Comparisons of Outcomes between Patients with Direct and Indirect Acute Respiratory Distress Syndrome Receiving Extracorporeal Membrane Oxygenation
Abstract
:1. Introduction
2. Materials and Methods
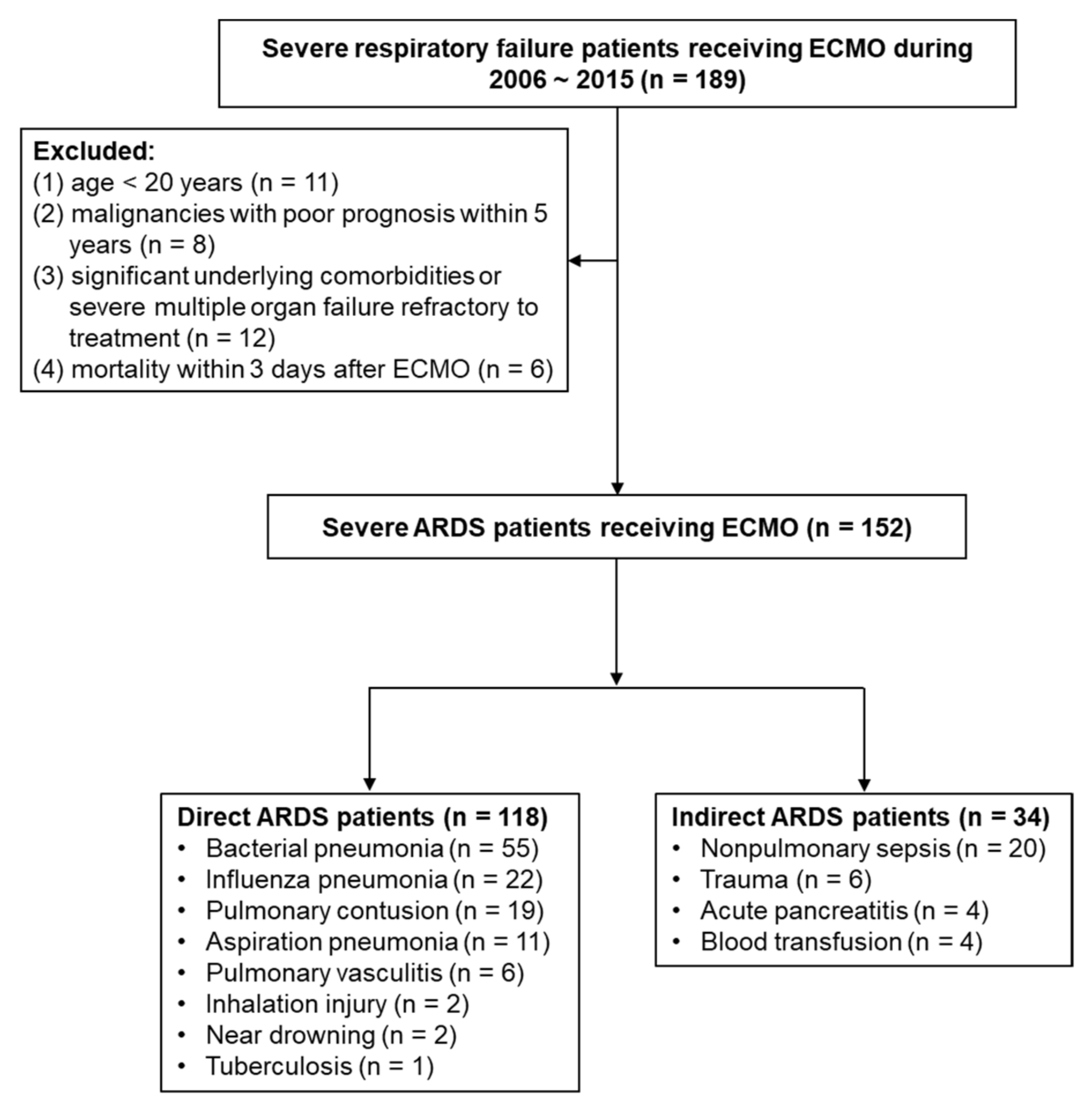
2.1. Study Design and Patient Inclusion
2.2. Definitions
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Study Patients
3.2. Comparisons of Direct and Indirect ARDS Patients
3.3. Clinical Outcomes of Direct and Indirect ARDS Patients
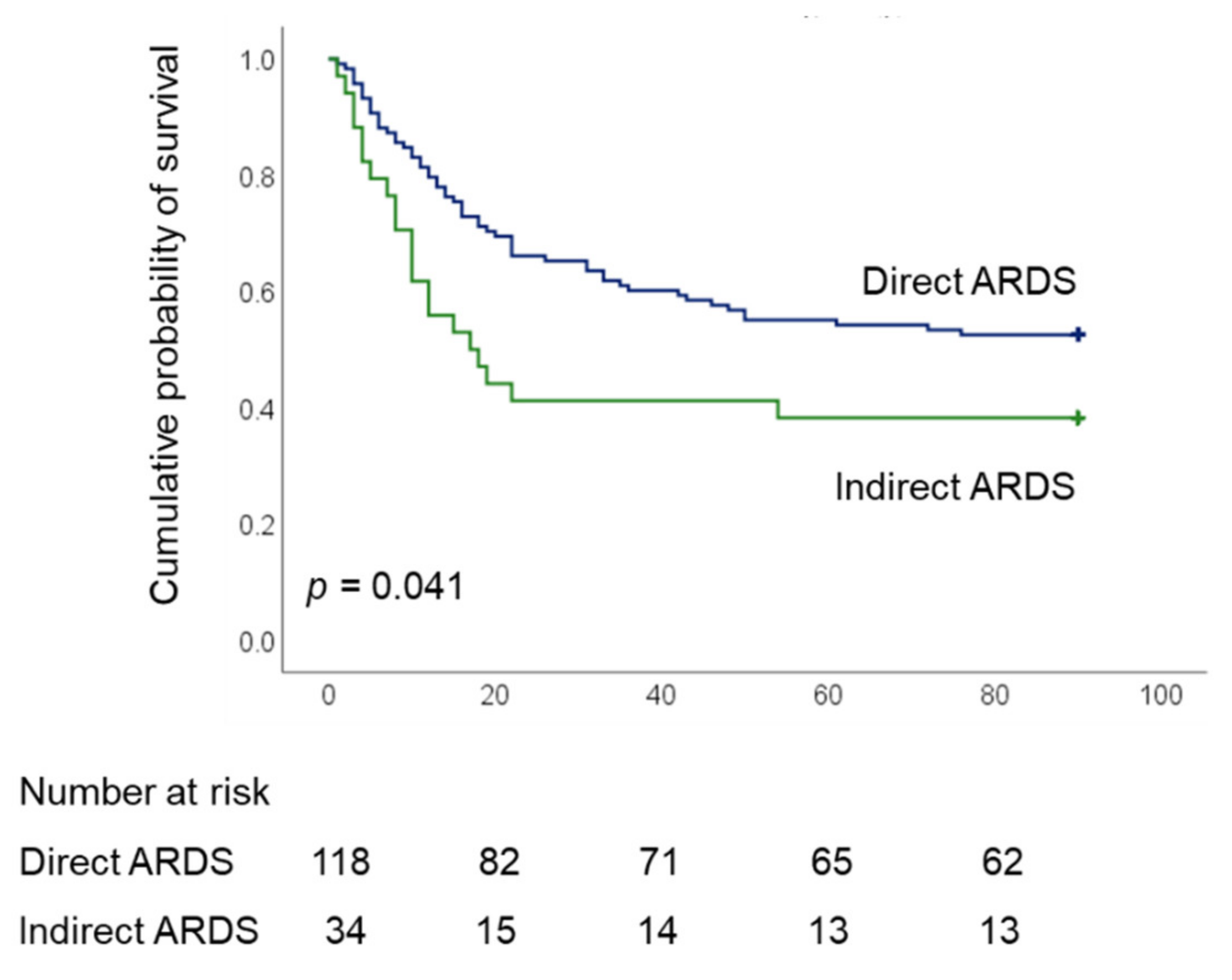
3.4. Comparison of Direct and Indirect ARDS Patients in Terms of Survival
3.5. Factors Associated with Hospital Mortality in Cases of Direct and Indirect ARDS
3.6. Comparisons of Direct and Indirect ARDS Patients after Excluding VA ECMO Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thompson, B.T.; Chambers, R.C.; Liu, K.D. Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2017, 377, 562–572. [Google Scholar] [CrossRef]
- Gattinoni, L.; Pelosi, P.; Suter, P.M.; Pedoto, A.; Vercesi, P.; Lissoni, A. Acute respiratory distress syndrome caused by pulmonary and extrapulmonary disease. Different syndromes? Am. J. Respir. Crit. Care Med. 1998, 158, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Pelosi, P.; D’Onofrio, D.; Chiumello, D.; Paolo, S.; Chiara, G.; Capelozzi, V.L.; Barbas, C.S.; Chiaranda, M.; Gattinoni, L. Pulmonary and extrapulmonary acute respiratory distress syndrome are different. Eur. Respir. J. Suppl. 2003, 42, 48s–56s. [Google Scholar] [CrossRef] [Green Version]
- Coppola, S.; Froio, S.; Marino, A.; Brioni, M.; Cesana, B.M.; Cressoni, M.; Gattinoni, L.; Chiumello, D. Respiratory Mechanics, Lung Recruitability, and Gas Exchange in Pulmonary and Extrapulmonary Acute Respiratory Distress Syndrome. Crit. Care Med. 2019, 47, 792–799. [Google Scholar] [CrossRef]
- Shaver, C.M.; Bastarache, J.A. Clinical and biological heterogeneity in acute respiratory distress syndrome: Direct versus indirect lung injury. Clin. Chest Med. 2014, 35, 639–653. [Google Scholar] [CrossRef] [Green Version]
- Calfee, C.S.; Janz, D.R.; Bernard, G.R.; May, A.K.; Kangelaris, K.N.; Matthay, M.A.; Ware, L.B. Distinct molecular phenotypes of direct vs indirect ARDS in single-center and multicenter studies. Chest 2015, 147, 1539–1548. [Google Scholar] [CrossRef] [Green Version]
- Sinha, P.; Calfee, C.S. Phenotypes in acute respiratory distress syndrome: Moving towards precision medicine. Curr. Opin. Crit. Care 2019, 25, 12–20. [Google Scholar] [CrossRef]
- Wilson, J.G.; Calfee, C.S. ARDS Subphenotypes: Understanding a Heterogeneous Syndrome. Crit. Care 2020, 24, 102. [Google Scholar] [CrossRef] [Green Version]
- Englert, J.A.; Bobba, C.; Baron, R.M. Integrating molecular pathogenesis and clinical translation in sepsis-induced acute respiratory distress syndrome. JCI Insight 2019, 4, e124061. [Google Scholar] [CrossRef] [Green Version]
- Eisner, M.D.; Thompson, T.; Hudson, L.D.; Luce, J.M.; Hayden, D.; Schoenfeld, D.; Matthay, M.A. Acute Respiratory Distress Syndrome Network. Efficacy of low tidal volume ventilation in patients with different clinical risk factors for acute lung injury and the acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2001, 164, 231–236. [Google Scholar] [CrossRef]
- Luo, L.; Shaver, C.M.; Zhao, Z.; Koyama, T.; Calfee, C.S.; Bastarache, J.A.; Ware, L.B. Clinical Predictors of Hospital Mortality Differ Between Direct and Indirect ARDS. Chest 2017, 151, 755–763. [Google Scholar] [CrossRef] [Green Version]
- Abrams, D.; Schmidt, M.; Pham, T.; Beitler, J.R.; Fan, E.; Goligher, E.C.; McNamee, J.J.; Patroniti, N.; Wilcox, M.E.; Combes, A.; et al. Mechanical Ventilation for Acute Respiratory Distress Syndrome during Extracorporeal Life Support. Research and Practice. Am. J. Respir Crit. Care Med. 2020, 201, 514–525. [Google Scholar] [CrossRef]
- Rozencwajg, S.; Pilcher, D.; Combes, A.; Schmidt, M. Outcomes and survival prediction models for severe adult acute respiratory distress syndrome treated with extracorporeal membrane oxygenation. Crit. Care 2016, 20, 392. [Google Scholar] [CrossRef] [Green Version]
- Giani, M.; Redaelli, S.; Siragusa, A.; Fumagalli, B.; Rona, R.; Foti, G. Extracorporeal Gas Exchange for Acute Respiratory Distress Syndrome: Open Questions, Controversies and Future Directions. Membranes 2021, 11, 172. [Google Scholar] [CrossRef]
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar]
- Chiu, L.C.; Lin, S.W.; Chuang, L.P.; Li, H.H.; Liu, P.H.; Tsai, F.C.; Chang, C.H.; Hung, C.Y.; Lee, C.S.; Leu, S.W.; et al. Mechanical power during extracorporeal membrane oxygenation and hospital mortality in patients with acute respiratory distress syndrome. Crit. Care 2021, 25, 13. [Google Scholar] [CrossRef]
- Sinha, P.; Calfee, C.S.; Beitler, J.R.; Soni, N.; Ho, K.; Matthay, M.A.; Kallet, R.H. Physiologic Analysis and Clinical Performance of the Ventilatory Ratio in Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2019, 199, 333–341. [Google Scholar] [CrossRef]
- Schmidt, M.; Bailey, M.; Sheldrake, J.; Hodgson, C.; Aubron, C.; Rycus, P.T.; Scheinkestel, C.; Cooper, D.J.; Brodie, D.; Pellegrino, V. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am. J. Respir. Crit. Care Med. 2014, 189, 1374–1382. [Google Scholar] [CrossRef]
- Robba, C.; Ortu, A.; Bilotta, F.; Lombardo, A.; Sekhon, M.S.; Gallo, F.; Matta, B.F. Extracorporeal membrane oxygenation for adult respiratory distress syndrome in trauma patients: A case series and systematic literature review. J. Trauma Acute Care Surg. 2017, 82, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Chiu, L.C.; Chuang, L.P.; Leu, S.W.; Lin, Y.J.; Chang, C.J.; Li, H.H.; Tsai, F.C.; Chang, C.H.; Hung, C.Y.; Lin, S.W.; et al. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome: Propensity Score Matching. Membranes 2021, 11, 393. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Stewart, C.; Bailey, M.; Nieszkowska, A.; Kelly, J.; Murphy, L.; Pilcher, D.; Cooper, D.J.; Scheinkestel, C.; Pellegrino, V.; et al. Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome: A retrospective international multicenter study. Crit. Care Med. 2015, 43, 654–664. [Google Scholar] [CrossRef] [Green Version]
- Serpa, N.A.; Schmidt, M.; Azevedo, L.C.; Bein, T.; Brochard, L.; Beutel, G.; Combes, A.; Costa, E.L.; Hodgson, C.; Lindskov, C.; et al. ReVA Research Network and the PROVE Network Investigators. Associations between ventilator settings during extracorporeal membrane oxygenation for refractory hypoxemia and outcome in patients with acute respiratory distress syndrome: A pooled individual patient data analysis: Mechanical ventilation during ECMO. Intensive Care Med. 2016, 42, 1672–1684. [Google Scholar]
- Kim, H.S.; Kim, J.H.; Chung, C.R.; Hong, S.B.; Cho, W.H.; Cho, Y.J.; Sim, Y.S.; Kim, W.Y.; Kang, B.J.; Park, S.H.; et al. Lung Compliance and Outcomes in Patients With Acute Respiratory Distress Syndrome Receiving ECMO. Ann. Thorac. Surg. 2019, 108, 176–182. [Google Scholar] [CrossRef]
- Calfee, C.S.; Delucchi, K.; Parsons, P.E.; Thompson, B.T.; Ware, L.B.; Matthay, M.A.; NHLBI ARDS Network. Subphenotypes in acute respiratory distress syndrome: Latent class analysis of data from two randomised controlled trials. Lancet Respir. Med. 2014, 2, 611–620. [Google Scholar] [CrossRef] [Green Version]
- Kon, Z.N.; Bittle, G.J.; Pasrija, C.; Pham, S.M.; Mazzeffi, M.A.; Herr, D.L.; Sanchez, P.G.; Griffith, B.P. Venovenous Versus Venoarterial Extracorporeal Membrane Oxygenation for Adult Patients With Acute Respiratory Distress Syndrome Requiring Precannulation Hemodynamic Support: A Review of the ELSO Registry. Ann. Thorac. Surg. 2017, 104, 645–649. [Google Scholar] [CrossRef] [Green Version]
- Thiagarajan, R.R.; Barbaro, R.P.; Rycus, P.T.; Mcmullan, D.M.; Conrad, S.A.; Fortenberry, J.D.; Paden, M.L. ELSO member centers. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J. 2017, 63, 60–67. [Google Scholar] [CrossRef]
- Kim, H.; Paek, J.H.; Song, J.H.; Lee, H.; Jhee, J.H.; Park, S.; Yun, H.R.; Kee, Y.K.; Han, S.H.; Yoo, T.H.; et al. Permissive fluid volume in adult patients undergoing extracorporeal membrane oxygenation treatment. Crit. Care 2018, 22, 270. [Google Scholar] [CrossRef] [Green Version]
- Ostermann, M.; Straaten, H.M.; Forni, L.G. Fluid overload and acute kidney injury: Cause or consequence? Crit. Care 2015, 19, 443. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, M.; Pham, T.; Arcadipane, A.; Agerstrand, C.; Ohshimo, S.; Pellegrino, V.; Vuylsteke, A.; Guervilly, C.; McGuinness, S.; Pierard, S.; et al. Mechanical Ventilation Management during Extracorporeal Membrane Oxygenation for Acute Respiratory Distress Syndrome. An International Multicenter Prospective Cohort. Am. J. Respir Crit Care Med. 2019, 200, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Curley, G.F.; Laffey, J.G.; Zhang, H.; Slutsky, A.S. Biotrauma and Ventilator-Induced Lung Injury: Clinical Implications. Chest 2016, 150, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Christiani, D.C.; Thompson, B.T.; Bajwa, E.K.; Gong, M.N. Role of diabetes in the development of acute respiratory distress syndrome. Crit. Care Med. 2013, 41, 2720–2732. [Google Scholar] [CrossRef]
- Boyle, A.J.; Madotto, F.; Laffey, J.G.; Bellani, G.; Pham, T.; Pesenti, A.; Thompson, B.T.; O’Kane, C.M.; Deane, A.M.; McAuley, D.F.; et al. Identifying associations between diabetes and acute respiratory distress syndrome in patients with acute hypoxemic respiratory failure: An analysis of the LUNG SAFE database. Crit. Care 2018, 22, 268. [Google Scholar] [CrossRef] [Green Version]
- Fujii, Y.; Abe, T.; Ikegami, K. Diabetic Pathophysiology Enhances Inflammation during Extracorporeal Membrane Oxygenation in a Rat Model. Membranes 2021, 11, 283. [Google Scholar] [CrossRef]
- Lin, P.; Zhao, Y.; Li, X.; Jiang, F.; Liang, Z. Decreased mortality in acute respiratory distress syndrome patients treated with corticosteroids: An updated meta-analysis of randomized clinical trials with trial sequential analysis. Crit. Care 2021, 25, 122. [Google Scholar] [CrossRef]
| Variables | All | Direct ARDS | Indirect ARDS | p |
|---|---|---|---|---|
| (n = 152) | (n = 118) | (n = 34) | ||
| Age (years) | 50.3 ± 16.4 | 50.8 ± 16.3 | 48.5 ± 16.6 | 0.463 |
| Gender (male) | 103 (67.8%) | 83 (70.3%) | 20 (58.8%) | 0.206 |
| Body mass index (kg/m2) | 25.8 ± 5.3 | 25.9 ± 5.4 | 25.5 ± 4.8 | 0.766 |
| Diabetes mellitus | 40 (26%) | 33 (28%) | 7 (20.6%) | 0.389 |
| Chronic liver disease | 21 (14%) | 16 (13.6%) | 5 (14.7%) | 0.864 |
| Immunocompromised status | 40 (26%) | 28 (23.7%) | 12 (35.3%) | 0.177 |
| Chronic kidney disease | 17 (11.2%) | 13 (11%) | 4 (11.8%) | 1.000 |
| SOFA score before ECMO | 10.8 ± 3.2 | 10.6 ± 3.0 | 11.5 ± 3.4 | 0.154 |
| Lung injury score before ECMO | 3.4 ± 0.4 | 3.4 ± 0.4 | 3.3 ± 0.4 | 0.036 |
| ARDS duration before ECMO (h) | 28 (7–122) | 29 (7–122) | 24 (5–192) | 0.306 |
| pH before ECMO | 7.28 ± 0.14 | 7.28 ± 0.14 | 7.26 ± 0.13 | 0.494 |
| PaCO2 (mm Hg) before ECMO | 52.5 ± 19.0 | 52.6 ± 19.2 | 51.9 ± 18.6 | 0.848 |
| PaO2/FiO2 (mm Hg) before ECMO | 63 (52–88) | 63 (52–87) | 65 (53–97) | 0.430 |
| Ventilator settings before ECMO | ||||
| Mechanical power (J/min) | 23.8 ± 9.6 | 24.7 ± 9.5 | 20.5 ± 9.4 | 0.023 |
| Tidal volume (mL/kg PBW) | 7.7 ± 2.4 | 7.7 ± 2.3 | 7.7 ± 2.9 | 0.981 |
| PEEP (cm H2O) | 12.0 ± 2.8 | 12.2 ± 2.8 | 11.3 ± 2.8 | 0.106 |
| Peak inspiratory pressure (cm H2O) | 33.9 ± 6.5 | 34.2 ± 6.5 | 33.2 ± 6.6 | 0.457 |
| Mean airway pressure (cm H2O) | 18.6 ± 4.4 | 19.0 ± 4.4 | 17.5 ± 4.4 | 0.094 |
| Dynamic compliance (mL/cm H2O) | 22.6 ± 11.3 | 22.8 ± 11.2 | 21.8 ± 11.8 | 0.680 |
| Minute ventilation (L/min) | 10.6 ± 3.8 | 11.0 ± 3.9 | 9.2 ± 3.3 | 0.019 |
| Ventilatory ratio | 2.5 ± 1.1 | 2.5 ± 1.0 | 2.3 ± 1.2 | 0.183 |
| ECMO venoarterial mode | 24 (15.8%) | 14 (11.9%) | 10 (29.4%) | 0.013 |
| SOFA score from day 1 to day 3 on ECMO | 9.6 ± 2.3 | 9.4 ± 2.2 | 10.6 ± 2.3 | 0.015 |
| pH from day1 to day 3 on ECMO | 7.43 ± 0.08 | 7.44 ± 0.08 | 7.42 ± 0.08 | 0.146 |
| PaCO2 (mm Hg) from day1 to day 3 on ECMO | 38.2 ± 5.3 | 38.2 ± 5.1 | 38.2 ± 6.1 | 0.999 |
| PaO2/FiO2 (mm Hg) from day 1 to day 3 on ECMO | 178 (131–240) | 167 (130–224) | 194 (150–248) | 0.857 |
| Ventilator settings from day 1 to day 3 on ECMO | ||||
| Mechanical power (J/min) | 12.1 ± 6.2 | 12.0 ± 6.2 | 12.3 ± 6.7 | 0.867 |
| Tidal volume (mL/kg PBW) | 6.0 ± 2.2 | 6.1 ± 2.1 | 5.9 ± 2.7 | 0.705 |
| PEEP (cm H2O) | 12.0 ± 3.3 | 12.4 ± 3.4 | 10.7 ± 2.5 | 0.008 |
| Peak inspiratory pressure (cm H2O) | 31.7 ± 5.6 | 31.6 ± 5.9 | 32.2 ± 4.8 | 0.596 |
| Mean airway pressure (cm H2O) | 17.7 ± 4.0 | 17.9 ± 4.3 | 17.0 ± 2.9 | 0.196 |
| Dynamic compliance (mL/cm H2O) | 19.2 ± 8.1 | 19.7 ± 7.7 | 17.4 ± 9.3 | 0.153 |
| Minute ventilation (L/min) | 5.7 ± 2.8 | 5.6 ± 2.7 | 5.8 ± 3.1 | 0.679 |
| Fluid balance, ml | ||||
| Before ECMO | 923 (−258 to 2125) | 884 (−193 to 2145) | 1125 (−486 to 2094) | 0.836 |
| Cumulative 3 days | 1190 (−873 to 3935) | 947 (−1355 to 3253) | 1844 (−208 to 5679) | 0.046 |
| Inotropes (n) | 133 (87.5%) | 102 (86.4%) | 31 (91.2%) | 0.568 |
| Outcomes | Direct ARDS | Indirect ARDS | p |
|---|---|---|---|
| (n = 118) | (n = 34) | ||
| Mortality | |||
| 28 day hospital mortality, n (%) | 41 (34.7%) | 20 (58.8%) | 0.005 |
| 60 day hospital mortality, n (%) | 53 (44.9%) | 21 (61.8%) | 0.025 |
| 90 day hospital mortality, n (%) | 56 (47.5%) | 21 (61.8%) | 0.041 |
| Other outcomes | |||
| Duration of ECMO (days) | 10 (6–16) | 7 (4–11) | 0.044 |
| Duration of mechanical ventilator (days) | 22 (12–40) | 18 (10–34) | 0.201 |
| Length of ICU stay (days) | 25 (15–46) | 22 (11–38) | 0.191 |
| Length of hospital stay (days) | 42 (22–65) | 33 (19–68) | 0.626 |
| ECMO-free days at day 28 | 0 (0–9) | 0 (0–19) | 0.126 |
| Ventilator–free days on day 28 | 0 (0–9) | 0 (0–0) | 0.135 |
| Ventilator–free days on day 60 | 0 (0–41) | 0 (0–30) | 0.145 |
| Variables | Direct ARDS (n = 118) | Indirect ARDS (n = 34) | ||||
|---|---|---|---|---|---|---|
| Survivors | Non-Survivors | p | Survivors | Non-Survivors | p | |
| (n = 59) | (n = 59) | (n = 12) | (n = 22) | |||
| Age (years) | 47.3 ± 15.7 | 54.4 ± 16.3 | 0.017 | 39.8 ± 19.3 | 53.2 ± 13.1 | 0.022 |
| Gender (male) | 40 (67.8%) | 43 (72.9%) | 0.545 | 8 (66.7%) | 12 (54.5%) | 0.717 |
| Body mass index (kg/m2) | 26.4 ± 6.1 | 25.3 ± 4.7 | 0.292 | 24.1 ± 4.2 | 26.5 ± 5.1 | 0.218 |
| Diabetes mellitus | 21 (35.6%) | 12 (20.3%) | 0.065 | 2 (16.7%) | 5 (22.7%) | 1.000 |
| Chronic liver disease | 6 (10.2%) | 10 (16.9%) | 0.282 | 0 | 5 (22.7%) | 0.137 |
| Immunocompromised status | 8 (13.6%) | 20 (33.9%) | 0.009 | 3 (25%) | 9 (40.9%) | 0.465 |
| Chronic kidney disease | 8 (13.6%) | 5 (8.5%) | 0.378 | 0 | 4 (18.2%) | 0.273 |
| SOFA score before ECMO | 10.4 ± 3.0 | 10.8 ± 3.1 | 0.509 | 9.8 ± 3.2 | 12.5 ± 3.2 | 0.024 |
| Lung injury score before ECMO | 3.5 ± 0.4 | 3.3 ± 0.5 | 0.055 | 3.2 ± 0.6 | 3.3 ± 0.4 | 0.554 |
| ARDS duration before ECMO (h) | 10 (5–70) | 63 (16–154) | 0.003 | 6 (1–34) | 38 (16–355) | 0.018 |
| pH before ECMO | 7.28 ± 0.13 | 7.28 ± 0.15 | 0.731 | 7.26 ± 0.09 | 7.26 ± 0.16 | 0.989 |
| PaCO2 (mm Hg) before ECMO | 51.6 ± 21.0 | 53.6 ± 17.4 | 0.572 | 46.3 ± 9.9 | 54.9 ± 21.5 | 0.117 |
| PaO2/FiO2 (mm Hg) before ECMO | 61 (50–77) | 64 (52–107) | 0.083 | 75 (60–101) | 57 (51–98) | 0.495 |
| Ventilator settings before ECMO | ||||||
| Mechanical power (J/min) | 24.8 ± 10.5 | 24.6 ± 8.5 | 0.877 | 20.5 ± 8.8 | 20.4 ± 9.8 | 0.974 |
| Tidal volume (mL/kg PBW) | 7.7 ± 2.3 | 7.8 ± 2.3 | 0.722 | 7.6 ± 2.6 | 7.8 ± 3.1 | 0.791 |
| PEEP (cm H2O) | 12.4 ± 2.5 | 11.9 ± 3.1 | 0.343 | 11.3 ± 2.8 | 11.3 ± 2.8 | 0.952 |
| Peak inspiratory pressure (cm H2O) | 33.7 ± 5.9 | 34.6 ± 7.1 | 0.481 | 33.3 ± 7.1 | 33.2 ± 6.5 | 0.978 |
| Mean airway pressure (cm H2O) | 18.7 ± 4.1 | 19.2 ± 4.7 | 0.587 | 16.9 ± 4.3 | 17.9 ± 4.5 | 0.554 |
| Dynamic compliance (mL/cm H2O) | 24.1 ± 12.2 | 21.4 ± 10.0 | 0.207 | 19.9 ± 6.9 | 23.1 ± 14.1 | 0.469 |
| Minute ventilation (L/min) | 10.9 ± 4.2 | 11.0 ± 3.5 | 0.837 | 9.5 ± 3.1 | 9.1 ± 3.5 | 0.740 |
| Ventilatory ratio | 2.4 ± 1.0 | 2.6 ± 1.1 | 0.280 | 2.0 ± 0.8 | 2.4 ± 1.4 | 0.350 |
| ECMO venoarterial mode | 4 (6.8%) | 10 (16.9%) | 0.153 | 2 (16.7%) | 8 (36.4%) | 0.432 |
| SOFA score from day 1 to day 3 on ECMO | 8.8 ± 1.8 | 10.1 ± 2.4 | 0.001 | 9.5 ± 2.1 | 11.3 ± 2.3 | 0.060 |
| pH from day1 to day 3 on ECMO | 7.46 ± 0.06 | 7.42 ± 0.09 | 0.006 | 7.45 ± 0.08 | 7.40 ± 0.08 | 0.138 |
| PaCO2 (mm Hg) from day1 to day 3 on ECMO | 38.2 ± 4.9 | 38.2 ± 5.3 | 0.960 | 37.4 ± 5.5 | 38.6 ± 6.4 | 0.586 |
| PaO2/FiO2 (mm Hg) from day 1 to day 3 on ECMO | 194 (145–247) | 151 (122–203) | 0.844 | 224 (171–287) | 184 (134–237) | 0.313 |
| Ventilator settings from day 1 to day 3 on ECMO | ||||||
| Mechanical power (J/min) | 11.2 ± 4.4 | 12.9 ± 7.4 | 0.136 | 9.4 ± 3.4 | 13.8 ± 7.5 | 0.026 |
| volume (mL/kg PBW) | 6.0 ± 2.0 | 6.1 ± 2.1 | 0.878 | 6.1 ± 2.1 | 5.8 ± 3.0 | 0.716 |
| PEEP (cm H2O) | 12.7 ± 3.2 | 12.0 ± 3.5 | 0.299 | 10.7 ± 2.7 | 10.7 ± 2.5 | 0.989 |
| Peak inspiratory pressure (cm H2O) | 30.8 ± 5.1 | 32.4 ± 6.5 | 0.148 | 29.4 ± 5.4 | 33.7 ± 3.8 | 0.011 |
| Mean airway pressure (cm H2O) | 17.7 ± 3.8 | 18.1 ± 4.7 | 0.587 | 16.1 ± 2.4 | 17.5 ± 3.1 | 0.173 |
| Dynamic compliance (mL/cm H2O) | 21.1 ± 7.6 | 18.3 ± 7.6 | 0.055 | 21.2 ± 8.8 | 13.6 ± 7.2 | 0.015 |
| Minute ventilation (L/min) | 5.3 ± 2.1 | 5.9 ± 3.1 | 0.224 | 4.9 ± 1.9 | 6.4 ± 3.5 | 0.116 |
| Fluid balance, ml | ||||||
| Before ECMO | 991 (−262 to 2278) | 795 (−167 to 1723) | 0.983 | 1641 (−753 to 2951) | 951 (−486 to 1880) | 0.535 |
| Cumulative 3 days | −29 (−1831 to 2108) | 2051(−441 to 4534) | 0.001 | 1971 (−708 to 3828) | 1803 (77–7267) | 0.238 |
| Inotropes (n) | 43 (72.9%) | 59 (100%) | <0.001 | 10 (83.3%) | 21 (95.5%) | 0.279 |
| Variables | Direct ARDS (n = 118) | Indirect ARDS (n = 34) | ||
|---|---|---|---|---|
| Adjust HR (95% CI) | p | Adjust HR (95% CI) | p | |
| Diabetes mellitus | 0.246 (0.111–0.546) | 0.001 | ||
| Immunocompromised status | 3.860 (1.943–7.668) | <0.001 | ||
| ARDS duration before ECMO (h) | 1.002 (1.000–1.004) | 0.015 | ||
| SOFA score from day 1 to day 3 on ECMO | 1.225 (1.070–1.402) | 0.003 | 2.514 (1.474–4.286) | 0.001 |
| Dynamic compliance from day 1 to day 3 on ECMO | 0.886 (0.802–0.978) | 0.017 | ||
| Variables | All | Direct ARDS | Indirect ARDS | p |
|---|---|---|---|---|
| (n = 128) | (n = 104) | (n = 24) | ||
| Age (years) | 51.2 ± 16.5 | 51.1 ± 16.6 | 51.3 ± 16.5 | 0.975 |
| Gender (male) | 89 (69.5%) | 72 (69.2%) | 17 (70.8%) | 0.878 |
| Body mass index (kg/m2) | 25.8 ± 5.5 | 25.9 ± 5.6 | 25.4 ± 4.7 | 0.708 |
| Diabetes mellitus | 38 (29.7%) | 31 (29.8%) | 7 (29.2%) | 0.951 |
| Chronic liver disease | 20 (15.6%) | 16 (15.4%) | 4 (16.7%) | 1.000 |
| Immunocompromised status | 34 (26.6%) | 25 (24%) | 9 (37.5%) | 0.178 |
| Chronic kidney disease | 16 (12.5%) | 12 (11.5%) | 4 (16.7%) | 0.500 |
| SOFA score before ECMO | 10.7 ± 3.1 | 10.5 ± 3.1 | 11.7 ± 2.8 | 0.091 |
| Lung injury score before ECMO | 3.4 ± 0.4 | 3.4 ± 0.4 | 3.2 ± 0.4 | 0.041 |
| ARDS duration before ECMO (h) | 29 (8–133) | 29 (8–122) | 30 (8–339) | 0.143 |
| pH before ECMO | 7.28 ± 0.14 | 7.29 ± 0.14 | 7.24 ± 0.13 | 0.186 |
| PaCO2 (mm Hg) before ECMO | 52.8 ± 19.5 | 52.7 ± 19.3 | 53.5 ± 20.6 | 0.851 |
| PaO2/FiO2 (mm Hg) before ECMO | 63 (52–93) | 63 (52–86) | 65 (54–107) | 0.216 |
| Ventilator settings before ECMO | ||||
| Mechanical power (J/min) | 24.1 ± 9.8 | 24.7 ± 9.7 | 21.5 ± 9.8 | 0.152 |
| Tidal volume (mL/kg PBW) | 7.7 ± 2.3 | 7.7 ± 2.3 | 7.8 ± 2.2 | 0.948 |
| PEEP (cm H2O) | 12.2 ± 2.7 | 12.3 ± 2.7 | 11.5 ± 2.5 | 0.180 |
| Peak inspiratory pressure (cm H2O) | 33.9 ± 6.5 | 34.0 ± 6.2 | 33.6 ± 7.5 | 0.772 |
| Mean airway pressure (cm H2O) | 18.6 ± 4.4 | 18.8 ± 4.4 | 17.8 ± 4.7 | 0.331 |
| Dynamic compliance (mL/cm H2O) | 22.8 ± 11.3 | 22.7 ± 11.0 | 23.1 ± 13.1 | 0.874 |
| Minute ventilation (L/min) | 10.7 ± 3.9 | 11.0 ± 4.1 | 9.4 ± 3.1 | 0.089 |
| Ventilatory ratio | 2.5 ± 1.0 | 2.5 ± 1.0 | 2.3 ± 1.2 | 0.426 |
| SOFA score from day 1 to day 3 on ECMO | 9.7 ± 2.2 | 9.5 ± 2.1 | 11.0 ± 2.1 | 0.005 |
| pH from day1 to day 3 on ECMO | 7.44 ± 0.07 | 7.44 ± 0.07 | 7.41 ± 0.08 | 0.083 |
| PaCO2 (mm Hg) from day1 to day 3 on ECMO | 38.1 ± 5.0 | 38.0 ± 4.9 | 38.6 ± 5.4 | 0.576 |
| PaO2/FiO2 (mm Hg) from day 1 to day 3 on ECMO | 178 (134–216) | 167 (131–214) | 194 (156–240) | 0.763 |
| Ventilator settings from day 1 to day 3 on ECMO | ||||
| Mechanical power (J/min) | 11.7 ± 6.1 | 11.5 ± 6.0 | 12.2 ± 6.2 | 0.638 |
| Tidal volume (mL/kg PBW) | 5.9 ± 2.0 | 5.9 ± 2.1 | 5.6 ± 1.8 | 0.537 |
| PEEP (cm H2O) | 12.3 ± 3.3 | 12.6 ± 3.4 | 10.8 ± 2.5 | 0.017 |
| Peak inspiratory pressure (cm H2O) | 31.3 ± 5.3 | 31.2 ± 5.3 | 32.0 ± 5.2 | 0.467 |
| Mean airway pressure (cm H2O) | 17.7 ± 3.9 | 17.9 ± 4.2 | 17.2 ± 2.7 | 0.325 |
| Dynamic compliance (mL/cm H2O) | 19.3 ± 7.9 | 19.7 ± 7.6 | 17.6 ± 9.3 | 0.269 |
| Minute ventilation (L/min) | 5.5 ± 2.8 | 5.4 ± 2.7 | 5.8 ± 2.9 | 0.556 |
| Fluid balance, ml | ||||
| Before ECMO | 938 (−130 to 2125) | 938 (−78 to 2204) | 957 (−717 to 2002) | 0.731 |
| Cumulative 3 days | 1190 (−873 to 3846) | 801 (−1378 to 3275) | 2097 (1100 to 6976) | 0.029 |
| Inotropes (n) | 111 (89.5%) | 89 (85.6%) | 22 (91.7%) | 0.738 |
| 28 day hospital mortality, n (%) | 48 (37.5%) | 34 (32.7%) | 14 (58.3%) | 0.009 |
| 60 day hospital mortality, n (%) | 57 (44.5%) | 42 (40.4%) | 15 (62.5%) | 0.019 |
| 90 day hospital mortality, n (%) | 59 (46.1%) | 44 (42.3%) | 15 (62.5%) | 0.027 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiu, L.-C.; Chuang, L.-P.; Lin, S.-W.; Li, H.-H.; Leu, S.-W.; Chang, K.-W.; Huang, C.-H.; Chiu, T.-H.; Wu, H.-P.; Tsai, F.-C.; et al. Comparisons of Outcomes between Patients with Direct and Indirect Acute Respiratory Distress Syndrome Receiving Extracorporeal Membrane Oxygenation. Membranes 2021, 11, 644. https://doi.org/10.3390/membranes11080644
Chiu L-C, Chuang L-P, Lin S-W, Li H-H, Leu S-W, Chang K-W, Huang C-H, Chiu T-H, Wu H-P, Tsai F-C, et al. Comparisons of Outcomes between Patients with Direct and Indirect Acute Respiratory Distress Syndrome Receiving Extracorporeal Membrane Oxygenation. Membranes. 2021; 11(8):644. https://doi.org/10.3390/membranes11080644
Chicago/Turabian StyleChiu, Li-Chung, Li-Pang Chuang, Shih-Wei Lin, Hsin-Hsien Li, Shaw-Woei Leu, Ko-Wei Chang, Chi-Hsien Huang, Tzu-Hsuan Chiu, Huang-Pin Wu, Feng-Chun Tsai, and et al. 2021. "Comparisons of Outcomes between Patients with Direct and Indirect Acute Respiratory Distress Syndrome Receiving Extracorporeal Membrane Oxygenation" Membranes 11, no. 8: 644. https://doi.org/10.3390/membranes11080644
APA StyleChiu, L.-C., Chuang, L.-P., Lin, S.-W., Li, H.-H., Leu, S.-W., Chang, K.-W., Huang, C.-H., Chiu, T.-H., Wu, H.-P., Tsai, F.-C., Huang, C.-C., Hu, H.-C., & Kao, K.-C. (2021). Comparisons of Outcomes between Patients with Direct and Indirect Acute Respiratory Distress Syndrome Receiving Extracorporeal Membrane Oxygenation. Membranes, 11(8), 644. https://doi.org/10.3390/membranes11080644






