J. Clin. Med. 2022, 11(8), 2164; https://doi.org/10.3390/jcm11082164 - 13 Apr 2022
Cited by 24 | Viewed by 8703
Abstract
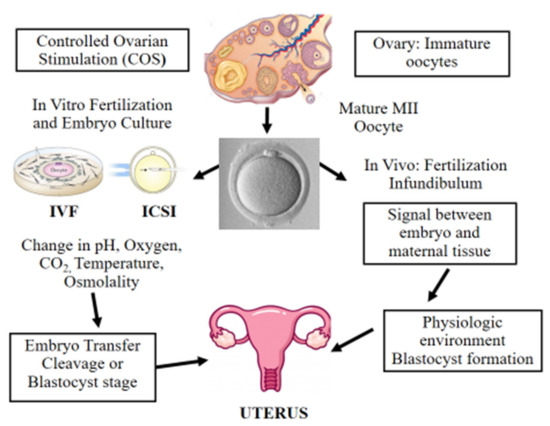
Diagnosis of antiphospholipid syndrome (APS) requires the presence of a clinical criterion (thrombosis and/or pregnancy morbidity), combined with persistently circulating antiphospholipid antibodies (aPL). Currently, laboratory criteria aPL consist of lupus anticoagulant (LAC), anticardiolipin antibodies (aCL) IgG/IgM, and anti-β2 glycoprotein I antibodies (aβ2GPI) IgG/IgM.
[...] Read more.
Diagnosis of antiphospholipid syndrome (APS) requires the presence of a clinical criterion (thrombosis and/or pregnancy morbidity), combined with persistently circulating antiphospholipid antibodies (aPL). Currently, laboratory criteria aPL consist of lupus anticoagulant (LAC), anticardiolipin antibodies (aCL) IgG/IgM, and anti-β2 glycoprotein I antibodies (aβ2GPI) IgG/IgM. Diagnosis and risk stratification of APS are complex and efforts to standardize and optimize laboratory tests have been ongoing since the initial description of the syndrome. LAC detection is based on functional coagulation assays, while aCL and aβ2GPI are measured with immunological solid-phase assays. LAC assays are especially prone to interference by anticoagulation therapy, but strategies to circumvent this interference are promising. Alternative techniques such as thrombin generation for LAC detection and to estimate LAC pathogenicity have been suggested, but are not applicable yet in routine setting. For aCL and aβ2GPI, a lot of different assays and detection techniques such as enzyme-linked immunosorbent and chemiluminescent assays are available. Furthermore, a lack of universal calibrators or standards results in high variability between the different solid-phase assays. Other non-criteria aPL such as anti-domain I β2 glycoprotein I and antiphosphatidylserine/prothrombin antibodies have been suggested for risk stratification purposes in APS, while their added value to diagnostic criteria seems limited. In this review, we will describe laboratory assays for diagnostic and risk evaluation in APS, integrating applicable guidelines and classification criteria. Current insights and hindrances are addressed with respect to both laboratory and clinical implications.
Full article
(This article belongs to the Special Issue Management, Diagnosis and Pathophysiology of Antiphospholipid Syndrome: Current Updates and Future Approaches)
►
Show Figures