Overview of Oxidative Stress in Systemic Lupus Erythematosus
Abstract
:1. Introduction
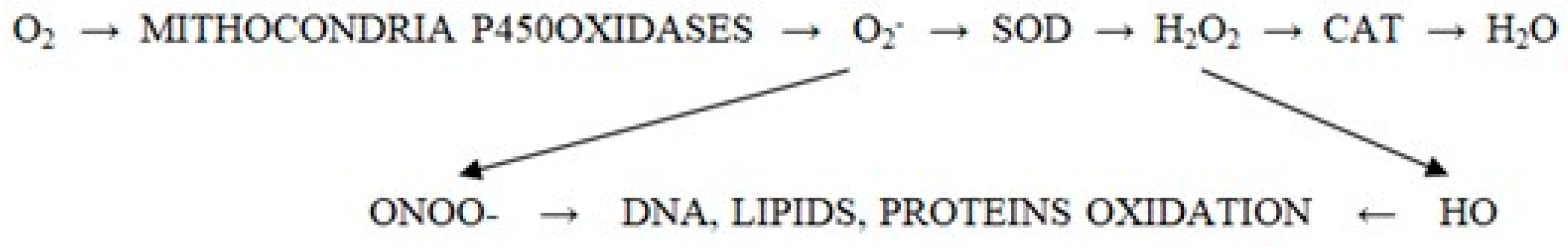
2. Understanding Oxidative Stress
3. Biomarkers of Oxidative Stress in Systemic Lupus Erythematosus
4. The Role and Impact of Oxidative Stress on Organs in Systemic Lupus Erythematosus
5. Therapeutic Strategies Targeting Oxidative Stress
6. Lifestyle Modifications to Reduce Oxidative Stress
7. Downsides of the Most Frequent Therapies
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Perl, A. Oxidative stress in the pathology and treatment of systemic lupus erythematosus. Nat. Rev. Rheumatol. 2013, 9, 674–686. [Google Scholar] [CrossRef] [PubMed]
- Perl, A. Chapter 28—Oxidative Stress in Systemic Lupus Erythematosus: Causes, Consequences, and Treatment. In Systemic Lupus Erythematosus; Tsokos, G.C., Ed.; Academic Press: Cambridge, MA, USA, 2016; pp. 237–242. ISBN 9780128019177. [Google Scholar]
- Justiz Vaillant, A.A.; Goyal, A.; Varacallo, M. Systemic Lupus Erythematosus. [Updated 2023 Aug 4]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK535405/ (accessed on 22 December 2024).
- Song, Y.; Li, J.; Wu, Y. Evolving understanding of autoimmune mechanisms and new therapeutic strategies of autoimmune disorders. Sig. Transduct. Target. Ther. 2024, 9, 263. [Google Scholar] [CrossRef]
- Wójcik, P.; Gęgotek, A.; Žarković, N.; Skrzydlewska, E. Oxidative Stress and Lipid Mediators Modulate Immune Cell Functions in Autoimmune Diseases. Int. J. Mol. Sci. 2021, 22, 723. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y.; Hogquist, K.A. T-cell tolerance: Central and peripheral. Cold Spring Harb. Perspect. Biol. 2012, 4, a006957. [Google Scholar] [CrossRef]
- Smallwood, M.J.; Nissim, A.; Knight, A.R.; Whiteman, M.; Haigh, R.; Winyard, P.G. Oxidative stress in autoimmune rheumatic diseases. Free Radic. Biol. Med. 2018, 125, 3–14. [Google Scholar] [CrossRef]
- Malech, H.L.; Deleo, F.R.; Quinn, M.T. The role of neutrophils in the immune system: An overview. Methods Mol. Biol. 2014, 1124, 3–10. [Google Scholar] [CrossRef]
- Molina-Rios, S.; Rojas-Martinez, R.; Estévez-Ramirez, G.M.; Medina, Y.F. Systemic lupus erythematosus and antiphospholipid syndrome after COVID-19 vaccination. A case report. Mod. Rheumatol. Case Rep. 2023, 7, 43–46. [Google Scholar] [CrossRef]
- Malíčková, K.; Duricová, D.; Bortlík, M.; Hrušková, Z.; Svobodová, B.; Machková, N.; Komárek, V.; Fučíková, T.; Janatková, I.; Zima, T.; et al. Impaired deoxyribonuclease I activity in patients with inflammatory bowel diseases. Autoimmune Dis. 2011, 2011, 945861. [Google Scholar] [CrossRef]
- Lee, D.S.W.; Rojas, O.L.; Gommerman, J.L. B cell depletion therapies in autoimmune disease: Advances and mechanistic insights. Nat. Rev. Drug Discov. 2021, 20, 179–199. [Google Scholar] [CrossRef]
- Ioniuc, I.K.; Lupu, A.; Dragan, F.; Tarnita, I.; Alexoae, M.M.; Streanga, V.; Mitrofan, C.; Thet, A.A.; Nedelcu, A.H.; Salaru, D.L.; et al. Oxidative stress and antioxidants in pediatric asthma’s evolution and management. Antioxidants 2024, 13, 1331. [Google Scholar] [CrossRef]
- Nicola, S.; Borrelli, R.; Corradi, F.; Lo Sardo, L.; Badiu, I.; Romito, A.; Rashidy, N.; Quinternetto, A.; Mazzola, M.; Meli, F.; et al. Relationship between clinical manifestations and serological profile in patients affected by Systemic Lupus Erythematosus. Front. Immunol. 2024, 15, 1390642. [Google Scholar] [CrossRef] [PubMed]
- Ruacho, G.; Lira-Junior, R.; Gunnarsson, I.; Svenungsson, E.; Boström, E.A. Inflammatory markers in saliva and urine reflect disease activity in patients with systemic lupus erythematosus. Lupus Sci. Med. 2022, 9, e000607. [Google Scholar] [CrossRef]
- Kayser, C.; Dutra, L.A.; Dos Reis-Neto, E.T.; Castro, C.H.M.; Fritzler, M.J.; Andrade, L.E.C. The Role of Autoantibody Testing in Modern Personalized Medicine. Clin. Rev. Allergy Immunol. 2022, 63, 251–288. [Google Scholar] [CrossRef] [PubMed]
- Sarma, J.V.; Ward, P.A. The complement system. Cell Tissue Res. 2011, 343, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Dunkelberger, J.; Song, W.C. Complement and its role in innate and adaptive immune responses. Cell Res. 2010, 20, 34–50. [Google Scholar] [CrossRef]
- Usman, N.; Annamaraju, P. Type III Hypersensitivity Reaction. [Updated 2023 May 22]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK559122/ (accessed on 22 December 2024).
- Aringer, M.; Costenbader, K.; Johnson, S.R. Assessing the EULAR/ACR classification criteria for patients with systemic lupus erythematosus. Expert. Rev. Clin. Immunol. 2022, 18, 135–144. [Google Scholar] [CrossRef]
- Lu, W.; Zhong, Y.; Weng, C.; Wang, Q.; Tang, M.; Liu, Z.; Xue, L. Utility of the ACR-1997, SLICC-2012 and EULAR/ACR-2019 classification criteria for systemic lupus erythematosus: A single-centre retrospective study. Lupus Sci. Med. 2022, 9, e000718. [Google Scholar] [CrossRef]
- Rodrigues Fonseca, A.; Felix Rodrigues, M.C.; Sztajnbok, F.R.; Land, M.G.P.; de Oliveira, S.K.F. Comparison among ACR1997, SLICC and the new EULAR/ACR classification criteria in childhood-onset systemic lupus erythematosus. Adv. Rheumatol. 2019, 59, 20. [Google Scholar] [CrossRef]
- Selvaraja, M.; Too, C.L.; Tan, L.K.; Koay, B.T.; Abdullah, M.; Shah, A.M.; Arip, M.; Amin-Nordin, S. Human. leucocyte antigens profiling in Malay. female patients with systemic lupus erythematosus: Are we the same or different? Lupus Sci. Med. 2022, 9, e000554. [Google Scholar] [CrossRef]
- Hsu, T.; Nguyen, P.; Petronic-Rosic, V. A case of systemic lupus erythematosus with cutaneous granulomatous vasculitis. JAAD Case Rep. 2022, 21, 93–96. [Google Scholar] [CrossRef]
- Tayem, M.G.; Shahin, L.; Shook, J.; Kesselman, M.M. A Review of Cardiac Manifestations in Patients With Systemic Lupus Erythematosus and Antiphospholipid Syndrome With Focus on Endocarditis. Cureus 2022, 14, e21698. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Deng, H.; Cui, H.; Fang, J.; Zuo, Z.; Deng, J.; Li, Y.; Wang, X.; Zhao, L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget 2017, 9, 7204–7218. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Selected Immune Disorders and Disability. Selected Immune Disorders and Disability; National Academies Press: Washington, DC, USA, Systemic Lupus Erythematosus. Available online: https://www.ncbi.nlm.nih.gov/books/NBK584485/ (accessed on 24 May 2022).
- Takeshima, Y.; Iwasaki, Y.; Nakano, M.; Narushima, Y.; Ota, M.; Nagafuchi, Y.; Sumitomo, S.; Okamura, T.; Elkon, K.; Ishigaki, K.; et al. Immune cell multiomics analysis reveals contribution of oxidative phosphorylation to B-cell functions and organ damage of lupus. Ann. Rheum. Dis. 2022, 81, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Skudalski, L.; Shahriari, N.; Torre, K.; Santiago, S.; Bibb, L.; Kodomudi, V.; Grant-Kels, J.M.; Lu, J. Emerging therapeutics in the management of connective tissue disease. Part I. Lupus erythematosus and Sjögren syndrome. J. Am. Acad. Dermatol. 2022, 87, 1–18. [Google Scholar] [CrossRef]
- Mukkera, S.; Mannem, M.; Chamarti, K.; Pillarisetty, L.; Vulasala, S.S.; Alahari, L.; Ammu, A.; Mukkera, A.; Vadlapatla, R.K. Systemic Lupus Erythematosus-Associated Serositis Managed With Intravenous Belimumab: A Case Report. Cureus 2022, 14, e22639. [Google Scholar] [CrossRef] [PubMed]
- Emorinken, A.; Dic-Ijiewere, M.O.; Erameh, C.O.; Ugheoke, A.J.; Agbadaola, O.R.; Agbebaku, F.O. Clinical and laboratory profile of systemic lupus erythematosus patients at a rural tertiary centre in South-South Nigeria: Experience from a new rheumatology clinic. Reumatologia 2021, 59, 402–410. [Google Scholar] [CrossRef]
- Burnard, S.; Lechner-Scott, J.; Scott, R.J. EBV and MS: Major cause, minor contribution or red-herring? Mult. Scler. Relat. Disord. 2017, 16, 24–30. [Google Scholar] [CrossRef]
- Francis, L.; Perl, A. Pharmacotherapy of systemic lupus erythematosus. Expert. Opin. Pharmacother. 2009, 10, 1481–1494. [Google Scholar] [CrossRef]
- Ahmad, G.; Almasry, M.; Dhillon, A.S.; Abuayyash, M.M.; Kothandaraman, N.; Cakar, Z. Overview and Sources of Reactive Oxygen Species (ROS) in the Reproductive System. In Oxidative Stress in Human Reproduction; Agarwal, A., Allamaneni, S., Eds.; Springer: Cham, Switzerland, 2017. [Google Scholar] [CrossRef]
- Gilkeson, G.; Cannon, C.; Oates, J.; Rreilly, C.; Goldman, D.; Petri, M. Correlation of serum measures of nitric oxide production with lupus disease activity. J. Rheumatol. 1999, 26, 318–324. [Google Scholar]
- Weichhart, T. Mammalian target of rapamycin: A signaling kinase for every aspect of cellular life. Methods Mol. Biol. 2012, 821, 1–14. [Google Scholar] [CrossRef]
- Huang, N.; Winans, T.; Wyman, B.; Oaks, Z.; Faludi, T.; Choudhary, G.; Lai, Z.-W.; Lewis, J.; Beckford, M.; Duarte, M.; et al. Rab4A-directed endosome traffic shapes pro-inflammatory mitochondrial metabolism in T cells via mitophagy, CD98 expression, and kynurenine-sensitive mTOR activation. Nat. Commun. 2024, 15, 2598. [Google Scholar] [CrossRef]
- Jenks, S.A.; Sanz, I. Altered B cell receptor signaling in human systemic lupus erythematosus. Autoimmun. Rev. 2009, 8, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Mutua, V.; Gershwin, L.J. A Review of Neutrophil Extracellular Traps (NETs) in Disease: Potential Anti-NETs Therapeutics. Clin. Rev. Allergy Immunol. 2021, 61, 194–211. [Google Scholar] [CrossRef] [PubMed]
- Midgley, A.; Watson, L.; Beresford, M.W. New insights into the pathogenesis and management of lupus in children. Arch. Dis. Child. 2014, 99, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Tsai, P.Y.; Ka, S.M.; Chang, J.M.; Lai, J.H.; Dai, M.S.; Jheng, H.L.; Kuo, M.T.; Chen, P.; Chen, A. Antroquinonol differentially modulates T cell activity and reduces interleukin-18 production, but enhances Nrf2 activation, in murine accelerated severe lupus nephritis. Arthritis Rheum. 2012, 64, 232–242. [Google Scholar] [CrossRef]
- Waldmann, H. Mechanisms of immunologicaltolerance. Clin. Biochem. 2016, 49, 324–328. [Google Scholar] [CrossRef]
- Jacob, C.O.; Eisenstein, M.; Dinauer, M.C.; Ming, W.; Liu, Q.; John, S.; Quismorio, F.P., Jr.; Reiff, A.; Myones, B.L.; Kaufman, K.M.; et al. Lupus-associated causal mutation in neutrophil cytosolic factor 2 (NCF2) brings unique insights to the structure and function of NADPH oxidase. Proc. Natl. Acad. Sci. USA. 2012, 109, E59–E67. [Google Scholar] [CrossRef]
- Cyr, A.R.; Domann, F.E. The redox basis of epigenetic modifications: From mechanisms to functional consequences. Antioxid. Redox Signal. 2011, 15, 551–589. [Google Scholar] [CrossRef]
- Pillai, S. Chapter 3—Tolerance and activation of peripheral B and T cells. In The Rose and Mackay Textbook of Autoimmune Diseases, 7th ed.; Gershwin, M.E., Tsokos, G.C., Diamond, B., Eds.; Academic Press: Cambridge, MA, USA, 2024; pp. 27–34. ISBN 9780443239472. [Google Scholar] [CrossRef]
- Lai, Z.W.; Kelly, R.; Winans, T.; Marchena, I.; Shadakshari, A.; Yu, J.; Dawood, M.; Garcia, R.; Tily, H.; Francis, L.; et al. Sirolimus in patients with clinically active systemic lupus erythematosus resistant to, or intolerant of, conventional medications: A single-arm, open-label, phase 1/2 trial. Lancet 2018, 391, 1186–1196. [Google Scholar] [CrossRef] [PubMed]
- Comte, D.; Karampetsou, M.P.; Yoshida, N.; Kis-Toth, K.; Kyttaris, V.C.; Tsokos, G.C. Signaling Lymphocytic Activation Molecule Family Member 7 Engagement Restores Defective Effector CD8+ T Cell Function in Systemic Lupus Erythematosus. Arthritis Rheumatol. 2017, 69, 1035–1044. [Google Scholar] [CrossRef] [PubMed]
- Anolik, J.; Sanz, I. B cells in human and murine systemic lupus erythematosus. Curr. Opin. Rheumatol. 2004, 16, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Chi, H. Regulation and function of mTOR signalling in T cell fate decisions. Nat. Rev. Immunol. 2012, 12, 325–338. [Google Scholar] [CrossRef] [PubMed]
- Tsokos, G.C. Systemic lupus erythematosus. N. Engl. J. Med. 2011, 365, 2110–2121. [Google Scholar] [CrossRef]
- Yan, Z.; Chen, Q.; Xia, Y. Oxidative Stress Contributes to Inflammatory and Cellular Damage in Systemic Lupus Erythematosus: Cellular Markers and Molecular Mechanism. J. Inflamm. Res. 2023, 16, 453–465. [Google Scholar] [CrossRef]
- Halliwell, B.; Gutteridge, J.M. Role of free radicals and catalytic metal ions in human disease: An overview. Methods Enzymol. 1990, 186, 1–85. [Google Scholar] [CrossRef] [PubMed]
- Doherty, E.; Oaks, Z.; Perl, A. Increased mitochondrial electron transport chain activity at complex I is regulated by N-acetylcysteine in lymphocytes of patients with systemic lupus erythematosus. Antioxid. Redox Signal. 2014, 21, 56–65. [Google Scholar] [CrossRef]
- Jog, N.R.; James, J.A. Epstein Barr Virus and Autoimmune Responses in Systemic Lupus Erythematosus. Front. Immunol. 2021, 11, 623944. [Google Scholar] [CrossRef] [PubMed]
- Draborg, A.H.; Duus, K.; Houen, G. Epstein-Barr virus in systemic autoimmune diseases. Clin. Dev. Immunol. 2013, 2013, 535738. [Google Scholar] [CrossRef]
- Perl, A.; Fernandez, D.; Telarico, T.; Phillips, P.E. Endogenous retroviral pathogenesis in lupus. Curr. Opin. Rheumatol. 2010, 22, 483–492. [Google Scholar] [CrossRef]
- Leitinger, N. The role of phospholipid oxidation products in inflammatory and autoimmune diseases: Evidence from animal models and in humans. Subcell. Biochem. 2008, 49, 325–350. [Google Scholar] [CrossRef]
- Otaki, N.; Chikazawa, M.; Nagae, R.; Shimozu, Y.; Shibata, T.; Ito, S.; Takasaki, Y.; Fujii, J.; Uchida, K. Identification of a lipid peroxidation product as the source of oxidation-specific epitopes recognized by anti-DNA autoantibodies. J. Biol. Chem. 2010, 285, 33834–33842. [Google Scholar] [CrossRef]
- Wang, S.; Liu, Y.; Liu, J.; Tian, W.; Zhang, X.; Cai, H.; Fang, S.; Yu, B. Mitochondria-derived methylmalonic acid, a surrogate biomarker of mitochondrial dysfunction and oxidative stress, predicts all-cause and cardiovascular mortality in the general population. Redox Biol. 2020, 37, 101741. [Google Scholar] [CrossRef] [PubMed]
- Suwannaroj, S.; Lagoo, A.; Keisler, D.; McMurray, R.W. Antioxidants suppress mortality in the female NZB x NZW F1 mouse model of systemic lupus erythematosus (SLE). Lupus 2001, 10, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Rho, Y.H.; Chung, C.P.; Oeser, A.; Solus, J.F.; Gebretsadik, T.; Shintani, A.; Raggi, P.; Milne, G.L.; Stein, C.M. Interaction between oxidative stress and high-density lipoprotein cholesterol is associated with severity of coronary artery calcification in rheumatoid arthritis. Arthritis Care Res. 2010, 62, 1473–1480. [Google Scholar] [CrossRef]
- Lai, Z.W.; Hanczko, R.; Bonilla, E.; Caza, T.N.; Clair, B.; Bartos, A.; Miklossy, G.; Jimah, J.; Doherty, E.; Tily, H.; et al. N-acetylcysteine reduces disease activity by blocking mammalian target of rapamycin in T cells from systemic lupus erythematosus patients: A randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2012, 64, 2937–2946. [Google Scholar] [CrossRef]
- Lupu, V.V.; Miron, I.; Trandafir, L.M.; Jechel, E.; Starcea, I.M.; Ioniuc, I.; Frasinariu, O.E.; Mocanu, A.; Petrariu, F.D.; Danielescu, C.; et al. Challenging directions in pediatric diabetes—The place of oxidative stress and antioxidants in systemic decline. Front. Pharmacol. 2024, 15, 1472670. [Google Scholar] [CrossRef] [PubMed]
- Kanderi, T.; Kim, J.; Chan Gomez, J.; Joseph, M.; Bhandari, B. Warm Autoimmune Hemolytic Anemia as the Initial Presentation of Systemic Lupus Erythematosus (SLE): A Case Report. Am. J. Case Rep. 2021, 2, e932965. [Google Scholar] [CrossRef]
- Shah, D.; Kiran, R.; Wanchu, A.; Bhatnagar, A. Oxidative stress in systemic lupus erythematosus: Relationship to Th1 cytokine and disease activity. Immunol. Lett. 2010, 129, 7–12. [Google Scholar] [CrossRef]
- Wang, G.; Pierangeli, S.S.; Papalardo, E.; Ansari, G.A.; Khan, M.F. Markers of oxidative and nitrosative stress in systemic lupus erythematosus: Correlation with disease activity. Arthritis Rheum. 2010, 62, 2064–2072. [Google Scholar] [CrossRef]
- Lai, Z.W.; Borsuk, R.; Shadakshari, A.; Yu, J.; Dawood, M.; Garcia, R.; Francis, L.; Tily, H.; Bartos, A.; Faraone, S.V.; et al. Mechanistic target of rapamycin activation triggers IL-4 production and necrotic death of double-negative T cells in patients with systemic lupus erythematosus. J. Immunol. 2013, 191, 2236–2246. [Google Scholar] [CrossRef]
- Dean, G.S.; Anand, A.; Blofeld, A.; Isenberg, D.A.; Lydyard, P.M. Characterization of CD3+ CD4- CD8- (double negative) T cells in patients with systemic lupus erythematosus: Production of IL-4. Lupus 2002, 11, 501–507. [Google Scholar] [CrossRef]
- Georgescu, L.; Vakkalanka, R.K.; Elkon, K.B.; Crow, M.K. Interleukin-10 promotes activation-induced cell death of SLE lymphocytes mediated by Fas ligand. J. Clin. Investig. 1997, 100, 2622–2633. [Google Scholar] [CrossRef] [PubMed]
- Avalos, I.; Chung, C.P.; Oeser, A.; Milne, G.L.; Morrow, J.D.; Gebretsadik, T.; Shintani, A.; Yu, C.; Stein, C.M. Oxidative stress in systemic lupus erythematosus: Relationship to disease activity and symptoms. Lupus 2007, 16, 195–200. [Google Scholar] [CrossRef]
- Mao, Z.; Tan, Y.; Tao, J.; Li, L.; Wang, H.; Yu, F.; Perl, A.; Zhao, M. Renal mTORC1 activation is associated with disease activity and prognosis in lupus nephritis. Rheumatology 2022, 61, 3830–3840. [Google Scholar] [CrossRef] [PubMed]
- Sinha, A.; Rivera, A.S.; Chadha, S.A.; Prasada, S.; Pawlowski, A.E.; Thorp, E.; DeBerge, M.; Ramsey-Goldman, R.; Lee, Y.C.; Achenbach, C.J.; et al. Comparative Risk of Incident Coronary Heart Disease Across Chronic Inflammatory Diseases. Front. Cardiovasc. Med. 2021, 8, 757738. [Google Scholar] [CrossRef] [PubMed]
- Giannelou, M.; Mavragani, C.P. Cardiovascular disease in systemic lupus erythematosus: A comprehensive update. J. Autoimmun. 2017, 82, 1–12. [Google Scholar] [CrossRef]
- Ioannou, Y.; Zhang, J.Y.; Qi, M.; Gao, L.; Qi, J.C.; Yu, D.M.; Lau, H.; Sturgess, A.D.; Vlachoyiannopoulos, P.G.; Moutsopoulos, H.M.; et al. Novel assays of thrombogenic pathogenicity in the antiphospholipid syndrome based on the detection of molecular oxidative modification of the major autoantigen β2-glycoprotein I. Arthritis Rheum. 2011, 63, 2774–2782. [Google Scholar] [CrossRef]
- Scheen, M.; Adedjouma, A.; Esteve, E.; Buob, D.; Abisror, N.; Planche, V.; Fain, O.; Boffa, J.J.; De Seigneux, S.; Mekinian, A.; et al. Kidney disease in antiphospholipid antibody syndrome: Risk factors, pathophysiology and management. Autoimmun. Rev. 2022, 21, 103072. [Google Scholar] [CrossRef]
- Cavalli, S.; Lonati, P.A.; Gerosa, M.; Caporali, R.; Cimaz, R.; Chighizola, C.B. Beyond Systemic Lupus Erythematosus and Anti-Phospholipid Syndrome: The Relevance of Complement From Pathogenesis to Pregnancy Outcome in Other Systemic Rheumatologic Diseases. Front. Pharmacol. 2022, 13, 841785. [Google Scholar] [CrossRef]
- Jomova, K.; Raptova, R.; Alomar, S.Y.; Alwasel, S.H.; Nepovimova, E.; Kuca, K.; Valko, M. Reactive oxygen species, toxicity, oxidative stress, and antioxidants: Chronic diseases and aging. Arch. Toxicol. 2023, 97, 2499–2574. [Google Scholar] [CrossRef]
- Villanueva, E.; Yalavarthi, S.; Berthier, C.C.; Hodgin, J.B.; Khandpur, R.; Lin, A.M.; Rubin, C.J.; Zhao, W.; Olsen, S.H.; Klinker, M.; et al. Netting neutrophils induce endothelial damage, infiltrate tissues, and expose immunostimulatory molecules in systemic lupus erythematosus. J. Immunol. 2011, 187, 538–552. [Google Scholar] [CrossRef] [PubMed]
- Harley, I.T.W.; Sawalha, A.H. Systemic lupus erythematosus as a genetic disease. Clin. Immunol. 2022, 236, 108953. [Google Scholar] [CrossRef]
- Kunzler, E.; Hynan, L.S.; Chong, B.F. Autoimmune Diseases in Patients With Cutaneous Lupus Erythematosus. JAMA Dermatol. 2018, 154, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Lupu, V.V.; Sasaran, M.O.; Jechel, E.; Starcea, I.M.; Ioniuc, I.; Mocanu, A.; Rosu, S.T.; Munteanu, V.; Nedelcu, A.H.; Danielescu, C.; et al. Celiac disease—A pluripathological model in pediatric practice. Front. Immunol. 2024, 15, 1390755. [Google Scholar] [CrossRef] [PubMed]
- Winans, T.; Oaks, Z.; Choudhary, G.; Patel, A.; Huang, N.; Faludi, T.; Krakko, D.; Nolan, J.; Lewis, J.; Blair, S.; et al. mTOR-dependent loss of PON1 secretion and antiphospholipid autoantibody production underlie autoimmunity-mediated cirrhosis in transaldolase deficiency. J. Autoimmun. 2023, 140, 103112. [Google Scholar] [CrossRef]
- Kunachowicz, D.; Ściskalska, M.; Kepinska, M. Modulatory Effect of Lifestyle-Related, Environmental and Genetic Factors on Paraoxonase-1 Activity: A Review. Int. J. Environ. Res. Public Health 2023, 20, 2813. [Google Scholar] [CrossRef] [PubMed]
- Laniak, O.T.; Winans, T.; Patel, A.; Park, J.; Perl, A. Redox Pathogenesis in Rheumatic Diseases. ACR Open Rheumatol. 2024, 6, 334–346. [Google Scholar] [CrossRef]
- Imagawa, K.; de Andrés, M.C.; Hashimoto, K.; Pitt, D.; Itoi, E.; Goldring, M.B.; Roach, H.I.; Oreffo, R.O. The epigenetic effect of glucosamine and a nuclear factor-kappa B (NF-kB) inhibitor on primary human chondrocytes--implications for osteoarthritis. Biochem. Biophys Res. Commun. 2011, 405, 362–367. [Google Scholar] [CrossRef]
- Lupu, A.; Miron, I.C.; Gavrilovici, C.; Raileanu, A.A.; Starcea, I.M.; Ioniuc, I.; Azoicai, A.; Mocanu, A.; Butnariu, L.I.; Dragan, F.; et al. Pediatric Systemic Lupus Erythematous in COVID-19 Era. Viruses 2023, 15, 272. [Google Scholar] [CrossRef]
- Gupta, M.; Balachandran, H.; Louie, R.H.Y.; Li, H.; Agapiou, D.; Keoshkerian, E.; Christ, D.; Rawlinson, W.; Mina, M.M.; Post, J.J.; et al. High activation levels maintained in receptor-binding domain-specific memory B cells in people with severe coronavirus disease 2019. Immunol. Cell Biol. 2022, 101, 142–155. [Google Scholar] [CrossRef]
- Puskas, F.; Gergely, P., Jr.; Banki, K.; Perl, A. Stimulation of the pentose phosphate pathway and glutathione levels by dehydroascorbate, the oxidized form of vitamin C. FASEB J. 2000, 14, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Stohl, W.; Yu, N.; Chalmers, S.; Putterman, C.; Jacob, C.O. Development of murine systemic lupus erythematosus in the absence of BAFF. Arthritis Rheumatol. 2020, 72, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Ortona, E.; Maselli, A.; Delunardo, F.; Colasanti, T.; Giovannetti, A.; Pierdominici, M. Relationship between redox status and cell fate in immunity and autoimmunity. Antioxid. Redox Signal. 2014, 21, 103–122. [Google Scholar] [CrossRef]
- López-Pedrera, C.; Villalba, J.M.; Patiño-Trives, A.M.; Luque-Tévar, M.; Barbarroja, N.; Aguirre, M.Á.; Escudero-Contreras, A.; Pérez-Sánchez, C. Therapeutic Potential and Immunomodulatory Role of Coenzyme Q10 and Its Analogues in Systemic Autoimmune Diseases. Antioxidants 2021, 10, 600. [Google Scholar] [CrossRef]
- Blanco, L.P.; Pedersen, H.L.; Wang, X.; Lightfoot, Y.L.; Seto, N.; Carmona-Rivera, C.; Yu, Z.X.; Hoffmann, V.; Yuen, P.S.T.; Kaplan, M.J. Improved Mitochondrial Metabolism and Reduced Inflammation Following Attenuation of Murine Lupus With Coenzyme Q10 Analog Idebenone. Arthritis Rheumatol. 2020, 72, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Sánchez, C.; Aguirre, M.Á.; Ruiz-Limón, P.; Ábalos-Aguilera, M.C.; Jiménez-Gómez, Y.; Arias-de la Rosa, I.; Rodriguez-Ariza, A.; Fernández-Del Río, L.; González-Reyes, J.A.; Segui, P.; et al. Ubiquinol Effects on Antiphospholipid Syndrome Prothrombotic Profile: A Randomized, Placebo-Controlled Trial. Arter. Thromb. Vasc. Biol. 2017, 37, 1923–1932. [Google Scholar] [CrossRef]
- Bergamo, P.; Maurano, F.; Rossi, M. Phase 2 enzyme induction by conjugated linoleic acid improves lupus-associated oxidative stress. Free Radic. Biol. Med. 2007, 43, 71–79. [Google Scholar] [CrossRef]
- Lupu, V.V.; Lupu, A.; Jechel, E.; Starcea, I.M.; Stoleriu, G.; Ioniuc, I.; Azoicai, A.; Danielescu, C.; Knieling, A.; Borka-Balas, R.; et al. The role of vitamin D in pediatric systemic lupus erythematosus—A double pawn in the immune and microbial balance. Front. Immunol. 2024, 15, 1373904. [Google Scholar] [CrossRef]
- Nasr, S.; Perl, A. Principles behind SLE treatment with N-acetylcysteine. Immunometabolism 2022, 4, e00010. [Google Scholar] [CrossRef]
- Freire de Carvalho, J.; Skare, T. Coenzyme Q10 supplementation in rheumatic diseases: A systematic review. Clin. Nutr. ESPEN 2024, 59, 63–69. [Google Scholar] [CrossRef]
- Selmi, C.; Tsuneyama, K. Nutrition, geoepidemiology, and autoimmunity. Autoimmun. Rev. 2010, 9, A267–A270. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.C.; Lin, B.F. Dietary factors regulate cytokines in murine models of systemic lupus erythematosus. Autoimmun. Rev. 2011, 11, 22–27. [Google Scholar] [CrossRef]
- De Rosa, V.; Galgani, M.; Santopaolo, M.; Colamatteo, A.; Laccetti, R.; Matarese, G. Nutritional control of immunity: Balancing the metabolic requirements with an appropriate immune function. Semin. Immunol. 2015, 27, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Issazadeh-Navikas, S.; Teimer, R.; Bockermann, R. Influence of dietary components on regulatory T cells. Mol. Med. 2012, 18, 95–110. [Google Scholar] [CrossRef]
- Harbige, L.S. Dietary n-6 and n-3 fatty acids in immunity and autoimmune disease. Proc. Nutr. Soc. 1998, 57, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Bedard, K.; Krause, K.H. The NOX family of ROS-generating NADPH oxidases: Physiology and pathophysiology. Physiol. Rev. 2007, 87, 245–313. [Google Scholar] [CrossRef]
- Lupu, V.V.; Jechel, E.; Mihai, C.M.; Mitrofan, E.C.; Lupu, A.; Starcea, I.M.; Fotea, S.; Mocanu, A.; Ghica, D.C.; Mitrofan, C.; et al. Connection between Celiac Disease and Systemic Lupus Erythematosus in Children—A Development Model of Autoimmune Diseases Starting from What We Inherit to What We Eat. Nutrients 2023, 15, 2535. [Google Scholar] [CrossRef]
- Shah, D.; Mahajan, N.; Sah, S.; Nath, S.K.; Paudyal, B. Oxidative stress and its biomarkers in systemic lupus erythematosus. J. Biomed. Sci. 2014, 21, 23. [Google Scholar] [CrossRef]
- Nesci, S.; Spagnoletta, A.; Oppedisano, F. Inflammation, Mitochondria and Natural Compounds Together in the Circle of Trust. Int. J. Mol. Sci. 2023, 24, 6106. [Google Scholar] [CrossRef]
- Skaggs, B.J.; Hahn, B.H.; McMahon, M. Accelerated atherosclerosis in patients with SLE--mechanisms and management. Nat. Rev. Rheumatol. 2012, 8, 214–223. [Google Scholar] [CrossRef]
- Kong, X.; Liu, J.; Cetinbas, M.; Sadreyev, R.; Koh, M.; Huang, H.; Adeseye, A.; He, P.; Zhu, J.; Russell, H.; et al. New and Preliminary Evidence on Altered Oral and Gut Microbiota in Individuals with Autism Spectrum Disorder (ASD): Implications for ASD Diagnosis and Subtyping Based on Microbial Biomarkers. Nutrients 2019, 11, 2128. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Irastorza, G.; Bertsias, G. Treating systemic lupus erythematosus in the 21st century: New drugs and new perspectives on old drugs. Rheumatology 2020, 59 (Suppl. 5), v69–v81. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Irastorza, G.; Ramos-Casals, M.; Brito-Zeron, P.; Khamashta, M.A. Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: A systematic review. Ann. Rheum. Dis. 2010, 69, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Tselios, K.; Deeb, M.; Gladman, D.D.; Harvey, P.; Urowitz, M.B. Antimalarial-induced cardiomyopathy: A systematic review of the literature. Lupus 2018, 27, 591–599. [Google Scholar] [CrossRef]
- Mok, C.C.; Tse, S.M.; Chan, K.L.; Ho, L.Y. Effect of immunosuppressive therapies on survival of systemic lupus erythematosus: A propensity score analysis of a longitudinal cohort. Lupus 2018, 27, 722–727. [Google Scholar] [CrossRef]
- Ruiz-Arruza, I.; Ugarte, A.; Cabezas-Rodriguez, I.; Medina, J.A.; Moran, M.A.; Ruiz-Irastorza, G. Glucocorticoids and irreversible damage in patients with systemic lupus erythematosus. Rheumatology 2014, 53, 1470–1476. [Google Scholar] [CrossRef]


| Antibodies | Associated Manifestations |
|---|---|
| High anti-dsDNA antibodies | Malar rash and proteinuria |
| High anti-Ro/SSA antibodies | Photosensitivity and pericarditis |
| High anti-Ro antibodies + anti-dsDNA | Proteinuria (a sevenfold increased risk is observed in patients with both antibodies being positive) |
| High anti-La/SSB antibodies | Pericarditis (a threefold increase in the risk) |
| High anti-Smith antibodies | Lupus nephritis and hemolytic anemia and thrombocytopenia. |
| Low complement | Proteinuria |
| Clinical Criteria | |||
|---|---|---|---|
| Mucocutaneous manifestations (Over80% of patients with SLE suffer from mucocutaneous involvement) | Skin | 1. Malar rash—the hallmark acute SLE lesion is the butterfly rash, an erythematous raised pruritic rash on the cheeks and nasal bridge which spares the nasolabial folds. | |
| 2. Discoid rash—chronic cutaneous lesion which may mimic squamous cell carcinoma histologically. | |||
| 3. Photosensitivity. | |||
| Alopecia and Raynaud phenomenon. | |||
| Mucosa | 4. Ulcers of the mouth and nose. | ||
| Serosa manifestations | 5. Serositis (pleuritis; pericarditis—it can cause the inflammation of any heart tissue; Libman–Sacks endocarditis, which is a sterile verrucous endocarditis with vegetations of fibrin and immune cells on the mitral valve; and myocarditis, for which an association between this condition and high anti-Ro (SSA) antibodies has been proven). Moreover, patients suffering from systemic lupus erythematosus (SLE) are predisposed to an elevated risk of developing coronary artery disease, a condition that may be attributable to coronary vasculitis or, more commonly, to widespread atherosclerosis. | ||
| Musculoskeletal manifestations (80 to 90% of individuals with SLE suffer from musculoskeletal involvement at some point during their disease course) | 6. Arthritis is a nonerosive, symmetrical inflammatory polyarthritis affecting predominantly the small joints of the hands, known as Jaccoud arthropathy. This condition results in joint capsule and ligament laxity, leading to subluxation of the metacarpophalangeal joints. These symptoms have been observed in a number of cases, and there is a possibility of these being mistaken for symptoms of rheumatoid arthritis. | ||
| Renal disorder | 7. Glomerulonephritis which is characterized by proteinuria greater than 500 mg daily or RBC in urine or casts. | ||
| Neurologic disorders | 8. Seizures and psychosis. | ||
| Hematologic disorders | 9. Anemia—over 50% of patients with SLE have this condition and can be accompanied by leukopenia of less than 4000/mm3 or thrombocytopenia of less than 100,000/mm3. | ||
| Immunologic criteria | 10. Antinuclear antibodies are very sensitive, but not very specific—ANAs are the signature of the disease and shall be the primary test performed. An immunofluorescence assay is regarded as the gold standard test for ANA. A positive ANA is observed in more than 97% of cases of SLE. It is important to acknowledge that the specificity of this antibody is only 20%, which indicates that a positive ANA does not serve as definitive confirmation of a diagnosis of SLE due to the fact that a significant proportion of the healthy population may have high levels of ANA. However, a negative ANA significantly reduces the likelihood of a diagnosis being made. | ||
| 11.a. Anti-Smith—binds to ribonucleoproteins. | |||
| 11.b. Anti dsDNA—binds to double stranded DNA and is seen during active disease. | |||
| 11.c. Anti-phospholipid—usually targets the proteins which are bound to phospholipids. The presence of these antibodies leads to a hypercoagulable state → deep vein thrombosis, hepatic vein thrombosis, and stroke. As a result, lifelong anticoagulation therapy is needed. There are three types of anti-phospholipid antibodies. | Anticardiolipin—which can prove to be a false-positive for syphilis. | ||
| Lupus anticoagulant. | |||
| Anti-B2 glycoprotein. | |||
| Diagnostic Time | ACR1997 | SLICC 2012 |
|---|---|---|
| Clinical time | 204 | 259 |
| Earlier than clinical diagnosis | 8 | 17 |
| Later than clinical diagnosis | 33 | 17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lupu, A.; Stoleriu, G.; Nedelcu, A.H.; Perju, S.N.; Gavrilovici, C.; Baciu, G.; Mihai, C.M.; Chisnoiu, T.; Morariu, I.D.; Grigore, E.; et al. Overview of Oxidative Stress in Systemic Lupus Erythematosus. Antioxidants 2025, 14, 303. https://doi.org/10.3390/antiox14030303
Lupu A, Stoleriu G, Nedelcu AH, Perju SN, Gavrilovici C, Baciu G, Mihai CM, Chisnoiu T, Morariu ID, Grigore E, et al. Overview of Oxidative Stress in Systemic Lupus Erythematosus. Antioxidants. 2025; 14(3):303. https://doi.org/10.3390/antiox14030303
Chicago/Turabian StyleLupu, Ancuta, Gabriela Stoleriu, Alin Horatiu Nedelcu, Sara Nadeea Perju, Cristina Gavrilovici, Ginel Baciu, Cristina Maria Mihai, Tatiana Chisnoiu, Ionela Daniela Morariu, Ecaterina Grigore, and et al. 2025. "Overview of Oxidative Stress in Systemic Lupus Erythematosus" Antioxidants 14, no. 3: 303. https://doi.org/10.3390/antiox14030303
APA StyleLupu, A., Stoleriu, G., Nedelcu, A. H., Perju, S. N., Gavrilovici, C., Baciu, G., Mihai, C. M., Chisnoiu, T., Morariu, I. D., Grigore, E., Shawais, S. K., Salaru, D. L., Revenco, N., & Lupu, V. V. (2025). Overview of Oxidative Stress in Systemic Lupus Erythematosus. Antioxidants, 14(3), 303. https://doi.org/10.3390/antiox14030303







