Role of a Chest X-ray Severity Score in a Multivariable Predictive Model for Mortality in Patients with COVID-19: A Single-Center, Retrospective Study
Abstract
:1. Introduction
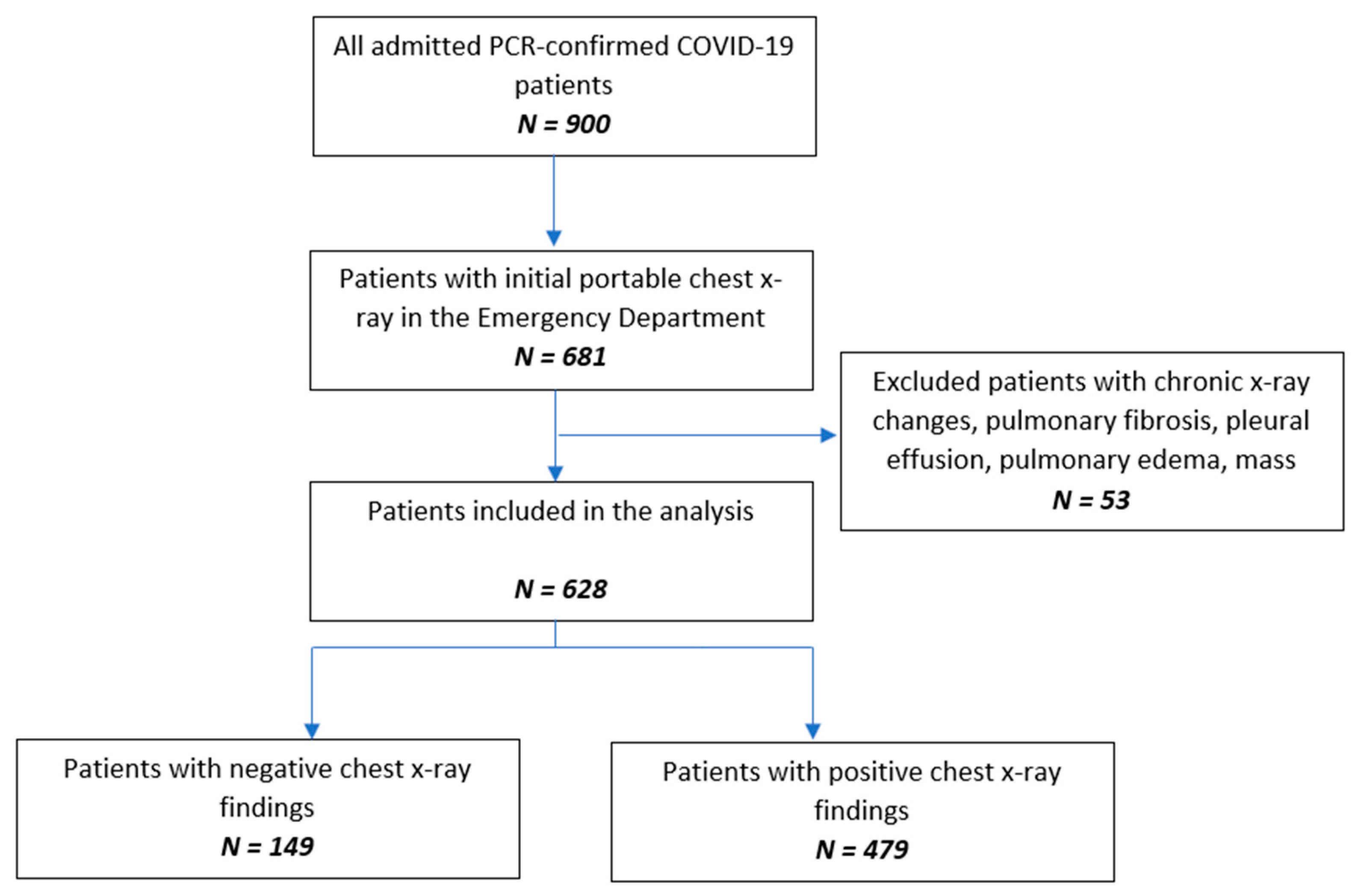
2. Materials and Methods
2.1. Study Design and Sample Population
2.2. Data Collection
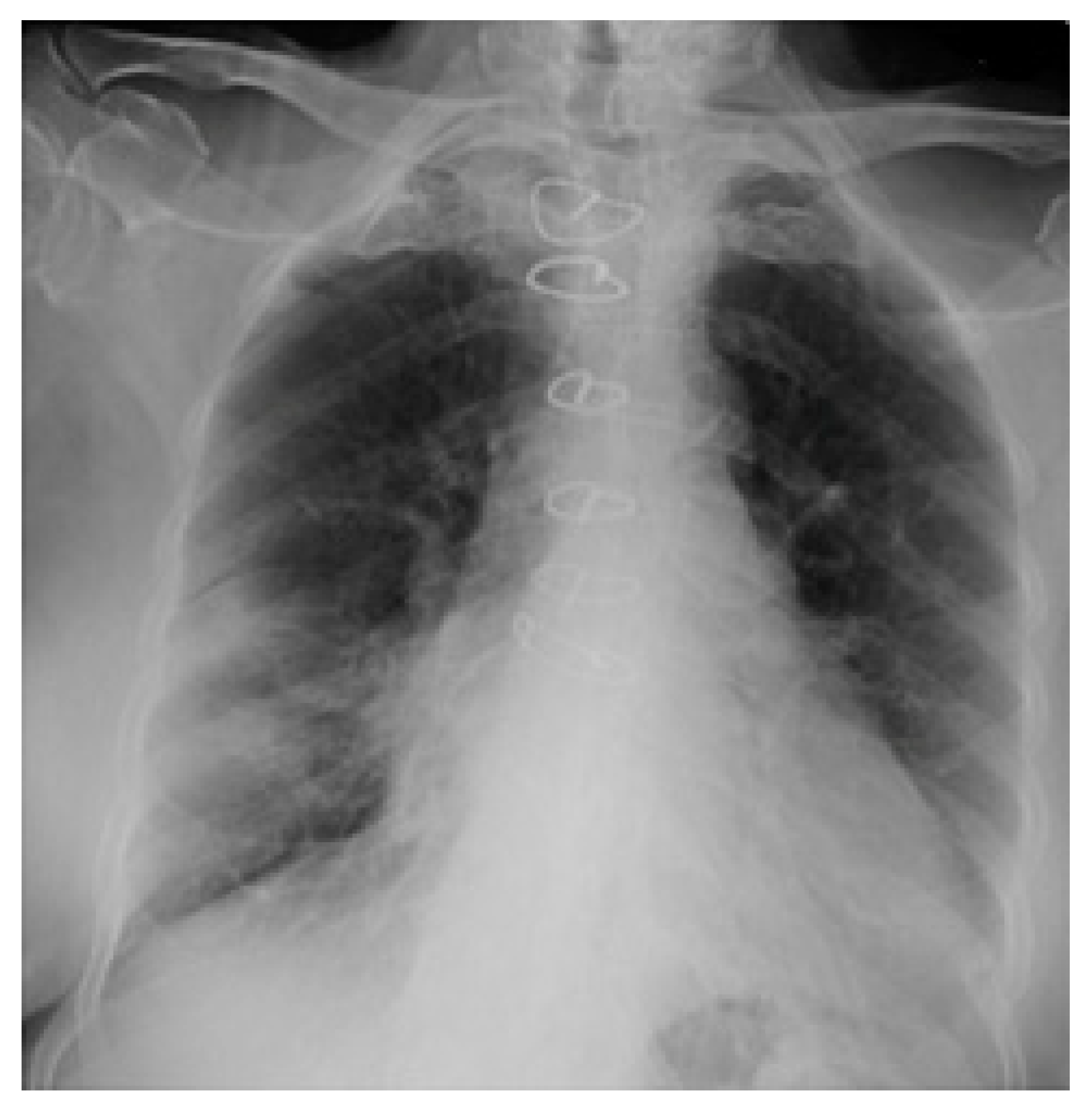
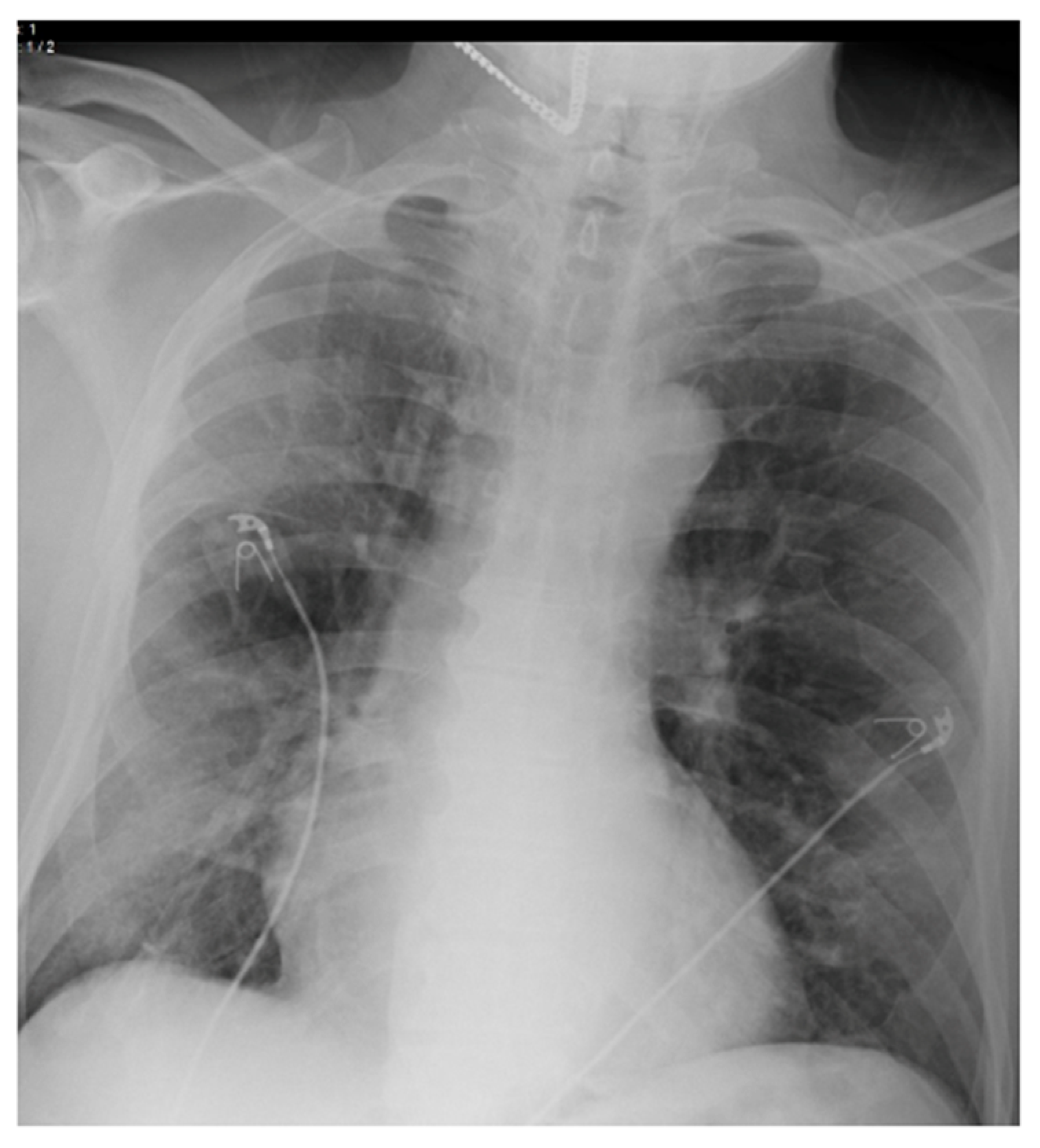
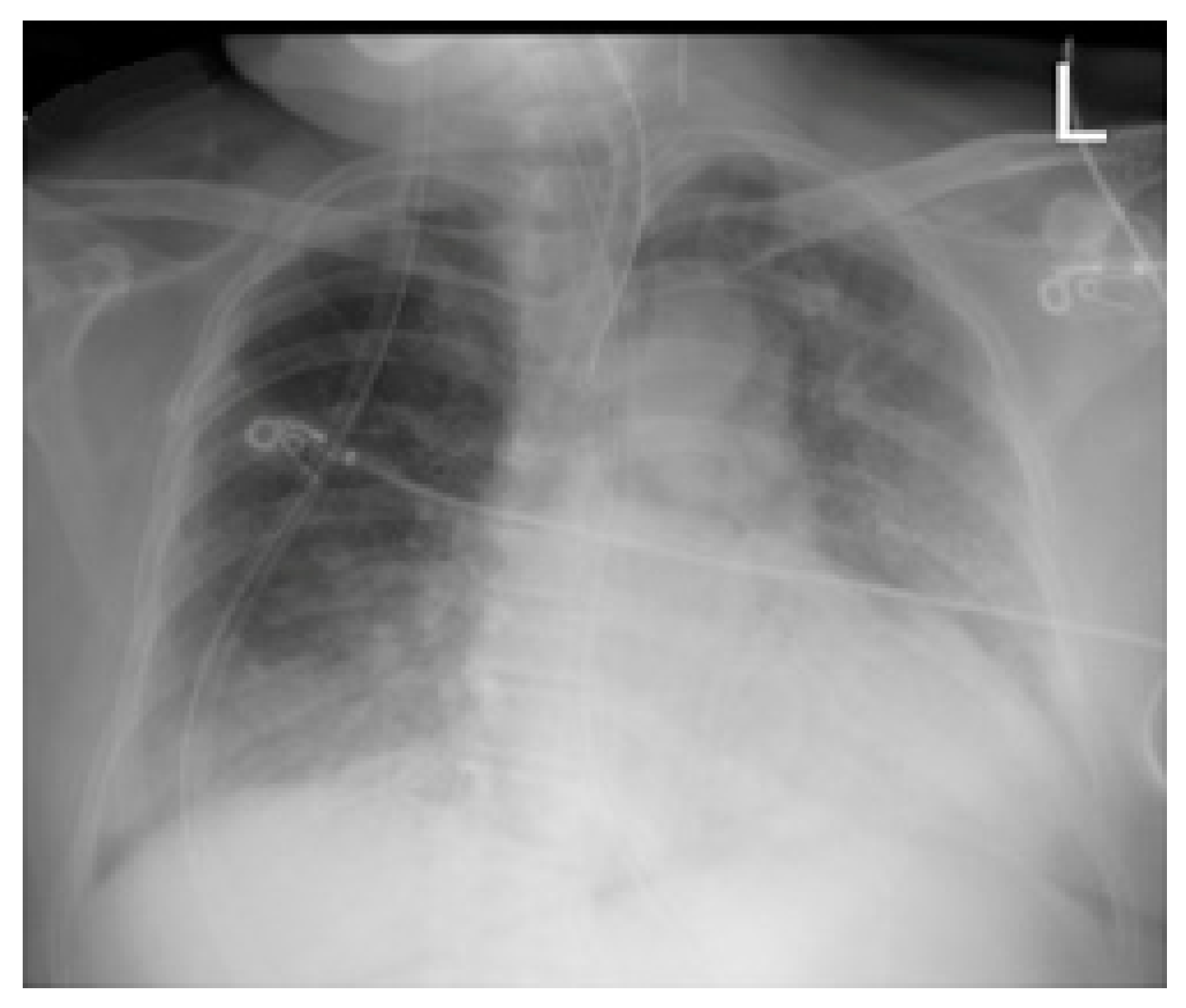
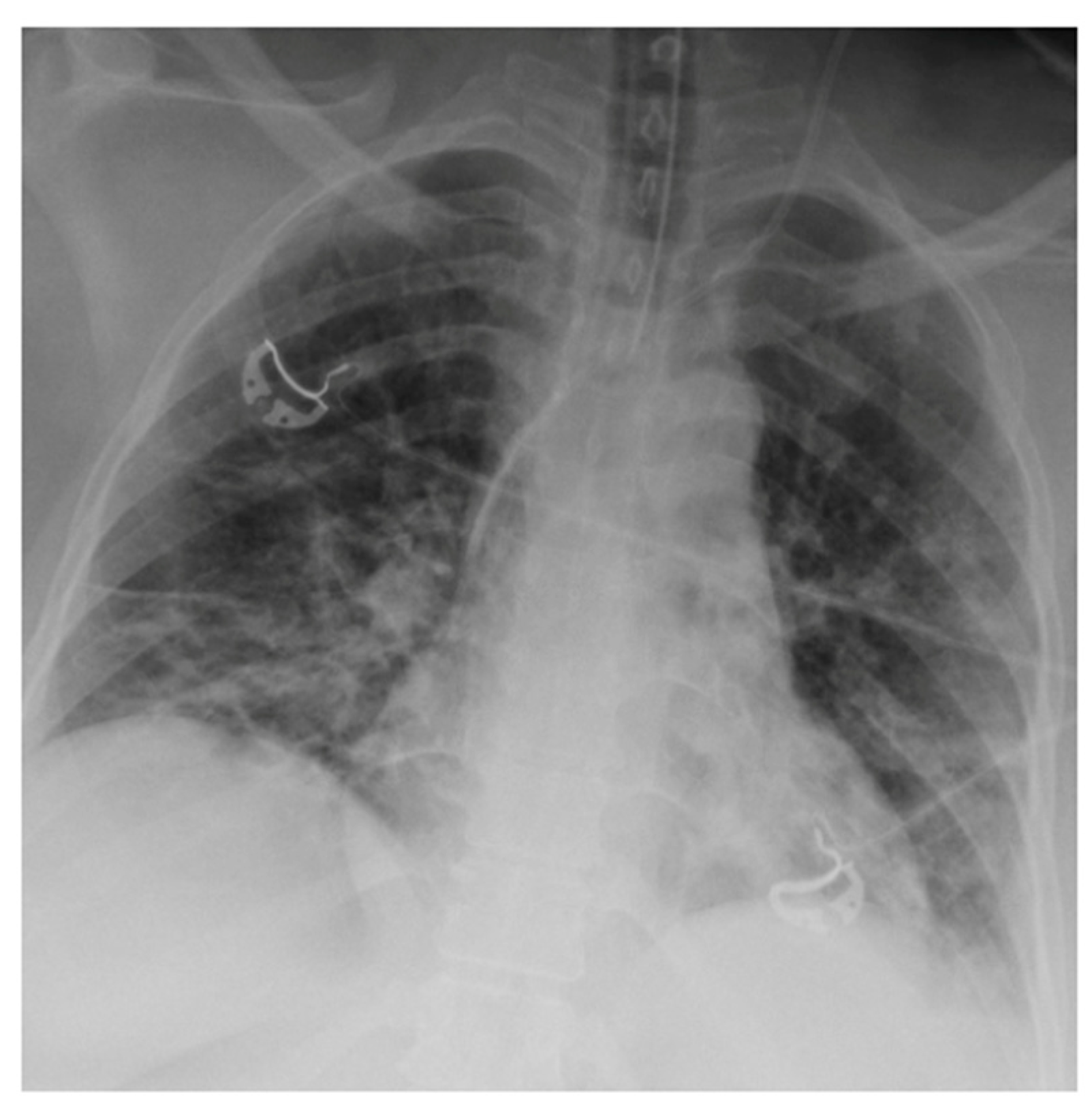
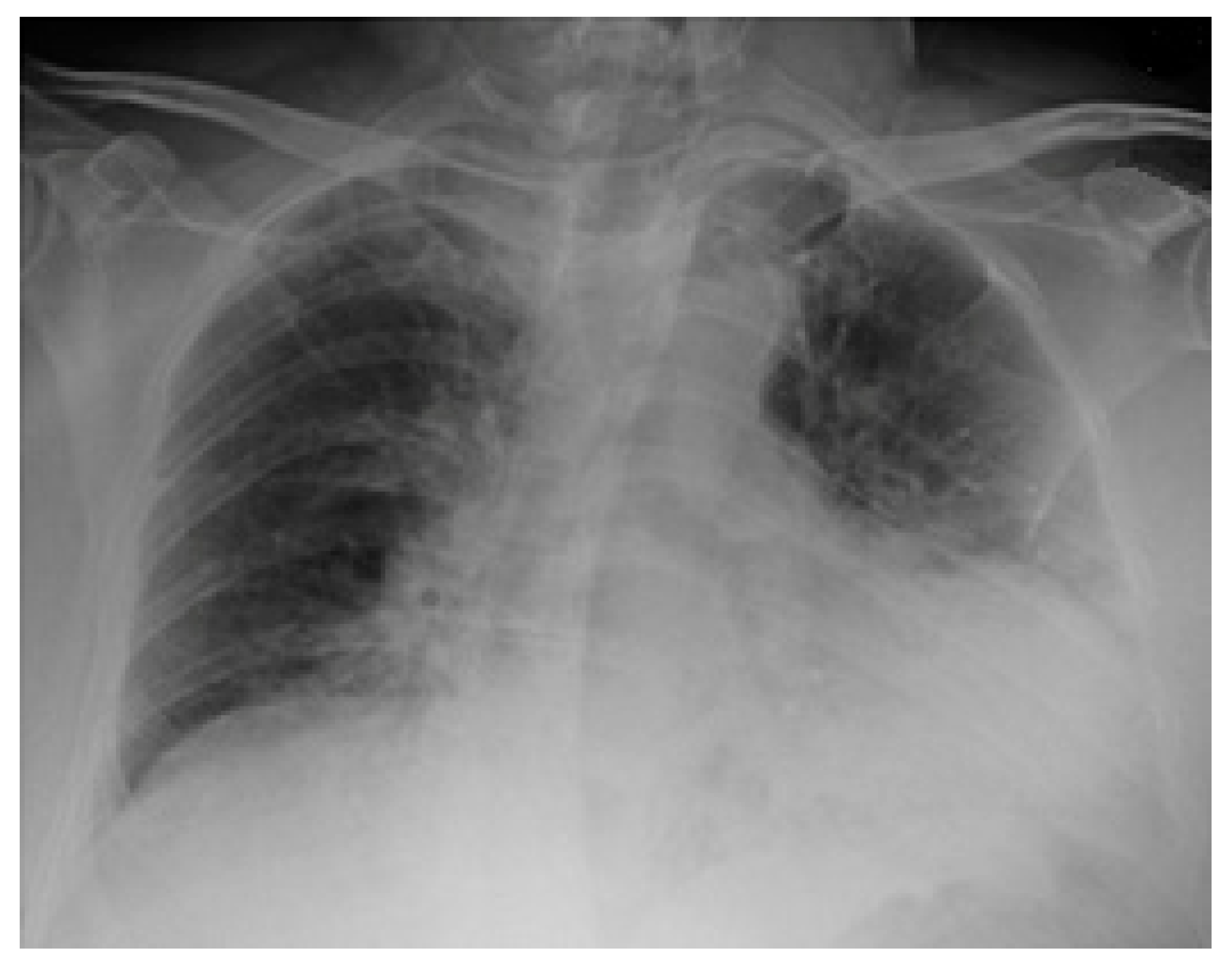
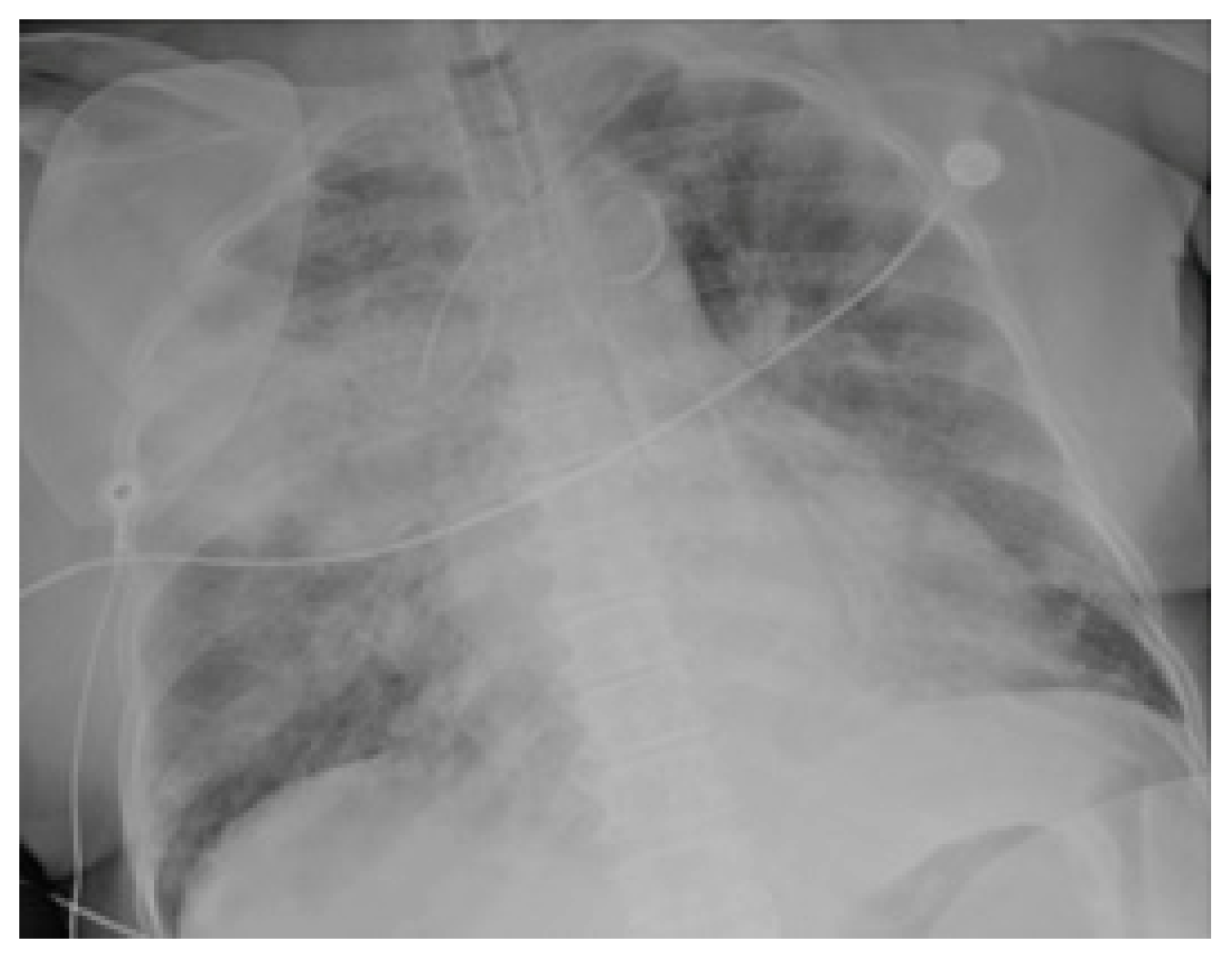
2.3. Imaging and Analysis
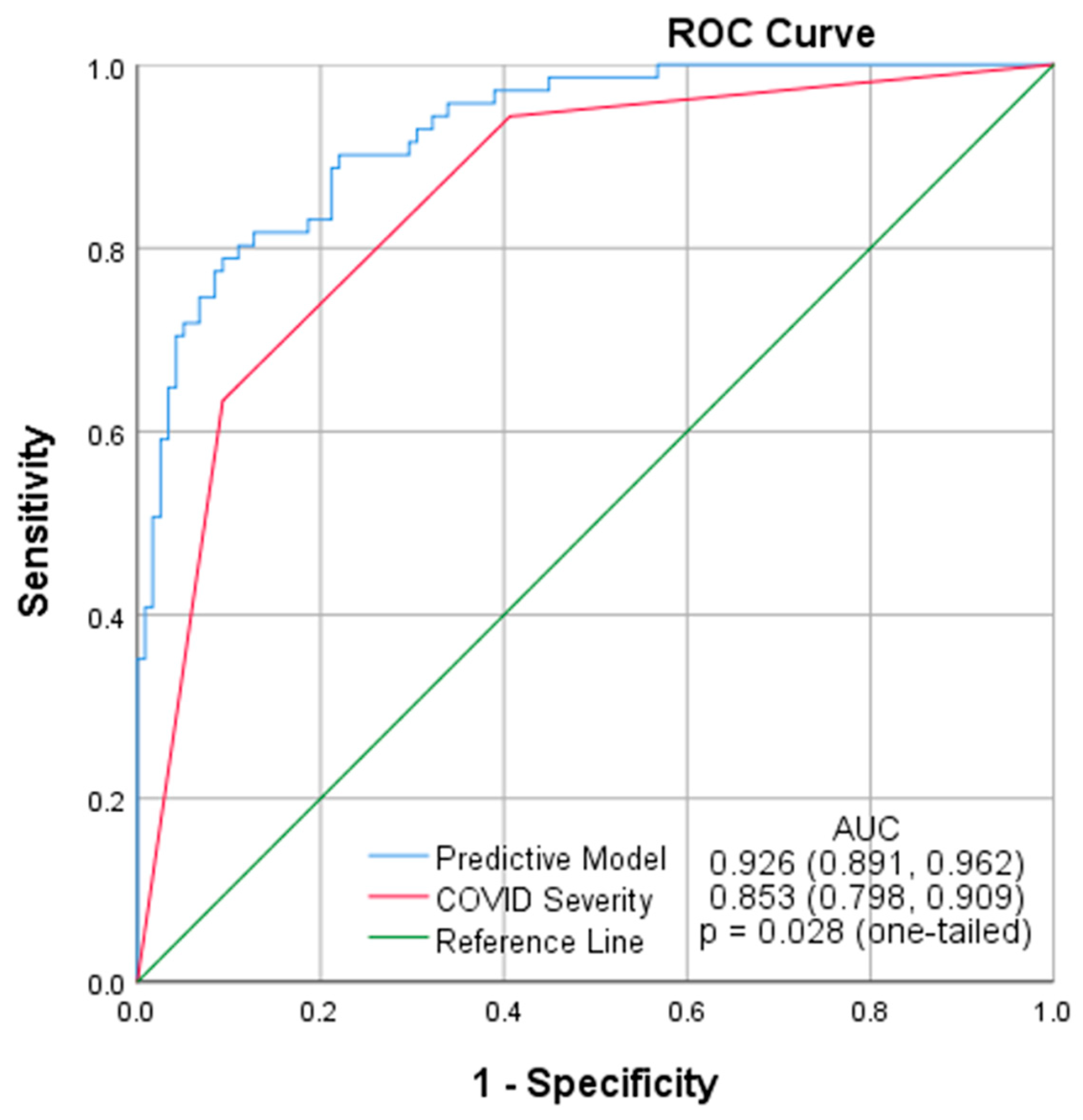
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pascarella, G.; Strumia, A.; Piliego, C.; Bruno, F.; Del Buono, R.; Costa, F.; Scarlata, S.; Agrò, F.E. COVID-19 diagnosis and management: A comprehensive review. J. Intern. Med. 2020, 288, 192–206. [Google Scholar] [CrossRef] [PubMed]
- Kanne, J.P.; Bai, H.; Bernheim, A.; Chung, M.; Haramati, L.B.; Kallmes, D.F.; Little, B.P.; Rubin, G.D.; Sverzellati, N. COVID-19 Imaging: What We Know Now and What Remains Unknown. Radiology 2021, 299, E262–E279. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.; Bernheim, A.; Mei, X.; Zhang, N.; Huang, M.; Zeng, X.; Cui, J.; Xu, W.; Yang, Y.; Fayad, Z.A.; et al. CT imaging features of 2019 novel coronavirus (2019–nCoV). Radiology 2020, 295, 202–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cellina, M.; Orsi, M.; Pittino, C.V.; Toluian, T.; Oliva, G. Chest computed tomography findings of COVID-19 pneumonia: Pictorial essay with literature review. Jpn. J. Radiol. 2020, 38, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Zhang, Y.; Wang, Y.; Huang, Z.; Song, B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): A pictorial review. Eur. Radiol. 2020, 30, 4381–4389. [Google Scholar] [CrossRef] [Green Version]
- Cleverley, J.; Piper, J.; Jones, M.M. The role of chest radiography in confirming COVID-19 pneumonia. BMJ 2020, 370, m2426. [Google Scholar] [CrossRef]
- Wong, H.Y.F.; Lam, H.Y.S.; Fong, A.H.-T.; Leung, S.T.; Chin, T.W.-Y.; Lo, C.S.Y.; Lui, M.M.-S.; Lee, J.C.Y.; Chiu, K.W.-H.; Chung, T.W.-H.; et al. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology 2020, 296, E72–E78. [Google Scholar] [CrossRef] [Green Version]
- Lei, Y.; Zhang, H.; Yu, J.; Patlas, M.N. COVID-19 Infection: Early Lessons. Can. Assoc. Radiol. J. 2020, 71, 251–252. [Google Scholar] [CrossRef] [Green Version]
- Simpson, S.; Kay, F.U.; Abbara, S.; Bhalla, S.; Chung, J.H.; Chung, M.; Henry, T.S.; Kanne, J.P.; Kligerman, S.; Ko, J.P.; et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA—Secondary Publication. J. Thorac. Imaging 2020, 35, 219–227. [Google Scholar] [CrossRef]
- Rubin, G.D.; Ryerson, C.J.; Haramati, L.B.; Sverzellati, N.; Kanne, J.; Raoof, S.; Schluger, N.W.; Volpi, A.; Yim, J.-J.; Martin, I.B.K.; et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology 2020, 296, 172–180. [Google Scholar] [CrossRef] [Green Version]
- American College of Radiology. ACR Recommendations for the Use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection; American College of Radiology: Reston, VA, USA, 2020. [Google Scholar]
- Bedair, E.M.; Soliman, A.; De Sanctis, V.; Nair, A.P.; Al Masalamani, M.A.; Abdulmajeed, H.A.K.; Yassin, M.A. Proposed Scoring System for Evaluating Clinico-radiological Severity of COVID- 19 using Plain Chest X-ray (CXR) changes (CO X-RADS): Preliminary results. Acta Bio Med. Atenei Parm. 2020, 91, e2020172. [Google Scholar]
- Li, Y.; Yang, Z.; Ai, T.; Wu, S.; Xia, L. Association of “initial CT” findings with mortality in older patients with coronavirus disease 2019 (COVID-19). Eur. Radiol. 2020, 30, 6186–6193. [Google Scholar] [CrossRef] [PubMed]
- Orsi, M.A.; Oliva, G.; Toluian, T.; Pittino, C.V.; Panzeri, M.; Cellina, M. Feasibility, Reproducibility, and Clinical Validity of a Quantitative Chest X-ray Assessment for COVID-19. Am. J. Trop. Med. Hyg. 2020, 103, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Toussie, D.; Voutsinas, N.; Finkelstein, M.; Cedillo, M.A.; Manna, S.; Maron, S.Z.; Jacobi, A.; Chung, M.; Bernheim, A.; Eber, C.; et al. Clinical and Chest Radiography Features Determine Patient Outcomes in Young and Middle Age Adults with COVID-19. Radiology 2020, 297, E197–E206. [Google Scholar] [CrossRef] [PubMed]
- Borghesi, A.; Maroldi, R. COVID-19 outbreak in Italy: Experimental chest X-ray scoring system for quantifying and monitoring disease progression. La Radiol. Med. 2020, 125, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Cozzi, D.; Albanesi, M.; Cavigli, E.; Moroni, C.; Bindi, A.; Luvarà, S.; Lucarini, S.; Busoni, S.; Mazzoni, L.N.; Miele, V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: Findings and correlation with clinical outcome. La Radiol. Med. 2020, 125, 730–737. [Google Scholar] [CrossRef]
- Miller, D.; Sarwal, A.; Yu, B.; Gomez, E.; Perez-Gutierrez, V.; Gossai, M.; Valdez, E.; Mendez, A.; Chaudry, S.; Venugopal, U.; et al. Impact of Residential Neighborhood and Race/Ethnicity on Outcomes of Hospitalized Patients with COVID-19 in the Bronx. medRxiv 2021. [Google Scholar] [CrossRef]
- Koch, C.; Edinger, F.; Fischer, T.; Brenck, F.; Hecker, A.; Katzer, C.; Markmann, M.; Sander, M.; Schneck, E. Comparison of qSOFA score, SOFA score, and SIRS criteria for the prediction of infection and mortality among surgical intermediate and intensive care patients. World J. Emerg. Surg. 2020, 15, 63. [Google Scholar] [CrossRef]
- Hanley, J.A.; McNeil, B.J. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983, 148, 839–843. [Google Scholar] [CrossRef] [Green Version]
- Borghesi, A.; Zigliani, A.; Golemi, S.; Carapella, N.; Maculotti, P.; Farina, D.; Maroldi, R. Chest X-ray severity index as a predictor of in-hospital mortality in coronavirus disease 2019: A study of 302 patients from Italy. Int. J. Infect. Dis. 2020, 96, 291–293. [Google Scholar] [CrossRef]
- Garrafa, E.; Vezzoli, M.; Ravanelli, M.; Farina, D.; Borghesi, A.; Calza, S.; Maroldi, R. Early prediction of in-hospital death of COVID-19 patients: A machine-learning model based on age, blood analyses, and chest X-ray score. eLife 2021, 10, e70640. [Google Scholar] [CrossRef] [PubMed]
- Warren, M.A.; Zhao, Z.; Koyama, T.; Bastarache, J.A.; Shaver, C.M.; Semler, M.W.; Rice, T.W.; Matthay, M.A.; Calfee, C.S.; Ware, L.B. Severity scoring of lung oedema on the chest radiograph is associated with clinical outcomes in ARDS. Thorax 2018, 73, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Homayounieh, F.; Zhang, E.W.; Babaei, R.; Mobin, H.K.; Sharifian, M.; Mohseni, I.; Kuo, A.; Arru, C.; Kalra, M.K.; Digumarthy, S.R. Clinical and imaging features predict mortality in COVID-19 infection in Iran. PLoS ONE 2020, 15, e0239519. [Google Scholar] [CrossRef] [PubMed]
- Joseph, N.; Reid, N.J.; Som, A.; Li, M.D.; Hyle, E.P.; Dugdale, C.M.; Lang, M.; Betancourt, J.R.; Deng, F.; Mendoza, D.P.; et al. Racial and Ethnic Disparities in Disease Severity on Admission Chest Radiographs among Patients Admitted with Confirmed Coronavirus Disease 2019: A Retrospective Cohort Study. Radiology 2020, 297, E303–E312. [Google Scholar] [CrossRef]
- Balbi, M.; Caroli, A.; Corsi, A.; Milanese, G.; Surace, A.; Di Marco, F.; Novelli, L.; Silva, M.; Lorini, F.L.; Duca, A.; et al. Chest X-ray for predicting mortality and the need for ventilatory support in COVID-19 patients presenting to the emergency department. Eur. Radiol. 2021, 31, 1999–2012. [Google Scholar] [CrossRef]
- Schalekamp, S.; Huisman, M.; Van Dijk, R.A.; Boomsma, M.F.; Jorge, P.J.F.; De Boer, W.S.; Herder, G.J.M.; Bonarius, M.; Groot, O.A.; Jong, E.; et al. Model-based Prediction of Critical Illness in Hospitalized Patients with COVID-19. Radiology 2021, 298, E46–E54. [Google Scholar] [CrossRef]
- Altschul, D.J.; Unda, S.R.; Benton, J.; de la Garza Ramos, R.; Cezayirli, P.; Mehler, M.; Eskandar, E.N. A novel severity score to predict inpatient mortality in COVID-19 patients. Sci. Rep. 2020, 10, 16726. [Google Scholar] [CrossRef]
- Webb, B.J.; Levin, N.M.; Grisel, N.; Brown, S.M.; Peltan, I.D.; Spivak, E.S.; Shah, M.; Stenehjem, E.; Bledsoe, J. Simple scoring tool to estimate risk of hospitalization and mortality in ambulatory and emergency department patients with COVID-19. PLoS ONE 2022, 17, e0261508. [Google Scholar] [CrossRef]
- Shang, Y.; Liu, T.; Wei, Y.; Li, J.; Shao, L.; Liu, M.; Zhang, Y.; Zhao, Z.; Xu, H.; Peng, Z.; et al. Scoring systems for predicting mortality for severe patients with COVID-19. eClinicalMedicine 2020, 24, 100426. [Google Scholar] [CrossRef]
- Vaid, A.; Somani, S.; Russak, A.J.; De Freitas, J.K.; Chaudhry, F.F.; Paranjpe, I.; Johnson, K.W.; Lee, S.J.; Miotto, R.; Richter, F.; et al. Machine Learning to Predict Mortality and Critical Events in COVID-19 Positive New York City Patients: A Cohort Study. J. Med. Internet Res. 2020, 22, e24018. [Google Scholar] [CrossRef]
- Booth, A.L.; Abels, E.; McCaffrey, P. Development of a prognostic model for mortality in COVID-19 infection using machine learning. Mod. Pathol. 2020, 34, 522–531. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total (N = 628) | Status at Discharge | ||
|---|---|---|---|---|
| Alive (N = 402) | Expired (N = 226) | |||
| Age * | 59.6 (16.0) | 55.4 (15.7) | 67.1 (13.9) | |
| Gender | Female | 263 (41.9%) | 174 (43.3%) | 89 (39.4%) |
| Male | 365 (58.1%) | 228 (56.7%) | 137 (60.6%) | |
| Race | Hispanic | 409 (65.1%) | 252 (62.7%) | 157 (69.5%) |
| African American | 165 (26.3%) | 112 (27.9%) | 53 (23.5%) | |
| White | 21 (3.3%) | 16 (4.0%) | 5 (2.2%) | |
| Asian | 13 (2.1%) | 9 (2.2%) | 4 (1.8%) | |
| Other | 20 (3.2%) | 13 (3.2%) | 7 (3.1%) | |
| Smoking | 37 (6.0%) | 27 (6.8%) | 10 (4.6%) | |
| BMI | Underweight | 7 (1.2%) | 3 (0.8%) | 4 (1.9%) |
| Normal | 95 (16.3%) | 62 (16.7%) | 33 (15.7%) | |
| Overweight | 187 (32.1%) | 126 (33.9%) | 61 (29.0%) | |
| Obese | 293 (50.3%) | 181 (48.7%) | 112 (53.3%) | |
| Past Medical History | ||||
| Asthma/COPD | 112 (17.8%) | 67 (16.7%) | 45 (19.9%) | |
| Hypertension | 280 (44.6) | 182 (45.3%) | 98 (43.4%) | |
| CHF | 47 (7.5%) | 23 (5.7%) | 24 (10.6%) | |
| CKD | 76 (12.1%) | 40 (10.0%) | 36 (15.9%) | |
| DM | 269 (42.8%) | 152 (37.8%) | 117 (51.8%) | |
| Rheumatological Diseases | 22 (3.5%) | 10 (2.5%) | 12 (5.3%) | |
| Cirrhosis | 7 (1.1%) | 6 (1.5%) | 1 (0.4%) | |
| Transplant | 4 (0.6%) | 2 (0.5%) | 2 (0.9%) | |
| Immunosuppression | 14 (2.2%) | 8 (2.0%) | 6 (2.7%) | |
| HIV | 16 (2.5%) | 11 (2.7%) | 5 (2.2%) | |
| Cancer | 39 (6.2%) | 15 (3.7%) | 24 (10.6%) | |
| Symptoms | ||||
| Fever | 408 (65.0%) | 275 (68.4%) | 133 (58.8%) | |
| Cough | 447 (71.2%) | 302 (75.1%) | 145 (64.2%) | |
| Shortness of Breath | 435 (69.3%) | 254 (63.2%) | 181 (80.1%) | |
| Gastrointestinal Symptoms | 141 (22.5%) | 110 (27.4%) | 31 (13.7%) | |
| Altered Mental Status/Seizures | 80 (12.7%) | 32 (8.0%) | 48 (21.2%) | |
| Days from Onset of Symptoms ** | 4.0 (2.0, 7.0) | 5.0 (3.0, 7.0) | 4.0 (2.0, 7.0) | |
| Sepsis Syndrome | 189 (30.1%) | 53 (13.2%) | 136 (60.2%) | |
| S/F ratio ** | 303.1 (102.1, 447.6) | 342.9 (263.9, 457.1) | 102.2 (97.0, 266.7) | |
| COVID Severity | Moderate | 259 (41.2%) | 247 (61.4%) | 12 (5.3%) |
| Severe | 178 (28.3%) | 112 (27.9%) | 66 (29.2%) | |
| Critical | 191 (30.4%) | 43 (10.7%) | 148 (65.5%) | |
| Length of Stay ** | 6.0 (3.0, 11.0) | 5.0 (2.0, 10.0) | 7.0 (4.0, 11.0) | |
| Mechanical Ventilation on Admission | 134 (21.3%) | 28 (7.0%) | 106 (46.9%) | |
| Mechanical Ventilation | 251 (40.0%) | 67 (16.7%) | 184 (81.4%) | |
| Days to Intubation ** | 0.0 (0.0, 3.0) | 3.0 (0.0, 8.0) | 0.0 (0.0, 2.0) | |
| Duration of Mechanical Ventilation ** | 7.0 (4.0, 12.0) | 11.0 (4.0, 26.0) | 7.0 (4.0, 10.0) | |
| CXR Severity Score ** | 3.0 (1.0, 4.0) | 3.0 (0.0, 3.0) | 3.0 (3.0, 6.0) | |
| N (%) | |
|---|---|
| Radiology Findings | |
| No | 149 (23.7%) |
| Yes | 479 (76.3%) |
| Radiologic Characteristics | |
| Distribution | |
| Unilateral Unilobar | 64 (13.4%) |
| Unilateral Multilobar | 21 (4.4%) |
| Bilateral—not diffuse | 63 (13.2%) |
| Diffuse Bilateral | 331 (69.1%) |
| Opacity | |
| Hazy or Interstitial Opacities | 357 (74.5%) |
| Dense Opacities | 122 (25.5%) |
| Specific Patterns | |
| Diffuse-Bilateral with hazy opacities | 256 (53.4%) |
| Diffuse-Bilateral with dense opacities | 75 (15.7%) |
| Unilateral-Unilobar with Hazy opacities | 49 (10.2%) |
| Bilateral with predominance with hazy opacities | 37 (7.7%) |
| Bilateral with predominance with dense opacities | 26 (5.4%) |
| Unilateral-Multilobar with Hazy opacities | 15 (3.1%) |
| Unilateral-Unilobar with dense opacities | 15 (3.1%) |
| Unilateral-Multilobar with dense opacities | 6 (1.3%) |
| Variables | Adjusted OR (95% CI) | p-Value |
|---|---|---|
| Age | 1.063 (1.043, 1.083) | <0.001 |
| Gender | 1.433 (0.865, 2.374) | 0.162 |
| Smoking | 0.962 (0.330, 2.799) | 0.943 |
| Asthma/COPD | 1.045 (0.552, 1.977) | 0.893 |
| CHF | 0.864 (0.345, 2.165) | 0.755 |
| CKD | 0.886 (0.426, 1.842) | 0.745 |
| DM | 1.238 (0.757, 2.023) | 0.395 |
| Cancer | 1.579 (0.618, 4.037) | 0.340 |
| Days from Onset of Symptoms | 0.991 (0.936, 1.050) | 0.766 |
| Sepsis Syndrome | 7.353 (4.434, 12.194) | <0.001 |
| S/F ratio | 0.995 (0.993, 0.997) | <0.001 |
| Mechanical Ventilation on Admission | 5.389 (2.931, 9.908) | <0.001 |
| CXR Severity Score | 1.184 (1.054, 1.330) | 0.005 |
| Model | Coefficient | p-Value | Adjusted OR (95% CI) |
|---|---|---|---|
| Age | 0.052 | <0.001 | 1.053 (1.032, 1.074) |
| Sepsis Syndrome | 1.865 | <0.001 | 6.459 (3.667, 11.379) |
| S/F ratio | −0.005 | <0.001 | 0.995 (0.993, 0.997) |
| Mechanical Ventilation on Admission | 1.606 | <0.001 | 4.981 (2.519, 9.850) |
| CXR Severity Score | 0.132 | 0.046 | 1.141 (1.003, 1.299) |
| Constant | −3.867 | <0.001 | 0.021 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baikpour, M.; Carlos, A.; Morasse, R.; Gissel, H.; Perez-Gutierrez, V.; Nino, J.; Amaya-Suarez, J.; Ali, F.; Toledano, T.; Arampulikan, J.; et al. Role of a Chest X-ray Severity Score in a Multivariable Predictive Model for Mortality in Patients with COVID-19: A Single-Center, Retrospective Study. J. Clin. Med. 2022, 11, 2157. https://doi.org/10.3390/jcm11082157
Baikpour M, Carlos A, Morasse R, Gissel H, Perez-Gutierrez V, Nino J, Amaya-Suarez J, Ali F, Toledano T, Arampulikan J, et al. Role of a Chest X-ray Severity Score in a Multivariable Predictive Model for Mortality in Patients with COVID-19: A Single-Center, Retrospective Study. Journal of Clinical Medicine. 2022; 11(8):2157. https://doi.org/10.3390/jcm11082157
Chicago/Turabian StyleBaikpour, Masoud, Alex Carlos, Ryan Morasse, Hannah Gissel, Victor Perez-Gutierrez, Jessica Nino, Jose Amaya-Suarez, Fatimatu Ali, Talya Toledano, Joseph Arampulikan, and et al. 2022. "Role of a Chest X-ray Severity Score in a Multivariable Predictive Model for Mortality in Patients with COVID-19: A Single-Center, Retrospective Study" Journal of Clinical Medicine 11, no. 8: 2157. https://doi.org/10.3390/jcm11082157
APA StyleBaikpour, M., Carlos, A., Morasse, R., Gissel, H., Perez-Gutierrez, V., Nino, J., Amaya-Suarez, J., Ali, F., Toledano, T., Arampulikan, J., Gold, M., Venugopal, U., Pillai, A., Omonuwa, K., & Menon, V. (2022). Role of a Chest X-ray Severity Score in a Multivariable Predictive Model for Mortality in Patients with COVID-19: A Single-Center, Retrospective Study. Journal of Clinical Medicine, 11(8), 2157. https://doi.org/10.3390/jcm11082157






