J. Clin. Med. 2020, 9(8), 2380; https://doi.org/10.3390/jcm9082380 - 26 Jul 2020
Cited by 53 | Viewed by 9744
Abstract
Summary: Exosomes are extracellular vesicles released by the vast majority of cell types both in vivo and ex vivo, upon the fusion of multivesicular bodies (MVBs) with the cellular plasma membrane. Two main functions have been attributed to exosomes: their capacity to transport
[...] Read more.
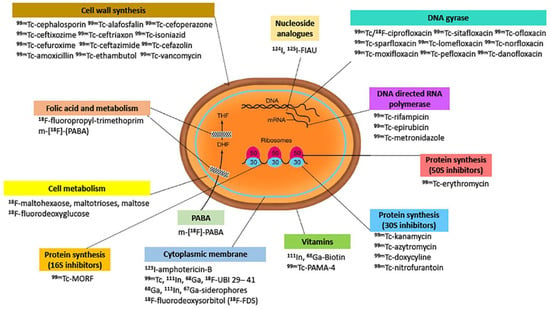
Summary: Exosomes are extracellular vesicles released by the vast majority of cell types both in vivo and ex vivo, upon the fusion of multivesicular bodies (MVBs) with the cellular plasma membrane. Two main functions have been attributed to exosomes: their capacity to transport proteins, lipids and nucleic acids between cells and organs, as well as their potential to act as natural intercellular communicators in normal biological processes and in pathologies. From a clinical perspective, the majority of applications use exosomes as biomarkers of disease. A new approach uses exosomes as biologically active carriers to provide a platform for the enhanced delivery of cargo in vivo. One of the major limitations in developing exosome-based therapies is the difficulty of producing sufficient amounts of safe and efficient exosomes. The identification of potential proteins involved in exosome biogenesis is expected to directly cause a deliberate increase in exosome production. In this review, we summarize the current state of knowledge regarding exosomes, with particular emphasis on their structural features, biosynthesis pathways, production techniques and potential clinical applications.
Full article
(This article belongs to the Special Issue Therapies Based on Mesenchymal Stem Cells (MSCs) and MSC-Derived Exosomes)
►
Show Figures