SPIONs Conjugate Supported Anticancer Drug Doxorubicin’s Delivery: Current Status, Challenges, and Prospects
Abstract
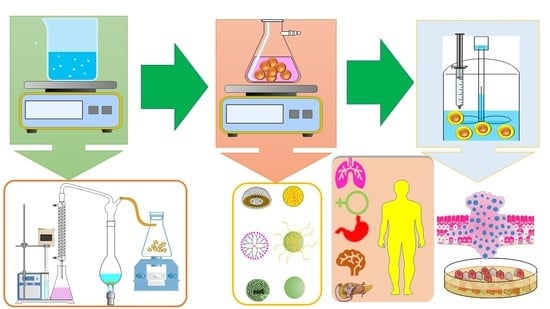
:1. SPIONs: Outlook, Applications, Biological Outreach, and Limitations
2. DOX Delivery: SPIONs’ Polymeric, Monomeric, and Miscellaneous Conjugates
2.1. Synthetic Single-Polymer-Based DOX Conjugates
2.1.1. Polyethylene Glycol
2.1.2. Poly-Lactic-co-Glycolic Acid
2.2. Combination/Copolymers-Based DOX-SPIONs Conjugates
2.2.1. Polyethylene Glycol-Poly-Lactic-co-Glycolic Acid
2.2.2. Polyethylene Glycol-3-Aminopropyl Triethoxy Silane
2.2.3. Polyethylene Glycol-Poly-ε-Caprolactone
2.2.4. DSPE-Polyethylene Glycol 2000
2.2.5. Polyethylene Glycol-Polyethylene Imine
2.2.6. Polyethylene Glycol-Block-Poly-ε-Caprolactone
2.2.7. Polyamidoamine-Polyethylene Glycol-Dodecyl Amine
2.2.8. Polylactic Acid-Polyethylene Glycol
2.2.9. Bis-[(p-sulfonato-phenyl)-phenylphosphine]-methoxy-polyethylene glycol-thiol
2.2.10. Polyethylene Oxide-Trimellitic Anhydride Chloride-Folate
2.3. Single Characteristically Specified Polymer-Based SPIONs Conjugates
2.3.1. Polyvinyl Alcohol: The Thermoplastic Polymer
2.3.2. Polyethylene Imine: The Cationic Polymer
2.3.3. Polydopamine: Amines and Catechol-Ends Polymer
2.3.4. Poly-(N,N-dimethyl)acrylamide: Conductive Co-Polymeric Material
2.4. Thermo-Responsive Polymer Conjugates
2.5. PAMAM-Dendrimer’s Conjugate
2.6. Zwitter Ionic Polymer Conjugates
2.7. Natural Polymer-Based DOX-SPIONs Conjugates
2.7.1. Dextran
2.7.2. Chitosan
2.7.3. Chondroitin-4-Sulfate
2.7.4. Hyaluronan
2.7.5. Starch-Octanoic Acid Micelles
2.7.6. Heparin
2.7.7. Albumin
2.7.8. Spider Silk
2.7.9. Prostate-Specific Membrane Antigen Aptamers
2.8. Capped SPIONs-Based DOX Conjugates
2.8.1. Citric-Acid-Capped SPIONs-DOX Conjugate
2.8.2. Folic-Acid-Capped SPIONs-DOX Conjugate
2.9. SPIONs Monomer Conjugate: Trimethoxy Silylpropyl Ethylenediamine Triacetic Acid
2.10. SPIONs-Miscellaneous Entities DOX Conjugates
2.10.1. Graphene Oxide
2.10.2. Hydroxyapatite
2.10.3. Iodinated Oils
3. Polymer Comparatives: Nano-systems Sizes, Drug Loading, Zeta Potential, and Stability
4. Polymer Conjugates Comparatives: Cell Lines and Cytotoxicity
5. SPIONs-Inspired Magnetic Spectroscopy: Development of a Medical Diagnostic, Tomographic Imaging, and Quantification Tools
6. SPIONs-DOX Conjugate: Nano-theranostic Agent in Diagnosis and Therapy
7. SPIONs and Polymeric Conjugates: Toxicological Issues and Biosafety Facts
7.1. Toxicological Issues
7.2. Biosafety Facts
8. Conclusions
9. Prospects and Future Directions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Renu, K.; Abilash, V.G.; Tirupathi, P.P.B.; Arunachalam, S. Molecular mechanism of doxorubicin-induced cardiomyopathy–An update. Eur. J. Pharmacol. 2018, 818, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Wallace, K.B.; Sardão, V.A.; Oliveira, P.J. Mitochondrial determinants of doxorubicin-induced cardiomyopathy. Circ. Res. 2020, 126, 926–941. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, Z.; Wang, J.; Luo, Y.; Zeng, R.; Zhang, C.; Zhou, W.; Guo, K.; Wu, H.; Sha, W.; Chen, H. Targeted extracellular vesicle delivery systems employing superparamagnetic iron oxide nanoparticles. Acta Biomater. 2021, 134, 13–31. [Google Scholar] [CrossRef] [PubMed]
- Musielak, M.; Piotrowski, I.; Suchorska, W.M. Superparamagnetic iron oxide nanoparticles (SPIONs) as a multifunctional tool in various cancer therapies. Rep. Pr. Oncol. Radiother. 2019, 24, 307–314. [Google Scholar] [CrossRef]
- Frantellizzi, V.; Conte, M.; Pontico, M.; Pani, A.; Pani, R.; De Vincentis, G. New Frontiers in Molecular Imaging with Superparamagnetic Iron Oxide Nanoparticles (SPIONs): Efficacy, Toxicity, and Future Applications. Nucl. Med. Mol. Imaging 2020, 54, 65–80. [Google Scholar] [CrossRef]
- Dulińska-Litewka, J.; Łazarczyk, A.; Hałubiec, P.; Szafrański, O.; Karnas, K.; Karewicz, A. Superparamagnetic Iron Oxide Nanoparticles—Current and Prospective Medical Applications. Materials 2019, 12, 617. [Google Scholar] [CrossRef] [Green Version]
- Reczyńska, K.; Marszałek, M.; Zarzycki, A.; Reczyński, W.; Kornaus, K.; Pamuła, E.; Chrzanowski, W. Superparamagnetic Iron Oxide Nanoparticles Modified with Silica Layers as Potential Agents for Lung Cancer Treatment. Nanomaterials 2020, 10, 1076. [Google Scholar] [CrossRef]
- Seo, W.S.; Lee, J.H.; Sun, X.; Suzuki, Y.; Mann, D.; Liu, Z.; Terashima, M.; Yang, P.C.; McConnell, M.; Nishimura, D.G.; et al. FeCo/graphitic-shell nanocrystals as advanced magnetic-resonance-imaging and near-infrared agents. Nat. Mater. 2006, 5, 971–976. [Google Scholar] [CrossRef]
- Tran, H.-V.; Ngo, N.M.; Medhi, R.; Srinoi, P.; Liu, T.; Rittikulsittichai, S.; Lee, T.R. Multifunctional Iron Oxide Magnetic Nanoparticles for Biomedical Applications: A Review. Materials 2022, 15, 503. [Google Scholar] [CrossRef]
- Manescu, V.; Paltanea, G.; Antoniac, I.; Vasilescu, M. Magnetic Nanoparticles Used in Oncology. Materials 2021, 14, 5948. [Google Scholar] [CrossRef]
- Husen, A.; Siddiqi, K.S. Phytosynthesis of nanoparticles: Concept, controversy and application. Nanoscale Res. Lett. 2014, 9, 229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.-X.; Hussain, S.; Krestin, G. Superparamagnetic iron oxide contrast agents: Physicochemical characteristics and applications in MR imaging. Eur. Radiol. 2001, 11, 2319–2331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vakili-Ghartavol, R.; Momtazi-Borojeni, A.A.; Vakili-Ghartavol, Z.; Aiyelabegan, H.T.; Jaafari, M.R.; Rezayat, S.M.; Bidgoli, S.A. Toxicity assessment of superparamagnetic iron oxide nanoparticles in different tissues. Artif. Cells Nanomed. Biotechnol. 2020, 48, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Couto, D.; Freitas, M.; Carvalho, F.; Fernandes, E. Iron Oxide Nanoparticles: An Insight into their Biomedical Applications. Curr. Med. Chem. 2015, 22, 1808–1828. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, B.R.; Frendo, M.; Vogan, J.; Louie, A.Y. Size-controlled synthesis of dextran sulfate coated iron oxide nanoparticles for magnetic resonance imaging. Nanotechnology 2007, 18, 035603. [Google Scholar] [CrossRef] [PubMed]
- Laurent, S.; Saei, A.A.; Behzadi, S.; Panahifar, A.; Mahmoudi, M. Superparamagnetic iron oxide nanoparticles for delivery of therapeutic agents: Opportunities and challenges. Expert Opin. Drug Deliv. 2014, 11, 1449–1470. [Google Scholar] [CrossRef]
- Mahmoudi, M.; Sant, S.; Wang, B.; Laurent, S.; Sen, T. Superparamagnetic iron oxide nanoparticles (SPIONs): Development, surface modification and applications in chemotherapy. Adv. Drug Deliv. Rev. 2011, 63, 24–46. [Google Scholar] [CrossRef] [Green Version]
- Rosen, J.E.; Chan, L.; Shieh, D.-B.; Gu, F.X. Iron oxide nanoparticles for targeted cancer imaging and diagnostics. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 275–290. [Google Scholar] [CrossRef]
- Muthiah, M.; Park, I.-K.; Cho, C.-S. Surface modification of iron oxide nanoparticles by biocompatible polymers for tissue imaging and targeting. Biotechnol. Adv. 2013, 31, 1224–1236. [Google Scholar] [CrossRef]
- Xu, C.; Sun, S. New forms of superparamagnetic nanoparticles for biomedical applications. Adv. Drug Deliv. Rev. 2012, 65, 732–743. [Google Scholar] [CrossRef]
- Bustamante-Torres, M.; Romero-Fierro, D.; Estrella-Nuñez, J.; Arcentales-Vera, B.; Chichande-Proaño, E.; Bucio, E. Polymeric Composite of Magnetite Iron Oxide Nanoparticles and Their Application in Biomedicine: A Review. Polymers 2022, 14, 752. [Google Scholar] [CrossRef] [PubMed]
- Matos, J.C.; Gonçalves, M.C.; Pereira, L.C.J.; Vieira, B.J.C.; Waerenborgh, J.C. SPIONs Prepared in Air through Improved Synthesis Methodology: The Influence of γ-Fe2O3/Fe3O4 Ratio and Coating Composition on Magnetic Properties. Nanomaterials 2019, 9, 943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Souza, A.A.; Shegokar, R. Polyethylene glycol (PEG): A versatile polymer for pharmaceutical applications. Expert Opin. Drug Deliv. 2016, 13, 1257–1275. [Google Scholar] [CrossRef] [PubMed]
- Suk, J.S.; Xu, Q.; Kim, N.; Hanes, J.; Ensign, L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016, 99 Pt A, 28–51. [Google Scholar] [CrossRef] [Green Version]
- Abdelfattah, A.; Aboutaleb, A.E.; Abdel-Aal, A.M.; Abdellatif, A.A.; Tawfeek, H.M.; Abdel-Rahman, S.I. Design and optimization of PEGylated silver nanoparticles for efficient delivery of doxorubicin to cancer cells. J. Drug Deliv. Sci. Technol. 2022, 71, 103347. [Google Scholar] [CrossRef]
- Quinto, C.A.; Mohindra, P.; Tong, S.; Bao, G. Multifunctional superparamagnetic iron oxide nanoparticles for combined chemotherapy and hyperthermia cancer treatment. Nanoscale 2015, 7, 12728–12736. [Google Scholar] [CrossRef] [Green Version]
- Khafaji, M.; Zamani, M.; Vossoughi, M.; Zad, A.I. Doxorubicin/Cisplatin-Loaded Superparamagnetic Nanoparticles As A Stimuli-Responsive Co-Delivery System For Chemo-Photothermal Therapy. Int. J. Nanomed. 2019, 14, 8769–8786. [Google Scholar] [CrossRef] [Green Version]
- Shaik, A.P.; Shaik, A.S.; Al Majwal, A.; Al Faraj, A. Blocking Interleukin-4 Receptor α Using Polyethylene Glycol Functionalized Superparamagnetic Iron Oxide Nanocarriers to Inhibit Breast Cancer Cell Proliferation. Cancer Res. Treat. 2017, 49, 322–329. [Google Scholar] [CrossRef] [Green Version]
- Zhu, L.; Wang, D.; Wei, X.; Zhu, X.; Li, J.; Tu, C.; Su, Y.; Wu, J.; Zhu, B.; Yan, D. Multifunctional pH-sensitive superparamagnetic iron-oxide nanocomposites for targeted drug delivery and MR imaging. J. Control. Release 2013, 169, 228–238. [Google Scholar] [CrossRef]
- Semkina, A.; Abakumov, M.; Grinenko, N.; Skorikov, A.; Mironova, E.; Davydova, G.; Majouga, A.; Nukolova, N.; Kabanov, A.; Chekhonin, V. Core–shell–corona doxorubicin-loaded superparamagnetic Fe3O4 nanoparticles for cancer theranostics. Colloids Surf. B Biointerfaces 2015, 136, 1073–1080. [Google Scholar] [CrossRef]
- Yang, X.; Hong, H.; Grailer, J.J.; Rowland, I.J.; Javadi, A.; Hurley, S.A.; Xiao, Y.; Yang, Y.; Zhang, Y.; Nickles, R.J.; et al. cRGD-functionalized, DOX-conjugated, and 64Cu-labeled superparamagnetic iron oxide nanoparticles for targeted anticancer drug delivery and PET/MR imaging. Biomaterials 2011, 32, 4151–4160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zou, P.; Yu, Y.; Wang, Y.A.; Zhong, Y.; Welton, A.; Galbán, C.; Wang, S.; Sun, D. Superparamagnetic Iron Oxide Nanotheranostics for Targeted Cancer Cell Imaging and pH-Dependent Intracellular Drug Release. Mol. Pharm. 2010, 7, 1974–1984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mirakabad, F.S.T.; Nejati-Koshki, K.; Akbarzadeh, A.; Yamchi, M.R.; Milani, M.; Zarghami, N.; Zeighamian, V.; Rahimzadeh, A.; Alimohammadi, S.; Hanifehpour, Y.; et al. PLGA-Based Nanoparticles as Cancer Drug Delivery Systems. Asian Pac. J. Cancer Prev. 2014, 15, 517–535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mosafer, J.; Teymouri, M. Comparative study of superparamagnetic iron oxide/doxorubicin co-loaded poly (lactic-co-glycolic acid) nanospheres prepared by different emulsion solvent evaporation methods. Artif. Cells Nanomed. Biotechnol. 2017, 46, 1146–1155. [Google Scholar] [CrossRef] [Green Version]
- Gao, P.; Mei, C.; He, L.; Xiao, Z.; Chan, L.; Zhang, D.; Shi, C.; Chen, T.; Luo, L. Designing multifunctional cancer-targeted nanosystem for magnetic resonance molecular imaging-guided theranostics of lung cancer. Drug Deliv. 2018, 25, 1811–1825. [Google Scholar] [CrossRef] [Green Version]
- Vu, M.T.; Jeong, Y.I.; Choi, C.; Nam, J.P.; Son, D.H.; Park, J.K.; Kim, W.S.; Kim, M.Y.; Jang, M.K.; Nah, J.W. Surfactant-free nanoparticles of doxorubicin-conjugated poly(DL-lactide-co-glycolide). Macromol. Res. 2010, 18, 1115–1120. [Google Scholar] [CrossRef]
- Luque-Michel, E.; Sebastian, V.; Larrea, A.; Marquina, C.; Blanco-Prieto, M.J. Co-encapsulation of superparamagnetic nanoparticles and doxorubicin in PLGA nanocarriers: Development, characterization and in vitro antitumor efficacy in glioma cells. Eur. J. Pharm. Biopharm. 2019, 145, 65–75. [Google Scholar] [CrossRef]
- Niu, C.; Wang, Z.; Lu, G.; Krupka, T.M.; Sun, Y.; You, Y.; Song, W.; Ran, H.; Li, P.; Zheng, Y. Doxorubicin loaded superparamagnetic PLGA-iron oxide multifunctional microbubbles for dual-mode US/MR imaging and therapy of metastasis in lymph nodes. Biomaterials 2012, 34, 2307–2317. [Google Scholar] [CrossRef]
- Thirunavukkarasu, G.K.; Cherukula, K.; Lee, H.; Jeong, Y.Y.; Park, I.-K.; Lee, J.Y. Magnetic field-inducible drug-eluting nanoparticles for image-guided thermo-chemotherapy. Biomaterials 2018, 180, 240–252. [Google Scholar] [CrossRef]
- Dong, Q.; Wan, C.; Yang, H.; Zheng, D.; Xu, L.; Zhou, Z.; Xie, S.; Du, J.; Li, F. Targeted gold nanoshelled hybrid nanocapsules encapsulating doxorubicin for bimodal imaging and near-infrared triggered synergistic therapy of Her2-positve breast cancer. J. Biomater. Appl. 2020, 35, 430–445. [Google Scholar] [CrossRef]
- Shi, L.; Zhang, J.; Zhao, M.; Tang, S.; Cheng, X.; Zhang, W.; Li, W.; Liu, X.; Peng, H.; Wang, Q. Effects of polyethylene glycol on the surface of nanoparticles for targeted drug delivery. Nanoscale 2021, 13, 10748–10764. [Google Scholar] [CrossRef] [PubMed]
- Nehate, C.; Alex, M.A.; Kumar, A.; Koul, V. Combinatorial delivery of superparamagnetic iron oxide nanoparticles (γFe2O3) and doxorubicin using folate conjugated redox sensitive multiblock polymeric nanocarriers for enhancing the chemotherapeutic efficacy in cancer cells. Mater. Sci. Eng. C 2017, 75, 1128–1143. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Tang, X.; Zhang, J.; Lu, W.; Lin, X.; Zhang, Y.; Tian, B.; Yang, H.; He, H. PEG–PLGA copolymers: Their structure and structure-influenced drug delivery applications. J. Control. Release 2014, 183, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Davaran, S.; Asgari, D.; Akbarzadeh, A.; Zarghami, N.; Mikaeili, H.; Mohammad, R. Preparation and in vitro evaluation of doxorubicin-loaded Fe3O4 magnetic nanoparticles modified with biocompatible copolymers. Int. J. Nanomed. 2012, 7, 511–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alghunaim, A.; Brink, E.T.; Newby, B.-M.Z. Surface immobilization of thermo-responsive poly(N-isopropylacrylamide) by simple entrapment in a 3-aminopropyltriethoxysilane network. Polymer 2016, 101, 139–150. [Google Scholar] [CrossRef] [Green Version]
- Zolata, H.; Davani, F.A.; Afarideh, H. Synthesis, characterization and theranostic evaluation of Indium-111 labeled multifunctional superparamagnetic iron oxide nanoparticles. Nucl. Med. Biol. 2015, 42, 164–170. [Google Scholar] [CrossRef]
- Saxena, N.; Agraval, H.; Barick, K.; Ray, D.; Aswal, V.; Singh, A.; Yadav, U.C.; Dube, C.L. Thermal and microwave synthesized SPIONs: Energy effects on the efficiency of nano drug carriers. Mater. Sci. Eng. C 2020, 111, 110792. [Google Scholar] [CrossRef]
- Shuai, X.; Ai, H.; Nasongkla, N.; Kim, S.; Gao, J. Micellar carriers based on block copolymers of poly(ε-caprolactone) and poly(ethylene glycol) for doxorubicin delivery. J. Control. Release 2004, 98, 415–426. [Google Scholar] [CrossRef]
- Li, L.; He, X.; Su, H.; Zhou, D.; Song, H.; Wang, L.; Jiang, X. Poly(ethylene glycol)-block-poly(ε-caprolactone)–and phospholipid-based stealth nanoparticles with enhanced therapeutic efficacy on murine breast cancer by improved intracellular drug delivery. Int. J. Nanomed. 2015, 10, 1791–1804. [Google Scholar] [CrossRef] [Green Version]
- Mousavi, S.-D.; Maghsoodi, F.; Panahandeh, F.; Yazdian-Robati, R.; Reisi-Vanani, A.; Tafaghodi, M. Doxorubicin delivery via magnetic nanomicelles comprising from reduction-responsive poly(ethylene glycol)-b-poly(ε-caprolactone) (PEG-SS-PCL) and loaded with superparamagnetic iron oxide (SPIO) nanoparticles: Preparation, characterization and simulation. Mater. Sci. Eng. C 2018, 92, 631–643. [Google Scholar] [CrossRef]
- Liu, Y.; Hu, Y.; Huang, L. Influence of polyethylene glycol density and surface lipid on pharmacokinetics and biodistribution of lipid-calcium-phosphate nanoparticles. Biomaterials 2014, 35, 3027–3034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, C.; Wang, X.; Zheng, Z.; Gao, C.; Chen, X.; Zhao, S.; Dai, Z. Doxorubicin and indocyanine green loaded superparamagnetic iron oxide nanoparticles with PEGylated phospholipid coating for magnetic resonance with fluorescence imaging and chemotherapy of glioma. Int. J. Nanomed. 2018, 14, 101–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lutz, G.J.; Sirsi, S.R.; Williams, J.H.; Le Doux, J.M. PEG–PEI Copolymers for Oligonucleotide Delivery to Cells and Tissues. Methods Mol. Biol. 2008, 433, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Mao, K.; Zhang, B.; Zhao, Y. Superparamagnetic iron oxide nanoparticles conjugated with folic acid for dual target-specific drug delivery and MRI in cancer theranostics. Mater. Sci. Eng. C 2017, 70, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.; Sun, Q.; Liang, B.; Shen, J.; Shuai, X. Targeting EGFR-overexpressing tumor cells using Cetuximab-immunomicelles loaded with doxorubicin and superparamagnetic iron oxide. Eur. J. Radiol. 2011, 80, 699–705. [Google Scholar] [CrossRef]
- Kim, Y.; Klutz, A.M.; Jacobson, K. Systematic Investigation of Polyamidoamine Dendrimers Surface-Modified with Poly(ethylene glycol) for Drug Delivery Applications: Synthesis, Characterization, and Evaluation of Cytotoxicity. Bioconjugate Chem. 2008, 19, 1660–1672. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.; Shi, M.; Liu, P.; Ko, A.; Zhong, W.; Liao, W.; Xing, M.M. Reducible polyamidoamine-magnetic iron oxide self-assembled nanoparticles for doxorubicin delivery. Biomaterials 2013, 35, 1240–1248. [Google Scholar] [CrossRef]
- Zeng, Z.W.; Xiao, R.Z.; Zhou, G.L.; Wang, J.J.; Li, F.Z.; Wang, A.M. Recent advances in PEG–PLA block copolymer nanoparticles. Int. J. Nanomed. 2010, 5, 1057–1065. [Google Scholar] [CrossRef] [Green Version]
- Khaledian, M.; Nourbakhsh, M.S.; Saber, R.; Hashemzadeh, H.; Darvishi, M.H. Preparation and Evaluation of Doxorubicin-Loaded PLA–PEG–FA Copolymer Containing Superparamagnetic Iron Oxide Nanoparticles (SPIONs) for Cancer Treatment: Combination Therapy with Hyperthermia and Chemotherapy. Int. J. Nanomed. 2020, 15, 6167–6182. [Google Scholar] [CrossRef]
- Thorat, N.D.; Lemine, O.M.; Bohara, R.A.; Omri, K.; El Mir, L.; Tofail, S.A.M. Superparamagnetic iron oxide nanocargoes for combined cancer thermotherapy and MRI applications. Phys. Chem. Chem. Phys. 2016, 18, 21331–21339. [Google Scholar] [CrossRef]
- Grammer, L.C.; Shaughnessy, M.A.; Zeiss, C.R.; Greenberger, P.A.; Patterson, R. Review of trimellitic anhydride (TMA) induced respiratory response. Allergy Asthma Proc. 1997, 18, 235–237. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, D.; Bernstein, J.A. Health Effects of Trimellitic Anhydride Occupational Exposure: Insights from Animal Models and Immunosurveillance Programs. Clin. Rev. Allergy Immunol. 2020, 59, 61–77. [Google Scholar] [CrossRef] [PubMed]
- Maeng, J.H.; Lee, D.-H.; Jung, K.H.; Bae, Y.-H.; Park, I.-S.; Jeong, S.; Jeon, Y.-S.; Shim, C.-K.; Kim, W.; Kim, J.; et al. Multifunctional doxorubicin loaded superparamagnetic iron oxide nanoparticles for chemotherapy and magnetic resonance imaging in liver cancer. Biomaterials 2010, 31, 4995–5006. [Google Scholar] [CrossRef]
- Rivera-Hernández, G.; Antunes-Ricardo, M.; Martínez-Morales, P.; Sánchez, M.L. Polyvinyl alcohol based-drug delivery systems for cancer treatment. Int. J. Pharm. 2021, 600, 120478. [Google Scholar] [CrossRef] [PubMed]
- Liang, Q.; Wang, Y.-X.; Ding, J.-S.; He, W.; Deng, L.-L.; Li, N.; Liao, Y.-J.; Li, Z.; Ye, B.; Wang, W. Intra-arterial delivery of superparamagnetic iron-oxide nanoshell and polyvinyl alcohol based chemoembolization system for the treatment of liver tumor. Discov. Med. 2017, 23, 27–39. [Google Scholar]
- Nadeem, M.; Ahmad, M.; Akhtar, S.; Shaari, A.; Riaz, S.; Naseem, S.; Masood, M.; Saeed, M.A. Magnetic Properties of Polyvinyl Alcohol and Doxorubicine Loaded Iron Oxide Nanoparticles for Anticancer Drug Delivery Applications. PLoS ONE 2016, 11, e0158084. [Google Scholar] [CrossRef] [Green Version]
- Patnaik, S.; Gupta, K.C. Novel polyethylenimine-derived nanoparticles for in vivo gene delivery. Expert Opin. Drug Deliv. 2012, 10, 215–228. [Google Scholar] [CrossRef]
- Wan, L.; Chen, Z.; Deng, Y.; Liao, T.; Kuang, Y.; Liu, J.; Duan, J.; Xu, Z.; Jiang, B.; Li, C. A novel intratumoral pH/redox-dual-responsive nanoplatform for cancer MR imaging and therapy. J. Colloid Interface Sci. 2020, 573, 263–277. [Google Scholar] [CrossRef]
- Jin, A.; Wang, Y.; Lin, K.; Jiang, L. Nanoparticles modified by polydopamine: Working as “drug” carriers. Bioact. Mater. 2020, 5, 522–541. [Google Scholar] [CrossRef]
- Singh, N.; Sallem, F.; Mirjolet, C.; Nury, T.; Sahoo, S.K.; Millot, N.; Kumar, R. Polydopamine Modified Superparamagnetic Iron Oxide Nanoparticles as Multifunctional Nanocarrier for Targeted Prostate Cancer Treatment. Nanomaterials 2019, 9, 138. [Google Scholar] [CrossRef] [Green Version]
- Zasónska, B.A.; Boiko, N.; Horák, D.; Klyuchivska, O.; Macková, H.; Beneš, M.J.; Babič, M.; Trchová, M.; Hromádková, J.; Stoika, R. The Use of Hydrophilic Poly(N,N-dimethylacrylamide) for Promoting Engulfment of Magnetic γ-Fe2O3 Nanoparticles by Mammalian Cells. J. Biomed. Nanotechnol. 2013, 9, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Babič, M.; Horák, D.; Jendelová, P.; Glogarová, K.; Herynek, V.; Trchová, M.; Likavčanová, K.; Lesný, P.; Pollert, E.; Hájek, M.; et al. Poly(N,N-dimethylacrylamide)-Coated Maghemite Nanoparticles for Stem Cell Labeling. Bioconjugate Chem. 2009, 20, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Oleksa, V.; Macková, H.; Patsula, V.; Dydowiczová, A.; Janoušková, O.; Horák, D. Doxorubicin-Conjugated Iron Oxide Nanoparticles: Surface Engineering and Biomedical Investigation. ChemPlusChem 2020, 85, 1156–1163. [Google Scholar] [CrossRef] [PubMed]
- Majeed, M.I.; Lu, Q.; Yan, W.; Li, Z.; Hussain, I.; Tahir, M.N.; Tremel, W.; Tan, B. Highly water-soluble magnetic iron oxide (Fe3O4) nanoparticles for drug delivery: Enhanced in vitro therapeutic efficacy of doxorubicin and MION conjugates. J. Mater. Chem. B 2013, 1, 2874–2884. [Google Scholar] [CrossRef] [Green Version]
- Pandey, N.; Menon, J.; Takahashi, M.; Hsieh, J.-T.; Yang, J.; Nguyen, K.T.; Wadajkar, A.S. Thermo-responsive Fluorescent Nanoparticles for Multimodal Imaging and Treatment of Cancers. Nanotheranostics 2020, 4, 1–13. [Google Scholar] [CrossRef]
- Tomankova, K.; Polakova, K.; Pizova, K.; Binder, S.; Kolarova, M.; Kriegova, E.; Zapletalova, J.; Malina, L.; Horakova, J.; Malohlava, J.; et al. In vitro cytotoxicity analysis of doxorubicin-loaded/superparamagnetic iron oxide colloidal nanoassemblies on MCF7 and NIH3T3 cell lines. Int. J. Nanomed. 2015, 10, 949–961. [Google Scholar] [CrossRef] [Green Version]
- Asghar, K.; Qasim, M.; Dharmapuri, G.; Das, D.D. Thermoresponsive polymer gated and superparamagnetic nanoparticle embedded hollow mesoporous silica nanoparticles as smart multifunctional nanocarrier for targeted and controlled delivery of doxorubicin. Nanotechnology 2020, 31, 455604. [Google Scholar] [CrossRef]
- Ferjaoui, Z.; Al Dine, E.J.; Kulmukhamedova, A.; Bezdetnaya, L.; Chang, C.S.; Schneider, R.; Mutelet, F.; Mertz, D.; Begin-Colin, S.; Quilès, F.; et al. Doxorubicin-Loaded Thermoresponsive Superparamagnetic Nanocarriers for Controlled Drug Delivery and Magnetic Hyperthermia Applications. ACS Appl. Mater. Interfaces 2019, 11, 30610–30620. [Google Scholar] [CrossRef]
- Chauhan, A.S. Dendrimers for Drug Delivery. Molecules 2018, 23, 938. [Google Scholar] [CrossRef] [Green Version]
- Chang, Y.; Meng, X.; Zhao, Y.; Li, K.; Zhao, B.; Zhu, M.; Li, Y.; Chen, X.; Wang, J. Novel water-soluble and pH-responsive anticancer drug nanocarriers: Doxorubicin–PAMAM dendrimer conjugates attached to superparamagnetic iron oxide nanoparticles (IONPs). J. Colloid Interface Sci. 2011, 363, 403–409. [Google Scholar] [CrossRef]
- Blackman, L.D.; Gunatillake, P.A.; Cass, P.; Locock, K.E.S. An introduction to zwitterionic polymer behavior and applications in solution and at surfaces. Chem. Soc. Rev. 2018, 48, 757–770. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Sundaram, H.S.; Wei, Z.; Li, C.; Yuan, Z. Applications of zwitterionic polymers. React. Funct. Polym. 2017, 118, 51–61. [Google Scholar] [CrossRef]
- Debayle, M.; Balloul, E.; Dembele, F.; Xu, X.; Hanafi, M.; Ribot, F.; Monzel, C.; Coppey, M.; Fragola, A.; Dahan, M.; et al. Zwitterionic polymer ligands: An ideal surface coating to totally suppress protein-nanoparticle corona formation? Biomaterials 2019, 219, 119357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, H.; Liu, Y.; Wang, D.; Wu, C.; Xia, C.; Gong, Q.; Song, B.; Ai, H. Amphiphilic starlike dextran wrapped superparamagnetic iron oxide nanoparticle clsuters as effective magnetic resonance imaging probes. Biomaterials 2013, 34, 1193–1203. [Google Scholar] [CrossRef]
- Rizeq, B.R.; Younes, N.N.; Rasool, K.; Nasrallah, G.K. Synthesis, Bioapplications, and Toxicity Evaluation of Chitosan-Based Nanoparticles. Int. J. Mol. Sci. 2019, 20, 5776. [Google Scholar] [CrossRef] [Green Version]
- Javid, A.; Ahmadian, S.; Saboury, A.A.; Kalantar, S.M.; Rezaei-Zarchi, S. Chitosan-Coated Superparamagnetic Iron Oxide Nanoparticles for Doxorubicin Delivery: Synthesis and Anticancer Effect Against Human Ovarian Cancer Cells. Chem. Biol. Drug Des. 2013, 82, 296–306. [Google Scholar] [CrossRef]
- Yang, J.; Shen, M.; Wen, H.; Luo, Y.; Huang, R.; Rong, L.; Xie, J. Recent advance in delivery system and tissue engineering applications of chondroitin sulfate. Carbohydr. Polym. 2020, 230, 115650. [Google Scholar] [CrossRef]
- Mallick, N.; Anwar, M.; Asfer, M.; Mehdi, S.H.; Alam Rizvi, M.M.; Panda, A.K.; Talegaonkar, S.; Ahmad, F. Chondroitin sulfate-capped super-paramagnetic iron oxide nanoparticles as potential carriers of doxorubicin hydrochloride. Carbohydr. Polym. 2016, 151, 546–556. [Google Scholar] [CrossRef]
- Sakurai, Y.; Harashima, H. Hyaluronan-modified nanoparticles for tumor-targeting. Expert Opin. Drug Deliv. 2019, 16, 915–936. [Google Scholar] [CrossRef]
- Vyas, D.; Lopez-Hisijos, N.; Gandhi, S.; El-Dakdouki, M.; Basson, M.D.; Walsh, M.F.; Huang, X.; Vyas, A.K.; Chaturvedi, L.S. Doxorubicin-Hyaluronan Conjugated Super-Paramagnetic Iron Oxide Nanoparticles (DOX-HA-SPIONs) Enhanced Cytoplasmic Uptake of Doxorubicin and Modulated Apoptosis, IL-6 Release and NF-kappaB Activity in Human MDA-MB-231 Breast Cancer Cells. J. Nanosci. Nanotechnol. 2015, 15, 6413–6422. [Google Scholar] [CrossRef] [Green Version]
- Jie, L.; Lang, D.; Kang, X.; Yang, Z.; Du, Y.; Ying, X. Superparamagnetic Iron Oxide Nanoparticles/Doxorubicin-Loaded Starch-Octanoic Micelles for Targeted Tumor Therapy. J. Nanosci. Nanotechnol. 2019, 19, 5456–5462. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.P.; Thuy, V.T.T.; Kim, D. Integration of iron oxide nanoparticles and polyaspartamide biopolymer for MRI image contrast enhancement and an efficient drug-delivery system in cancer therapy. Nanotechnology 2020, 31, 335712. [Google Scholar] [CrossRef] [PubMed]
- An, F.-F.; Zhang, X.-H. Strategies for Preparing Albumin-based Nanoparticles for Multifunctional Bioimaging and Drug Delivery. Theranostics 2017, 7, 3667–3689. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Guo, Q.; Peng, J.; Su, J.; Lu, X.; Zhao, Y.; Qian, Z. Doxorubicin-Conjugated Heparin-Coated Superparamagnetic Iron Oxide Nanoparticles for Combined Anticancer Drug Delivery and Magnetic Resonance Imaging. J. Biomed. Nanotechnol. 2016, 12, 1963–1974. [Google Scholar] [CrossRef] [PubMed]
- Widder, K.J.; Morris, R.M.; Poore, G.; Howard, D.P.; Senyei, A.E. Tumor remission in Yoshida sarcoma-bearing rats by selective targeting of magnetic albumin microspheres containing doxorubicin. Proc. Natl. Acad. Sci. USA 1981, 78, 579–581. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Ji, F.; Liu, R. The interaction of bovine serum albumin with doxorubicin-loaded superparamagnetic iron oxide nanoparticles: Spectroscope and molecular modelling identification. Nanotoxicology 2011, 7, 97–104. [Google Scholar] [CrossRef]
- Kucharczyk, K.; Rybka, J.D.; Hilgendorff, M.; Krupinski, M.; Slachcinski, M.; Mackiewicz, A.; Giersig, M.; Dams-Kozlowska, H. Composite spheres made of bioengineered spider silk and iron oxide nanoparticles for theranostics applications. PLoS ONE 2019, 14, e0219790. [Google Scholar] [CrossRef] [Green Version]
- Yu, M.K.; Kim, D.; Lee, I.-H.; So, J.-S.; Jeong, Y.Y.; Jon, S. Image-Guided Prostate Cancer Therapy Using Aptamer-Functionalized Thermally Cross-Linked Superparamagnetic Iron Oxide Nanoparticles. Small 2011, 7, 2241–2249. [Google Scholar] [CrossRef]
- Pooresmaeil, M.; Javanbakht, S.; Namazi, H.; Shaabani, A. Application or function of citric acid in drug delivery platforms. Med. Res. Rev. 2021, 42, 800–849. [Google Scholar] [CrossRef]
- Kumar, P.; Agnihotri, S.; Roy, I. Preparation and characterization of superparamagnetic iron oxide nanoparticles for magnetically guided drug delivery. Int. J. Nanomed. 2018, 13, 43–46. [Google Scholar] [CrossRef] [Green Version]
- Narmani, A.; Rezvani, M.; Farhood, B.; Darkhor, P.; Mohammadnejad, J.; Amini, B.; Refahi, S.; Goushbolagh, N.A. Folic acid functionalized nanoparticles as pharmaceutical carriers in drug delivery systems. Drug Dev. Res. 2019, 80, 404–424. [Google Scholar] [CrossRef] [PubMed]
- Unnikrishnan, B.; Sen, A.; Preethi, G.; Joseph, M.M.; Maya, S.; Shiji, R.; Anusree, K.; Sreelekha, T. Folic acid-appended galactoxyloglucan-capped iron oxide nanoparticles as a biocompatible nanotheranostic agent for tumor-targeted delivery of doxorubicin. Int. J. Biol. Macromol. 2021, 168, 130–142. [Google Scholar] [CrossRef] [PubMed]
- Norouzi, M.; Yathindranath, V.; Thliveris, J.A.; Kopec, B.M.; Siahaan, T.J.; Miller, D.W. Doxorubicin-loaded iron oxide nanoparticles for glioblastoma therapy: A combinational approach for enhanced delivery of nanoparticles. Sci. Rep. 2020, 10, 1–18. [Google Scholar] [CrossRef]
- Mihanfar, A.; Targhazeh, N.; Sadighparvar, S.; Darband, S.G.; Majidinia, M.; Yousefi, B. Doxorubicin loaded magnetism nanoparticles based on cyclodextrin dendritic-graphene oxide inhibited MCF-7 cell proliferation. Biomol. Concepts 2021, 12, 8–15. [Google Scholar] [CrossRef]
- Gonzalez-Rodriguez, R.; Campbell, E.; Naumov, A. Multifunctional graphene oxide/iron oxide nanoparticles for magnetic targeted drug delivery dual magnetic resonance/fluorescence imaging and cancer sensing. PLoS ONE 2019, 14, e0217072. [Google Scholar] [CrossRef]
- Balcioglu, M.; Rana, M.; Yigit, M.V. Doxorubicin loading on graphene oxide, iron oxide and gold nanoparticle hybrid. J. Mater. Chem. B 2013, 1, 6187–6193. [Google Scholar] [CrossRef]
- Ramesh, N.; Moratti, S.C.; Dias, G.J. Hydroxyapatite-polymer biocomposites for bone regeneration: A review of current trends. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018, 106, 2046–2057. [Google Scholar] [CrossRef]
- Aval, N.A.; Islamian, J.P.; Hatamian, M.; Arabfirouzjaei, M.; Javadpour, J.; Rashidi, M.-R. Doxorubicin loaded large-pore mesoporous hydroxyapatite coated superparamagnetic Fe 3 O 4 nanoparticles for cancer treatment. Int. J. Pharm. 2016, 509, 159–167. [Google Scholar] [CrossRef]
- Lee, I.J.; Ahn, C.-H.; Cha, E.-J.; Chung, I.J.; Chung, J.W.; Kim, Y.I. Improved Drug Targeting to Liver Tumors After Intra-arterial Delivery Using Superparamagnetic Iron Oxide and Iodized Oil. Investig. Radiol. 2013, 48, 826–833. [Google Scholar] [CrossRef]
- Gholami, L.; Tafaghodi, M.; Abbasi, B.; Daroudi, M.; Oskuee, R.K. Preparation of superparamagnetic iron oxide/doxorubicin loaded chitosan nanoparticles as a promising glioblastoma theranostic tool. J. Cell. Physiol. 2018, 234, 1547–1559. [Google Scholar] [CrossRef]
- Chen, F.; Ilyas, N.; Liu, X.; Li, Z.; Yan, S.; Fu, H. Size Effect of Fe3O4 Nanoparticles on Magnetism and Dispersion Stability of Magnetic Nanofluid. Front. Energy Res. 2021, 9, 1–9. [Google Scholar] [CrossRef]
- Rodríguez-López, J.L.; Montejano-Carrizales, J.M.; Palomares-Báez, J.P.; Barrón-Escobar, H.; Velázquez-Salazar, J.J.; Cabrera-Trujillo, J.M.; José-Yacamán, M. Size effect and shape stability of nanoparticles. In Key Engineering Materials; Trans Tech Publications Ltd.: Wollerau, Switzerland, 2010; Volume 444, pp. 47–68. [Google Scholar]
- Das, S.; Bandyopadhyay, K.; Ghosh, M.M. Effect of stabilizer concentration on the size of silver nanoparticles synthesized through chemical route. Inorg. Chem. Commun. 2021, 123, 108319. [Google Scholar] [CrossRef]
- Ball, R.L.; Bajaj, P.; A Whitehead, K. Achieving long-term stability of lipid nanoparticles: Examining the effect of pH, temperature, and lyophilization. Int. J. Nanomed. 2016, 12, 305–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halder, S.; Ahmed, A.N.; Gafur, M.A.; Seong, G.; Hossain, M.Z. Size-Controlled Facile Synthesis of Silver Nanoparticles by Chemical Reduction Method and Analysis of Their Antibacterial Performance. ChemistrySelect 2021, 6, 9714–9720. [Google Scholar] [CrossRef]
- Mohapatra, S.; Asfer, M.; Anwar, M.; Sharma, K.; Akhter, M.; Ahmad, F.; Siddiqui, A.A. Doxorubicin loaded carboxymethyl Assam bora rice starch coated superparamagnetic iron oxide nanoparticles as potential antitumor cargo. Heliyon 2019, 5, e01955. [Google Scholar] [CrossRef] [Green Version]
- Schneider, M.G.M.; Martín, M.J.; Otarola, J.; Vakarelska, E.; Simeonov, V.; Lassalle, V.; Nedyalkova, M. Biomedical Applications of Iron Oxide Nanoparticles: Current Insights Progress and Perspectives. Pharmaceutics 2022, 14, 204. [Google Scholar] [CrossRef]
- McDonough, C.N.D.; Tonyushkin, A. 1-D Imaging of a Superparamagnetic Iron Oxide Nanoparticle Distribution by a Single-Sided FFL Magnetic Particle Imaging Scanner. IEEE Trans. Magn. 2022, 58, 1–5. [Google Scholar] [CrossRef]
- Hodneland, E.; Keilegavlen, E.; Hanson, E.A.; Andersen, E.; Monssen, J.A.; Rørvik, J.; Leh, S.; Marti, H.P.; Lundervold, A.; Svarstad, E.; et al. In vivo detection of chronic kidney disease using tissue deformation fields from dynamic MR imaging. IEEE Trans. Biomed. Eng. 2018, 66, 1779–1790. [Google Scholar] [CrossRef]
- Arami, H.; Krishnan, K.M. Highly Stable Amine Functionalized Iron Oxide Nanoparticles Designed for Magnetic Particle Imaging (MPI). IEEE Trans. Magn. 2013, 49, 3500–3503. [Google Scholar] [CrossRef] [Green Version]
- Munir, M.; Setiawan, H.; Awaludin, R.; Kett, V.L. Aerosolised micro and nanoparticle: Formulation and delivery method for lung imaging. Clin. Transl. Imaging 2022, 1–18. [Google Scholar] [CrossRef]
- Ferguson, R.M.; Khandhar, A.P.; Kemp, S.J.; Arami, H.; Saritas, E.U.; Croft, L.R.; Konkle, J.; Goodwill, P.W.; Halkola, A.; Rahmer, J.; et al. Magnetic Particle Imaging With Tailored Iron Oxide Nanoparticle Tracers. IEEE Trans. Med. Imaging 2014, 34, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Radon, P.; Liebl, M.; Pömpner, N.; Stapf, M.; Wiekhorst, F.; Gitter, K.; Hilger, I.; Odenbach, S.; Trahms, L. Magnetic particle spectroscopy to determine the magnetic drug targeting efficiency of different magnetic nanoparticles in a flow phantom. IEEE Trans. Magn. 2015, 51, 1–4. [Google Scholar] [CrossRef]
- Ludewig, P.; Graeser, M.; Forkert, N.D.; Thieben, F.; Rández-Garbayo, J.; Rieckhoff, J.; Lessmann, K.; Förger, F.; Szwargulski, P.; Magnus, T.; et al. Magnetic particle imaging for assessment of cerebral perfusion and ischemia. WIREs Nanomed. Nanobiotechnol. 2021, 14, e1757. [Google Scholar] [CrossRef] [PubMed]
- Irfan, M.; Dogan, N. Comprehensive Evaluation of Magnetic particle Imaging (MPI) Scanners for Biomedical Applications (June 2022). IEEE Access 2022, 10, 86718–86732. [Google Scholar] [CrossRef]
- Qiao, H.; Jia, J.; Chen, W.; Di, B.; Scherman, O.A.; Hu, C. Magnetic Regulation of Thermo-Chemotherapy from a Cucurbit[7]uril-Crosslinked Hybrid Hydrogel. Adv. Health Mater. 2018, 8, e1801458. [Google Scholar] [CrossRef]
- Wang, C.-H.; Kang, S.-T.; Yeh, C.-K. Superparamagnetic iron oxide and drug complex-embedded acoustic droplets for ultrasound targeted theranosis. Biomaterials 2013, 34, 1852–1861. [Google Scholar] [CrossRef]
- Yousef, M.; Al-Hamadani, M.; Kamel, M.A. Reproductive Toxicity of Aluminum Oxide Nanoparticles and Zinc Oxide Nanoparticles in Male Rats. Nanoparticle 2019, 1, 1–10. [Google Scholar] [CrossRef]
- Brohi, R.D.; Wang, L.; Talpur, H.S.; Wu, D.; Khan, F.A.; Bhattarai, D.; Rehman, Z.-U.; FarmanUllah, F.; Huo, L.-J. Toxicity of Nanoparticles on the Reproductive System in Animal Models: A Review. Front. Pharmacol. 2017, 8, 606. [Google Scholar] [CrossRef]
- Kumar, V.; Sharma, N.; Maitra, S.S. In vitro and in vivo toxicity assessment of nanoparticles. Int. Nano Lett. 2017, 7, 243–256. [Google Scholar] [CrossRef] [Green Version]
- Voigt, N.; Henrich-Noack, P.; Kockentiedt, S.; Hintz, W.; Tomas, J.; Sabel, B.A. Toxicity of polymeric nanoparticles in vivo and in vitro. J. Nanoparticle Res. 2014, 16, 1–13. [Google Scholar] [CrossRef]
- Jesus, S.; Schmutz, M.; Som, C.; Borchard, G.; Wick, P.; Borges, O. Hazard Assessment of Polymeric Nanobiomaterials for Drug Delivery: What Can We Learn From Literature So Far. Front. Bioeng. Biotechnol. 2019, 7, 261. [Google Scholar] [CrossRef] [PubMed]
- Kansara, K.; Kumar, A. Chapter 2- In vitro methods to assess the cellular toxicity of nanoparticles. In Nanotoxicity; Rajendran, S., Mukherjee, A., Nguyen, T.A., Godugu, C., Shukla, R.K., Eds.; Elsevier Ltd.: Amsterdam, The Netherlands, 2020; pp. 21–40. ISBN 9780128199435. [Google Scholar] [CrossRef]
- Lewinski, N.; Colvin, V.; Drezek, R. Cytotoxicity of Nanoparticles. Small 2008, 4, 26–49. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Nienhaus, K.; Nienhaus, G.U. Engineered nanoparticles interacting with cells: Size matters. J. Nanobiotechnology 2014, 12, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; Wang, J.; Jiang, K.; Chung, E.J. Improving kidney targeting: The influence of nanoparticle physicochemical properties on kidney interactions. J. Control. Release 2021, 334, 127–137. [Google Scholar] [CrossRef]
- Ma, K.; Li, W.; Zhu, G.; Chi, H.; Yin, Y.; Li, Y.; Zong, Y.; Guo, Z.; Wang, L.; Xu, W.; et al. PEGylated DOX-coated nano graphene oxide as pH-responsive multifunctional nanocarrier for targeted drug delivery. J. Drug Target. 2021, 29, 884–891. [Google Scholar] [CrossRef]
- Wang, C.; Chen, B.; Zou, M.; Cheng, G. Cyclic RGD-modified chitosan/graphene oxide polymers for drug delivery and cellular imaging. Colloids Surf. B Biointerfaces 2014, 122, 332–340. [Google Scholar] [CrossRef]
- Teimouri, M.; Nia, A.H.; Abnous, K.; Eshghi, H.; Ramezani, M. Graphene oxide–cationic polymer conjugates: Synthesis and application as gene delivery vectors. Plasmid 2016, 84–85, 51–60. [Google Scholar] [CrossRef]
- Han, S.; Su, L.; Zhai, M.; Ma, L.; Liu, S.; Teng, Y. A molecularly imprinted composite based on graphene oxide for targeted drug delivery to tumor cells. J. Mater Sci. 2019, 54, 3331–3341. [Google Scholar] [CrossRef]
- Pei, X.; Zhu, Z.; Gan, Z.; Chen, J.; Zhang, X.; Cheng, X.; Wan, Q.; Wang, J. PEGylated nano-graphene oxide as a nanocarrier for delivering mixed anticancer drugs to improve anticancer activity. Sci. Rep. 2020, 10, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Jiao, Z.; Zhang, B.; Li, C.; Kuang, W.; Zhang, J.; Xiong, Y.; Tan, S.; Cai, X.; Huang, L. Carboxymethyl cellulose-grafted graphene oxide for efficient antitumor drug delivery. Nanotech. Rev. 2018, 7, 291–301. [Google Scholar] [CrossRef]
- Zhang, L.; Ouyang, S.; Zhang, H.; Qiu, M.; Dai, Y.; Wang, S.; Wang, Y.; Ou, J. Graphene oxide induces dose-dependent lung injury in rats by regulating autophagy. Exp. Ther. Med. 2021, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Yang, J.; Huang, Q.; Zhang, Y.; Peng, C.; Zhang, Y.; He, Y.; Shi, J.; Li, W.; Hu, J.; et al. Biodistribution and pulmonary toxicity of intratracheally instilled graphene oxide in mice. NPG Asia Mater. 2013, 5, e44. [Google Scholar] [CrossRef] [Green Version]
- Malhotra, N.; Villaflores, O.B.; Audira, G.; Siregar, P.; Lee, J.-S.; Ger, T.-R.; Hsiao, C.-D. Toxicity Studies on Graphene-Based Nanomaterials in Aquatic Organisms: Current Understanding. Molecules 2020, 25, 3618. [Google Scholar] [CrossRef] [PubMed]
- Ou, L.; Song, B.; Liang, H.; Liu, J.; Feng, X.; Deng, B.; Sun, T.; Shao, L. Toxicity of graphene-family nanoparticles: A general review of the origins and mechanisms. Part. Fibre Toxicol. 2016, 13, 1–24. [Google Scholar] [CrossRef] [Green Version]
- Xiaoli, F.; Qiyue, C.; Weihong, G.; Yaqing, Z.; Chen, H.; Junrong, W.; Longquan, S. Toxicology data of graphene-family nanomaterials: An update. Arch. Toxicol. 2020, 94, 1915–1939. [Google Scholar] [CrossRef]
- Nowak-Jary, J.; Machnicka, B. Pharmacokinetics of magnetic iron oxide nanoparticles for medical applications. J. Nanobiotechnology 2022, 20, 1–30. [Google Scholar] [CrossRef]
- Volatron, J.; Carn, F.; Kolosnjaj-Tabi, J.; Javed, Y.; Vuong, Q.L.; Gossuin, Y.; Ménager, C.; Luciani, N.; Charron, G.; Hémadi, M.; et al. Ferritin protein regulates the degradation of iron oxide nanoparticles. Small 2017, 13, 1602030. [Google Scholar] [CrossRef]
- Zelepukin, I.V.; Yaremenko, A.V.; Ivanov, I.N.; Yuryev, M.V.; Cherkasov, V.R.; Deyev, S.M.; Nikitin, P.I.; Nikitin, M.P. Long-term fate of magnetic particles in mice: A comprehensive study. ACS Nano 2021, 15, 11341–11357. [Google Scholar] [CrossRef]
- Akhtar, K.; Shad, N.A.; Sajid, M.M.; Javed, Y.; Muhammad, F.; Akhtar, B.; Irfan Hussain, M.; Sharif, A.; Abbas, W.; Munawar, A. In vivo toxicity and biodegradation studies in mimicked biological media of bare and functionalised haematite nanoparticles. Adv. Appl. Ceram. 2021, 120, 287–299. [Google Scholar] [CrossRef]
- Wu, X.; Zhang, M. Toxic effects of iron oxide nanoparticles on human umbilical vein endothelial cells. Int. J. Nanomed. 2010, 5, 385–399. [Google Scholar] [CrossRef]
- Sukhanova, A.; Bozrova, S.; Sokolov, P.; Berestovoy, M.; Karaulov, A.; Nabiev, I. Dependence of Nanoparticle Toxicity on Their Physical and Chemical Properties. Nanoscale Res. Lett. 2018, 13, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casalini, T.; Limongelli, V.; Schmutz, M.; Som, C.; Jordan, O.; Wick, P.; Borchard, G.; Perale, G. Molecular Modeling for Nanomaterial-Biology Interactions: Opportunities, Challenges, and Perspectives. Front. Bioeng. Biotechnol. 2019, 7, 268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roman, D.L.; Roman, M.; Som, C.; Schmutz, M.; Hernandez, E.; Wick, P.; Casalini, T.; Perale, G.; Ostafe, V.; Isvoran, A. Computational Assessment of the Pharmacological Profiles of Degradation Products of Chitosan. Front. Bioeng. Biotechnol. 2019, 7, 214. [Google Scholar] [CrossRef] [PubMed]
- Schmutz, M.; Borges, O.; Jesus, S.; Borchard, G.; Perale, G.; Zinn, M.; Sips, A.; Soeteman-Hernandez, L.G.; Wick, P.; Som, C. A Methodological Safe-by-Design Approach for the Development of Nanomedicines. Front. Bioeng. Biotechnol. 2020, 8, 258. [Google Scholar] [CrossRef] [PubMed]




| Polymer | Coating/Capping | Observations | Reference |
|---|---|---|---|
| Polyethylene glycol (PEG) | Phospholipid | 30.8% w/w loading capacity observed with optimized PEG lengths | [26] |
| Silyls | Significant cytotoxicity (97.3 ± 0.8%) of SPIONs achieved | [27] | |
| Anti-IL4R blocking antibodies | Significant increase in cell death, apoptosis, and oxidative stress through SPIONs-IL4R-alpha and DOX | [28] | |
| pH-sensitive acyl hydrazone linkages | Better antitumor effect under magnetic field using SPIONs | [29] | |
| Bovine serum albumin (BSA) | DOX-SPIONs absorption through a combination of electrostatic and hydrophobic interactions | [30] | |
| Chelators and tumor-targeting ligands | cRGD-conjugated SPIONs in vitro exhibited higher levels of cellular uptake than the cRGD-free product | [31] | |
| Amphiphilic polymers and fluorescent dye 5-FAM | Antibody HuCC49DeltaCH2 and fluorescent dye, 5-FAM, conjugated to PEG-iron oxide NPs (IONPs) | [32] | |
| Poly-lactic-co-glycolic acid (PLGA) | Folic acid | SPIONs reduced toxicity and improved diagnosis and treatment | [35] |
| Tween 80, Brij-35, Pluronic F68, or Vitamin E-TPGS (d-α-tocopheryl polyethylene glycol 1000 succinate) | SPIONs provided efficient loading of drugs and high value of relaxivity | [37] | |
| Perfluorocarbon gas | In vitro delivered DOX-SPIONs microtubules enhanced ultrasound/magnetic resonance | [38] | |
| Per fluorooctyl bromide | High photo-thermal cytotoxicity on SKBR3 cells using SPIONs | [40] | |
| Polyethylene glycol and poly-lactic-co-glycolic acid (PEG-PLGA) | Folate | SPIONs with synergistic cytotoxic effects in folate-overexpressing cells (HeLa and MDA-MB-231) | [42] |
| D,L-Lactide and glycolide | In vitro cytotoxicity showed no cytotoxicity of DOX-SPIONs, biocompatible | [44] | |
| Anti-EGFR monoclonal antibody | Significant reduction in the signal intensity of A431 cells treated with SPIONs | [55] | |
| Polyethylene glycol and 3-aminopropyl triethoxy silane (APTES) | Indium-111 (labeled) Trastuzumab | Active and passive tumor targeting by SPIONs-DOX through anti-HER2 (human epidermal growth factor receptor 2), trastuzumab antibody | [46] |
| Amino acid, serine | Significant differences in amount of serine coating and enhanced drug release behavior to A549 cells | [47] | |
| Polyethylene glycol and poly-ε-caprolactone | Disulfide bond linkage | Disulfide linkage responsible for co-polymer exhibited redox-responsive properties | [50] |
| DSPE-PEG 2000 | Indocyanine green (ICG) | DOX-SPIONs crossed the BBB and accumulated at tumor site, seen with in vivo fluorescence and MR imaging | [52] |
| Polyethylene glycol and cationic polyethylene imine (PEG-PEI) | Folic acid | Increased growth inhibition with DOX-FA-SPIONs on xenograft MCF-7 breast tumor in nude mice | [54] |
| Poly amido amine (rPAA) with PEG-dodecyl amine | Oleic acid | rPAA-SPIONs showed better performance in mice with xenograft MDA-MB-231 breast tumor models | [57] |
| Poly lactic acid and poly ethylene glycol (PLA-PEG) | Folic acid | Higher cellular uptake of DOX-loaded PLA–PEG–FA-SPIONs than DOX-loaded-PLA–PEG-SPIONs | [59] |
| Polyethylene-oxide-trimellitic-anhydride-chloride-folate (PEO-TMA-FA) | Folate | Tumor volume decreased 4-fold with DOX-SPIONs compared to the DOXIL® (commercial DOX) in rabbit models | [63] |
| Polyethylene imine (PEI) | Silica coat | Rapid release of DOX-SPIONs, instant tumor cell destruction | [68] |
| Polydopamine (PDA) | Glutathione disulfide (GS-SG) | Enhanced DOX loading efficiency at 243 mol/g achieved through SPIONs-PDA conjugation | [70] |
| Methoxy-PEG (mPEG)-PAMAM dendrimers | Hydrazine | Enhanced permeability of DOX to tumor by polymer-SPIONs conjugation | [80] |
| Polymer/Conjugating Entity | Coating/Capping | Observations | Reference |
|---|---|---|---|
| Chitosan | Poly-L-arginine-chitosan-triphosphate | Enhanced absorption of DOX at the optimum dose, validated by MRI imaging of C6 glioma cells | [110] |
| Dextran | β-Cyclodextrin | Optimized SPIONs formulation with a higher T(2) relaxivity, 436.8 Fe mM−1S−1 | [84] |
| Polyaspartamide | Biotin | SPIONs enhanced the transverse 1/T2 relaxation rate for cancer detection | [92] |
| Graphene oxide | Gold | Improved SPIONs relaxivity | [106] |
| N,N-dimethyl acrylamide | N-Acryloyl glycine methyl ester | DOX-conjugated particles delivered in the U-87 glioblastoma cell line | [73] |
| SPIONs-hollow mesoporous silica (HmSiO2-SPIONs) | Fe3O4 | DOX-SPIONs through HmSiO2 conjugation integrated into HeLa cells | [77] |
| 2-(2-Methoxy)ethyl methacrylate (MEO2MA) | Oligo(ethylene glycol) methacrylate (OEGMA) | DOX-SPIONs for cytotoxicity against SKOV-3 cells in human ovarian cancer | [78] |
| Polymer Conjugate/Modification/Coating | Size (nm) | Zeta Potential(mV) | Drug Loading (%) | Drug Release (h/%) | Reference |
|---|---|---|---|---|---|
| PEG 2000-DSPE | 22.9 | −38.19 | 4.86% | 37% (10 h) | [52] |
| DSPE-2000-phospholipid | 14 | - | 30.8%, w/w | 20% (2 h) | [26] |
| PEGylated | 44.6 ± 20.3 | −26.1 | 6.91± 0.47% | 33.4–42.0% (24 h) | [32] |
| PEGylated-Silica | 20 ± 3 | −2.27 | 69.3 ± 1.4% | 23 ± 2.2% (24 h) | [27] |
| PLA-PEG | 41.98 ± 3 | −25.6 | 79.6 ± 6.4% | 92% (2 h) | [59] |
| PLGA-perfluorooctyl bromide | 296 | - | 39 ± 1.45% | 100% (52 h) | [40] |
| PLGA-FA | 85 | - | - | 63.3% | [35] |
| PLGA-PEG-folate | 170 | ~-33 | - | ~4.47 folds | [42] |
| PLGA:PEG(4000) | 30–60 | −17.4 | 78% | 30.1% (12 h) | [44] |
| NIPAM-MAm-HmSiO2 | 100–300 nm | −19.0 | 95% | - | [77] |
| GO-APTES | 260 | −3.18 ± 1.07 | 61.42% | - | [105] |
| pDA-GSSG | 33 ± 5 | −26.1 | 78% | - | [70] |
| TMSP-EDT | 51.8 ± 1.3 | −27.3 ± 1.0 | 5 ± 0.05% | 42% (3 h) | [103] |
| Spider silk | 112 | −25.3 ± 0.9 | - | 80% (7 d) | [97] |
| Chondritin-4-sulfate (CS) | 91.2 | −49.1 ± 1.66 | - | 96.67% (24 h) | [88] |
| CM-ABRS | 205.6 ± 0.211 | −26.1 | 6% (w/w) | 68.23% (24 h) | [116] |
| Polymer Conjugate (Modified/Coated) | Cytotoxicity (Cells Viability, %) | IC50 | Cell Line | Reference |
|---|---|---|---|---|
| PEG-PAMAM | 28–50% | 32 µM | Caco-2 | [56] |
| DSPE-PEG 2000 | 90% | 100 µg/mL | U251 | [52] |
| DSPE-2000-phospholipid | 64 ± 11% | 2.42 μg/ml | HeLa | [26] |
| PEGylated-silica | 88 ± 5.2% | 500 μg/mL | L929 | [27] |
| PEG and PEI-FA | 60% | 4 μg/mL | MCF-7 | [54] |
| PLA-PEG-FA | 82.83 ± 4.1% | 5 mg/mL | HeLa | [59] |
| PLGA-FA | 60% | 0.132 μM | A549 | [35] |
| Chondritin-4-sulfate | 98% | 7.1 mm | A2780 | [86] |
| GO-APTES | 37% | ~0.3 μg/mL | HeLa | [105] |
| GO-β-CD | 50% | 1 μM | MCF-7 | [104] |
| pDA-GSSG | 37.1 ± 9.5% | 334.4–836.1 nM | PC3 | [70] |
| TMSP-EDT | 40% | 300 ng/mL | U251 | [103] |
| CM-ABRS | 50% | 5.9 ± 0.13 μg/mL | HeLa | [116] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akhtar, N.; Mohammed, H.A.; Yusuf, M.; Al-Subaiyel, A.; Sulaiman, G.M.; Khan, R.A. SPIONs Conjugate Supported Anticancer Drug Doxorubicin’s Delivery: Current Status, Challenges, and Prospects. Nanomaterials 2022, 12, 3686. https://doi.org/10.3390/nano12203686
Akhtar N, Mohammed HA, Yusuf M, Al-Subaiyel A, Sulaiman GM, Khan RA. SPIONs Conjugate Supported Anticancer Drug Doxorubicin’s Delivery: Current Status, Challenges, and Prospects. Nanomaterials. 2022; 12(20):3686. https://doi.org/10.3390/nano12203686
Chicago/Turabian StyleAkhtar, Naseem, Hamdoon A. Mohammed, Mohammed Yusuf, Amal Al-Subaiyel, Ghassan M. Sulaiman, and Riaz A. Khan. 2022. "SPIONs Conjugate Supported Anticancer Drug Doxorubicin’s Delivery: Current Status, Challenges, and Prospects" Nanomaterials 12, no. 20: 3686. https://doi.org/10.3390/nano12203686