Antimicrobial Activity of Zinc Oxide Nano/Microparticles and Their Combinations against Pathogenic Microorganisms for Biomedical Applications: From Physicochemical Characteristics to Pharmacological Aspects
Abstract
:1. Introduction
2. Characteristics of ZnO Materials Based on Synthesis Techniques
2.1. Synthesis Techniques of ZnO Materials
2.2. Physicochemical Characteristics of ZnO Materials
3. Antimicrobial ctivity against Pathogenic Microorganisms
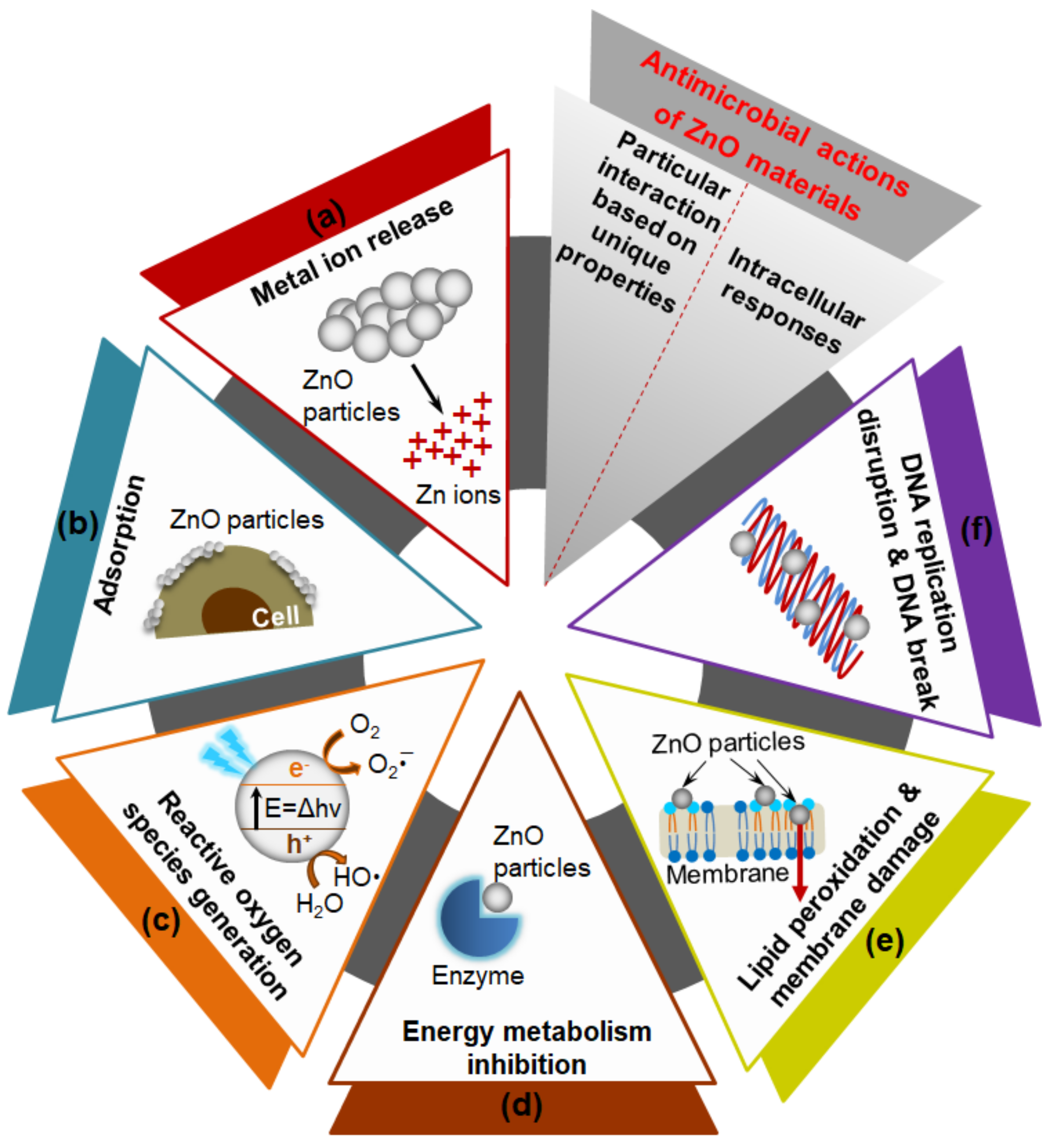
3.1. Antimicrobial Mechanisms of ZnO Materials
3.2. ZnO Materials and Combinations Based on Antimicrobial Functions
3.2.1. ZnO Materials
3.2.2. ZnO Materials with Drugs
3.2.3. ZnO Materials with Other Metal Oxide NPs/MPs or Metal Doping
3.2.4. ZnO Materials with Other Biomaterials
3.2.5. ZnO QDs
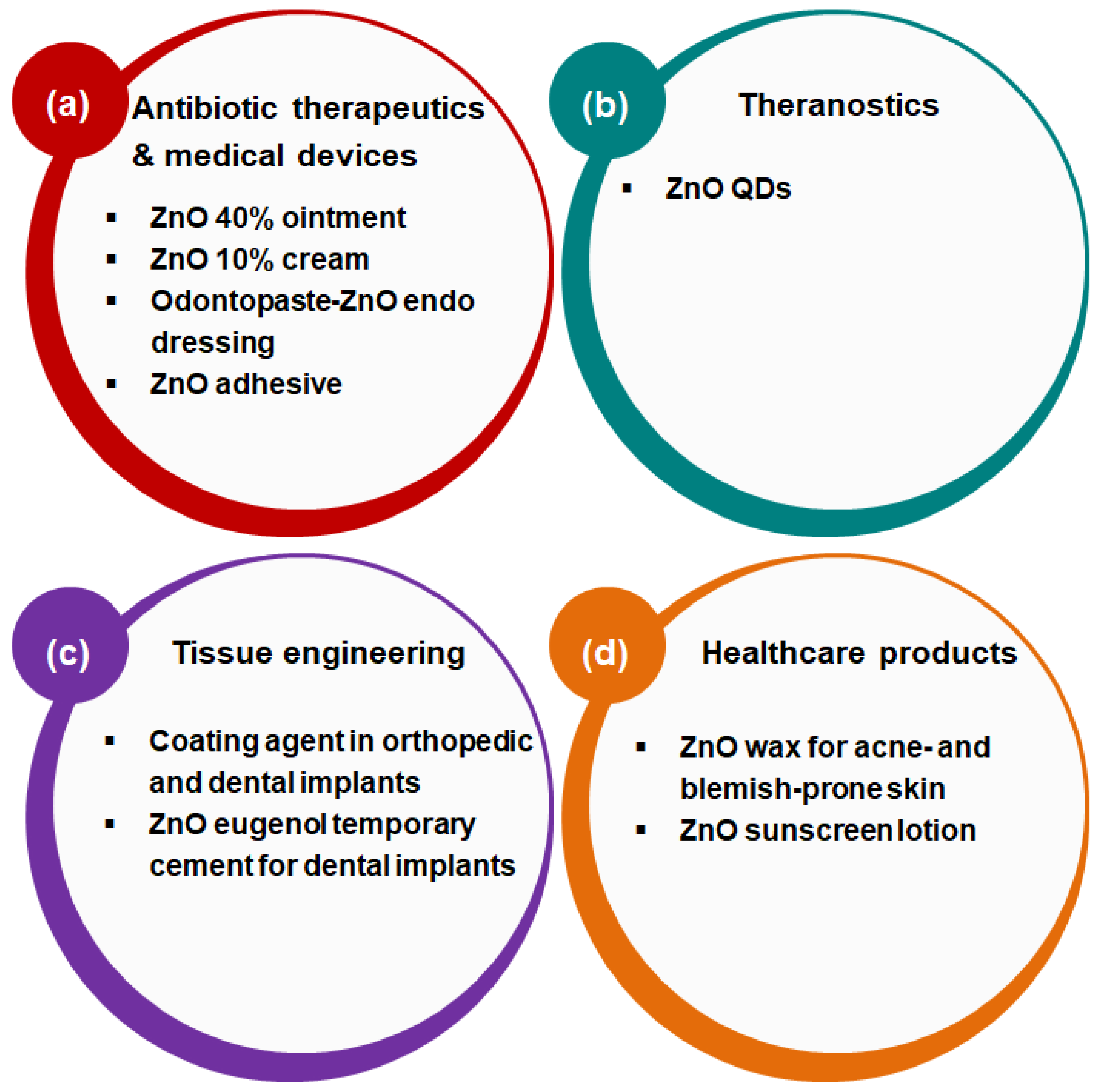
4. Current Biomedical Applications
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| BC | Bacterial cellulose |
| BSA | Bovine serum albumin |
| CFU | Colony forming unit |
| CFX | Ceftriaxone |
| CFZ | Ceftazidime |
| C-jZnO | Curcumin-loaded ZnO javelin |
| C-lpZnO | Curcumin-loaded long petal zno nanoflower |
| C-nZnO | Cotton-ZnO nanoparticle nanocomposite |
| C-rZnO | Curcumin-loaded ZnO rod |
| C-spZnO | Curcumin-loaded short petal zno nanoflower |
| C-sZnO | Curcumin-loaded ZnO sphere |
| C-ZnO | Curcumin-loaded ZnO |
| C-ZnO@gal | Chitosan-ZnO nanoparticle-loaded gallic acid |
| D | Dark |
| GO | Graphene oxide |
| GTM | Gentamicin |
| HA-ZnO-Alg | Hydroxyapatite-biphasic ZnO nanoparticle/microparticle-embedded alginate |
| HSV-2 | Herpes simplex virus type-2 |
| KC | K-carrageenan |
| L | Light |
| Met | Methicillin |
| MIC | Minimum inhibitory concentration |
| MPs | Microparticles |
| MRSA | Methicillin-resistant staphylococcus aureus |
| nZnO-chitosan/gelatin | ZnO NP-containing chitosan/gelatin hybrid nanocomposite |
| PE | Polyethylene |
| PVP | Polyvinylpyrrolidone |
| QDs | Quantum dots |
| rGO | Reduced graphene oxide |
| UV | Ultraviolet |
| Van | Vancomycin |
| W-PEG-ZnO | Tungsten-doped polyethylene glycol-capped ZnO |
References
- Makabenta, J.M.V.; Nabawy, A.; Li, C.-H.; Schmidt-Malan, S.; Patel, R.; Rotello, V.M. Nanomaterial-based therapeutics for antibiotic-resistant bacterial infections. Nat. Rev. Microbiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Muzammil, S.; Hayat, S.; Fakhar, E.A.M.; Aslam, B.; Siddique, M.H.; Nisar, M.A.; Saqalein, M.; Atif, M.; Sarwar, A.; Khurshid, A.; et al. Nanoantibiotics: Future nanotechnologies to combat antibiotic resistance. Front. Biosci. 2018, 10, 352–374. [Google Scholar] [CrossRef] [Green Version]
- da Silva, B.L.; Abuçafy, M.P.; Berbel Manaia, E.; Oshiro Junior, J.A.; Chiari-Andréo, B.G.; Pietro, R.C.R.; Chiavacci, L.A. Relationship Between Structure And Antimicrobial Activity Of Zinc Oxide Nanoparticles: An Overview. Int. J. Nanomed. 2019, 14, 9395–9410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dizaj, S.M.; Lotfipour, F.; Barzegar-Jalali, M.; Zarrintan, M.H.; Adibkia, K. Antimicrobial activity of the metals and metal oxide nanoparticles. Mater. Sci. Eng. C 2014, 44, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.-E.; Jin, H.-E. Synthesis, Characterization, and Three-Dimensional Structure Generation of Zinc Oxide-Based Nanomedicine for Biomedical Applications. Pharmaceutics 2019, 11, 575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ul Haq, A.N.; Nadhman, A.; Ullah, I.; Mustafa, G.; Yasinzai, M.; Khan, I. Synthesis Approaches of Zinc Oxide Nanoparticles: The Dilemma of Ecotoxicity. J. Nanomater. 2017, 2017, 8510342. [Google Scholar] [CrossRef]
- Sánchez-López, E.; Gomes, D.; Esteruelas, G.; Bonilla, L.; Lopez-Machado, A.L.; Galindo, R.; Cano, A.; Espina, M.; Ettcheto, M.; Camins, A.; et al. Metal-Based Nanoparticles as Antimicrobial Agents: An Overview. Nanomaterials 2020, 10, 292. [Google Scholar] [CrossRef] [Green Version]
- Van Giau, V.; An, S.S.A.; Hulme, J. Recent advances in the treatment of pathogenic infections using antibiotics and nano-drug delivery vehicles. Drug Des. Dev. Ther. 2019, 13, 327–343. [Google Scholar] [CrossRef] [Green Version]
- Bajwa, N.; Mehra, N.K.; Jain, K.; Jain, N.K. Pharmaceutical and biomedical applications of quantum dots. Artif. Cells Nanomed. Biotechnol. 2016, 44, 758–768. [Google Scholar] [CrossRef]
- Khan, S.T.; Musarrat, J.; Al-Khedhairy, A.A. Countering drug resistance, infectious diseases, and sepsis using metal and metal oxides nanoparticles: Current status. Colloids Surf. B Biointerfaces 2016, 146, 70–83. [Google Scholar] [CrossRef]
- Martínez-Carmona, M.; Gun’ko, Y.; Vallet-Regí, M. ZnO Nanostructures for Drug Delivery and Theranostic Applications. Nanomaterials 2018, 8, 268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pelgrift, R.Y.; Friedman, A.J. Nanotechnology as a therapeutic tool to combat microbial resistance. Adv. Drug Deliv. Rev. 2013, 65, 1803–1815. [Google Scholar] [CrossRef] [PubMed]
- Czyżowska, A.; Barbasz, A. A review: Zinc oxide nanoparticles—Friends or enemies? Int. J. Environ. Health Res. 2020. [Google Scholar] [CrossRef]
- Sirelkhatim, A.; Mahmud, S.; Seeni, A.; Kaus, N.H.M.; Ann, L.C.; Bakhori, S.K.M.; Hasan, H.; Mohamad, D. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nano-micro Lett. 2015, 7, 219–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Z.; Li, Q.; Wang, J.; Yu, Y.; Wang, Y.; Zhou, Q.; Li, P. Reactive Oxygen Species-Related Nanoparticle Toxicity in the Biomedical Field. Nanoscale Res. Lett. 2020, 15, 115. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, K.R.; Koodali, R.T.; Manna, A.C. Size-Dependent Bacterial Growth Inhibition and Mechanism of Antibacterial Activity of Zinc Oxide Nanoparticles. Langmuir 2011, 27, 4020–4028. [Google Scholar] [CrossRef]
- Sharma, S.; Kumar, K.; Thakur, N.; Chauhan, S.; Chauhan, M.S. The effect of shape and size of ZnO nanoparticles on their antimicrobial and photocatalytic activities: A green approach. Bull. Mater. Sci. 2019, 43, 20. [Google Scholar] [CrossRef]
- Jin, S.E.; Jin, J.E.; Hwang, W.; Hong, S.W. Photocatalytic antibacterial application of zinc oxide nanoparticles and self-assembled networks under dual UV irradiation for enhanced disinfection. Int. J. Nanomed. 2019, 14, 1737–1751. [Google Scholar] [CrossRef] [Green Version]
- de Lucas-Gil, E.; Leret, P.; Monte-Serrano, M.; Reinosa, J.J.; Enríquez, E.; Del Campo, A.; Cañete, M.; Menéndez, J.; Fernández, J.F.; Rubio-Marcos, F. ZnO Nanoporous Spheres with Broad-Spectrum Antimicrobial Activity by Physicochemical Interactions. ACS Appl. Nano Mater. 2018, 1, 3214–3225. [Google Scholar] [CrossRef]
- Abo-Shama, U.H.; El-Gendy, H.; Mousa, W.S.; Hamouda, R.A.; Yousuf, W.E.; Hetta, H.F.; Abdeen, E.E. Synergistic and Antagonistic Effects of Metal Nanoparticles in Combination with Antibiotics Against Some Reference Strains of Pathogenic Microorganisms. Infect. Drug Resist. 2020, 13, 351–362. [Google Scholar] [CrossRef] [Green Version]
- Al-Hisnawi, M.S.; Jabor, M.A. Preparation of nanohybrid compound from the drugs (naproxen and cephalexin) with zinc oxide and studying biological activities against Aeromonas bacteria. J. Contemp. Med. Sci. 2016, 1, 16–19. [Google Scholar]
- Bian, Z.; Tachikawa, T.; Zhang, P.; Fujitsuka, M.; Majima, T. A nanocomposite superstructure of metal oxides with effective charge transfer interfaces. Nat. Commun. 2014, 5, 3038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shanmugam, N.R.; Muthukumar, S.; Prasad, S. A review on ZnO-based electrical biosensors for cardiac biomarker detection. Future Sci. OA 2017, 3, FSO196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stankic, S.; Suman, S.; Haque, F.; Vidic, J. Pure and multi metal oxide nanoparticles: Synthesis, antibacterial and cytotoxic properties. J. Nanobiotechnol. 2016, 14, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giannossa, L.; Longano, D.; Ditaranto, N.; Nitti, M.; Paladini, F.; Pollini, M.; Rai, M.; Sannino, A.; Valentini, A.; Cioffi, N. Metal nanoantimicrobials for textile applications. Nanotechnol. Rev. 2013, 2. [Google Scholar] [CrossRef]
- González-Henríquez, C.M.; Sarabia-Vallejos, M.A.; Rodriguez-Hernandez, J. Advances in the Fabrication of Antimicrobial Hydrogels for Biomedical Applications. Materials 2017, 10, 232. [Google Scholar] [CrossRef] [Green Version]
- Vijayakumar, S.; Saravanakumar, K.; Malaikozhundan, B.; Divya, M.; Vaseeharan, B.; Durán-Lara, E.F.; Wang, M.H. Biopolymer K-carrageenan wrapped ZnO nanoparticles as drug delivery vehicles for anti MRSA therapy. Int. J. Biol. Macromol. 2020, 144, 9–18. [Google Scholar] [CrossRef]
- Yadav, S.; Mehrotra, G.K.; Dutta, P.K. Chitosan based ZnO nanoparticles loaded gallic-acid films for active food packaging. Food Chem. 2021, 334, 127605. [Google Scholar] [CrossRef]
- Banerjee, D.; Shivapriya, P.M.; Gautam, P.K.; Misra, K.; Sahoo, A.K.; Samanta, S.K. A Review on Basic Biology of Bacterial Biofilm Infections and Their Treatments by Nanotechnology-Based Approaches. Proc. Natl. Acad. Sci. India Sect. B Biol. Sci. 2020, 90, 243–259. [Google Scholar] [CrossRef]
- Sharma, D.; Misba, L.; Khan, A.U. Antibiotics versus biofilm: An emerging battleground in microbial communities. Antimicrob. Resist. Infect. Control 2019, 8, 76. [Google Scholar] [CrossRef]
- Canta, M.; Cauda, V. The investigation of the parameters affecting the ZnO nanoparticle cytotoxicity behaviour: A tutorial review. Biomater. Sci. 2020, 8, 6157–6174. [Google Scholar] [CrossRef] [PubMed]
- Mu, Q.; David, C.A.; Galceran, J.; Rey-Castro, C.; Krzemiński, L.; Wallace, R.; Bamiduro, F.; Milne, S.J.; Hondow, N.S.; Brydson, R.; et al. Systematic investigation of the physicochemical factors that contribute to the toxicity of ZnO nanoparticles. Chem. Res. Toxicol. 2014, 27, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Pomastowski, P.; Król-Górniak, A.; Railean-Plugaru, V.; Buszewski, B. Zinc Oxide Nanocomposites—Extracellular Synthesis, Physicochemical Characterization and Antibacterial Potential. Materials 2020, 13, 4347. [Google Scholar] [CrossRef] [PubMed]
- Hao, N.; Zhang, M.; Zhang, J.X.J. Microfluidics for ZnO micro-/nanomaterials development: Rational design, controllable synthesis, and on-chip bioapplications. Biomater. Sci. 2020, 8, 1783–1801. [Google Scholar] [CrossRef]
- Nikam, A.V.; Prasad, B.L.V.; Kulkarni, A.A. Wet chemical synthesis of metal oxide nanoparticles: A review. CrystEngComm 2018, 20, 5091–5107. [Google Scholar] [CrossRef]
- Thakur, V.; Verma, U.P.; Rajaram, P. Wet chemical synthesis of ZnO nanocrystals: Dependence of growth and morphology on the solvent composition. J. Mater. Sci. Mater. Electron. 2014, 25, 3242–3250. [Google Scholar] [CrossRef]
- Bandeira, M.; Giovanela, M.; Roesch-Ely, M.; Devine, D.M.; da Silva Crespo, J. Green synthesis of zinc oxide nanoparticles: A review of the synthesis methodology and mechanism of formation. Sustain. Chem. Pharm. 2020, 15, 100223. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, X. Why microfluidics? Merits and trends in chemical synthesis. Lab Chip 2017, 17, 3960–3978. [Google Scholar] [CrossRef]
- Balucani, M.; Nenzi, P.; Chubenko, E.; Klyshko, A.; Bondarenko, V. Electrochemical and hydrothermal deposition of ZnO on silicon: From continuous films to nanocrystals. J. Nanopart. Res. 2011, 13, 5985–5997. [Google Scholar] [CrossRef]
- Kumar, M.; Sasikumar, C. Electrodeposition of Nanostructured ZnO Thin Film: A Review. Am. J. Mater. Sci. Eng. 2014, 2, 18–23. [Google Scholar] [CrossRef]
- Izzi, M.; Sportelli, M.C.; Ditaranto, N.; Picca, R.A.; Innocenti, M.; Sabbatini, L.; Cioffi, N. Pros and Cons of Sacrificial Anode Electrolysis for the Preparation of Transition Metal Colloids: A Review. ChemElectroChem 2020, 7, 386–394. [Google Scholar] [CrossRef]
- Dierstein, A.; Natter, H.; Meyer, F.; Stephan, H.O.; Kropf, C.; Hempelmann, R. Electrochemical deposition under oxidizing conditions (EDOC): A new synthesis for nanocrystalline metal oxides. Scr. Mater. 2001, 44, 2209–2212. [Google Scholar] [CrossRef]
- Natter, H.; Hempelmann, R. Tailor-made nanomaterials designed by electrochemical methods. Electrochim. Acta 2003, 49, 51–61. [Google Scholar] [CrossRef]
- Picca, R.A.; Sportelli, M.C.; Hötger, D.; Manoli, K.; Kranz, C.; Mizaikoff, B.; Torsi, L.; Cioffi, N. Electrosynthesis and characterization of ZnO nanoparticles as inorganic component in organic thin-film transistor active layers. Electrochim. Acta 2015, 178, 45–54. [Google Scholar] [CrossRef]
- Sportelli, M.C.; Picca, R.A.; Izzi, M.; Palazzo, G.; Gristina, R.; Innocenti, M.; Torsi, L.; Cioffi, N. ZnO Nanostructures with Antibacterial Properties Prepared by a Green Electrochemical-Thermal Approach. Nanomaterials 2020, 10, 473. [Google Scholar] [CrossRef] [Green Version]
- Jabeera, B.; Anirudhan, T.; Shibli, S.M.A. Nano zinc oxide for efficient activation of aluminium zinc alloy sacrificial anode. J. New Mater. Electrochem. Syst. 2005, 8, 291. [Google Scholar]
- Gupta, M.; Tomar, R.S.; Kaushik, S.; Mishra, R.K.; Sharma, D. Effective Antimicrobial Activity of Green ZnO Nano Particles of Catharanthus roseus. Front. Microbiol. 2018, 9. [Google Scholar] [CrossRef]
- Shanavas, S.; Duraimurugan, J.; Kumar, G.S.; Ramesh, R.; Acevedo, R.; Anbarasan, P.M.; Maadeswaran, P. Ecofriendly green synthesis of ZnO nanostructures using Artabotrys Hexapetalu and Bambusa Vulgaris plant extract and investigation on their photocatalytic and antibacterial activity. Mater. Res. Express 2019, 6, 105098. [Google Scholar] [CrossRef]
- Alamdari, S.; Sasani Ghamsari, M.; Lee, C.; Han, W.; Park, H.-H.; Tafreshi, M.J.; Afarideh, H.; Ara, M.H.M. Preparation and Characterization of Zinc Oxide Nanoparticles Using Leaf Extract of Sambucus ebulus. Appl. Sci. 2020, 10, 3620. [Google Scholar] [CrossRef]
- Bala, N.; Saha, S.; Chakraborty, M.; Maiti, M.; Das, S.; Basu, R.; Nandy, P. Green synthesis of zinc oxide nanoparticles using Hibiscus subdariffa leaf extract: Effect of temperature on synthesis, anti-bacterial activity and anti-diabetic activity. RSC Adv. 2015, 5, 4993–5003. [Google Scholar] [CrossRef]
- Borade, P.; Joshi, K.U.; Gokarna, A.; Lerondel, G.; Walke, P.; Late, D.; Jejurikar, S.M. Synthesis and self-assembly of dumbbell shaped ZnO sub-micron structures using low temperature chemical bath deposition technique. Mater. Chem. Phys. 2016, 169, 152–157. [Google Scholar] [CrossRef]
- Singh, J.; Juneja, S.; Palsaniya, S.; Manna, A.K.; Soni, R.K.; Bhattacharya, J. Evidence of oxygen defects mediated enhanced photocatalytic and antibacterial performance of ZnO nanorods. Colloids Surf. B Biointerfaces 2019, 184, 110541. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Arshi, N.; Jeong, Y.S.; Anwar, M.S.; Dwivedi, S.; Alsharaeh, E.; Koo, B.H. Novel Biomimatic Synthesis of ZnO Nanorods Using Egg White (Albumen) and Their Antibacterial Studies. J. Nanosci. Nanotechnol. 2016, 16, 5959–5965. [Google Scholar] [CrossRef] [PubMed]
- Elkady, M.F.; Shokry Hassan, H.; Hafez, E.E.; Fouad, A. Construction of Zinc Oxide into Different Morphological Structures to Be Utilized as Antimicrobial Agent against Multidrug Resistant Bacteria. Bioinorg. Chem. Appl. 2015, 2015, 536854. [Google Scholar] [CrossRef] [Green Version]
- de Dicastillo, C.L.; Vidal, C.P.; Falcó, I.; Sánchez, G.; Márquez, P.; Escrig, J. Antimicrobial Bilayer Nanocomposites Based on the Incorporation of As-Synthetized Hollow Zinc Oxide Nanotubes. Nanomaterials 2020, 10, 503. [Google Scholar] [CrossRef] [Green Version]
- Chandra, H.; Patel, D.; Kumari, P.; Jangwan, J.S.; Yadav, S. Phyto-mediated synthesis of zinc oxide nanoparticles of Berberis aristata: Characterization, antioxidant activity and antibacterial activity with special reference to urinary tract pathogens. Mater. Sci. Eng. C 2019, 102, 212–220. [Google Scholar] [CrossRef]
- Ali, A.; Ambreen, S.; Javed, R.; Tabassum, S.; ul Haq, I.; Zia, M. ZnO nanostructure fabrication in different solvents transforms physio-chemical, biological and photodegradable properties. Mater. Sci. Eng. C 2017, 74, 137–145. [Google Scholar] [CrossRef]
- Pasquet, J.; Chevalier, Y.; Couval, E.; Bouvier, D.; Noizet, G.; Morlière, C.; Bolzinger, M.-A. Antimicrobial activity of zinc oxide particles on five micro-organisms of the Challenge Tests related to their physicochemical properties. Int. J. Pharm. 2014, 460, 92–100. [Google Scholar] [CrossRef]
- Khan, M.F.; Hameedullah, M.; Ansari, A.H.; Ahmad, E.; Lohani, M.B.; Khan, R.H.; Alam, M.M.; Khan, W.; Husain, F.M.; Ahmad, I. Flower-shaped ZnO nanoparticles synthesized by a novel approach at near-room temperatures with antibacterial and antifungal properties. Int. J. Nanomed. 2014, 9, 853–864. [Google Scholar] [CrossRef]
- Quek, J.A.; Lam, S.M.; Sin, J.C.; Mohamed, A.R. Visible light responsive flower-like ZnO in photocatalytic antibacterial mechanism towards Enterococcus faecalis and Micrococcus luteus. J. Photochem. Photobiol. B Biol. 2018, 187, 66–75. [Google Scholar] [CrossRef]
- Talebian, N.; Amininezhad, S.M.; Doudi, M. Controllable synthesis of ZnO nanoparticles and their morphology-dependent antibacterial and optical properties. J. Photochem. Photobiol. B Biol. 2013, 120, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Mousa, M.; Khairy, M. Synthesis of nano-zinc oxide with different morphologies and its application on fabrics for UV protection and microbe-resistant defense clothing. Text. Res. J. 2020, 90, 2492–2503. [Google Scholar] [CrossRef]
- Mahalakshmi, S.; Hema, N.; Vijaya, P.P. In Vitro Biocompatibility and Antimicrobial activities of Zinc Oxide Nanoparticles (ZnO NPs) Prepared by Chemical and Green Synthetic Route—A Comparative Study. BioNanoScience 2020, 10, 112–121. [Google Scholar] [CrossRef]
- Auría-Soro, C.; Nesma, T.; Juanes-Velasco, P.; Landeira-Viñuela, A.; Fidalgo-Gomez, H.; Acebes-Fernandez, V.; Gongora, R.; Almendral Parra, M.J.; Manzano-Roman, R.; Fuentes, M.; et al. Interactions of Nanoparticles and Biosystems: Microenvironment of Nanoparticles and Biomolecules in Nanomedicine. Nanomaterials 2019, 9, 1365. [Google Scholar]
- Gharpure, S.; Ankamwar, B. Synthesis and Antimicrobial Properties of Zinc Oxide Nanoparticles. J. Nanosci. Nanotechnol. 2020, 20, 5977–5996. [Google Scholar] [CrossRef]
- Espitia, P.J.P.; Soares, N.d.F.F.; Coimbra, J.S.d.R.; de Andrade, N.J.; Cruz, R.S.; Medeiros, E.A.A. Zinc Oxide Nanoparticles: Synthesis, Antimicrobial Activity and Food Packaging Applications. Food Bioprocess Technol. 2012, 5, 1447–1464. [Google Scholar] [CrossRef]
- Cheeseman, S.; Christofferson, A.J.; Kariuki, R.; Cozzolino, D.; Daeneke, T.; Crawford, R.J.; Truong, V.K.; Chapman, J.; Elbourne, A. Antimicrobial Metal Nanomaterials: From Passive to Stimuli-Activated Applications. Adv. Sci. 2020, 7, 1902913. [Google Scholar] [CrossRef] [Green Version]
- Lemire, J.A.; Harrison, J.J.; Turner, R.J. Antimicrobial activity of metals: Mechanisms, molecular targets and applications. Nat. Rev. Microbiol. 2013, 11, 371–384. [Google Scholar] [CrossRef]
- Ali, A.; Phull, A.-R.; Zia, M. Elemental zinc to zinc nanoparticles: Is ZnO NPs crucial for life? Synthesis, toxicological, and environmental concerns. Nanotechnol. Rev. 2018, 7, 413. [Google Scholar] [CrossRef]
- Pasquet, J.; Chevalier, Y.; Pelletier, J.; Couval, E.; Bouvier, D.; Bolzinger, M.-A. The contribution of zinc ions to the antimicrobial activity of zinc oxide. Colloids Surf. A Physicochem. Eng. Asp. 2014, 457, 263–274. [Google Scholar] [CrossRef]
- Adhikari, S.; Gupta, R.; Surin, A.; Kumar, T.S.; Chakraborty, S.; Sarkar, D.; Madras, G. Visible light assisted improved photocatalytic activity of combustion synthesized spongy-ZnO towards dye degradation and bacterial inactivation. RSC Adv. 2016, 6, 80086–80098. [Google Scholar] [CrossRef]
- Kaliraj, L.; Ahn, J.C.; Rupa, E.J.; Abid, S.; Lu, J.; Yang, D.C. Synthesis of panos extract mediated ZnO nano-flowers as photocatalyst for industrial dye degradation by UV illumination. J. Photochem. Photobiol. B Biol. 2019, 199, 111588. [Google Scholar] [CrossRef] [PubMed]
- Hajipour, M.J.; Fromm, K.M.; Akbar Ashkarran, A.; de Aberasturi, D.J.; Larramendi, I.R.d.; Rojo, T.; Serpooshan, V.; Parak, W.J.; Mahmoudi, M. Antibacterial properties of nanoparticles. Trends Biotechnol. 2012, 30, 499–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lakshmi Prasanna, V.; Vijayaraghavan, R. Insight into the Mechanism of Antibacterial Activity of ZnO: Surface Defects Mediated Reactive Oxygen Species Even in the Dark. Langmuir 2015, 31, 9155–9162. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Fu, Z.-Y.; Su, B.-L. Hierarchically Structured Porous Materials for Energy Conversion and Storage. Adv. Funct. Mater. 2012, 22, 4634–4667. [Google Scholar] [CrossRef]
- Picone, A.; Riva, M.; Brambilla, A.; Calloni, A.; Bussetti, G.; Finazzi, M.; Ciccacci, F.; Duò, L. Reactive metal–oxide interfaces: A microscopic view. Surf. Sci. Rep. 2016, 71, 32–76. [Google Scholar] [CrossRef]
- Eleraky, N.E.; Allam, A.; Hassan, S.B.; Omar, M.M. Nanomedicine Fight against Antibacterial Resistance: An Overview of the Recent Pharmaceutical Innovations. Pharmaceutics 2020, 12, 142. [Google Scholar] [CrossRef] [Green Version]
- Wahid, F.; Zhong, C.; Wang, H.S.; Hu, X.H.; Chu, L.Q. Recent Advances in Antimicrobial Hydrogels Containing Metal Ions and Metals/Metal Oxide Nanoparticles. Polymers 2017, 9. [Google Scholar] [CrossRef] [Green Version]
- Farzana, R.; Iqra, P.; Shafaq, F.; Sumaira, S.; Zkia, K.; Hunaiza, T.; Husna, M. Antimicrobial Behavior of Zinc Oxide Nanoparticles and β-Lactam Antibiotics against Pathogenic Bacteria. Arch. Clin. Microbiol. 2017, 8, 57. [Google Scholar]
- Azizi-Lalabadi, M.; Ehsani, A.; Divband, B.; Alizadeh-Sani, M. Antimicrobial activity of Titanium dioxide and Zinc oxide nanoparticles supported in 4A zeolite and evaluation the morphological characteristic. Sci. Rep. 2019, 9, 17439. [Google Scholar] [CrossRef] [Green Version]
- Bednář, J.; Svoboda, L.; Rybková, Z.; Dvorský, R.; Malachová, K.; Stachurová, T.; Matýsek, D.; Foldyna, V. Antimicrobial Synergistic Effect Between Ag and Zn in Ag-ZnO·mSiO2 Silicate Composite with High Specific Surface Area. Nanomaterials 2019, 9, 1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Nabulsi, A.; Osaili, T.; Sawalha, A.; Olaimat, A.N.; Albiss, B.A.; Mehyar, G.; Ayyash, M.; Holley, R. Antimicrobial activity of chitosan coating containing ZnO nanoparticles against E. coli O157:H7 on the surface of white brined cheese. Int. J. Food Microbiol. 2020, 334, 108838. [Google Scholar] [CrossRef] [PubMed]
- Turlybekuly, A.; Pogrebnjak, A.D.; Sukhodub, L.F.; Sukhodub, L.B.; Kistaubayeva, A.S.; Savitskaya, I.S.; Shokatayeva, D.H.; Bondar, O.V.; Shaimardanov, Z.K.; Plotnikov, S.V.; et al. Synthesis, characterization, in vitro biocompatibility and antibacterial properties study of nanocomposite materials based on hydroxyapatite-biphasic ZnO micro- and nanoparticles embedded in Alginate matrix. Mater. Sci. Eng. C 2019, 104, 109965. [Google Scholar] [CrossRef] [PubMed]
- Kulshrestha, S.; Khan, S.; Meena, R.; Singh, B.R.; Khan, A.U. A graphene/zinc oxide nanocomposite film protects dental implant surfaces against cariogenic Streptococcus mutans. Biofouling 2014, 30, 1281–1294. [Google Scholar] [CrossRef] [PubMed]
- Oves, M.; Rauf, M.A.; Ansari, M.O.; Aslam Parwaz Khan, A.; Qari, H.A.; Alajmi, M.F.; Sau, S.; Iyer, A.K. Graphene Decorated Zinc Oxide and Curcumin to Disinfect the Methicillin-Resistant Staphylococcus aureus. Nanomaterials 2020, 10, 1004. [Google Scholar] [CrossRef]
- Dharmalingam, P.; Jp, P.; Sundararajan, V.; Veluswamy, P.; Chelliah, R.; Samal, D.; Oh, D.-H.; Sahabudeen, S.M.; Venkatasubbu, D. Mechanism of inhibition of graphene oxide/zinc oxide nanocomposite against wound infection causing pathogens. Appl. Nanosci. 2019, 10. [Google Scholar] [CrossRef]
- Wang, Y.-W.; Cao, A.; Jiang, Y.; Zhang, X.; Liu, J.-H.; Liu, Y.; Wang, H. Superior Antibacterial Activity of Zinc Oxide/Graphene Oxide Composites Originating from High Zinc Concentration Localized around Bacteria. ACS Appl. Mater. Interfaces 2014, 6, 2791–2798. [Google Scholar] [CrossRef]
- Valenzuela, L.; Iglesias-Juez, A.; Bachiller-Baeza, B.; Faraldos, M.; Bahamonde, A.; Rosal, R. Biocide mechanism of highly efficient and stable antimicrobial surfaces based on zinc oxide–reduced graphene oxide photocatalytic coatings. J. Mater. Chem. B 2020, 8, 8294–8304. [Google Scholar] [CrossRef]
- Fakhroueian, Z.; Harsini, F.; Chalabian, F.; Katouzian, F.; Shafiekhani, A.; Esmaeilzadeh, P. Influence of Modified ZnO Quantum Dots and Nanostructures as New Antibacterials. Adv. Nanopart. 2013, 2, 247–258. [Google Scholar] [CrossRef] [Green Version]
- Singh, A.K.; Pal, P.; Gupta, V.; Yadav, T.P.; Gupta, V.; Singh, S.P. Green synthesis, characterization and antimicrobial activity of zinc oxide quantum dots using Eclipta alba. Mater. Chem. Phys. 2018, 203, 40–48. [Google Scholar] [CrossRef]
- Kumar, S.; Mudai, A.; Roy, B.; Basumatary, I.B.; Mukherjee, A.; Dutta, J. Biodegradable Hybrid Nanocomposite of Chitosan/Gelatin and Green Synthesized Zinc Oxide Nanoparticles for Food Packaging. Foods 2020, 9, 1143. [Google Scholar] [CrossRef] [PubMed]
- Madhumitha, G.; Elango, G.; Roopan, S.M. Biotechnological aspects of ZnO nanoparticles: Overview on synthesis and its applications. Appl. Microbiol. Biotechnol. 2016, 100, 571–581. [Google Scholar] [CrossRef] [PubMed]
- Gold, K.; Slay, B.; Knackstedt, M.; Gaharwar, A.K. Antimicrobial Activity of Metal and Metal-Oxide Based Nanoparticles. Adv. Ther. 2018, 1, 1700033. [Google Scholar] [CrossRef]
- Melchionna, M.; Prato, M.; Fornasiero, P. Mix and match metal oxides and nanocarbons for new photocatalytic frontiers. Catal. Today 2016. [Google Scholar] [CrossRef]
- Agelidis, A.; Koujah, L.; Suryawanshi, R.; Yadavalli, T.; Mishra, Y.K.; Adelung, R.; Shukla, D. An Intra-Vaginal Zinc Oxide Tetrapod Nanoparticles (ZOTEN) and Genital Herpesvirus Cocktail Can Provide a Novel Platform for Live Virus Vaccine. Front. Immunol. 2019, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kadiyala, U.; Turali-Emre, E.S.; Bahng, J.H.; Kotov, N.A.; VanEpps, J.S. Unexpected insights into antibacterial activity of zinc oxide nanoparticles against methicillin resistant Staphylococcus aureus (MRSA). Nanoscale 2018, 10, 4927–4939. [Google Scholar] [CrossRef] [PubMed]
- Rago, I.; Chandraiahgari, C.R.; Bracciale, M.P.; De Bellis, G.; Zanni, E.; Cestelli Guidi, M.; Sali, D.; Broggi, A.; Palleschi, C.; Sarto, M.S.; et al. Zinc oxide microrods and nanorods: Different antibacterial activity and their mode of action against Gram-positive bacteria. RSC Adv. 2014, 4, 56031–56040. [Google Scholar] [CrossRef]
- Yi, G.-C.; Wang, C.; Park, W. ZnO Nanorods: Synthesis, Characterization and Applications. Semicond. Sci. Technol. 2005, 20, 22–34. [Google Scholar] [CrossRef]
- Reddy, L.S.; Nisha, M.M.; Joice, M.; Shilpa, P.N. Antimicrobial activity of zinc oxide (ZnO) nanoparticle against Klebsiella pneumoniae. Pharm. Biol. 2014, 52, 1388–1397. [Google Scholar] [CrossRef]
- Taghizadeh, S.-M.; Lal, N.; Ebrahiminezhad, A.; Moeini, F.; Seifan, M.; Ghasemi, Y.; Berenjian, A. Green and Economic Fabrication of Zinc Oxide (ZnO) Nanorods as a Broadband UV Blocker and Antimicrobial Agent. Nanomaterials 2020, 10, 530. [Google Scholar] [CrossRef] [Green Version]
- Sharma, S.; Naik, D.; Agarwala, V. Synthesis, Characterization and Antibacterial Activity of ZnO Nanoparticles of Different Morphology. Adv. Mater. Res. 2012, 585, 154–158. [Google Scholar] [CrossRef]
- Ali, S.G.; Ansari, M.A.; Alzohairy, M.A.; Alomary, M.N.; Jalal, M.; AlYahya, S.; Asiri, S.M.M.; Khan, H.M. Effect of Biosynthesized ZnO Nanoparticles on Multi-Drug Resistant Pseudomonas Aeruginosa. Antibiotics 2020, 9, 260. [Google Scholar] [CrossRef] [PubMed]
- Mishra, Y.K.; Modi, G.; Cretu, V.; Postica, V.; Lupan, O.; Reimer, T.; Paulowicz, I.; Hrkac, V.; Benecke, W.; Kienle, L.; et al. Direct Growth of Freestanding ZnO Tetrapod Networks for Multifunctional Applications in Photocatalysis, UV Photodetection, and Gas Sensing. ACS Appl. Mater. Interfaces 2015, 7, 14303–14316. [Google Scholar] [CrossRef] [PubMed]
- Jeyabharathi, S.; Mahalakshmi, R.; Chandramohan, S.; Naveenkumar, S.; Sundar, K.; Muthukumaran, A. Self-assembled hollow ZnO nano and micro donut shape by starch and its antimicrobial potentials. Mater. Lett. 2020, 275, 128128. [Google Scholar] [CrossRef]
- Ashajyothi, C.; Harish, K.H.; Dubey, N.; Chandrakanth, R.K. Antibiofilm activity of biogenic copper and zinc oxide nanoparticles-antimicrobials collegiate against multiple drug resistant bacteria: A nanoscale approach. J. Nanostruct. Chem. 2016, 6, 329–341. [Google Scholar] [CrossRef] [Green Version]
- Sharma, N.; Singh, V.; Pandey, A.K.; Mishra, B.N.; Kulsoom, M.; Dasgupta, N.; Khan, S.; El-Enshasy, H.A.; Haque, S. Preparation and Evaluation of the ZnO NP–Ampicillin/Sulbactam Nanoantibiotic: Optimization of Formulation Variables Using RSM Coupled GA Method and Antibacterial Activities. Biomolecules 2019, 9, 764. [Google Scholar] [CrossRef] [Green Version]
- Eftekhar, B.; Moghimipour, E.; Jahandideh, P.P.; Jalali, S.; Mahmoudian, M. Analgesic effect of odontopaste and a compound intracanal medicament between root canal therapy appointments. Jundishapur J. Nat. Pharm. Prod. 2013, 8, 169–174. [Google Scholar] [CrossRef] [Green Version]
- Koch, T.; Peutzfeldt, A.; Malinovskii, V.; Flury, S.; Häner, R.; Lussi, A. Temporary zinc oxide-eugenol cement: Eugenol quantity in dentin and bond strength of resin composite. Eur. J. Oral Sci. 2013, 121, 363–369. [Google Scholar] [CrossRef]
- Panzarini, S.R.; Trevisan, C.L.; Brandini, D.A.; Poi, W.R.; Sonoda, C.K.; Luvizuto, E.R.; Dos Santos, C.L. Intracanal dressing and root canal filling materials in tooth replantation: A literature review. Dent. Traumatol. 2012, 28, 42–48. [Google Scholar] [CrossRef]
- Ghorbani, M.; Nezhad-Mokhtari, P.; Ramazani, S. Aloe vera-loaded nanofibrous scaffold based on Zein/Polycaprolactone/Collagen for wound healing. Int. J. Biol. Macromol. 2020, 153, 921–930. [Google Scholar] [CrossRef]
- Hamdan, S.; Pastar, I.; Drakulich, S.; Dikici, E.; Tomic-Canic, M.; Deo, S.; Daunert, S. Nanotechnology-Driven Therapeutic Interventions in Wound Healing: Potential Uses and Applications. ACS Cent. Sci. 2017, 3, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Ramya, R.; Venkatesan, J.; Kim, S.; Sudha, P.N. Biomedical Applications of Chitosan: An Overview. J. Biomater. Tissue Eng. 2012, 2, 100–111. [Google Scholar] [CrossRef]
- Sahariah, P.; Másson, M. Antimicrobial Chitosan and Chitosan Derivatives: A Review of the Structure–Activity Relationship. Biomacromolecules 2017, 18, 3846–3868. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xia, W.; Liu, P.; Cheng, Q.; Tahirou, T.; Gu, W.; Li, B. Chitosan Modification and Pharmaceutical/Biomedical Applications. Mar. Drugs 2010, 8, 1962–1987. [Google Scholar] [CrossRef] [Green Version]
- Donnadio, A.; Cardinali, G.; Latterini, L.; Roscini, L.; Ambrogi, V. Nanostructured zinc oxide on silica surface: Preparation, physicochemical characterization and antimicrobial activity. Mater. Sci. Eng. C 2019, 104, 109977. [Google Scholar] [CrossRef]
- Mousavi, S.A.; Ghotaslou, R.; Khorramdel, A.; Akbarzadeh, A.; Aeinfar, A. Antibacterial and antifungal impacts of combined silver, zinc oxide, and chitosan nanoparticles within tissue conditioners of complete dentures in vitro. Ir. J. Med Sci. 2020. [Google Scholar] [CrossRef]
- Qiu, S.; Zhou, H.; Shen, Z.; Hao, L.; Chen, H.; Zhou, X. Synthesis, characterization, and comparison of antibacterial effects and elucidating the mechanism of ZnO, CuO and CuZnO nanoparticles supported on mesoporous silica SBA-3. RSC Adv. 2020, 10, 2767–2785. [Google Scholar] [CrossRef]
- Sophee, S.; Prasad, V.; Srinivas, J.; Aparna, R.; Phani, A. Antibacterial Activity of TiO2 and ZnO Microparticles Combination on Water Polluting Bacteria. J. Green Sci. Technol. 2013, 1. [Google Scholar] [CrossRef]
- Predoi, D.; Iconaru, S.L.; Predoi, M.V.; Stan, G.E.; Buton, N. Synthesis, Characterization, and Antimicrobial Activity of Magnesium-Doped Hydroxyapatite Suspensions. Nanomaterials 2019, 9, 1295. [Google Scholar] [CrossRef] [Green Version]
- Jose, A.; Sunaja Devi, K.R.; Pinheiro, D.; Lakshmi Narayana, S. Electrochemical synthesis, photodegradation and antibacterial properties of PEG capped zinc oxide nanoparticles. J. Photochem. Photobiol. B Biol. 2018, 187, 25–34. [Google Scholar] [CrossRef]
- Mocanu, A.; Isopencu, G.; Busuioc, C.; Popa, O.-M.; Dietrich, P.; Socaciu-Siebert, L. Bacterial cellulose films with ZnO nanoparticles and propolis extracts: Synergistic antimicrobial effect. Sci. Rep. 2019, 9, 17687. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.-W.; Guo, C.-R.; Hu, Y.-Z.; Guo, Y.-R.; Pan, Q.-J. The preparation and antibacterial activity of cellulose/ZnO composite: A review. Open Chem. 2018, 16, 9. [Google Scholar] [CrossRef]
- Hewlings, S.J.; Kalman, D.S. Curcumin: A Review of Its Effects on Human Health. Foods 2017, 6, 92. [Google Scholar] [CrossRef] [PubMed]
- Perera, W.P.T.D.; Dissanayake, R.K.; Ranatunga, U.I.; Hettiarachchi, N.M.; Perera, K.D.C.; Unagolla, J.M.; De Silva, R.T.; Pahalagedara, L.R. Curcumin loaded zinc oxide nanoparticles for activity-enhanced antibacterial and anticancer applications. RSC Adv. 2020, 10, 30785–30795. [Google Scholar] [CrossRef]
- Teh, S.J.; Yeoh, S.L.; Lee, K.M.; Lai, C.W.; Abdul Hamid, S.B.; Thong, K.L. Effect of reduced graphene oxide-hybridized ZnO thin films on the photoinactivation of Staphylococcus aureus and Salmonella enterica serovar Typhi. J. Photochem. Photobiol. B Biol. 2016, 161, 25–33. [Google Scholar] [CrossRef]
- Bajpai, S.K.; Thomas, V.; Bajpai, M. Novel Strategy for Synthesis of ZnO Microparticles Loaded Cotton Fabrics and Investigation of their Antibacterial Properties. J. Eng. Fibers Fabr. 2011, 6, 155892501100600310. [Google Scholar] [CrossRef] [Green Version]
- Noman, M.T.; Petrů, M. Functional Properties of Sonochemically Synthesized Zinc Oxide Nanoparticles and Cotton Composites. Nanomaterials 2020, 10, 1661. [Google Scholar] [CrossRef]
- Salat, M.; Petkova, P.; Hoyo, J.; Perelshtein, I.; Gedanken, A.; Tzanov, T. Durable antimicrobial cotton textiles coated sonochemically with ZnO nanoparticles embedded in an in-situ enzymatically generated bioadhesive. Carbohydr. Polym. 2018, 189, 198–203. [Google Scholar] [CrossRef]
- Subash, A.A.; Chandramouli, K.V.; Ramachandran, T.; Rajendran, R.; Muthusamy, M. Preparation, characterization, and functional analysis of zinc oxide nanoparticle-coated cotton fabric for antibacterial efficacy. J. Text. Inst. 2012, 103, 298–303. [Google Scholar] [CrossRef]
- Yilmaz Atay, H. Antibacterial Activity of Chitosan-Based Systems. Funct. Chitosan 2020. [Google Scholar] [CrossRef]
- Jaros, J.; Wilson, C.; Shi, V.Y. Fabric Selection in Atopic Dermatitis: An Evidence-Based Review. Am. J. Clin. Dermatol. 2020, 21, 467–482. [Google Scholar] [CrossRef] [PubMed]
- Perinelli, D.R.; Fagioli, L.; Campana, R.; Lam, J.K.W.; Baffone, W.; Palmieri, G.F.; Casettari, L.; Bonacucina, G. Chitosan-based nanosystems and their exploited antimicrobial activity. Eur. J. Pharm. Sci. 2018, 117, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Tanpichai, S.; Witayakran, S.; Wootthikanokkhan, J.; Srimarut, Y.; Woraprayote, W.; Malila, Y. Mechanical and antibacterial properties of the chitosan coated cellulose paper for packaging applications: Effects of molecular weight types and concentrations of chitosan. Int. J. Biol. Macromol. 2020, 155, 1510–1519. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Qian, J.; Ding, F. Emerging Chitosan-Based Films for Food Packaging Applications. J. Agric. Food Chem. 2018, 66, 395–413. [Google Scholar] [CrossRef]
- Marpu, S.B.; Benton, E.N. Shining Light on Chitosan: A Review on the Usage of Chitosan for Photonics and Nanomaterials Research. Int. J. Mol. Sci. 2018, 19, 1795. [Google Scholar] [CrossRef] [Green Version]
- Karahaliloglu, Z.; Kilicay, E.; Denkbas, E.B. Antibacterial chitosan/silk sericin 3D porous scaffolds as a wound dressing material. Artif. Cells Nanomed. Biotechnol. 2017, 45, 1172–1185. [Google Scholar] [CrossRef] [Green Version]
- Javed, R.; Rais, F.; Fatima, H.; Haq, I.U.; Kaleem, M.; Naz, S.S.; Ao, Q. Chitosan encapsulated ZnO nanocomposites: Fabrication, characterization, and functionalization of bio-dental approaches. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 116, 111184. [Google Scholar] [CrossRef]
- Morais, D.S.; Guedes, R.M.; Lopes, M.A. Antimicrobial Approaches for Textiles: From Research to Market. Materials 2016, 9, 498. [Google Scholar] [CrossRef]
- Rajendiran, K.; Zhao, Z.; Pei, D.-S.; Fu, A. Antimicrobial Activity and Mechanism of Functionalized Quantum Dots. Polymers 2019, 11, 1670. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.-Y.; Xiong, H.-M. Photoluminescent ZnO Nanoparticles and Their Biological Applications. Materials 2015, 8, 3101–3127. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, M.; Li, B.; Chen, D.; Dong, X.; Wang, Y.; Gu, Y. Versatile antimicrobial peptide-based ZnO quantum dots for in vivo bacteria diagnosis and treatment with high specificity. Biomaterials 2015, 53, 532–544. [Google Scholar] [CrossRef] [PubMed]
- Jin, T.; Sun, D.; Su, J.Y.; Zhang, H.; Sue, H.J. Antimicrobial efficacy of zinc oxide quantum dots against Listeria monocytogenes, Salmonella Enteritidis, and Escherichia coli O157:H7. J. Food Sci. 2009, 74, M46–M52. [Google Scholar] [CrossRef] [PubMed]
- Gabros, S.; Nessel, T.A.; Zito, P.M. Sunscreens and Photoprotection; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- Gao, A.L.; Cole, J.G.; Woolsey, Z.T.; Stoecker, W.V. Structured zinc oxide dressing for secondary intention wounds. J. Wound Care 2017, 26, S30–S36. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Han, Y.; Cui, M.; Tey, H.L.; Wang, L.; Xu, C. ZnO nanoparticles as an antimicrobial tissue adhesive for skin wound closure. J. Mater. Chem. B 2017, 5, 4535–4541. [Google Scholar] [CrossRef]
- Memarzadeh, K.; Sharili, A.S.; Huang, J.; Rawlinson, S.C.; Allaker, R.P. Nanoparticulate zinc oxide as a coating material for orthopedic and dental implants. J. Biomed. Mater. Res. Part A 2015, 103, 981–989. [Google Scholar] [CrossRef]
- Suozzi, K.; Turban, J.; Girardi, M. Cutaneous Photoprotection: A Review of the Current Status and Evolving Strategies. Yale J. Biol. Med. 2020, 93, 55–67. [Google Scholar]
- Thompson, C.B.; Wiemken, T.L.; Brown, T.S. Effect of Postoperative Dressing on Excisions Performed on the Leg: A Comparison Between Zinc Oxide Compression Dressings Versus Standard Wound Care. Dermatol. Surg. 2017, 43, 1379–1384. [Google Scholar] [CrossRef]
- Bae, J.Y.; Park, S.N. Evaluation of anti-microbial activities of ZnO, citric acid and a mixture of both against Propionibacterium acnes. Int. J. Cosmet. Sci. 2016, 38, 550–557. [Google Scholar] [CrossRef]
- Cervantes, J.; Eber, A.E.; Perper, M.; Nascimento, V.M.; Nouri, K.; Keri, J.E. The role of zinc in the treatment of acne: A review of the literature. Dermatol. Ther. 2018, 31. [Google Scholar] [CrossRef]
- Chuang, H.-C.; Yang, Y.-T.; Chen, H.-C.; Hwang, Y.-H.; Wu, K.-Y.; Chen, T.-F.; Chen, C.-L.; Jhan, M.-K.; Cheng, T.-J. Acute Effects of Pulmonary Exposure to Zinc Oxide Nanoparticles on the Brain in vivo. Aerosol Air Qual. Res. 2020. [Google Scholar] [CrossRef] [Green Version]
- Hadrup, N.; Rahmani, F.; Jacobsen, N.R.; Saber, A.T.; Jackson, P.; Bengtson, S.; Williams, A.; Wallin, H.; Halappanavar, S.; Vogel, U. Acute phase response and inflammation following pulmonary exposure to low doses of zinc oxide nanoparticles in mice. Nanotoxicology 2019, 13, 1275–1292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasmussen, K.; Rauscher, H.; Mech, A.; Riego Sintes, J.; Gilliland, D.; González, M.; Kearns, P.; Moss, K.; Visser, M.; Groenewold, M.; et al. Physico-chemical properties of manufactured nanomaterials—Characterisation and relevant methods. An outlook based on the OECD Testing Programme. Regul. Toxicol. Pharmacol. 2018, 92, 8–28. [Google Scholar] [CrossRef] [PubMed]
| Morphology | Particle Size | Porosity | Surface Area (m2/g) | Synthesis Method (Precursor) | Refs. |
|---|---|---|---|---|---|
| Spheres | 12 nm, 25 nm | Slit-like pores | 90.4, 42.8 |
| [16] |
| 62–94 nm | Not available | Not available |
| [47] | |
| 15–20 nm | Not available | Not available |
| [48] | |
| 25–30 nm (TEM); 65 ± 4 nm (dynamic light scattering) | Not available | Not available |
| [49] | |
| 12–46 nm | Not available | Not available |
| [50] | |
| Spheres in self-assembled network | 48.3 nm | Mesopores, 5–6.25 nm; macropores, 2–6 μm | Not available |
| [18] |
| Spheres in NP cluster | NPs-63 nm; cluster-590 nm | 34 nm | 20.72 |
| [19] |
| Dumbbells | Length 190–250 nm; breadth 50–60 nm | Not available | Not available |
| [50] |
| Nanorods | Length 523 nm; diameter 47 nm | Not available | 2.3 |
| [52] |
| Length ~2 μm; diameter ~50 nm | Not available | Not available |
| [53] | |
| Hollow nanotubes | Length ~500 nm | 53 nm (900 °C annealing), 114.6 nm (700 °C annealing), 255.4 nm (500 °C annealing), 278.6 nm (as-synthesized) | 2.4 (900 °C annealing), 7.2 (700 °C annealing), 16.7 (500 °C annealing), 17.8 (as-synthesized) |
| [54] |
| Length ~5 μm; thickness 59.5 nm | Internal diameter 178.2 nm | Not available |
| [55] | |
| Needles | Length ~2 μm; diameter 20–40 nm | Not available | Not available |
| [56] |
| Disks | 41 nm | Not available | Not available |
| [57] |
| Platelets | 14.7 nm, 17.5 nm; hydrodynamic environment- 6.4 μm, 5.0 μm | 17.3 nm, 11.6 nm | 39.0, 46.9 |
| [58] |
| Flowers | Length 200–500 nm; length 1–2 μm | Not available | Not available |
| [45] |
| 23.7–88.8 nm | Not available | Not available |
| [59] | |
| 700 nm–2.2 μm | Not available | Not available |
| [60] | |
| 45 nm | Not available | 28.8 |
| [61] | |
| Stars | 31 nm | Not available | Not available |
| [62] |
| Flakes | 32 nm | Not available | Not available |
| [63] |
| Materials | Synthesis Techniques (Precursor) | Material Description (Morphology/Particle Size) | Antimicrobial Activity Test Methods | Antimicrobial Activity against Pathogenic Microorganisms | Refs. |
|---|---|---|---|---|---|
| ZnO materials | |||||
| 0D structured ZnO NPs | Hydrothermal method or room temperature synthesis (zinc nitrate hexahydrate; zinc sulfate; zinc acetate dihydrate) | Spheres/12 nm, 25 nm; 30 nm, 88 nm, 142 nm, 212 nm, 307 nm | Turbidity | 6 mM, [Staphylococcus aureus] 30 nm: 10.11% growth; 88 nm: 54.34% growth; 142 nm: 78.12% growth; 212 nm: 79.79% growth; 307 nm: 96.67% growth, [Proteus vulgaris] 12 nm: 8.71% growth, [Salmonella typhimurium] 12 nm: 46.96% growth, [Shigella flexneri] 12 nm: 5.95% growth, [Bacillus cereus] 12 nm: 7.62% growth | [16] |
| Green method using Aloe vera leaf extract (zinc acetate dihydrate) |
| Well diffusion, broth microdilution; MIC | MIC, [E. coli] ZnO-1, ZnO-2, and ZnO-3: 1562 μg/mL; [S. aureus] ZnO-1: 781 μg/mL, ZnO-2 and ZnO-3: 391 μg/mL; [B. subtilis] ZnO-1 and ZnO-2: 391 μg/mL; ZnO-3: 195 μg/mL | [17] | |
| Precipitation method (zinc acetate dihydrate) | Nanopyramids/~15.4 nm in segments | Colony counting, serial dilution; MIC | [Methicillin-resistant S. aureus (MRSA)] MIC, 333 μg/mL (3 log (CFU/mL) inhibition at 800 μg/mL) | [96] | |
| Soft chemical synthesis (micrometric ZnO) | Spherical NP cluster/cluster-590 nm; NPs-63 nm | Colony counting | Antimicrobial activity value of log (control/sample), [E. coli] > 3.5; [S. aureus] > 3.5 | [19] | |
| 1D structured ZnO NPs | Hydrothermal method (zinc acetate dihydrate) | Hollow nanotubes/particle size ~500 nm in length; surface area 17.8 m2/g; average pore size, 278.6 nm | Disk diffusion; MIC | As-synthesized ZnO nanopowders, MIC, [Escherichia coli] 0.0585 mg/mL, [S. aureus] 0.234 mg/mL, [Pseudomonas aeruginosa] 0.234 mg/mL, [Bacillus subtilis] 0.938 mg/mL | [54] |
| Atomic layer deposition process over polymer template and template removal | Hollow nanotubes/length, ~5 μm; thickness, 59.5 nm; internal diameter, 178.2 nm | Colony counting | ZnO nanotubes at 1 wt% with acrylic polymer/extruded 32 μm-polyethylene (PE) substrate film coating [E. coli] 4.67 log reduction (cells/cm2), [S. aureus] 2.46 log reduction (cells/cm2) | [55] | |
| Precipitation method (zinc nitrate) | Nanorods/88.7 nm using 2-mercaptoethanol as a capping agent | Disk diffusion method, serial dilution; MIC | [Klebsiella pneumoniae] MIC, 40 μg/mL | [99] | |
| Green method using Chlorella vulgaris culture supernatant (zinc acetate dihydrate) | Nanorods/crystal size, 3.4 nm; length-150 nm; width-21 nm (aspect ratio of length to width 7.14) | Microdilution; MIC | [E. coli, P. aeruginosa, S. aureus] MIC, 250 μg/mL (excluding Enterococcus faecalis: resistant to ZnO nanorods) | [100] | |
| Sol–gel method (zinc nitrate hexahydrate) | Nanorods/500 nm–1 μm | Disk diffusion | [Capping agent: ethylenediamine] E. coli-inhibition, Micrococcus luteus-no inhibition, [Capping agent: citric acid monohydrate] E. coli-no inhibition, B. subtilis-inhibition | [101] | |
| 2D structured ZnO NPs | Not available (conventional products) |
| Disk diffusion, broth dilution; MIC | ZnO-1, ZnO-2, ZnO -3, MIC (wt%), [E. coli] 0.12, 0.18, 2.30; [S. aureus] 0.25, 0.30, 3.40; [P. aeruginosa] 1.28, 4.68, 5.70; [Candida albicans] >8; >8; >8; [Aspergillus brasiliensis] nil, nil, nil | [58] |
| 3D structured ZnO NP network | Sol–gel method (zinc acetylacetonate hydrate) | Spherical NP aggregate network/aggregates: ~3 μm; NPs: 48.3 nm | Colony counting; photocatalytic incubation | [E. coli] {Dual UV for 30 s} no particles-~approx. 2.8–3.0 log (CFU/mL), 0.05 mg/mL-no colonies detected | [18] |
| ZnO NP mixtures | Green method using Butea monsoperma seed extract (zinc nitrate hexahydrate) | Mixtures/25 nm | Broth dilution; MIC | [P. aeruginosa (resistant to amikacin (30 μg), cefepime (30 μg), sparfloxacin (5 μg), piperacillin (100 μg), levofloxacin (5 μg), piperacilin-tazobactum (100/10 μg), imipenem (10 μg), tobramycin (10 μg), nitrofurantoin (300 μg), and ceftazidime (30 μg))] MIC, 1600 μg/mL; 1600–3200 μg/mL for isolates from patients | [102] |
| ZnO MPs | Flame transport synthesis (zinc microparticles) | Tetrapods/~30 μm | Plaque assay | [Herpes simplex virus type-2 (HSV-2)] ZnO tetrapod NP and HSV-2 cocktail for live virus vaccine | [95,103] |
| Green method using starch (zinc acetate) | Self-assembled hollow microdonuts/1–2 μm | Disk diffusion | [Enterobacter aerogenes and Staphylococcus epidermidis] 0.5–5 mM | [104] | |
| Combinations of ZnO materials with drugs | |||||
| ZnO NPs with azithromycin, gentamicin, oxacillin, cefotaxime, cefuroxime, fosfomycin, chloramphenicol, and oxytetracycline | Green method using Ulva fasciata alga extract (zinc acetate dehydrate) | Flakes/length, ~200 nm | Disk diffusion; MIC |
| [20] |
| ZnO with cephalexin nanohybrids | Ion exchange via sol–gel method (ZnO, and 2,4-chlorophenoxyacetic acid) | Squeezed ZnO crystals/not available | Disk diffusion; MIC | ZnO with cephalexin nanohybrids: MIC, [Aeromonas spp.] 1 mg/mL | [21] |
| ZnO NPs with β-lactam antibiotics (ciprofloxacin and imipenem) | Not available (conventional product) | Not available | Disk diffusion; agar dilution; MIC | MIC
| [79] |
| ZnO NPs with ceftriaxone (CFX-ZnO NPs), ceftazidime (CFZ-ZnO NPs), and gentamicin (GTM-ZnO NPs) | Green method using Enterococcus faecalis culture supernatant (zinc sulfate) | Spheres/15.3–37 nm | Broth dilution; MIC |
| [105] |
| ZnO NPs with ampicillin/sulbactam | Milling method (zinc chloride) | Not available/25 nm | Disk diffusion; broth dilution; MIC | MIC,
| [106] |
| Combinations of ZnO materials with other metal oxide NPs/MPs, or metal doping | |||||
| ZnO NPs with TiO2 NPs in 4A zeolite | Ion exchange process (zinc acetate dehydrate) | Cubes/400–600 nm (NPs: spheres, ~50 nm) | Disk diffusion; MIC | MIC, [E. coli O157:H7] 1 mg/mL, [S. aureus] 2 mg/mL, [Pseudomonas fluorescens] 1 mg/mL, [Listeria Monocytogenes] 2 mg/mL | [80] |
| Ag-ZnOmSiO2 composites | Precipitation of sodium water glass in zinc acetate solution (zinc acetate dihydrate) | Lamellar porous nanostructure with silver spots/not available (specific surface area, 250 m2/g) | Microdilution; MIC | MIC, [E. coli] 2.9 mg/cm3, [P. aeruginosa] 3.9 mg/cm3, [Streptococcus salivarius] 5.9 mg/cm3, [S. aureus] 5.9 mg/cm3, [C. albicans] 23.5 mg/cm3—synergistic | [81] |
| ZnO-SiO2 composites | Solid state mixing (zinc acetate dihydrate) |
| Broth microdilution; MIC | MIC, [S. aureus] 2 mg/mL (except for ZnO/S-S-20, C-A-10, or C-A-20, >2) as 0.228–0.632 mg/mL of ZnO NPs, [C. albicans] 1 or 2 mg/mL (except for ZnO/S-A-10 or S-S-10 >2) as 0.187–0.632 mg/mL of ZnO NPs | [115] |
| CuZnO NPs on mesoporous silica SBA-3 | Co-condensation method (zinc nitrate) |
| Colony counting; MIC | MIC, [E. coli] 25 mg/mL (CuZnO, 0.558 mg/mL), [S. aureus] 6.25 mg/mL (CuZnO, 0.139 mg/mL) | [117] |
| ZnO MPs with TiO2 MPs | Sol–gel method (zinc chloride) |
| Broth dilution; MIC; photocatalytic incubation under visible light irradiation | ZnO MPs (0.25%) with TiO2 MPs (1%): [E. coli] 76.8% growth inhibition, [Streptococcus pyogenes] 70.2% growth inhibition, [K. pneumoniae] 80.8% growth inhibition | [118] |
| Combinations of ZnO materials with other biomaterials | |||||
| Chitosan | |||||
| Chitosan-ZnO NP-loaded gallic acid (C-ZnO@gal) films | Hydrothermal method (zinc sulfate) |
| Agar well diffusion | 0.5 mg/mL, [E. coli] 28 mm zone of inhibition, [B. subtilis] 25 mm zone of inhibition | [28] |
| ZnO NP-containing chitosan coating | Not available (conventional product: 2% w/v solution, 10–30 nm) |
| Broth dilution; MIC | [E. coli O157:H7] ▪ Chitosan (2.5%, w/v): 2.5 log (CFU/g) reduction at 4 °C ▪ ZnO NP (1%, w/v)-containing chitosan (2.5%, w/v): 2.8 log (CFU/g) reduction at 4 °C | [82] |
| ZnO NP-containing chitosan/gelatin hybrid nanocomposite (nZnO-chitosan/gelatin) films | Green method using Cassia fistula fruit extract (zinc nitrate hexahydrate) |
| Disk diffusion | [E. coli] ZnO NPs in films: 1%-10.5 mm zone of inhibition, 2%—10.5 mm zone of inhibition, 4%—10.7 mm zone of inhibition [S. aureus] not prominent compared to E. coli | [91] |
| 3D porous ZnO NP-chitosan/silk/sericin scaffolds for wound dressing | Not available (conventional product: solution, ~35 nm) | Porous microstructures/not available (porosity ~86%; pore size 4–200 μm) | Disk diffusion | 1.5 × 1.5 cm2, 2% (w/v) chitosan, 100 μL and 250 μL of ZnO NPs (40 wt% dispersion), [E. coli] 2–4.5 mm zone of growth inhibition, [S. aureus] 2.5–5.5 mm zone of growth inhibition | [136] |
| Chitosan-based ZnO nanocomposites | Co-precipitation (zinc acetate dihydrate) |
| Disc diffusion | Zone of inhibition (mm), [K. pneumoniae] 13 mm (the highest) > [E. coli] > [P. aeruginosa] > [B. subtillis], [S. aureus], and [MRSA] 6 mm (the lowest) | [137] |
| Hydroxyapatite & alginate | |||||
| Hydroxyapatite-biphasic ZnO NP/MP-embedded alginate beads | Precipitation (zinc nitrate) |
| Agar diffusion; colony counting; MIC | 0.1 mg/mL, [E. coli] 56% inhibition, [P. aeruginosa] 65% inhibition, [S. aureus and S. epidermidis] 100% inhibition | [83] |
| Polyethylene glycol | |||||
| Tungsten-doped polyethylene glycol-capped ZnO (W-PEG-ZnO) NPs | Electrochemical method (Zn electrodes) | Near-spheres/~40.46 nm | Agar well diffusion | ▪ Ampicillin: 100 μg/μL [E. coli] 35 mm zone of inhibition, [B. cereus] 20 mm zone of inhibition ▪ W-PEG-ZnO NPs: [E. coli] 400–600 μg/μL, 5–6 mm zone of inhibition, [B. cereus] 300–600 μg/μL, 6–8 mm zone of inhibition | [120] |
| K-carrageenan, bacterial cellulose, propolis extract& curcumin | |||||
| Biopolymer K-carrageenan wrapped ZnO (KC-ZnO) NPs | Precipitation (zinc acetate dehydrate) | KC-ZnO NPs: ovals/97 nm | Disk diffusion; MIC | [MRSA] MIC, 7.50 μg/mL | [27] |
| Bacterial cellulose-ZnO NP-propolis extract (BC-ZnO-propolis) films | Ultrasound (zinc acetate) |
| Disk diffusion; MIC; photocatalytic incubation (254 nm, 30 min) | MIC, [E. coli] >1.89 mg/mL, [B. subtilis] 0.44 or <0.44 mg/mL, [C. albicans] >0.8, 1.3, 1.89, >1.89 mg/mL | [121] |
| Curcumin-loaded ZnO (C-ZnO) NPs | Sol–gel method (zinc nitrate hexahydrate) |
| Well diffusion; colony counting | Zone of inhibition (mm), [E. coli] C-sZnO, 8.4; C-rZnO, 10.1; C-jZnO, 11.1; C-spZnO, 8.1; C-lpZnO, 9.8; C, 7.4 [S. epidermis] C-sZnO, 19.1; C-rZnO, 17.2; C-jZnO, 19.4; C-spZnO, 16.4; C-lpZnO, 20.1; C, 8.2 [S. aureus] C-sZnO, 15.4; C-rZnO, 16.6; C-jZnO, 13.4; C-spZnO, 15.2; C-lpZnO, 17.0; C, 8.1 [B. cereus] C-sZnO, 17.4; C-rZnO, 18.7; C-jZnO, 18.7; C-spZnO, 14.2; C-lpZnO, 14.2; C, 8.4 | [124] |
| Graphene, graphene oxide, & reduced graphene oxide | |||||
| Graphene/ZnO nanocomposite films | Ion exchange process (zinc acetate) |
| Microdilution; MIC | [Streptococcus mutans] MIC, 125 μg/mL | [84] |
| Graphene/ZnO nanocomposite with curcumin (C-ZnO) | Ion exchange process (zinc acetate dihydrate) |
| Agar diffusion; colony counting; microdilution; MIC | MIC,
| [85] |
| Graphene oxide (GO)/ZnO nanocomposite for wound care | Co-precipitation (zinc nitrate) | ▪ GO: smooth and wrinkled surface layers/not available▪ GO/ZnO nanocomposite: well incorporated and distributed ZnO NPs (0.1–0.4 M) on GO sheets forming agglomerates/not available | Disk diffusion, colony counting; dark (D) and visible light-irradiated (L) conditions | Zone of growth inhibition (mm), ▪ ZnO NPs (0.4 M) on GO sheets, 100 μg/mL [E. coli] GO-D, 11 mm; L, 11.5 mm; GO/ZnO (0.4 M)-D, 11 mm; L, 13 mm [P. aeruginosa] GO-D, 10 mm; L, 10.5 mm; GO/ZnO (0.4 M)-D, 10 mm; L, 13 mm [S. typhi] GO-D, 10.5 mm; L, 9 mm; GO/ZnO (0.4 M)-D, 11 mm; L, 11.5 mm [S. flexneri] GO-D, 8 mm; L, 10.6 mm; GO/ZnO (0.4 M)-D, 12 mm; L, 12.5 mm | [86] |
| GO/ZnO composites | Ion exchange process (zinc acetate dihydrate) |
| Agar disk diffusion; MIC | [E. coli] MIC, 2 μg | [87] |
| Reduced graphene oxide (rGO)/ZnO films | Sol–gel synthesis (zinc acetate dihydrate) |
| Serial dilution; colony counting; MIC; photocatalytic incubation (UV at 365 nm) | [S. aureus] 1 wt% rGO >99% (>2-log) reduction | [88] |
| Cotton fabric | |||||
| ZnO MPs-loaded chitosan-coated cotton fabrics | Precipitation (zinc chloride) | Uniformly distributed dense microstructure of rods/not available | Disk diffusion | [E. coli] 2.5 cm zone of growth inhibition (ZnCl2 4%, chitosan 1–2%/1 g cotton fabric) | [126] |
| Cotton-ZnO NP composites (C-nZnO) | Precipitation (zinc chloride) |
| Disk diffusion; colony counting | nZnO amounts in C-nZnO: 2.2, 1.7, 4.9, 4.3, 11.1, 7.8, 22.2, and 16.7 wt% 9 mm in diameter, [E. coli] 97–100% growth reduction, [S. aureus] 96–98% growth reduction | [127] |
| ZnO NP-coated fabric | Green method using starch (zinc nitrate) |
| Colony counting | 4.8 cm in diameter of fabric, [E. coli] 80% reduction [S. aureus] 99.99% reduction | [129] |
| ZnO quantum dots (QDs) | |||||
| Different nanostructure-based ZnO QDs (ZnO QD-1–ZnO QD-14) | Sol–gel method (zinc acetate dihydrate) | Nanorods, nanotubes, nanospheres, nanowhiskers, nanoflowers/not available | Agar well diffusion; agar dilution; MIC | MIC, [E. coli] ZnO QD-1: 25 mg/mL, [Enterobacter aerogenes] ZnO QD-4 and ZnO QD-6: 25 mg/mL, [K. pneumonia] ZnO QD-3 and ZnO QD-5: 12.5 mg/mL, [P. aeruginosa] ZnO QD-3 and ZnO QD-7: 12.5 mg/mL, [Bacillus anthracis] ZnO QD-2, ZnO QD-3 and ZnO QD-8: 6.25 mg/mL, [S. aureus] ZnO QD-8: 6.25 mg/mL, [L. monocytogenes] ZnO QD-6 and ZnO QD-7: 50 mg/mL, [E. faecalis] ZnO QD-2 and ZnO QD-7: 25 mg/mL, [B. cereus] ZnO QD-3 and ZnO QD-5: 12.5 mg/mL, [S. epidermidis] ZnO QD-8: 1.5 mg/mL | [89] |
| ZnO QDs | Green method using Eclipta alba leaf extract (zinc acetate dihydrate) | Spheres/~6 nm | Agar diffusion | [E. coli] 15.69 mm zone of inhibition (1.6-fold increase compared to bulk zinc acetate at 5 mM) | [90] |
| Antimicrobial peptide-based ZnO QDs containing vancomycin and methicillin (Van@ZnO-BSA-PEP-MPA; Met@ZnO-BSA-PEP-MPA) | Precipitation (zinc acetate) | ZnO@BSA-PEP-MPA: spheres/104 nm | Broth dilution; MIC; in vivo diagnostics-4 × 108 CFU S. aureus for infection and Van@ZnO-BSA-PEP-MPA at 5.0 mg/kg for theranostics | MIC,
| [141] |
| Polyvinylpyrrolidone-capped ZnO (PVP-ZnO) QDs | Precipitation (zinc acetate hydrate) |
| Agar diffusion; colony counting |
| [142] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, S.-E.; Jin, H.-E. Antimicrobial Activity of Zinc Oxide Nano/Microparticles and Their Combinations against Pathogenic Microorganisms for Biomedical Applications: From Physicochemical Characteristics to Pharmacological Aspects. Nanomaterials 2021, 11, 263. https://doi.org/10.3390/nano11020263
Jin S-E, Jin H-E. Antimicrobial Activity of Zinc Oxide Nano/Microparticles and Their Combinations against Pathogenic Microorganisms for Biomedical Applications: From Physicochemical Characteristics to Pharmacological Aspects. Nanomaterials. 2021; 11(2):263. https://doi.org/10.3390/nano11020263
Chicago/Turabian StyleJin, Su-Eon, and Hyo-Eon Jin. 2021. "Antimicrobial Activity of Zinc Oxide Nano/Microparticles and Their Combinations against Pathogenic Microorganisms for Biomedical Applications: From Physicochemical Characteristics to Pharmacological Aspects" Nanomaterials 11, no. 2: 263. https://doi.org/10.3390/nano11020263
APA StyleJin, S.-E., & Jin, H.-E. (2021). Antimicrobial Activity of Zinc Oxide Nano/Microparticles and Their Combinations against Pathogenic Microorganisms for Biomedical Applications: From Physicochemical Characteristics to Pharmacological Aspects. Nanomaterials, 11(2), 263. https://doi.org/10.3390/nano11020263






