Saf. 2019, 169, 551–563. [Google Scholar] [CrossRef]
- Wei, Y.; Cao, X.N.; Tang, X.L.; Shen, L.J.; Lin, T.; He, D.W.; Wu, S.D.; Wei, G.H. Urban fine particulate matter (PM2.5) exposure destroys blood–testis barrier (BTB) integrity through excessive ROS-mediated autophagy. Toxicol. Mech. Methods 2017, 28, 302–319. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zheng, F.; Liang, C.; Zhu, Y.; Shi, Y.; Han, Y.; Wang, J. Sulfur dioxide inhalation lowers sperm quality and alters testicular histology via increasing expression of CREM and ACT proteins in rat testes. Environ. Toxicol. Pharmacol. 2016, 47, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, N.; Oonuki, Y. Inhalation of diesel engine exhaust affects spermatogenesis in growing male rats. Environ. Health Perspect. 1999, 107, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Ding, S.; Nie, H.; Shi, Y.; Lai, W.; Liu, X.; Li, K.; Tian, L.; Xi, Z.; Lin, B. PM2.5 exposure at different concentrations and modes induces reproductive toxicity in male rats mediated by oxidative and endoplasmic reticulum stress. Ecotoxicol. Environ. Saf. 2022, 244, 114042. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Jin, X.; Su, R.; Li, Z. The reproductive toxicology of male SD rats after PM2.5 exposure mediated by the stimulation of endoplasmic reticulum stress. Chemosphere 2017, 189, 547–555. [Google Scholar] [CrossRef]
- Meng, Z.; Bai, W. Oxidation damage of sulfur dioxide on testicles of mice. Environ. Res. 2004, 96, 298–304. [Google Scholar] [CrossRef]
- Li, X.; Yi, H.; Wang, H. Sulphur dioxide and arsenic affect male reproduction via interfering with spermatogenesis in mice. Ecotoxicol. Environ. Saf. 2018, 165, 164–173. [Google Scholar] [CrossRef]
- Zhang, J.; Li, Z.; Qie, M.; Zheng, R.; Shetty, J.; Wang, J. Sodium fluoride and sulfur dioxide affected male reproduction by disturbing blood-testis barrier in mice. Food Chem. Toxicol. 2016, 94, 103–111. [Google Scholar] [CrossRef]
- Fiore, M.; Petruzzi, S.; Dell’omo, G.; Alleva, E. Prenatal sulfur dioxide exposure induces changes in the behavior of adult male mice during agonistic encounters. Neurotoxicol. Teratol. 1998, 20, 543–548. [Google Scholar] [CrossRef]
- Liu, J.; Huang, J.; Gao, L.; Sang, Y.; Li, X.; Zhou, G.; Cao, L.; Lu, H.; Zhou, X.; Ren, L. Maternal exposure to PM2.5 disrupting offspring spermatogenesis through induced sertoli cells apoptosis via inhibin B hypermethylation in mice. Ecotoxicol. Environ. Saf. 2022, 241, 113760. [Google Scholar] [CrossRef]
- Ma, Y.; Zhang, J.; Cai, G.; Xia, Q.; Xu, S.; Hu, C.; Cao, Y.; Pan, F. Inverse association between ambient particulate matter and semen quality in Central China: Evidence from a prospective cohort study of 15,112 participants. Sci. Total Environ. 2022, 833, 155252. [Google Scholar] [CrossRef]
- Ma, Y.; Peng, X.; Pan, Z.; Hu, C.; Xia, Q.; Cai, G.; Cao, Y.; Pan, F. Linear and non-linear relationships between sulfur dioxide and semen quality: A longitudinal study in Anhui, China. Environ. Res. 2023, 216, 114731. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Zhang, Q.; Wu, H.; Wang, Q.; Chen, Y.; Guo, P.; Zhao, Q. Sperm quality and ambient air pollution exposure: A retrospective, cohort study in a Southern province of China. Environ. Res. 2020, 188, 109756. [Google Scholar] [CrossRef]
- Zhou, N.; Cui, Z.; Yang, S.; Han, X.; Chen, G.; Zhou, Z.; Zhai, C.; Ma, M.; Li, L.; Cai, M.; et al. Air pollution and decreased semen quality: A comparative study of Chongqing urban and rural areas. Environ. Pollut. 2014, 187, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Hammoud, A.; Carrell, D.T.; Gibson, M.; Sanderson, M.; Parker-Jones, K.; Peterson, C.M. Decreased sperm motility is associated with air pollution in Salt Lake City. Fertil. Steril. 2010, 93, 1875–1879. [Google Scholar] [CrossRef] [PubMed]
- Seli, D.A.; Taylor, H.S. The impact of air pollution and endocrine disruptors on reproduction and assisted reproduction. Curr. Opin. Obstet. Gynecol. 2023, 35, 210–215. [Google Scholar] [CrossRef]
- Kumar, S.; Sharma, A.; Thaker, R. Air pollutants and impairments of male reproductive health-an overview. Rev. Environ. Health 2021, 36, 565–575. [Google Scholar] [CrossRef]
- Zhang, S.; Yue, D.M.; Zhang, J.Y.; Huang, Y.H.; Li, J.; Liu, S.; Chen, Y.L.; Li, L.L.; Jiang, C.Z.; Chen, Z.J.; et al. Maternal exposure to sulfur dioxide before and after conception and the risk of hypospadias in offspring. Ann. N. Y. Acad. Sci. 2021, 1502, 99–109. [Google Scholar] [CrossRef]
- Qiu, Y.; Yang, T.; Seyler, B.C.; Wang, X.; Wang, Y.; Jiang, M.; Liu, B.; Li, F. Ambient air pollution and male fecundity: A retrospective analysis of longitudinal data from a Chinese human sperm bank (2013–2018). Environ. Res. 2020, 186, 109528. [Google Scholar] [CrossRef]
- Guo, Y.; Chen, Q.; Zhan, Y.; Zhou, W.; Zhang, H.; Zhou, N.; Yang, H.; Chen, Y.; Wang, Y.; Sun, L.; et al. Semen damage contributed over 50% to air-pollutant-induced infertility: A prospective cohort study of 3940 men in China. Sci. Total Environ. 2023, 885, 163532. [Google Scholar] [CrossRef]
- Radwan, M.; Jurewicz, J.; Polańska, K.; Sobala, W.; Radwan, P.; Bochenek, M.; Hanke, W. Exposure to ambient air pollution-does it affect semen quality and the level of reproductive hormones? Ann. Hum. Biol. 2015, 43, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Santi, D.; Vezzani, S.; Granata, A.R.M.; Roli, L.; Santis, M.C.D.; Ongaro, C.; Donati, F.; Baraldi, E.; Trenti, T.; Setti, M.; et al. Sperm quality and environment: A retrospective, cohort study in a Northern province of Italy. Environ. Res. 2016, 150, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhou, Y.; Ma, J.; Bao, W.; Li, J.; Zhou, T.; Cui, X.; Peng, Z.; Zhang, H.; Feng, M.; et al. Inverse Association between Ambient Sulfur Dioxide Exposure and Semen Quality in Wuhan, China. Environ. Sci. Technol. 2017, 51, 12806–12814. [Google Scholar] [CrossRef]
- Zheng, P.; Chen, Z.; Shi, J.; Xue, Y.; Bai, Y.; Kang, Y.; Xu, H.; Jia, G.; Wang, T. Association between ambient air pollution and blood sex hormones levels in men. Environ. Res. 2022, 211, 113117. [Google Scholar] [CrossRef] [PubMed]
- Dejmek, J.; Jelínek, R.; Solanský, I.; Beneš, I.; Šrám, R.J. Fecundability and parental exposure to ambient sulfur dioxide. Environ. Health Perspect. 2000, 108, 647–654. [Google Scholar] [CrossRef]
- Chen, Y.A.; Chang, Y.K.; Su, Y.R.; Chang, H.C. Ambient sulfur dioxide could have an impact on testicular volume from a observational study on a population of infertile male. BMC Urol. 2020, 20, 149. [Google Scholar] [CrossRef]
- Zhang, F.; Li, H.; Xu, W.; Song, G.; Wang, Z.; Mao, X.; Wei, Y.; Dai, M.; Zhang, Y.; Shen, Q.; et al. Sulfur dioxide may predominate in the adverse effects of ambient air pollutants on semen quality among the general population in Hefei, China. Sci. Total Environ. 2023, 867, 161472. [Google Scholar] [CrossRef]
- Sun, S.; Zhao, J.; Cao, W.; Lu, W.; Zheng, T.; Zeng, Q. Identifying critical exposure windows for ambient air pollution and semen quality in Chinese men. Environ. Res. 2020, 189, 109894. [Google Scholar] [CrossRef]
- Sokol, R.Z.; Kraft, P.; Fowler, I.M.; Mamet, R.; Kim, E.; Berhane, K.T. Exposure to environmental ozone alters semen quality. Environ. Health Perspect. 2006, 114, 360–365. [Google Scholar] [CrossRef]
- Wang, X.; Tian, X.; Ye, B.; Zhang, Y.; Li, C.; Liao, J.; Zou, Y.; Zhang, S.; Zhu, Y.; Yang, J.; et al. Gaseous pollutant exposure affects semen quality in central China: A cross-sectional study. Andrology 2020, 8, 117–124. [Google Scholar] [CrossRef]
- Ayad, B.M.; Oyeyipo, I.P.; Van der Horst, G.; Du Plessis, S.S. Cementing the relationship between conventional and advanced semen parameters. Middle East. Fertil. Soc. J. 2021, 26, 39. [Google Scholar] [CrossRef]
- Kojima, Y.; Machida, Y.J. DNA-Protein Crosslinks from Environmental Exposure: Mechanisms of Formation and Repair. Environ. Mol. Mutagen. 2020, 61, 716. [Google Scholar] [CrossRef] [PubMed]
- Nakano, T.; Ando, S.; Takata, N.; Kawada, M.; Muguruma, K.; Sekiguchi, K.; Saito, K.; Yonemura, S.; Eiraku, M.; Sasai, Y. Self-formation of optic cups and storable stratified neural retina from human ESCs. Cell Stem Cell 2012, 10, 771–785. [Google Scholar] [CrossRef] [PubMed]
- Bosco, L.; Notari, T.; Ruvolo, G.; Roccheri, M.C.; Martino, C.; Chiappetta, R.; Carone, D.; Bosco, G.L.; Carrillo, L.; Raimondo, S.; et al. Sperm DNA fragmentation: An early and reliable marker of air pollution. Environ. Toxicol. Pharmacol. 2018, 58, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Ayad, B.; Omolaoye, T.S.; Louw, N.; Ramsunder, Y.; Skosana, B.T.; Oyeipo, P.I.; Du Plessis, S.S. Oxidative Stress and Male Infertility: Evidence From a Research Perspective. Front. Reprod. Health 2022, 4, 822257. [Google Scholar] [CrossRef] [PubMed]
- Selevan, S.G.; Borkovec, L.; Slott, V.L.; Zudová, Z.; Rubeš, J.; Evenson, D.P.; Perreault, S.D. Semen quality and reproductive health of young Czech men exposed to seasonal air pollution. Environ. Health Perspect. 2000, 108, 887–894. [Google Scholar] [CrossRef]
- Jurewicz, J.; Radwan, M.; Sobala, W.; Polańska, K.; Radwan, P.; Jakubowski, L.; Ulańska, A.; Hanke, W. The relationship between exposure to air pollution and sperm disomy. Environ. Mol. Mutagen. 2015, 56, 50–59. [Google Scholar] [CrossRef]
- Szczygiet, M.; Kurpisz, M. Chromosomal anomalies in human gametes and pre-implantation embryos, and their potential effect on reproduction. Andrologia 2001, 33, 249–265. [Google Scholar] [CrossRef]
- Robbins, W.A.; Vine, M.F.; Young Truong, K.; Everson, R.B. Use of fluorescence in situ hybridization (FISH] to assess effects of smoking, caffeine, and alcohol on aneuploidy load in sperm of healthy men. Environ. Mol. Mutagen. 1997, 30, 175–183. [Google Scholar] [CrossRef]
- Baumgartner, D.J. Water Pollution—Water Pollution Offences. Valuat. Soc. Cost. 2014, 30–43. [Google Scholar] [CrossRef]
- Recio-Vega, R.; Ocampo-Gómez, G.; Borja-Aburto, V.H.; Moran-Martínez, J.; Cebrian-Garcia, M.E. Organophosphorus pesticide exposure decreases sperm quality: Association between sperm parameters and urinary pesticide levels. J. Appl. Toxicol. 2008, 28, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Jirtle, R.L.; Skinner, M.K. Environmental epigenomics and disease susceptibility. Nat. Rev. Genet. 2007, 8, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Feil, R.; Fraga, M.F. Epigenetics and the environment: Emerging patterns and implications. Nat. Rev. Genet. 2012, 13, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Bind, M.A.; Coull, B.; Suh, H.; Wright, R.; Baccarelli, A.; Vokonas, P.; Schwartz, J. A novel genetic score approach using instruments to investigate interactions between pathways and environment: Application to air pollution. PLoS ONE 2014, 9, e96000. [Google Scholar] [CrossRef] [PubMed]
- Reichard, J.F.; Puga, A. Effects of arsenic exposure on DNA methylation and epigenetic gene regulation. Epigenomics 2010, 2, 87–104. [Google Scholar] [CrossRef] [PubMed]
- Manikkam, M.; Guerrero-Bosagna, C.; Tracey, R.; Haque, M.M.; Skinner, M.K. Transgenerational Actions of Environmental Compounds on Reproductive Disease and Identification of Epigenetic Biomarkers of Ancestral Exposures. PLoS ONE 2012, 7, 31901. [Google Scholar] [CrossRef]
- Landrigan, P.J.; Fuller, R.; Acosta, N.J.R.; Adeyi, O.; Arnold, R.; Baldé, A.B.; Bertollini, R.; Bose-O’Reilly, S.; Boufford, J.I.; Breysse, P.N.; et al. The Lancet Commission on pollution and health. Lancet 2018, 391, 462–512. [Google Scholar] [CrossRef]
- DeMarini, D.M.; Warren, S.H.; Lavrich, K.; Flen, A.; Aurell, J.; Mitchell, W.; Greenwell, D.; Preston, W.; Schmid, J.E.; Linak, W.P.; et al. Mutagenicity and oxidative damage induced by an organic extract of the particulate emissions from a simulation of the deepwater horizon surface oil burns. Environ. Mol. Mutagen. 2017, 58, 162–171. [Google Scholar] [CrossRef]
- Blackburn, E.H.; Epel, E.S.; Lin, J. Human telomere biology: A contributory and interactive factor in aging, disease risks, and protection. Science 2015, 350, 1193–1198. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194. [Google Scholar] [CrossRef]
- Eisenberg, I.W.; Bissett, P.G.; Zeynep Enkavi, A.; Li, J.; MacKinnon, D.P.; Marsch, L.A.; Poldrack, R.A. Uncovering the structure of self-regulation through data-driven ontology discovery. Nat. Commun. 2019, 10, 2319. [Google Scholar] [CrossRef]
- Wdowiak, A.; Wdowiak, E.; Bień, A.; Bojar, I.; Iwanowicz-Palus, G.; Raczkiewicz, D. Air pollution and semen parameters in men seeking fertility treatment for the first time. Int. J. Occup. Med. Environ. Health 2019, 32, 387–399. [Google Scholar] [CrossRef]
- Li, D.; Zhou, Z.; Qing, D.; He, Y.; Wu, T.; Miao, M.; Wang, J.; Weng, X.; Ferber, J.R.; Herrinton, L.J.; et al. Occupational exposure to bisphenol-A (BPA) and the risk of self-reported male sexual dysfunction. Hum. Reprod. 2010, 25, 519–527. [Google Scholar] [CrossRef]
- Zhao, S.; Wang, J.; Xie, Q.; Luo, L.; Zhu, Z.; Liu, Y.; Deng, Y.; Kang, R.; Luo, J.; Zhao, Z. Elucidating Mechanisms of Long-Term Gasoline Vehicle Exhaust Exposure-Induced Erectile Dysfunction in a Rat Model. J. Sex. Med. 2019, 16, 155–167. [Google Scholar] [CrossRef]
- Yafi, F.A.; Jenkins, L.; Albersen, M.; Corona, G.; Isidori, A.M.; Goldfarb, S.; Maggi, M.; Nelson, C.J.; Parish, S.; Salonia, A.; et al. Erectile dysfunction. Nat. Rev. Dis. Prim. 2016, 2, 16003. [Google Scholar] [CrossRef]
- Sooriyamoorthy, T.; Leslie, S.W. Erectile Dysfunction; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Tallon, L.A.; Manjourides, J.; Pun, V.C.; Mittleman, M.A.; Kioumourtzoglou, M.A.; Coull, B.; Suh, H. Erectile dysfunction and exposure to ambient Air pollution in a nationally representative cohort of older Men. Environ. Health 2017, 16, 12. [Google Scholar] [CrossRef]
- Wang, X.; Yang, Y.; Li, J.; Bai, Y.; Tang, Y.; Han, P. Effects of Fine Particulate Matter on Erectile Function and Its Potential Mechanism in Rats. Urology 2017, 102, 265.e9–265.e16. [Google Scholar] [CrossRef]
- Graziani, N.S.; Carreras, H.; Wannaz, E. Atmospheric levels of BPA associated with particulate matter in an urban environment. Heliyon 2019, 5, e01419. [Google Scholar] [CrossRef]
- Yang, T.; Wang, J.; Huang, J.; Kelly, F.J.; Li, G. Long-term Exposure to Multiple Ambient Air Pollutants and Association with Incident Depression and Anxiety. JAMA Psychiatry 2023, 80, 305–313. [Google Scholar] [CrossRef]
- Shi, W.; Sun, C.; Chen, Q.; Ye, M.; Niu, J.; Meng, Z.; Bukulmez, O.; Chen, M.; Teng, X. Association between ambient air pollution and pregnancy outcomes in patients undergoing in vitro fertilization in Shanghai, China: A retrospective cohort study. Environ. Int. 2021, 148, 106377. [Google Scholar] [CrossRef]
- Wu, S.; Zhang, Y.; Hao, G.; Chen, X.; Wu, X.; Ren, H.; Zhang, Y.; Fan, Y.; Du, C.; Bi, X.; et al. Interaction of air pollution and meteorological factors on IVF outcomes: A multicenter study in China. Ecotoxicol. Environ. Saf. 2023, 259, 115015. [Google Scholar] [CrossRef] [PubMed]
- González-Comadran, M.; Jacquemin, B.; Cirach, M.; Lafuente, R.; Cole-Hunter, T.; Nieuwenhuijsen, M.; Brassesco, M.; Coroleu, B.; Checa, M.A. The effect of short term exposure to outdoor air pollution on fertility. Reprod. Biol. Endocrinol. 2021, 19, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Carré, J.; Gatimel, N.; Moreau, J.; Parinaud, J.; Léandri, R. Does air pollution play a role in infertility?: A systematic review. Environ. Health A Glob. Access Sci. Source 2017, 16, 82. [Google Scholar] [CrossRef] [PubMed]
- Thampy, D.; Vieira, V.M. Association between traffic-related air pollution exposure and fertility-assisted births. Environ. Res. Health ERH 2023, 1, 021005. [Google Scholar] [CrossRef]
- Boulet, S.L.; Zhou, Y.; Shriber, J.; Kissin, D.M.; Strosnider, H.; Shin, M. Ambient air pollution and in vitro fertilization treatment outcomes. Hum. Reprod. 2019, 34, 2036–2043. [Google Scholar] [CrossRef]
- Choe, S.A.; Jun, Y.B.; Lee, W.S.; Yoon, T.K.; Kim, S.Y. Association between ambient air pollution and pregnancy rate in women who underwent IVF. Hum. Reprod. 2018, 33, 1071–1078. [Google Scholar] [CrossRef]
- Wang, L.; Luo, D.; Liu, X.; Zhu, J.; Wang, F.; Li, B.; Li, L. Effects of PM2.5 exposure on reproductive system and its mechanisms. Chemosphere 2021, 264, 128436. [Google Scholar] [CrossRef]
- Mudway, I.S.; Kelly, F.J.; Holgate, S.T. Oxidative stress in air pollution research. Free Radic. Biol. Med. 2020, 151, 2–6. [Google Scholar] [CrossRef]
- Weissenberg, A.; Sydlik, U.; Peuschel, H.; Schroeder, P.; Schneider, M.; Schins, R.P.F.; Abel, J.; Unfried, K. Reactive oxygen species as mediators of membrane-dependent signaling induced by ultrafine particles. Free Radic. Biol. Med. 2010, 49, 597–605. [Google Scholar] [CrossRef]
- Leisegang, K. Life Under Aerobic Conditions. In Oxidants, Antioxidants, Impact Oxidative Status Male Reproduction; Academic Press: Cambridg, MA, USA, 2019; pp. 3–8. [Google Scholar] [CrossRef]
- Cocuzza, M.; Athayde, K.S.; Agarwal, A.; Sharma, R.; Pagani, R.; Lucon, A.M.; Srougi, M.; Hallak, J. Age-Related Increase of Reactive Oxygen Species in Neat Semen in Healthy Fertile Men. Urology 2008, 71, 490–494. [Google Scholar] [CrossRef]
- Homa, S.T.; Vessey, W.; Perez-Miranda, A.; Riyait, T.; Agarwal, A. Reactive Oxygen Species (ROS) in human semen: Determination of a reference range. J. Assist. Reprod. Genet. 2015, 32, 757. [Google Scholar] [CrossRef] [PubMed]
- Du Plessis, S.S.; Agarwal, A.; Halabi, J.; Tvrda, E. Contemporary evidence on the physiological role of reactive oxygen species in human sperm function. J. Assist. Reprod. Genet. 2015, 32, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Mannucci, A.; Argento, F.R.; Fini, E.; Coccia, M.E.; Taddei, N.; Becatti, M.; Fiorillo, C. The Impact of Oxidative Stress in Male Infertility. Front. Mol. Biosci. 2022, 8, 799294. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H.; Cheng, J.W.; Ko, E.Y. Role of reactive oxygen species in male infertility: An updated review of literature. Arab. J. Urol. 2018, 16, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Wu, S.D.; Shen, L.J.; Zhao, T.X.; Wei, Y.; Tang, X.L.; Long, C.L.; Zhou, Y.; He, D.W.; Lin, T.; et al. Spermatogenesis dysfunction induced by PM2.5 from automobile exhaust via the ROS-mediated MAPK signaling pathway. Ecotoxicol. Environ. Saf. 2019, 167, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Saffari, A.; Daher, N.; Shafer, M.M.; Schauer, J.J.; Sioutas, C. Global perspective on the oxidative potential of airborne particulate matter: A synthesis of research findings. Environ. Sci. Technol. 2014, 48, 7576–7583. [Google Scholar] [CrossRef]
- Roberts, W. Air pollution and skin disorders. Int. J. Women’s Dermatol. 2021, 7, 91–97. [Google Scholar] [CrossRef]



| Reference | Type of Study Design | Model | Pollutants | Pollutant Concentrations and Duration | Sample Size | Study Outcome |
|---|---|---|---|---|---|---|
| [63] | Experimental | Mice | SO2 | 22, 56, and 112 mg/m3 administered at 6 h/day for 7 days | 30 | ○ Exposure to varying concentrations of SO2 for 7 days, administered 6 h/day resulted in the following: ○ Increased levels of testicular thiobarbituric acid reactive substances (TBARSs) ○ Decreased testicular SOD and GPx activities |
| [65] | Experimental | Mice | SO2 | 3 h/day | 48 | ○ Exposure to SO2 significantly decreased sperm quality and altered the BTB morphology and other ultrastructure of testis ○ Also observed was reduced mRNA expression of testicular occludin, claudin-11, ZO-1, N-cadherin, α-catenin, and connexin-43 |
| [64] | Experimental | Mice | SO2, Arsenic | 5 mg/m3 and/or 5 mg/L of arsenic | ○ Exposure to both SO2 and arsenic: ○ Reduced sperm count ○ Increased percentage of sperm malformation ○ Induced abnormal testicular pathological changes ○ Elevated H2O2 and MDA levels ○ Reduced testicular SOD activity ○ Decreased spermatogenic cell counts ○ Enhanced caspase-3 activity and increased TUNEL-positive cells, hence promoting apoptosis | |
| [66] | Comparative | Male mice | SO2 | ○ Exposure to SO2 induced changes in the social and/or agonistic behavior of these animals ○ They concluded that prenatal SO2 exposure can alter mouse social/agonistic behavior | ||
| [59] | Experimental | Rats | SO2 | 10 ppm, 4 h/day | 16 | ○ Exposure to SO2 resulted in the following: ○ Reduced sperm motility ○ Increased testis weight-to-body weight ○ Abnormal and loose histological arrangement of the spermatogenic cells ○ Increased local structural damage in the seminiferous tubules |
| [60] | Experimental | Rats | PM10, NO2, NOx | 6 h/day for 5 days/week for 3 months | ○ Exposure to the different pollutants caused a reduction in sperm production, and the activity of testicular hyaluronidase was significantly reduced ○ There was a decrease in the number of spermatids count in the seminiferous tubules in stages VI, VII, and VIII tubules in the testes ○ Altered serum sex hormone level was also reported | |
| [61] | Experimental | Rats, Primary spermatogonia, and Leydig cells | PM2.5 | 12 weeks, 24 h | 24 | ○ Animals exposed to PM2.5 presented with reductions in the following: ○ Total sperm count ○ Total motility ○ Sperm concentration ○ Sperm viability ○ Primary testicular spermatogonia and Leydig cells cultured with PM2.5 (0–320 μg/mL) for 24 h decreased cell survival rate, increased reactive oxygen species, lactate dehydrogenase, and 8-hydroxydeoxyguanosine levels, induced DNA damage, endoplasmic reticulum stress, and apoptosis, and inhibited the secretion and synthesis of testosterone in Leydig cells |
| [67] | Experimental | Mice, TM4 cells | PM2.5 | ○ Maternal exposure to PM2.5 resulted in a decreased number of adult offspring and reduced sperm motility ○ Also observed was increased vacuolization in the Sertoli cells of mice exposed to PM2.5 in utero ○ The levels of inhibin and testosterone were reduced and the levels of LH and FSH increased in the PM2.5 groups ○ In vitro exposure of TM4 cells to PM2.5 resulted in the inhibition of cell cycle and also increased apoptosis | ||
| [62] | Experimental | Rats | PM2.5 | Exposed once every 3 days for 2 months | ○ Exposure of rats to varying concentrations of PM2.5 during two seasons (winter and summer) resulted in reduced sperm motility and increased percentage of spermatozoa with abnormal morphology ○ Animals in the winter PM2.5 group showed severe testicular tissue injury, and the reproductive toxicity of winter PM2.5 in the testis was stronger than that of summer PM2.5 ○ Animals exposed to PM2.5 during the summer and winter showed testicular germ cell apoptosis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omolaoye, T.S.; Skosana, B.T.; Ferguson, L.M.; Ramsunder, Y.; Ayad, B.M.; Du Plessis, S.S. Implications of Exposure to Air Pollution on Male Reproduction: The Role of Oxidative Stress. Antioxidants 2024, 13, 64. https://doi.org/10.3390/antiox13010064
Omolaoye TS, Skosana BT, Ferguson LM, Ramsunder Y, Ayad BM, Du Plessis SS. Implications of Exposure to Air Pollution on Male Reproduction: The Role of Oxidative Stress. Antioxidants. 2024; 13(1):64. https://doi.org/10.3390/antiox13010064
Chicago/Turabian StyleOmolaoye, Temidayo S., Bongekile T. Skosana, Lisa Marie Ferguson, Yashthi Ramsunder, Bashir M. Ayad, and Stefan S. Du Plessis. 2024. "Implications of Exposure to Air Pollution on Male Reproduction: The Role of Oxidative Stress" Antioxidants 13, no. 1: 64. https://doi.org/10.3390/antiox13010064
APA StyleOmolaoye, T. S., Skosana, B. T., Ferguson, L. M., Ramsunder, Y., Ayad, B. M., & Du Plessis, S. S. (2024). Implications of Exposure to Air Pollution on Male Reproduction: The Role of Oxidative Stress. Antioxidants, 13(1), 64. https://doi.org/10.3390/antiox13010064







