Catalyst Twenty-Twenty: Post-Traumatic Growth at Scales of Person, Place and Planet
Abstract
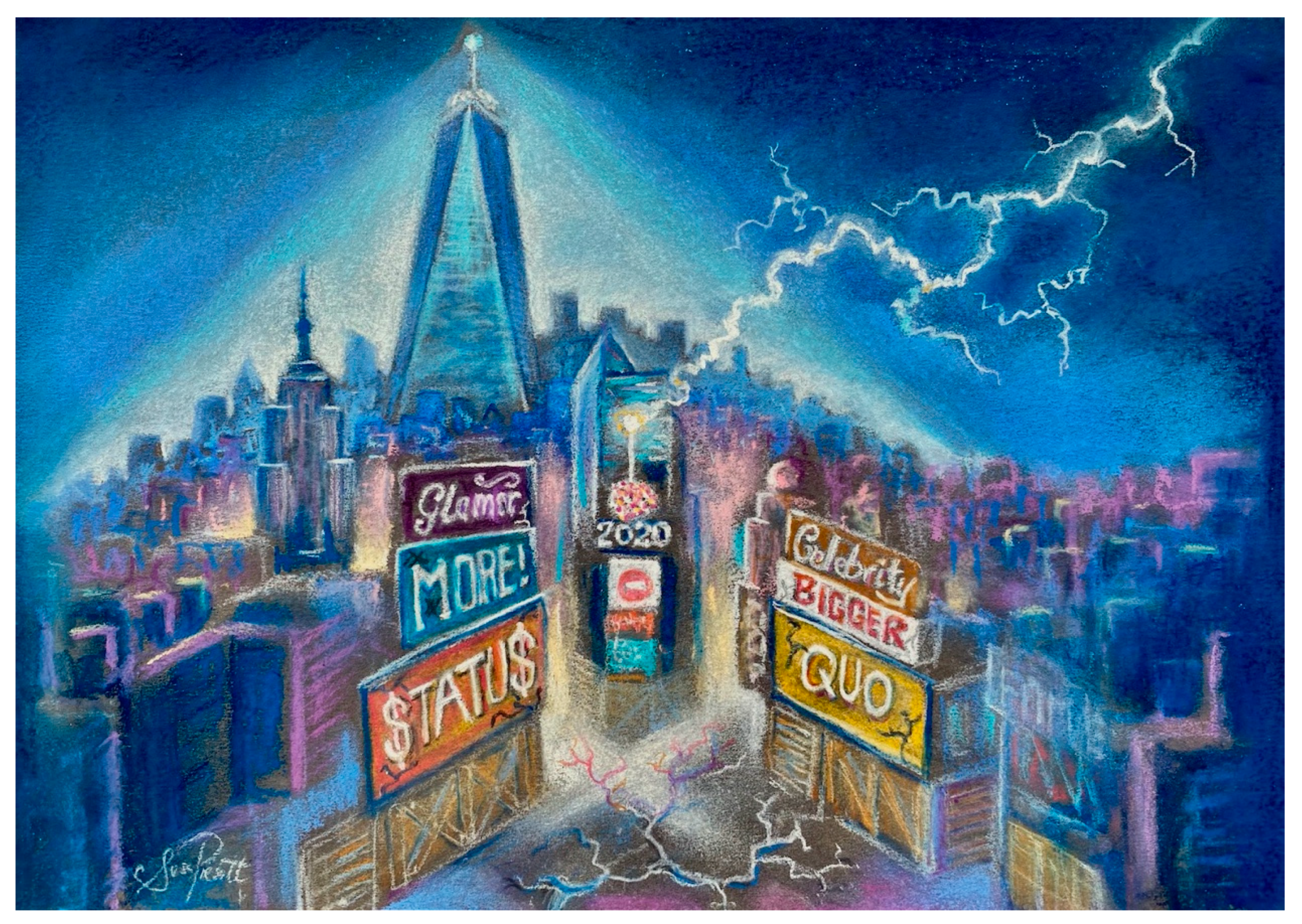
:1. Introduction
“With my barn burned down, nothing obstructs my view of the moon overhead”Mizuta Masahide, Japanese poet (1657–1723).
2. Post-Traumatic Growth
“The very greatest things—great thoughts, discoveries, inventions—have generally been nurtured in hardship, often pondered over in sorrow...if there were nothing to struggle for, there would be nothing to be achieved”Editors of The Friend magazine, 1866 [21].
3. New Awareness and Wisdom
“I want those who follow us to look back on us as wise ancestors, good ancestors”Jonas Salk. 1984 [45].
4. Post Twenty-Twenty
“Posttraumatic growth is not simply a return to baseline”Richard Tedeschi, Lawrence Calhoun. 2004.
5. Growth from One, to Many
“Everything can be taken [except] one thing: the last of the human freedoms—to choose one’s attitude in any given set of circumstances, to choose one’s own way,”Viktor E. Frankl, 1959 [96].
6. Conclusions
“We have a duty to trumpet the reality of post-traumatic growth, not only to those who have experienced PTSD or are likely to, but to society as a whole, so that when tragedy does strike we are prepared to receive its victims with a supportive and knowledgeable embrace; informed by science, warmed by compassion”Samuel Dickinson, Weill Cornell Medical College. 2020 [126].
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Horesh, D.; Brown, A.D. Traumatic Stress in the Age of COVID-19: A Call to Close Critical Gaps and Adapt to New Realities. Psychol. Trauma-Us 2020, 12, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Yang, Z.; Wang, X.; Li, J.; Dong, L.L.; Wang, F.S.; Li, Y.F.; Wei, R.H.; Zhang, J.P. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: A cross-sectional study. J. Clin. Nurs. 2020, 29, 4020–4029. [Google Scholar] [CrossRef]
- Fernandez Turienzo, C.; Newburn, M.; Agyepong, A.; Buabeng, R.; Dignam, A.; Abe, C.; Bedward, L.; Rayment-Jones, H.; Silverio, S.A.; Easter, A.; et al. Addressing inequities in maternal health among women living in communities of social disadvantage and ethnic diversity. BMC Public Health 2021, 21, 176. [Google Scholar] [CrossRef]
- Le, K.; Nguyen, M. The psychological burden of the COVID-19 pandemic severity. Econ. Hum. Biol 2021, 41, 100979. [Google Scholar] [CrossRef]
- Team, V.; Manderson, L. How COVID-19 Reveals Structures of Vulnerability. Med. Anthropol. 2020, 39, 671–674. [Google Scholar] [CrossRef] [PubMed]
- Poppas, A. 2020: A Year to Remember-And From Which to Learn. J. Am. Coll Cardiol 2021, 77, 659–660. [Google Scholar] [CrossRef] [PubMed]
- Eisner, D.A. 2020: An unusual year. J. Gen. Physiol. 2021, 153, 2. [Google Scholar] [CrossRef] [PubMed]
- Franklin, C. 2020—A year of changes, challenges and opportunities. J. Exp. Biol. 2021, 224 (Pt 1), jeb242155. [Google Scholar] [CrossRef]
- Roberts, D.J. 2020: A year we will remember. Transfus Med. 2020, 30, 416–417. [Google Scholar] [CrossRef] [PubMed]
- Nauleau, P.; Ralph, H. 2020: A year to remember. EBioMedicine 2021, 63, 103185. [Google Scholar] [CrossRef] [PubMed]
- Cipriano, P.F.; Boston-Leary, K.; McMillan, K.; Peterson, C. The US COVID-19 crises: Facts, science and solidarity. Int. Nurs. Rev. 2020, 67, 437–444. [Google Scholar] [CrossRef]
- Logan, A.C.; Berman, S.H.; Berman, B.M.; Prescott, S.L. Healing Anthropocene Syndrome: Planetary Health Requires Remediation of the Toxic Post-Truth Environment. Challenges 2021, 12, 1. [Google Scholar] [CrossRef]
- Morabia, A. The Fascist Threat. Am. J. Public Health 2021, e1–e2. [Google Scholar] [CrossRef]
- Zhang, Y.; Beggs, P.J.; McGushin, A.; Bambrick, H.; Trueck, S.; Hanigan, I.C.; Morgan, G.G.; Berry, H.L.; Linnenluecke, M.K.; Johnston, F.H.; et al. The 2020 special report of the MJA-Lancet Countdown on health and climate change: Lessons learnt from Australia’s “Black Summer”. Med. J. Aust. 2020, 213, 490–492. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.K.; Abrams, L.R.; Myrskyla, M. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc. Natl. Acad. Sci. USA 2020, 117, 6998–7000. [Google Scholar] [CrossRef] [Green Version]
- Harper, S.; Riddell, C.A.; King, N.B. Declining Life Expectancy in the United States: Missing the Trees for the Forest. Annu. Rev. Public Health 2020, 42, 2021. [Google Scholar]
- Collins, C. Updates: Billionaire Wealth, US Job Losses and Pandemic Profiteers. Inequality.Org. 26 January 2021. Available online: https://inequality.org/great-divide/updates-billionaire-pandemic/#:~:text=The%20collective%20wealth%20of%20all,10%20months%20of%20national%20emergency (accessed on 8 February 2021).
- Lauren, B.N.; Silver, E.R.; Faye, A.S.; Rogers, A.M.; Woo Baidal, J.A.; Ozanne, E.M.; Hur, C. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, C.; Hake, M.; Dewey, A.; Engelhard, E. Food Insecurity during COVID-19. 2021, ePub Ahead of Issue. Appl. Econ. Perspect. Policy 2021, 43, 153–161. [Google Scholar] [CrossRef]
- Benfer, E.A.; Vlahov, D.; Long, M.Y.; Walker-Wells, E.; Pottenger, J.L., Jr.; Gonsalves, G.; Keene, D.E. Eviction, Health Inequity, and the Spread of COVID-19: Housing Policy as a Primary Pandemic Mitigation Strategy. J. Urban. Health 2021, 98, 1–12. [Google Scholar] [CrossRef] [PubMed]
- The Editors (Anon). Self-Help. Friend 1866, 39, 117–118. [Google Scholar]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma Stress 1996, 9, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Turner, A.I.; Smyth, N.; Hall, S.J.; Torres, S.J.; Hussein, M.; Jayasinghe, S.U.; Ball, K.; Clow, A.J. Psychological stress reactivity and future health and disease outcomes: A systematic review of prospective evidence. Psychoneuroendocrinology 2020, 114, 104599. [Google Scholar] [CrossRef] [PubMed]
- Coimbra, B.M.; Carvalho, C.M.; Ota, V.K.; Vieira-Fonseca, T.; Bugiga, A.; Mello, A.F.; Mello, M.F.; Belangero, S.I. A systematic review on the effects of social discrimination on telomere length. Psychoneuroendocrinology 2020, 120, 104766. [Google Scholar] [CrossRef]
- Gavin, A.R.; Woo, B.; Conway, A.; Takeuchi, D. The Association between Racial Discrimination, Posttraumatic Stress Disorder, and Cardiovascular-Related Conditions among Non-Hispanic Blacks: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). J. Racial Ethn Health Disparities 2021. [Google Scholar] [CrossRef]
- Bourassa, K.J.; Hendrickson, R.C.; Reger, G.M.; Norr, A.M. Posttraumatic Stress Disorder Treatment Effects on Cardiovascular Physiology: A Systematic Review and Agenda for Future Research. J. Trauma Stress 2020. [Google Scholar] [CrossRef] [PubMed]
- Zieba, M.; Wiechec, K.; Bieganska-Banas, J.; Mieleszczenko-Kowszewicz, W. Coexistence of Post-traumatic Growth and Post-traumatic Depreciation in the Aftermath of Trauma: Qualitative and Quantitative Narrative Analysis. Front. Psychol. 2019, 10, 687. [Google Scholar] [CrossRef] [PubMed]
- Triplett, K.N.; Tedeschi, R.G.; Cann, A.; Calhoun, L.G.; Reeve, C.L. Posttraumatic Growth, Meaning in Life, and Life Satisfaction in Response to Trauma. Psychol. Trauma-Us 2012, 4, 400–410. [Google Scholar] [CrossRef] [Green Version]
- Mey, L.K.; Chmitorz, A.; Kurth, K.; Wenzel, M.; Kalisch, R.; Tuscher, O.; Kubiak, T. Increases of negative affect following daily hassles are not moderated by neuroticism: An ecological momentary assessment study. Stress Health 2020, 36, 615–628. [Google Scholar] [CrossRef]
- Jayawickreme, E.; Infurna, F.J.; Alajak, K.; Blackie, L.E.R.; Chopik, W.J.; Chung, J.M.; Dorfman, A.; Fleeson, W.; Forgeard, M.J.C.; Frazier, P.; et al. Post-traumatic growth as positive personality change: Challenges, opportunities, and recommendations. J. Personal. 2021, 89, 145–165. [Google Scholar] [CrossRef]
- Infurna, F.J.; Jayawickreme, E. Fixing the Growth Illusion: New Directions for Research in Resilience and Posttraumatic Growth. Curr. Dir. Psychol. Sci. 2019, 28, 152–158. [Google Scholar] [CrossRef]
- Tsai, J.; Pietrzak, R.H. Trajectories of posttraumatic growth among US military veterans: A 4-year nationally representative, prospective cohort study. Acta Psychiatr. Scand. 2017, 136, 483–492. [Google Scholar] [CrossRef]
- Tallman, B.; Shaw, K.; Schultz, J.; Altmaier, E. Well-being and posttraumatic growth in unrelated donor marrow transplant survivors: A nine-year longitudinal study. Rehabil. Psychol. 2010, 55, 204–210. [Google Scholar] [CrossRef]
- Wolchik, S.A.; Coxe, S.; Tein, J.Y.; Sandler, I.N.; Ayers, T.S. Six-year longitudinal predictors of posttraumatic growth in parentally bereaved adolescents and young adults. Omega (Westport) 2008, 58, 107–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boehm, J.K.; Chen, Y.; Williams, D.R.; Ryff, C.; Kubzansky, L.D. Unequally distributed psychological assets: Are there social disparities in optimism, life satisfaction, and positive affect? PLoS ONE 2015, 10, e0118066. [Google Scholar] [CrossRef] [Green Version]
- Zou, R.; Xu, X.; Hong, X.; Yuan, J. Higher Socioeconomic Status Predicts Less Risk of Depression in Adolescence: Serial Mediating Roles of Social Support and Optimism. Front. Psychol. 2020, 11, 1955. [Google Scholar] [CrossRef]
- Weyers, S.; Dragano, N.; Mobus, S.; Beck, E.M.; Stang, A.; Mohlenkamp, S.; Jockel, K.H.; Erbel, R.; Siegrist, J. Low socio-economic position is associated with poor social networks and social support: Results from the Heinz Nixdorf Recall Study. Int. J. Equity Health 2008, 7, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aartsen, M.; Veenstra, M.; Hansen, T. Social pathways to health: On the mediating role of the social network in the relation between socio-economic position and health. SSM Popul. Health 2017, 3, 419–426. [Google Scholar] [CrossRef]
- Prescott, S.L.; Logan, A.C. Each meal matters in the exposome: Biological and community considerations in fast-food-socioeconomic associations. Econ. Hum. Biol. 2017, 27 (Pt B), 328–335. [Google Scholar] [CrossRef]
- Hamama-Raz, Y.; Pat-Horenczyk, R.; Roziner, I.; Perry, S.; Stemmer, S.M. Can posttraumatic growth after breast cancer promote positive coping?-A cross-lagged study. Psychooncology 2019, 28, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Kaminga, A.C.; Dai, W.; Deng, J.; Wang, Z.; Pan, X.; Liu, A. The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. J. Affect. Disord. 2019, 243, 408–415. [Google Scholar] [CrossRef]
- Gilbert, D.T.; Pinel, E.C.; Wilson, T.D.; Blumberg, S.J.; Wheatley, T.P. Immune neglect: A source of durability bias in affective forecasting. J. Personal. Soc. Psychol. 1998, 75, 617–638. [Google Scholar] [CrossRef]
- Boals, A.; Bedford, L.A.; Callahan, J.L. Perceptions of Change after a Trauma and Perceived Posttraumatic Growth: A Prospective Examination. Behav. Sci. 2019, 9, 10. [Google Scholar] [CrossRef] [Green Version]
- Locke, R. Salk: Be a Good Ancestor; Standard-Speaker: Hazleton, PA, USA, 9 March 1984; p. 10. [Google Scholar]
- Walsh, D.M.J.; Groarke, A.M.; Morrison, T.G.; Durkan, G.; Rogers, E.; Sullivan, F.J. Measuring a new facet of post traumatic growth: Development of a scale of physical post traumatic growth in men with prostate cancer. PLoS ONE 2018, 13, e0195992. [Google Scholar] [CrossRef] [Green Version]
- Bhushan, B. Perspectives on Posttraumatic Growth. In Psychosocial Interventions for Health and Well-Being; Misra, G., Ed.; Springer: New Delhi, India, 2018. [Google Scholar] [CrossRef]
- Zeligman, M.; Varney, M.; Grad, R.I.; Huffstead, M. Posttraumatic Growth in Individuals With Chronic Illness: The Role of Social Support and Meaning Making. J. Couns. Dev. 2018, 96, 53–63. [Google Scholar] [CrossRef]
- King, L.A.; Hicks, J.A.; Krull, J.L.; Del Gaiso, A.K. Positive affect and the experience of meaning in life. J. Personal. Soc. Psychol. 2006, 90, 179–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martela, F.; Steger, M.F. The three meanings of meaning in life: Distinguishing coherence, purpose, and significance. J. Posit Psychol. 2016, 11, 531–545. [Google Scholar] [CrossRef]
- Burrow, A.L.; Spreng, R.N. Waiting with purpose: A reliable but small association between purpose in life and impulsivity. Personal. Individ. Differ. 2016, 90, 187–189. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.S.; Strecher, V.J.; Ryff, C.D. Purpose in life and use of preventive health care services. Proc. Natl. Acad. Sci. USA 2014, 111, 16331–16336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, E.S.; Shiba, K.; Boehm, J.K.; Kubzansky, L.D. Sense of purpose in life and five health behaviors in older adults. Prev. Med. 2020, 139, 106172. [Google Scholar] [CrossRef] [PubMed]
- Zilioli, S.; Slatcher, R.B.; Ong, A.D.; Gruenewald, T.L. Purpose in life predicts allostatic load ten years later. J. Psychosom. Res. 2015, 79, 451–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, R.; Bavishi, C.; Rozanski, A. Purpose in Life and Its Relationship to All-Cause Mortality and Cardiovascular Events: A Meta-Analysis. Psychosom. Med. 2016, 78, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Strecher, V.; Terry, P. Health and life purpose: What’s the connection? Am. J. Health Promot. 2014, 29, TAHP2-4. [Google Scholar] [PubMed]
- Straus, E.; Norman, S.B.; Tripp, J.C.; Pitts, M.; Pietrzak, R.H. Purpose in Life and Conscientiousness Protect Against the Development of Suicidal Ideation in U.S. Military Veterans with PTSD and MDD: Results from the National Health and Resilience in Veterans Study. Chronic Stress (Thousand Oaks) 2019, 3, 2470547019872172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinoshita, S.; Hirooka, N.; Kusano, T.; Saito, K.; Nakamoto, H. Does Improvement in Health-Related Lifestyle Habits Increase Purpose in Life among a Health Literate Cohort? Int. J. Environ. Res. Public Health 2020, 17, 8878. [Google Scholar] [CrossRef]
- Grossmann, I.; Weststrate, N.M.; Ardelt, M.; Brienza, J.P.; Dong, M.X.; Ferrari, M.; Fournier, M.A.; Hu, C.S.; Nusbaum, H.C.; Vervaeke, J. The Science of Wisdom in a Polarized World: Knowns and Unknowns. Psychol. Inq. 2020, 31, 103–133. [Google Scholar] [CrossRef]
- Koller, I.; Levenson, M.R.; Gluck, J. What Do You Think You Are Measuring? A Mixed-Methods Procedure for Assessing the Content Validity of Test Items and Theory-Based Scaling. Front. Psychol. 2017, 8, 126. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.K.; Ha, Y. Exploring the Relationships between Posttraumatic Growth, Wisdom, and Quality of Life in Older Cancer Survivors. Asian Pac. J. Cancer Prev. 2019, 20, 2667–2672. [Google Scholar] [CrossRef]
- Byra, S. Associations between post-traumatic growth and wisdom in people with long-term paraplegia—The role of disability appraisals and participation. Disabil. Rehabil. 2021, 1–8. [Google Scholar] [CrossRef]
- Ardelt, M.; Jeste, D.V. Wisdom and Hard Times: The Ameliorating Effect of Wisdom on the Negative Association Between Adverse Life Events and Well-Being. J. Gerontol. B Psychol. Sci. Soc. Sci. 2018, 73, 1374–1383. [Google Scholar] [CrossRef] [Green Version]
- Weststrate, N.M.; Gluck, J. Hard-Earned Wisdom: Exploratory Processing of Difficult Life Experience Is Positively Associated With Wisdom. Dev. Psychol. 2017, 53, 800–814. [Google Scholar] [CrossRef]
- Plews-Ogan, M.; Ardelt, M.; Owens, J. Growth through Adversity: Exploring Associations between Internal Strengths, Posttraumatic Growth, and Wisdom. J. Value Inquiry 2019, 53, 371–391. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Shakespeare-Finch, J.; Taku, K.; Calhoun, L.G. Posttraumatic growth beyond the individual. In Posttraumatic Growth: Theory, Research, and Applications; Tedeschi, R.G., Ed.; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Ferrari, M.; Alhosseini, F. Cultural differences in wisdom. In The Cambridge Handbook of Wisdom; Sternberg, R.J., Gluck, J., Eds.; Cambridge University Press: Cambridge, UK, 2019; pp. 409–428. [Google Scholar]
- Yang, S.; Intezari, A. Non-western lay conceptions of wisdom. In The Cambridge Handbook of Wisdom; Sternberg, R.J., Gluck, J., Eds.; Cambridge University Press: Cambridge, UK, 2019; pp. 429–452. [Google Scholar]
- Laslo-Roth, R.; George-Levi, S.; Margalit, M. Social participation and posttraumatic growth: The serial mediation of hope, social support, and reappraisal. J. Community Psychol. 2020. [Google Scholar] [CrossRef]
- Stallard, P.; Pereira, A.I.; Barros, L. Post-traumatic growth during the COVID-19 pandemic in carers of children in Portugal and the UK: Cross-sectional online survey. BJPsych Open 2021, 7, e37. [Google Scholar] [CrossRef]
- Vazquez, C.; Valiente, C.; Garcia, F.E.; Contreras, A.; Peinado, V.; Trucharte, A.; Bentall, R.P. Post-Traumatic Growth and Stress-Related Responses during the COVID-19 Pandemic in a National Representative Sample: The Role of Positive Core Beliefs about the World and Others. J. Happiness Stud. 2021, 1–21. [Google Scholar] [CrossRef]
- White, R.E.; Kuehn, M.M.; Duckworth, A.L.; Kross, E.; Ayduk, O. Focusing on the future from afar: Self-distancing from future stressors facilitates adaptive coping. Emotion 2019, 19, 903–916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grossmann, I.; Kross, E. The impact of culture on adaptive versus maladaptive self-reflection. Psychol. Sci. 2010, 21, 1150–1157. [Google Scholar] [CrossRef] [Green Version]
- Dorfman, A.; Oakes, H.; Santos, H.C.; Grossmann, I. Self-distancing promotes positive emotional change after adversity: Evidence from a micro-longitudinal field experiment. J. Personal. 2021, 89, 132–144. [Google Scholar] [CrossRef]
- Grossmann, I.; Kross, E. Exploring Solomon’s paradox: Self-distancing eliminates the self-other asymmetry in wise reasoning about close relationships in younger and older adults. Psychol. Sci. 2014, 25, 1571–1580. [Google Scholar] [CrossRef]
- Kross, E.; Grossmann, I. Boosting wisdom: Distance from the self enhances wise reasoning, attitudes, and behavior. J. Exp. Psychol. Gen. 2012, 141, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Huynh, A.C.; Yang, D.Y.J.; Grossmann, I. The Value of Prospective Reasoning for Close Relationships. Soc. Psychol. Personal. Sci. 2016, 7, 893–902. [Google Scholar] [CrossRef]
- Glueck, J.; Bluck, S.; Weststrate, N.M. More on the MORE Life Experience Model: What We Have Learned (So Far). J. Value Inquiry 2019, 53, 349–370. [Google Scholar] [CrossRef] [Green Version]
- Whitehead, R.; Bates, G.; Elphinstone, B. Growing by Letting Go: Nonattachment and Mindfulness as Qualities of Advanced Psychological Development. J. Adult Dev. 2020, 27, 12–22. [Google Scholar] [CrossRef]
- Shiyko, M.P.; Hallinan, S.; Naito, T. Effects of Mindfulness Training on Posttraumatic Growth: A Systematic Review and Meta-Analysis. Mindfulness 2017, 8, 848–858. [Google Scholar] [CrossRef]
- Ardelt, M. Can wisdom and psychosocial growth be learned in university courses? J. Moral Educ. 2020, 49, 30–45. [Google Scholar] [CrossRef]
- Boulware, J.; Huskey, B.; Mangelsdorf, H.; Nusbaum, H. The Effects of Mindfulness Training on Wisdom in Elementary School Teachers. J. Educ. Soc. Behav. Sci. 2019, 30, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Gluck, J. The Important Difference Between Psychologists’ Labs and Real Life: Evaluating the Validity of Models of Wisdom. Psychol. Inq. 2020, 31, 144–150. [Google Scholar] [CrossRef]
- Stellar, J.E.; Gordon, A.M.; Piff, P.K.; Cordaro, D.; Anderson, C.L.; Bai, Y.; Maruskin, L.A.; Keltner, D. Self-Transcendent Emotions and Their Social Functions: Compassion, Gratitude, and Awe Bind Us to Others Through Prosociality. Emot. Rev. 2017, 9, 200–207. [Google Scholar] [CrossRef] [Green Version]
- Keltner, D.; Piff, P.K. Self-Transcendent Awe as a Moral Grounding of Wisdom. Psychol. Inq. 2020, 31, 160–163. [Google Scholar] [CrossRef]
- Keltner, D.; Haidt, J. Approaching awe, a moral, spiritual, and aesthetic emotion. Cogn. Emot. 2003, 17, 297–314. [Google Scholar] [CrossRef] [PubMed]
- Sturm, V.E.; Datta, S.; Roy, A.R.K.; Sible, I.J.; Kosik, E.L.; Veziris, C.R.; Chow, T.E.; Morris, N.A.; Neuhaus, J.; Kramer, J.H.; et al. Big smile, small self: Awe walks promote prosocial positive emotions in older adults. Emotion 2020. [Google Scholar] [CrossRef]
- Arcangeli, M.; Sperduti, M.; Jacquot, A.; Piolino, P.; Dokic, J. Awe and the Experience of the Sublime: A Complex Relationship. Front. Psychol. 2020, 11, 1340. [Google Scholar] [CrossRef] [PubMed]
- Rudd, M.; Vohs, K.D.; Aaker, J. Awe Expands People’s Perception of Time, Alters Decision Making, and Enhances Well-Being. Psychol. Sci. 2012, 23, 1130–1136. [Google Scholar] [CrossRef] [PubMed]
- Shiota, M.N.; Keltner, D.; Mossman, A. The nature of awe: Elicitors, appraisals, and effects on self-concept. Cogn. Emot. 2007, 21, 944–963. [Google Scholar] [CrossRef]
- Van Cappellen, P.; Saroglou, V. Awe Activates Religious and Spiritual Feelings and Behavioral Intentions. Psychol. Relig. Spirit. 2012, 4, 223–236. [Google Scholar] [CrossRef] [Green Version]
- Stellar, J.E.; John-Henderson, N.; Anderson, C.L.; Gordon, A.M.; McNeil, G.D.; Keltner, D. Positive Affect and Markers of Inflammation: Discrete Positive Emotions Predict Lower Levels of Inflammatory Cytokines. Emotion 2015, 15, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Schneider, K.J. Awe: More than a lab experience—A rejoinder to “awe: ‘more than a feeling’” by Alice Chirico and Andrea Gaggioli. Humanist. Psychol. 2020, 48, 100–104. [Google Scholar] [CrossRef]
- Schneider, K.J. The Depolarizing of America. A Guidebook for Social Healing; University Professors Press: Colorado Springs, CO, USA, 2020. [Google Scholar]
- Sun, X.; Su, W.; Guo, X.; Tian, Z. The Impact of Awe Induced by COVID-19 Pandemic on Green Consumption Behavior in China. Int. J. Environ. Res. Public Health 2021, 18, 543. [Google Scholar] [CrossRef]
- Frankl, V. Man’s Search for Meaning; Beacon Press: Boston, MA, USA, 1959. [Google Scholar]
- Koliouli, F.; Canellopoulos, L. Dispositional Optimism, Stress, Post-traumatic stress Disorder and Post-traumatic Growth in Greek general population facing the COVID-19 crisis. Eur. J. Trauma Dissociation 2021, 100209. [Google Scholar] [CrossRef]
- Malouff, J.M.; Schutte, N.S. Can psychological interventions increase optimism? A meta-analysis. J. Posit Psychol. 2017, 12, 594–604. [Google Scholar] [CrossRef]
- Scheier, M.F.; Swanson, J.D.; Barlow, M.A.; Greenhouse, J.B.; Wrosch, C.; Tindle, H.A. Optimism versus pessimism as predictors of physical health: A comprehensive reanalysis of dispositional optimism research. Am. Psychol. 2020. [Google Scholar] [CrossRef]
- Heinonen, K.; Raikkonen, K.; Matthews, K.A.; Scheier, M.F.; Raitakari, O.T.; Pulkki, L.; Keltikangas-Jarvinen, L. Socioeconomic status in childhood and adulthood: Associations with dispositional optimism and pessimism over a 21-year follow-up. J. Personal. 2006, 74, 1111–1126. [Google Scholar] [CrossRef]
- Robb, K.A.; Simon, A.E.; Wardle, J. Socioeconomic disparities in optimism and pessimism. Int. J. Behav. Med. 2009, 16, 331–338. [Google Scholar] [CrossRef]
- Chipperfield, J.G.; Hamm, J.M.; Perry, R.P.; Parker, P.C.; Ruthig, J.C.; Lang, F.R. A healthy dose of realism: The role of optimistic and pessimistic expectations when facing a downward spiral in health. Soc. Sci. Med. 2019, 232, 444–452. [Google Scholar] [CrossRef]
- Alkalay, S.; Sagi-Schwartz, A.; Wiseman, H. Increased empathy and helping behavior toward the mother in daughters of Holocaust survivors. Traumatology 2020, 26, 84–95. [Google Scholar] [CrossRef]
- Zwahlen, D.; Hagenbuch, N.; Carley, M.I.; Jenewein, J.; Buchi, S. Posttraumatic growth in cancer patients and partners--effects of role, gender and the dyad on couples’ posttraumatic growth experience. Psychooncology 2010, 19, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Manne, S.; Ostroff, J.; Winkel, G.; Goldstein, L.; Fox, K.; Grana, G. Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosom. Med. 2004, 66, 442–454. [Google Scholar]
- Cormio, C.; Romito, F.; Viscanti, G.; Turaccio, M.; Lorusso, V.; Mattioli, V. Psychological well-being and posttraumatic growth in caregivers of cancer patients. Front. Psychol. 2014, 5, 1342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamibeppu, K.; Sato, I.; Honda, M.; Ozono, S.; Sakamoto, N.; Iwai, T.; Okamura, J.; Asami, K.; Maeda, N.; Inada, H.; et al. Mental health among young adult survivors of childhood cancer and their siblings including posttraumatic growth. J. Cancer Surviv. 2010, 4, 303–312. [Google Scholar] [CrossRef]
- Greene, T.; Lahav, Y.; Kanat-Maymon, Y.; Solomon, Z. A Longitudinal Study of Secondary Posttraumatic Growth in Wives of Ex-POWs. Psychiatry 2015, 78, 186–197. [Google Scholar] [PubMed]
- Dar, I.A.; Iqbal, N. Beyond linear evidence: The curvilinear relationship between secondary traumatic stress and vicarious posttraumatic growth among healthcare professionals. Stress Health 2020, 36, 203–212. [Google Scholar] [CrossRef]
- Doherty, M.E.; Scannell-Desch, E.; Bready, J. A Positive Side of Deployment: Vicarious Posttraumatic Growth in U.S. Military Nurses Who Served in the Iraq and Afghanistan Wars. J. Nurs. Scholarsh. 2020, 52, 233–241. [Google Scholar] [CrossRef]
- Zerach, G. “He ain’t heavy, he’s my brother”: Distress tolerance moderates the association between secondary posttraumatic symptoms and secondary posttraumatic growth among siblings of combat veterans. Psychol. Trauma 2020, 12, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Maitlis, S. Posttraumatic Growth at Work. Annu Rev. Organ. Psych. 2020, 7, 395–419. [Google Scholar] [CrossRef] [Green Version]
- Olson, K.; Shanafelt, T.; Southwick, S. Pandemic-Driven Posttraumatic Growth for Organizations and Individuals. JAMA 2020, 324, 1829–1830. [Google Scholar] [CrossRef]
- Hormann, S.; Vivian, P. Organizational trauma in university settings. In Emerging Contours of Excellence; Mohan, J., Ed.; Punjab University of Press: Chandigarh, India, 2017; pp. 188–198. [Google Scholar]
- Alexander, B.N.; Greenbaum, B.; Shani, A.B.; Mitki, Y. Organizational Post-Traumatic Growth: Thriving After Adversity. Acad. Manag. Proc. 2020, 2020, 18506. [Google Scholar] [CrossRef]
- Calhoun, L.G.; Tedeschi, R.G. Posttraumatic Growth in Clinical Practice; Routledge: East Sussex, UK, 2013. [Google Scholar]
- Vázquez, C.; Pérez-Sales, P.; Hervás, G. Positive effects of terrorism and posttraumatic growth: An individual and community perspective. In Trauma, Recovery, and Growth: Positive Psychological Perspectives on Posttraumatic Stress; Joseph, S., Linley, P.A., Eds.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2008; pp. 63–91. [Google Scholar]
- Eaton-Robb, P. Sandy Hook: Families Dedicate Time to Charity, Activism 5 Years after Tragedy; Associated Press, 14 December 2017; Available online: https://www.usatoday.com/story/news/nation/2017/12/13/sandy-hook-school-shooting-families-5-year-anniversary/951016001/ (accessed on 5 March 2021).
- Wilcox, A.M. “We’ve Had Enough”: Youth Activists’ Pathways to Participation and Social Media Practices Following the Parkland Shooting. Clemson University, All Dissertations. 2020, p. 2698. Available online: https://tigerprints.clemson.edu/all_dissertations/2698 (accessed on 5 March 2021).
- Kirby, T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir. Med. 2020, 8, 547–548. [Google Scholar] [CrossRef]
- Barber, R.; Law, S.F. Exposing Inequity in Australian Society: Are we all in it Together? Soc. Health Sci. 2020, 18, 96–115. [Google Scholar]
- Pauls, J.E. The Impact of Posttraumatic Growth on Authentic Leader Development: Five Portraits of Women Cancer Survivors in Leadership. Gonzaga University, ProQuest Dissertations Publishing. Number 10666061. 2017. Available online: https://search.proquest.com/openview/0a8862b27dba3b281b0f97e32ef32cc1/1?cbl=18750&diss=y&pq-origsite=gscholar (accessed on 12 February 2021).
- Gluck, J. Wisdom vs. populism and polarization: Learning to regulate our evolved intuitions. In Applying Wisdom to Contemporary World Problems; Sternberg, R.J., Ed.; Palgrave MacMillan: London, UK, 2019. [Google Scholar]
- Griskevicius, V.; Cantu, S.M.; van Vugt, M. The Evolutionary Bases for Sustainable Behavior: Implications for Marketing, Policy, and Social Entrepreneurship. J. Public Policy Mark. 2012, 31, 115–128. [Google Scholar] [CrossRef]
- Mischinski, M.; Jayawickreme, E. Can moral exemplars promote wisdom. In Applying Wisdom to Contemporary World Problems; Sternberg, R.J., Ed.; Palgrave MacMillan: London, UK, 2019. [Google Scholar]
- Dickinson, S. Post-traumatic growth in the twenty-first century: How current trends may threaten our ability to grow after trauma. J. Posit. Psychol. 2020. [Google Scholar] [CrossRef]
- Prescott, S.L.; Bland, J.S. Spaceship Earth Revisited: The Co-Benefits of Overcoming Biological Extinction of Experience at the Level of Person, Place and Planet. Int. J. Environ. Res. Public Health 2020, 17, 1407. [Google Scholar] [CrossRef] [Green Version]
- Seligman, M.; Flourish, A. Visionary New Understanding of Happiness and Well-Being; Free Press: New York, NY, USA, 2011. [Google Scholar]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Logan, A.C.; Berman, S.H.; Scott, R.B.; Berman, B.M.; Prescott, S.L. Catalyst Twenty-Twenty: Post-Traumatic Growth at Scales of Person, Place and Planet. Challenges 2021, 12, 9. https://doi.org/10.3390/challe12010009
Logan AC, Berman SH, Scott RB, Berman BM, Prescott SL. Catalyst Twenty-Twenty: Post-Traumatic Growth at Scales of Person, Place and Planet. Challenges. 2021; 12(1):9. https://doi.org/10.3390/challe12010009
Chicago/Turabian StyleLogan, Alan C., Susan H. Berman, Richard B. Scott, Brian M. Berman, and Susan L. Prescott. 2021. "Catalyst Twenty-Twenty: Post-Traumatic Growth at Scales of Person, Place and Planet" Challenges 12, no. 1: 9. https://doi.org/10.3390/challe12010009
APA StyleLogan, A. C., Berman, S. H., Scott, R. B., Berman, B. M., & Prescott, S. L. (2021). Catalyst Twenty-Twenty: Post-Traumatic Growth at Scales of Person, Place and Planet. Challenges, 12(1), 9. https://doi.org/10.3390/challe12010009




