Recent Advances in Wearable Optical Sensor Automation Powered by Battery versus Skin-like Battery-Free Devices for Personal Healthcare—A Review
Abstract
1. Introduction
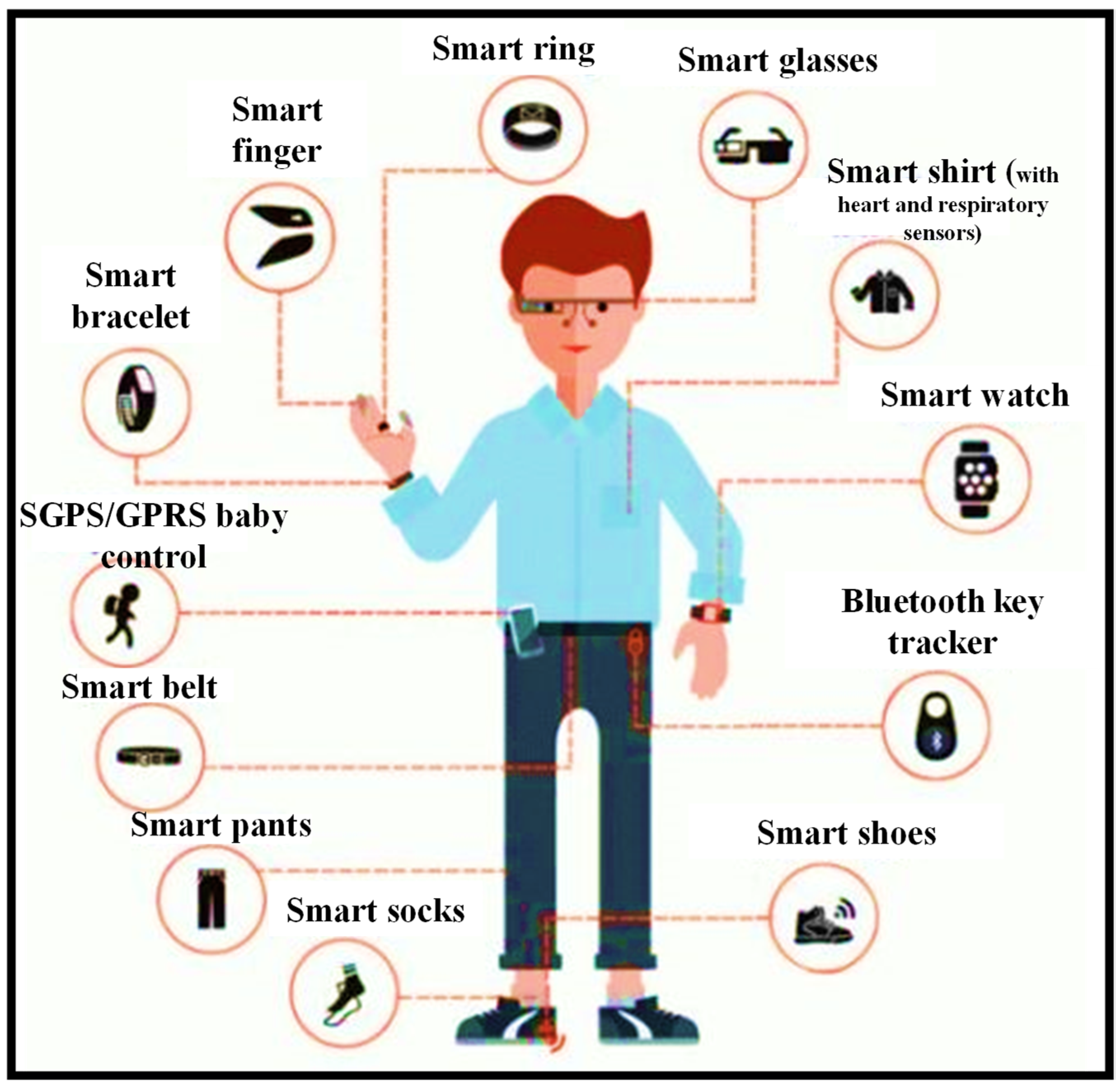
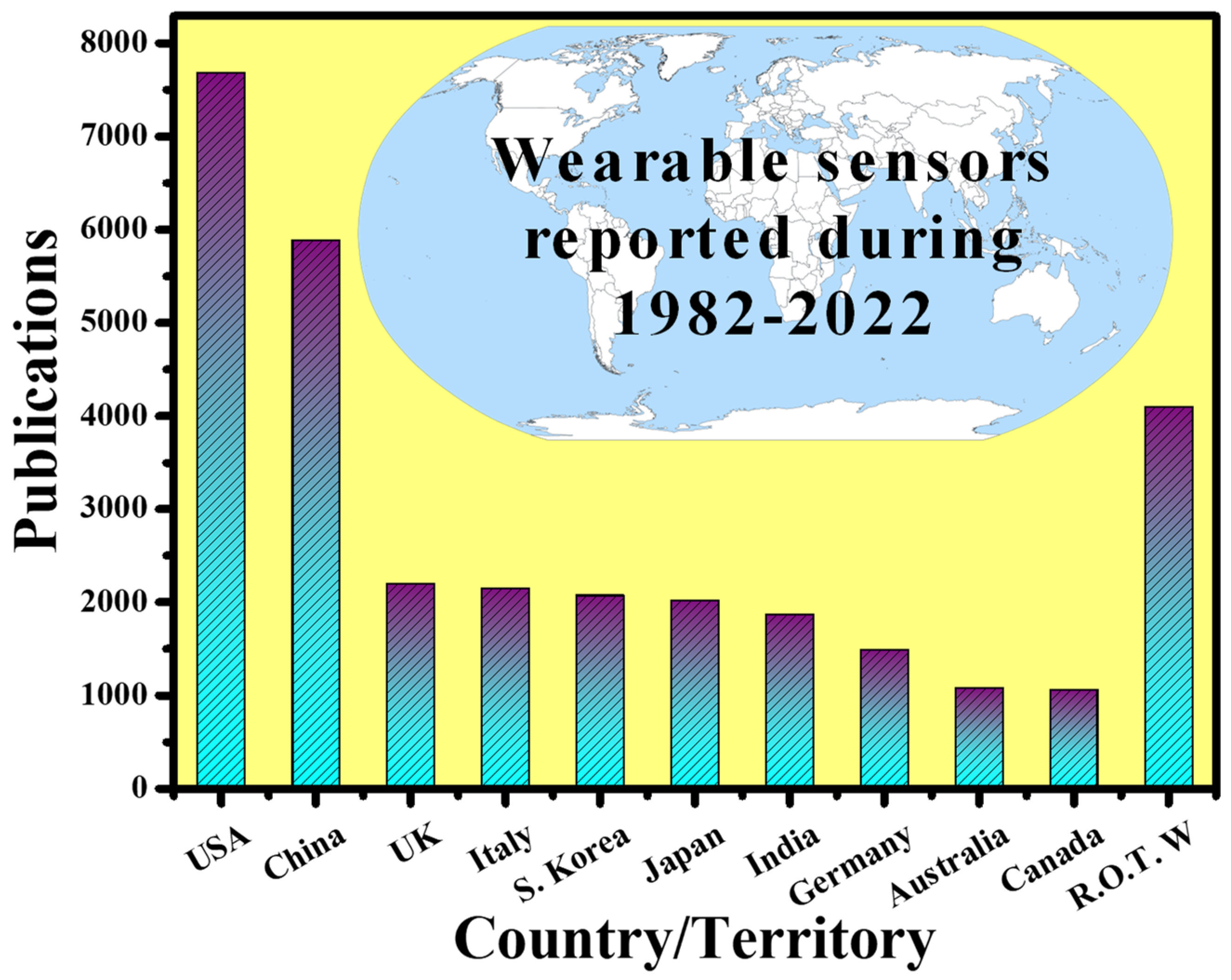
2. Demand for Wearable Optical Sensors
| Manufacturer | Model | Market | Cost (USD) | Form Factor | Sensors | US FDA Status | Ref. |
|---|---|---|---|---|---|---|---|
| Abbott | Libre | Ambulatory diabetes monitoring | 149.98 (cost for reader and 10-day sensor) | Semi-invasive | CGM | Approved | [52,53] |
| AliveCor | Kardia Band | Consumer | 199 | Wristband | ECG | Cleared | [54] |
| Apple | Watch Series 3 | Consumer | 329 | Watch | Accel, ambient light sensor, BALT, Gyro, PPG HR, GPS | Pre-certified | [55] |
| Ava Science, Inc | Ava Wristband | Consumer | 249 | Wristband | Accel, EDA, PPG HR, Temperature sensors | Approved | [56] |
| Bloomlife | Smart Pregnancy tracker | Consumer (rental) | 20/week | Abdominal patch | Accel, 3-channel AFE | - | [56] |
| Preventice | Bodyguardian Heart | Ambulatory cardiac monitoring | Ordered through physician, billed directly to insurance | Chest patch | Accel, EFG | Cleared | [57] |
| Oura | Oura ring | Consumer | 299–999 | Ring | Accel, Gyro, PPG HR, Skin temperature | - | [58] |
| Orpyx | Surro Gait Rx | Ambulatory gait monitoring | Ordered through physician | Watch, shoe insert, shoe pod | Pressure | - | [59] |
| Orpyx | Surro Sense Rx | Ambulatory gait monitoring | Ordered through physician | Watch, shoe insert, shoe pod | Pressure | Cleared | [60] |
| iRhythm | Ziopatch | Ambulatory cardiac monitoring | Ordered through physician, billed directly to insurance | Chest patch | ECG | Cleared | [61] |
| Medtronic | Enlite | Ambulatory diabetes monitoring | - | Semi-invasive | CGM | Approved | [62] |
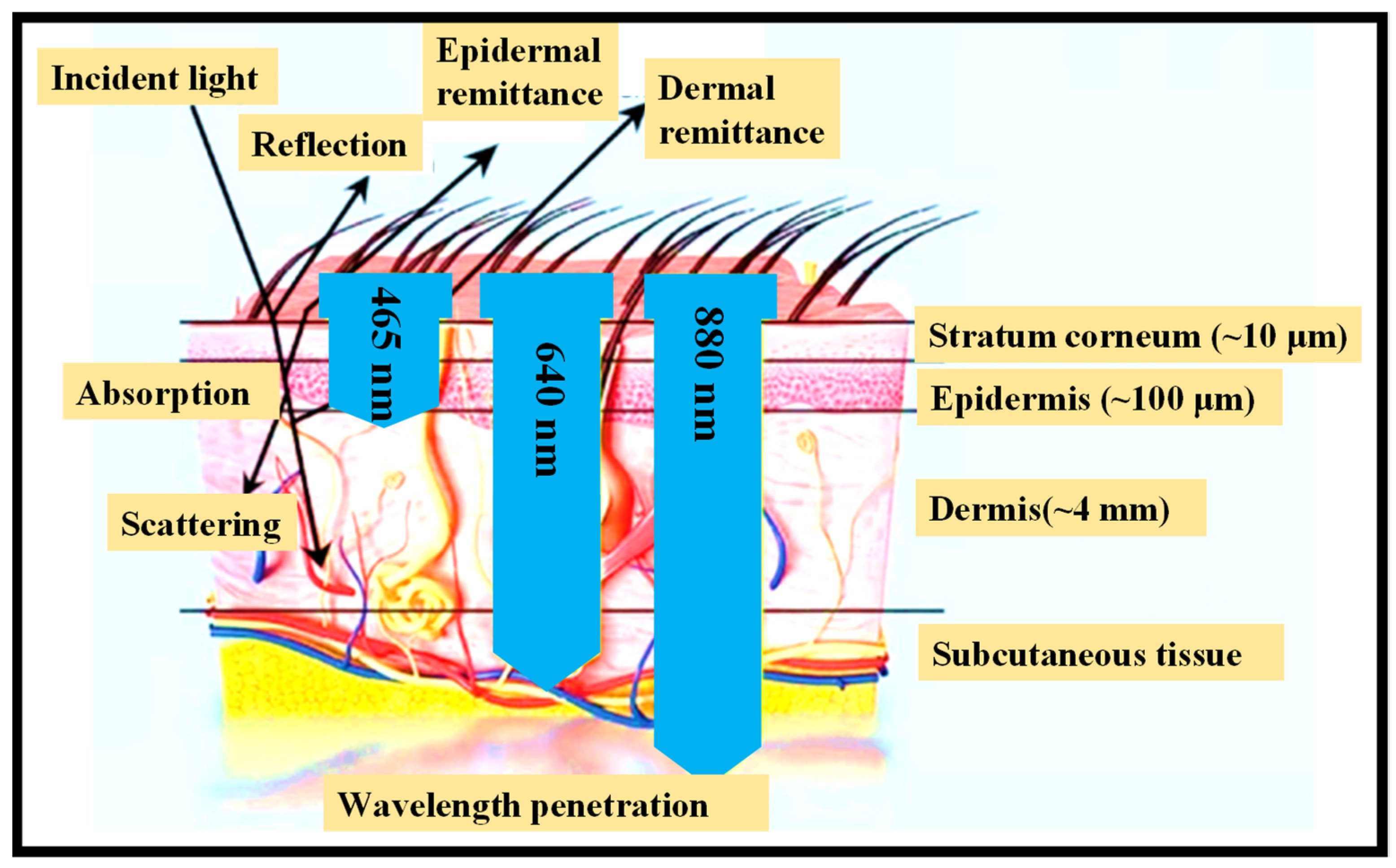
3. Working Mechanism of Unintrusive Optical Sensing Devices
- (1)
- The stratum corneum, which is extremely keratinized owing to the presence of dead squamous cells.
- (2)
- The hidden epidermis, which comprises skin pigmentation (mostly melanin) that absorbs shorter λ, such as UV, and visible (VIS) light to some extent [66].
- (3)
4. Continuous Body Tracking Devices Powered by Battery
4.1. Heart Rate Monitors (HRMs)
4.2. Continuous Glucose Monitoring (CGM)
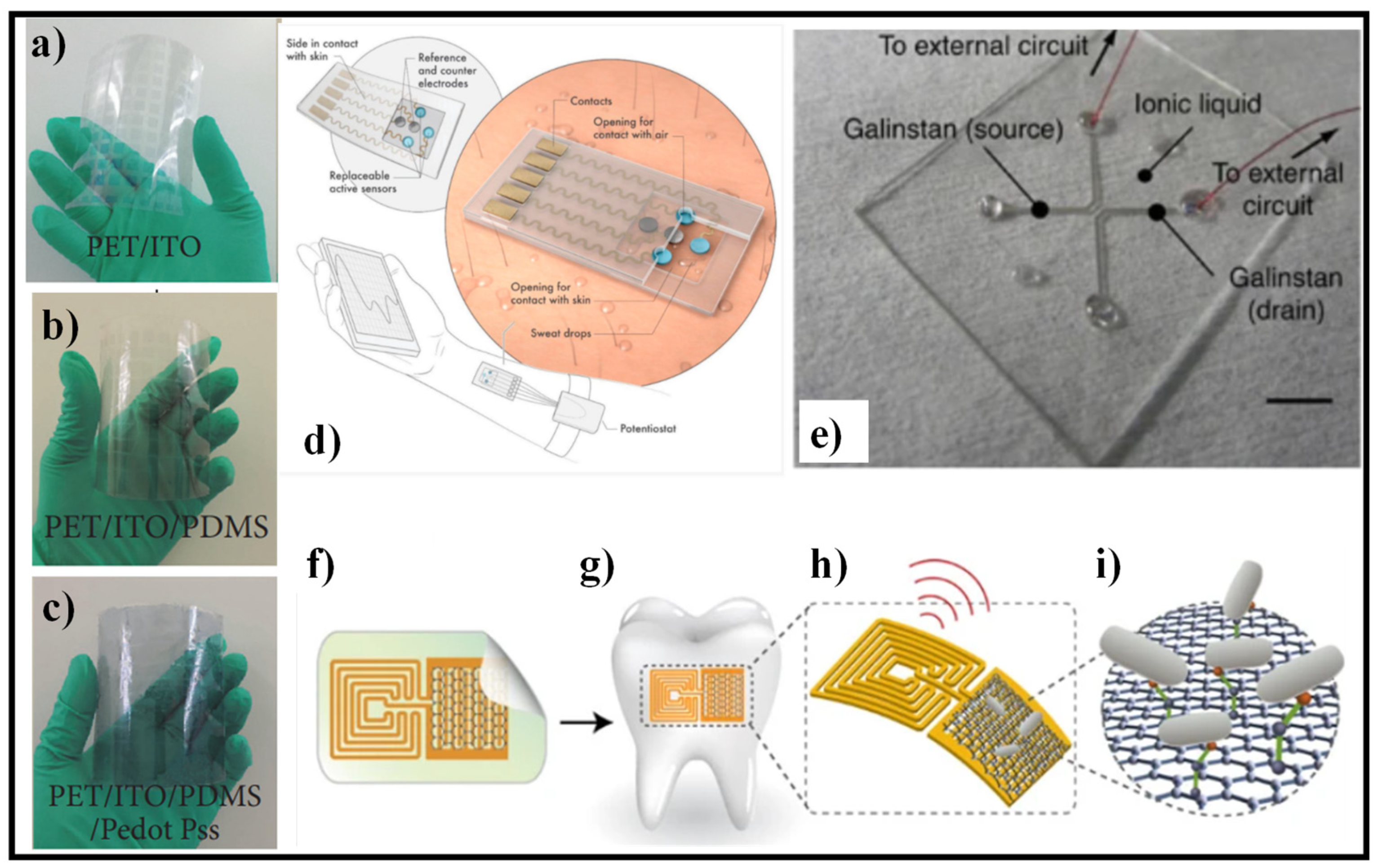
5. Skin-like Wearable Sensing Devices
5.1. Skin–Electronics Interface
- (i).
- Tattoo
- (ii).
- Band
- (iii).
- Textile
5.2. Materials and Structural Designs
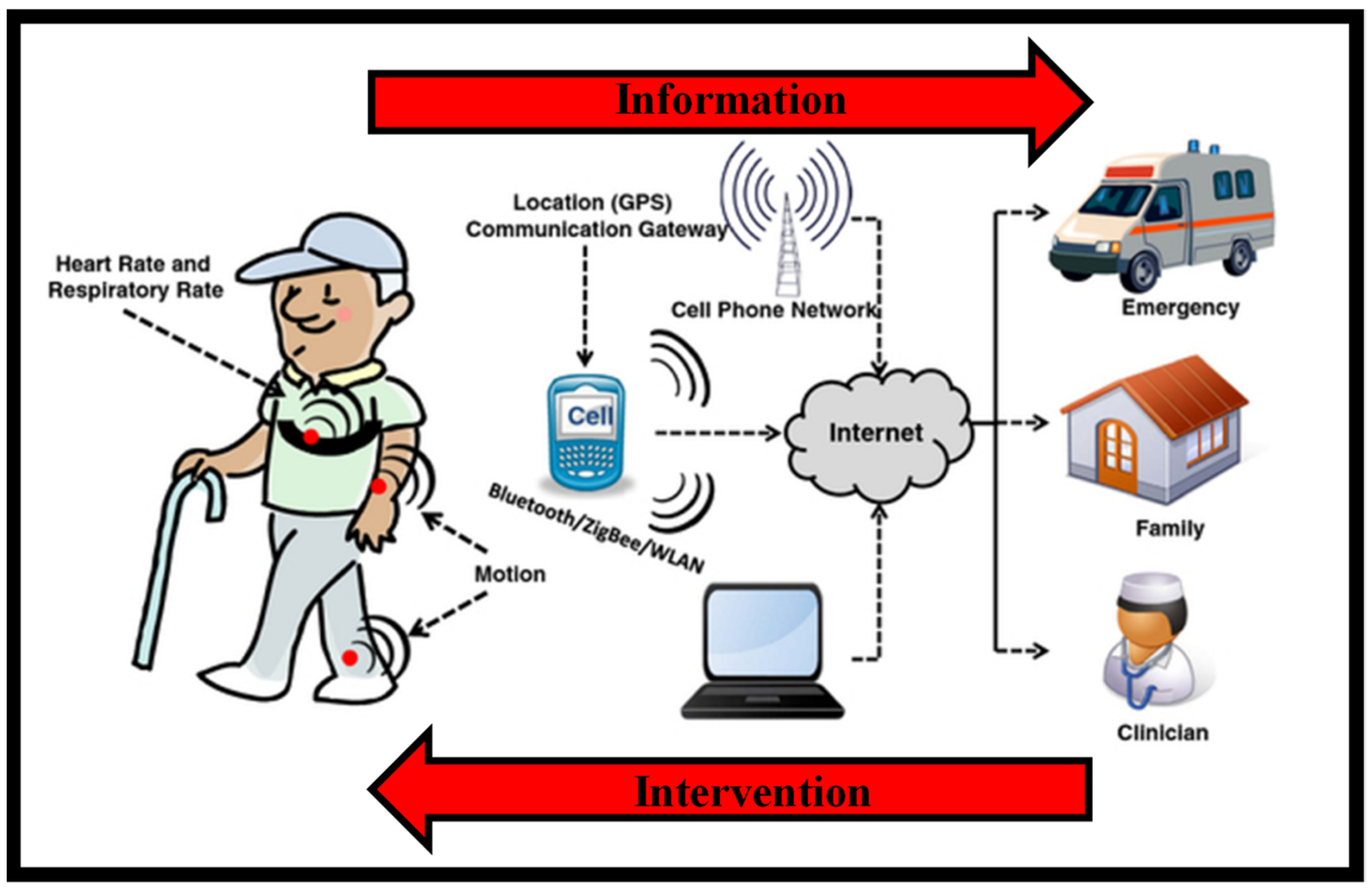
5.3. Communication and Data Analysis
5.4. Applications of Skin-like Sensors

6. Final Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Tricoli, A.; Nasiri, N.; De, S. Wearable and miniturized sensor technologies for personalized and preventive medicine. Adv. Funct. Mater. 2017, 27, 1605271. [Google Scholar] [CrossRef]
- Koymedir, H.; Ozcan, A. Wearable and implantable sensors for biomedical applications. Annu. Rev. Anal. Chem. 2018, 11, 127–146. [Google Scholar]
- Kenry; Yeo, J.C.; Lim, C.T. Emerging flexible and wearable physical sensing platforms for healthcare and biomedical applications. Microsyst. Nanoeng. 2016, 2, 16043. [Google Scholar] [CrossRef]
- Auepanwiriyakul, C.; Waibel, S.; Songa, J.; Bentley, P.; Faisal, A.A. Accuracy and Acceptability of Wearable Motion Tracking for Inpatient Monitoring Using Smartwatches. Sensors 2020, 20, 7313. [Google Scholar] [CrossRef]
- Fu, Y.; Liu, J. System Design for Wearable Blood Oxygen Saturation and Pulse Measurement Device. Procedia Manuf. 2015, 3, 1187–1194. [Google Scholar] [CrossRef]
- Casilari, E.; Álvarez-Marco, M.; García-Lagos, F. A Study of the Use of Gyroscope Measurements in Wearable Fall Detection Systems. Symmetry 2020, 12, 649. [Google Scholar] [CrossRef]
- Lim, G.B. Pacemaker powered by cardiac motion. Nat. Rev. Cardiol. 2019, 16, 386. [Google Scholar] [CrossRef] [PubMed]
- Haghjou, N.; Soheilian, M.; Abdekhodaie, M.J. Sustained Release Intraocular Drug Delivery Devices for Treatment of Uveitis. J. Ophthalmic Vis. Res. 2011, 6, 317–329. [Google Scholar]
- Lo, R.; Li, P.-Y.; Saati, S.; Agrawal, R.N.; Humayun, M.S.; Meng, E. A passive MEMS drug delivery pump for treatment of ocular diseases. Biomed. Microdevices 2009, 11, 959–970. [Google Scholar] [CrossRef] [PubMed]
- Manivasagam, G.; Dhinasekaran, D.; Rajamanickam, A. Biomedical implants: Corrosion and its prevention—A review. Recent Pat. Corros. Sci. 2010, 2, 40–54. [Google Scholar] [CrossRef]
- Msc, M.J.M.B.; Huizinga, E.; Van Loon, K.; Leenen, L.P.H.; Dohmen, D.A.J.; Kalkman, C.J.; Blokhuis, T.J. Reliability of wireless monitoring using a wearable patch sensor in high-risk surgical patients at a step-down unit in the Netherlands: A clinical validation study. BMJ Open 2018, 8, e020162. [Google Scholar] [CrossRef]
- Available online: https://www.sensortips.com/featured/where-are-wearable-sensors-worn/ (accessed on 1 December 2021).
- Moy, M.L.; Mentzer, S.J.; Reilly, J.J. Ambulatory monitoring of cumulative free-living activity. IEEE Eng. Med. Boil. Mag. 2003, 22, 89–95. [Google Scholar] [CrossRef]
- Sherrill, D.M.; Moy, M.L.; Reilly, J.J.; Bonato, P. Using hierarchical clustering methods to classify motor activities of COPD patients from wearable sensor data. J. Neuroeng. Rehabil. 2005, 2, 16. [Google Scholar] [CrossRef]
- Atallah, L.; Zhang, J.; Lo, B.P.; Shrikrishna, D.; Kelly, J.L.; Jackson, A.; Polkey, M.I.; Yang, G.-Z.; Hopkinson, N.S. Validation of an Ear Worn Sensor for Activity Monitoring in COPD. Am. J. Respir. Crit. Care Med. 2010, 181, A1211. [Google Scholar] [CrossRef]
- Steele, B.G.; Holt, L.; Belza, B.; Ferris, S.; Lakshminaryan, S.; Buchner, D.M. Quantitating Physical Activity in COPD Using a Triaxial Accelerometer. Chest 2000, 117, 1359–1367. [Google Scholar] [CrossRef]
- Belza, B.; Steele, B.G.; Hunziker, J.; Lakshminaryan, S.; Holt, L.; Buchner, D.M. Correlates of Physical Activity in Chronic Obstructive Pulmonary Disease. Nurs. Res. 2001, 50, 195–202. [Google Scholar] [CrossRef]
- Hecht, A.; Ma, S.; Porszasz, J.; Casaburi, R.; for the COPD Clinical Research Network. Methodology for Using Long-Term Accelerometry Monitoring to Describe Daily Activity Patterns in COPD. COPD J. Chronic Obstr. Pulm. Dis. 2009, 6, 121–129. [Google Scholar] [CrossRef]
- Patel, S.; Park, H.; Bonato, P.; Chan, L.; Rodgers, M. A review of wearable sensors and systems with application in rehabilitation. J. Neuroeng. Rehabil. 2012, 9, 21. [Google Scholar] [CrossRef]
- Nachiar, C.C.; Ambika, N.; Moulika, R.; Poovendran, R. Design of Cost-effective Wearable Sensors with integrated Health Monitoring System. In Proceedings of the Fourth International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud) (I-SMAC), Palladam, India, 7–9 October 2020; pp. 1289–1292. [Google Scholar] [CrossRef]
- Cappon, G.; Acciaroli, G.; Vettoretti, M.; Facchinetti, A.; Sparacino, G. Wearable Continuous Glucose Monitoring Sensors: A Revolution in Diabetes Treatment. Electronics 2017, 6, 65. [Google Scholar] [CrossRef]
- Jin, X.; Li, G.; Xu, T.; Su, L.; Yan, D.; Zhang, X. Fully integrated flexible biosensor for wearable continuous glucose monitoring. Biosens. Bioelectron. 2021, 196, 113760. [Google Scholar] [CrossRef]
- Butt, M.; Khonina, S.; Kazanskiy, N. Plasmonics: A Necessity in the Field of Sensing—A Review (Invited). Fiber Integr. Opt. 2021, 40, 14–47. [Google Scholar] [CrossRef]
- Butt, M.A.; Khonina, S.N.; Kazanskiy, N.L. Plasmonic refractive index sensor based on metal–insulator-metal waveguides with high sensitivity. J. Mod. Opt. 2019, 66, 1038–1043. [Google Scholar] [CrossRef]
- Butt, M.A.; Khonina, S.N.; Kazanskiy, N.L. Silicon on silicon dioxide slot waveguide evanescent field gas absorption sensor. J. Mod. Opt. 2017, 65, 174–178. [Google Scholar] [CrossRef]
- Butt, M.A. Numerical investigation of a small footprint plasmonic Bragg grating structure with a high extinction ratio. Photonics Lett. Pol. 2020, 12, 82–84. [Google Scholar] [CrossRef]
- Butt, M.A.; Khonina, S.N.; Kazanskiy, N.L. Sensitivity Enhancement of Silicon Strip Waveguide Ring Resonator by Incorporating a Thin Metal Film. IEEE Sens. J. 2020, 20, 1355–1362. [Google Scholar] [CrossRef]
- Butt, M.A.; Khonina, S.N.; Kazanskiy, N.L. Highly sensitive refractive index sensor based on hybrid plasmonic waveguide microring resonator. Waves Random Complex Media 2020, 30, 292–299. [Google Scholar] [CrossRef]
- Khonina, S.N.; Kazanskiy, N.L.; Butt, M.A. Evanescent Field Ratio Enhancement of a Modified Ridge Waveguide Structure for Methane Gas Sensing Application. IEEE Sens. J. 2020, 20, 8469–8476. [Google Scholar] [CrossRef]
- Butt, M.A.; Kazanskiy, N.L.; Khonina, S.N. Highly Sensitive Refractive Index Sensor Based on Plasmonic Bow Tie Configuration. Photonics Sens. 2020, 10, 223–232. [Google Scholar] [CrossRef]
- Leal-Junior, A.; Avellar, L.; Frizera, A.; Marques, C. Smart textiles for multimodal wearable sensing using highly stretchable multiplexed optical fiber system. Sci. Rep. 2020, 10, 13867. [Google Scholar] [CrossRef]
- Nguyen, T.-H.; Mugherli, L.; Rivron, C.; Tran-Thi, T.-H. Innovative colorimetric sensors for the selective detection of monochloramine in air and in water. Sens. Actuators B Chem. 2015, 208, 622–627. [Google Scholar] [CrossRef]
- Beutler, M.; Wiltshire, K.H.; Meyer, B.; Moldaenke, C.; Lüring, C.; Meyerhöfer, M.; Hansen, U.-P.; Dau, H. A fluorometric method for the differentiation of algal populations in vivo and in situ. Photosynth. Res. 2002, 72, 39–53. [Google Scholar] [CrossRef]
- Righini, G.C.; Krzak, J.; Lukowiak, A.; Macrelli, G.; Varas, S.; Ferrari, M. From flexible electronics to flexible photonics: A brief overview. Opt. Mater. 2021, 115, 111011. [Google Scholar] [CrossRef]
- Available online: Marketresearch.com (accessed on 1 December 2021).
- Tang, S.L.P. Wearable sensors for sports performance. Text. Sportsw. 2015, 169–196. [Google Scholar] [CrossRef]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable sensors for monitoring the physiological and biochemical profile of the athlete. NPJ Digit. Med. 2019, 2, 72. [Google Scholar] [CrossRef]
- Kwasnicki, R.M.; Chen, C.-M.; Noakes, A.J.; Hettiaratchy, S.; Yang, G.-Z.; Darzi, A. Developing a Wearable Sensor for Continuous Tissue Oxygenation Monitoring: A Proof of Concept Study. J. Reconstr. Microsurg. Open 2021, 6, e11–e19. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.; Deen, M.J. A Simple, Low-Cost and Efficient Gait Analyzer for Wearable Healthcare Applications. IEEE Sens. J. 2019, 19, 2320–2329. [Google Scholar] [CrossRef]
- Johnston, L.; Wang, G.; Hu, K.; Qian, C.; Liu, G. Advances in Biosensors for Continuous Glucose Monitoring Towards Wearables. Front. Bioeng. Biotechnol. 2021, 9, 733810. [Google Scholar] [CrossRef] [PubMed]
- Darwish, A.; Hassanien, A.E. Wearable and Implantable Wireless Sensor Network Solutions for Healthcare Monitoring. Sensors 2011, 11, 5561–5595. [Google Scholar] [CrossRef]
- Kong, M.; Li, Z.; Wu, J.; Hu, J.; Sheng, Y.; Wu, D.; Lin, Y.; Li, M.; Wang, X.; Wang, S. A wearable microfluidic device for rapid detection of HIV-1 DNA using recombinase polymerase amplification. Talanta 2019, 205, 120155. [Google Scholar] [CrossRef]
- Marquard, J.; Saver, B.; Kandaswamy, S.; Martinez, V.; Simoni, J.; Stekler, J.; Ganesan, D.; Scanlan, J. Designing a wrist-worn sensor to improve medication adherence: Accomodating diverse user behaviors and technology preferences. JAMIA Open 2018, 1, 153–158. [Google Scholar] [CrossRef]
- Varatharajan, R.; Manogaran, G.; Priyan, M.K.; Sundarasekar, R. Wearable sensor devices for early detection of Alzheimer disease using dynamic time warping algorithm. Clust. Comput. 2018, 21, 681–690. [Google Scholar] [CrossRef]
- Stavropoulos, T.G.; Lazarou, I.; Diaz, A.; Gove, D.; Georges, J.; Manyakov, N.V.; Pich, E.M.; Hinds, C.; Tsolaki, M.; Nikolopoulos, S.; et al. Wearable devices for assessing function in alzheimer’s disease: A european public involvement activity about the features and preferences of patients and caregivers. Front. Aging Neurosci. 2021, 13, 643135. [Google Scholar] [CrossRef]
- Parrilla, M.; Guinovart, T.; Ferré, J.; Blondeau, P.; Andrade, F.J. A Wearable Paper-Based Sweat Sensor for Human Perspiration Monitoring. Adv. Health Mater. 2019, 8, 1900342. [Google Scholar] [CrossRef]
- Cote, G.; Lec, R.; Pishko, M. Emerging biomedical sensing technologies and their applications. IEEE Sens. J. 2003, 3, 251–266. [Google Scholar] [CrossRef]
- Wang, S.; Oh, J.Y.; Xu, J.; Tran, H.; Bao, Z. Skin-Inspired Electronics: An Emerging Paradigm. Acc. Chem. Res. 2018, 51, 1033–1045. [Google Scholar] [CrossRef]
- Arif, M.; Kattan, A. Physical Activities Monitoring Using Wearable Acceleration Sensors Attached to the Body. PLoS ONE 2015, 10, e0130851. [Google Scholar] [CrossRef] [PubMed]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable sensors for monitoring the internal and external workload of the athlete. NPJ Digit. Med. 2019, 2, 71. [Google Scholar] [CrossRef]
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the medical revolution. Pers. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef] [PubMed]
- Boscari, F.; Galasso, S.; Acciaroli, G.; Facchinetti, A.; Marescotti, M.C.; Avogaro, A.; Bruttomesso, D. Head-to-head comparison of the accuracy of Abbott FreeStyle Libre and Dexcom G5 mobile. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 425–427. [Google Scholar] [CrossRef] [PubMed]
- Massa, G.G.; Gys, I.; Eyndt, A.O.; Bevilacqua, E.; Wijnands, A.; Declercq, P.; Zeevaert, R. Evaluation of the FreeStyle® Libre Flash Glucose Monitoring System in Children and Adolescents with Type 1 Diabetes. Horm. Res. Paediatr. 2018, 89, 189–199. [Google Scholar] [CrossRef]
- Halcox, J.P.; Wareham, K.; Cardew, A.; Gilmore, M.; Barry, J.P.; Phillips, C.; Gravenor, M.B. Assessment of remote heart rhythm sampling using the AliveCor heart monitor to screen for atrial fibrillation: The REHEARSE-AF study. Circulation 2017, 136, 1784–1794. [Google Scholar] [CrossRef] [PubMed]
- Tison, G.; Sanchez, J.M.; Ballinger, B.; Singh, A.; Olgin, J.E.; Pletcher, M.J.; Vittinghoff, E.; Lee, E.S.; Fan, S.M.; Gladstone, R.A.; et al. Passive Detection of Atrial Fibrillation Using a Commercially Available Smartwatch. JAMA Cardiol. 2018, 3, 409–416. [Google Scholar] [CrossRef]
- Shilaih, M.; Clerck, V.; Falco, L.; Kubler, F.; Leeners, B. Pulse rate measurement during sleep using wearable sensors, and its correlation with the menstrual cycle phases, a prospective observational study. Sci. Rep. 2017, 7, 1294. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, K.L.; Rowson, S.; Duma, S.M.; Broglio, S.P. Head-Impact–Measurement Devices: A Systematic Review. J. Athl. Train. 2017, 52, 206–227. [Google Scholar] [CrossRef] [PubMed]
- Zambotti, M.; Rosas, L.; Colrain, I.; Baker, F. The sleep of the ring: Comparison of the OURA sleep tracker against Polysomnography. Behav. Sleep Med. 2019, 17, 124–136. [Google Scholar] [CrossRef]
- Vienneau, J.; Bauman, J.; Nigg, S.; Nigg, B.; Jarvis, S. Investigating the effects of the SurroGait Rx device on postural stability, gait, and MSIS-29 outcomes in people with multiple sclerosis. Biomed. J. Sci. Tech. Res. 2018, 2, 2329. [Google Scholar] [CrossRef]
- Schlachetzki, J.C.M.; Barth, J.; Marxreiter, F.; Gossler, J.; Kohl, Z.; Reinfelder, S.; Gassner, H.; Aminian, K.; Eskofier, B.M.; Winkler, J.; et al. Wearable sensors objectively measure gait parameters in Parkinson’s disease. PLoS ONE 2017, 12, e0183989. [Google Scholar] [CrossRef]
- Solomon, M.D.; Yang, J.; Sung, S.H.; Livingston, M.L.; Sarlas, G.; Lenane, J.C.; Go, A.S. Incidence and timing of potentially high-risk arrhythmias detected through long term continuous ambulatory electrocardiographic monitoring. BMC Cardiovasc. Disord. 2016, 16, 35. [Google Scholar] [CrossRef]
- Sinha, M.; McKeon, K.M.; Parker, S.; Goergen, L.G.; Zheng, H.; El-Khatib, F.H.; Russell, S.J. A Comparison of Time Delay in Three Continuous Glucose Monitors for Adolescents and Adults. J. Diabetes Sci. Technol. 2017, 11, 1132–1137. [Google Scholar] [CrossRef] [PubMed]
- Jung, D.; Jung, D.; Kong, S. A lab-on-a-chip-based non-invasive optical sensor for measuring glucose in saliva. Sensors 2017, 17, 2607. [Google Scholar] [CrossRef]
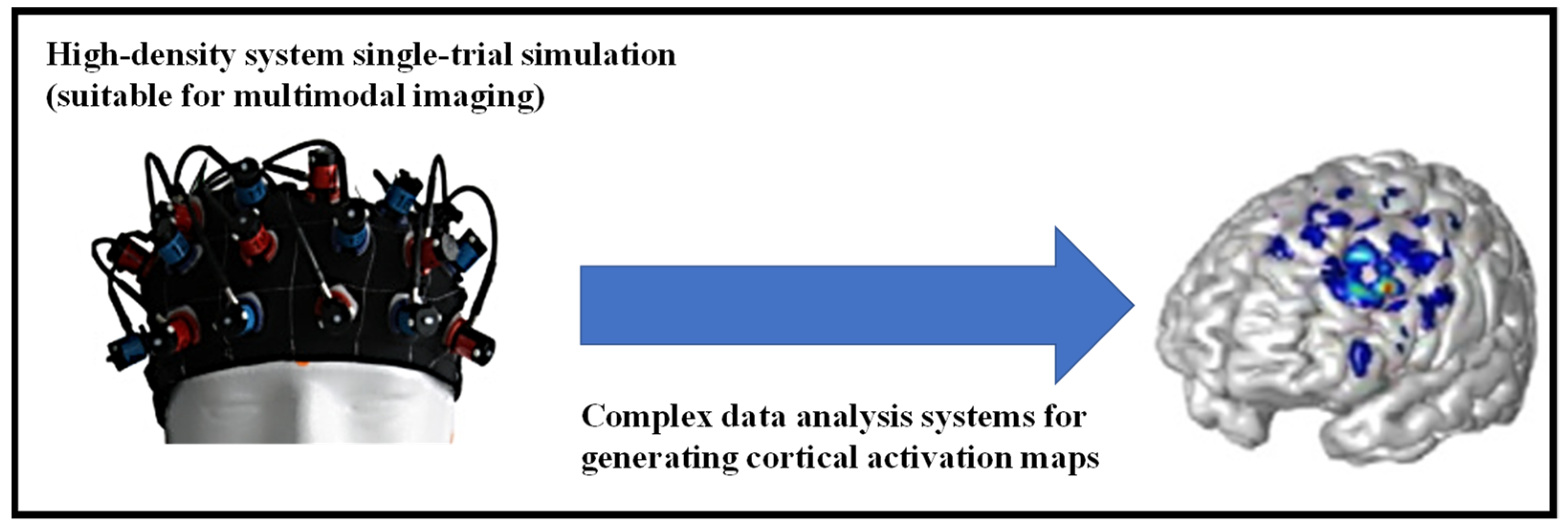
- Ferrari, M.; Quaresima, V. A brief review on the history of human functional near-infrared spectroscopy (fNIRS) development and fields of application. NeuroImage 2012, 63, 921–935. [Google Scholar] [CrossRef] [PubMed]
- Bashkatov, A.; Genina, E.; Kochubey, V.; Tuchin, V. Optical properties of human skin, subcutaneous and mucous tissues in the wavelength range from 400 to 2000 nm. J. Phys. D Appl. Phys. 2005, 38, 2543–2555. [Google Scholar] [CrossRef]
- Young, A.R. Chromophores in human skin. Phys. Med. Biol. 1997, 42, 789–802. [Google Scholar] [CrossRef]
- Goldsmith, L. Physiology, Biochemistry, and Molecular Biology of the Skin; Oxford University Press: New York, NY, USA, 1991. [Google Scholar]
- Tarar, A.; Mohammad, U.; Srivastava, S. Wearable skin sensors and their challenges: A review of transdermal, optical, and mechanical sensors. Biosensors 2020, 10, 56. [Google Scholar] [CrossRef]
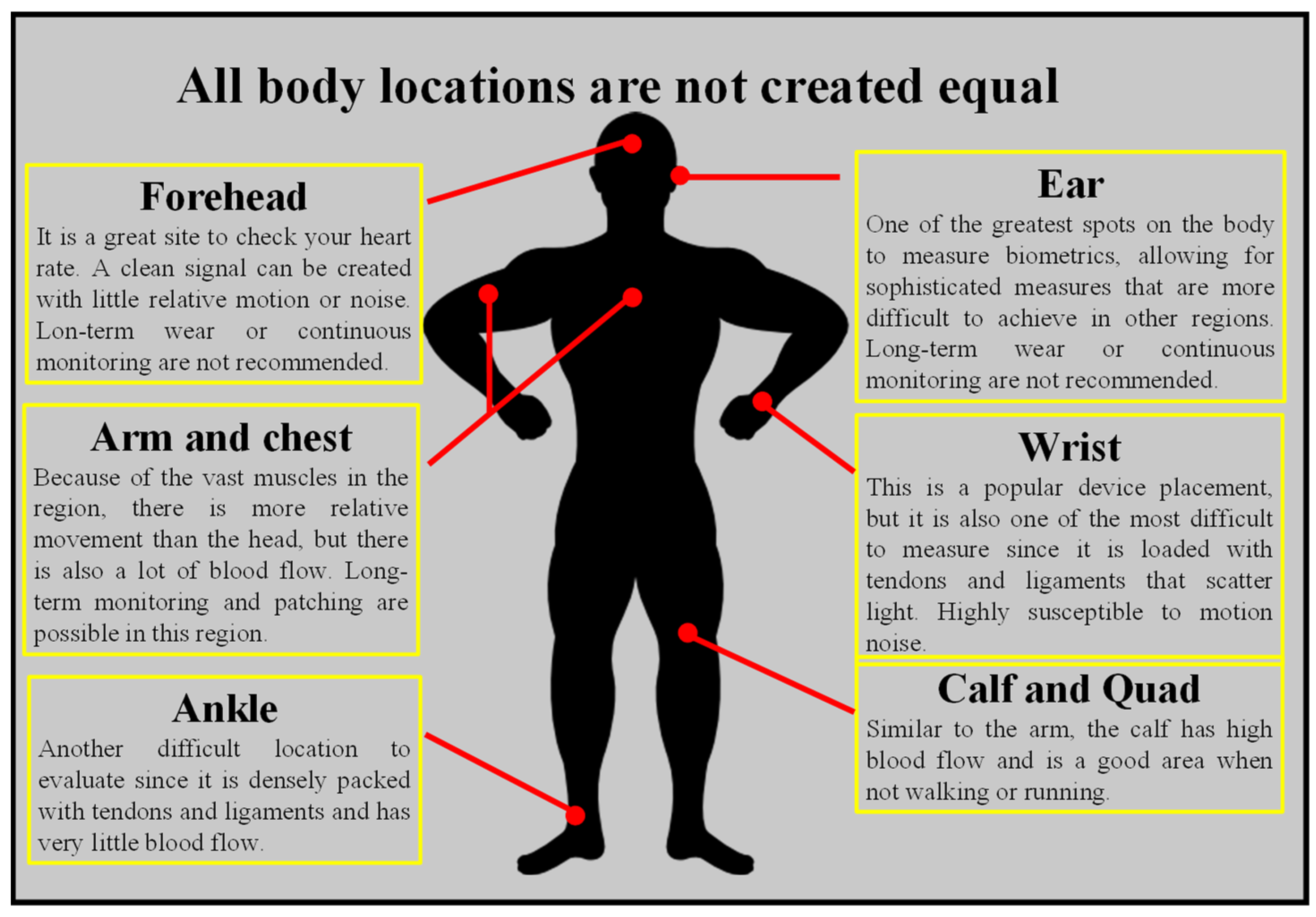
- Asada, H.H.; Shaltis, P.; Reisner, A.; Rhee, S.; Hutchinson, R.C. Mobile monitoring with wearable photoplethysmographic biosensors. IEEE Eng. Med. Biol. Mag. 2003, 22, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Moron, M.; Casilari, E.; Luque, R.; Gazquez, J.A. A Wireless Monitoring System for Pulse-Oximetry Sensors. In Proceedings of the International Conference on Systems Communications, Montreal, QC, Canada, 14–17 August 2005; pp. 79–84. [Google Scholar] [CrossRef]
- Kumar, S.; Buckley, J.L.; Barton, J.; Pigeon, M.; Newberry, R.; Rodencal, M.; Hajzeraj, A.; Hannon, T.; Rogers, K.; Casey, D.; et al. A Wristwatch-Based Wireless Sensor Platform for IoT Health Monitoring Applications. Sensors 2020, 20, 1675. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.-S.; Poon, C.C.; Zhang, Y.-T. Reduction of motion artifact in pulse oximetry by smoothed pseudo Wigner-Ville distribution. J. Neuroeng. Rehabil. 2005, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, Y.; Pujary, C. Measurement site and photodetector size considerations in optimizing power consumption of a wearable reflectance pulse oximeter. In Proceedings of the 25th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (IEEE Cat. No. 03CH37439), Cancun, Mexico, 17–21 September 2003; Volume 4, pp. 3016–3019. [Google Scholar] [CrossRef]
- Bent, B.; Goldstein, B.A.; Kibbe, W.A.; Dunn, J.P. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit. Med. 2020, 3, 18. [Google Scholar] [CrossRef]
- Pham, S.; Yeap, D.; Escalera, G.; Basu, R.; Wu, X.; Kenyon, N.J.; Hertz-Picciotto, I.; Ko, M.J.; Davis, C.E. Wearable Sensor System to Monitor Physical Activity and the Physiological Effects of Heat Exposure. Sensors 2020, 20, 855. [Google Scholar] [CrossRef]
- Millikan, G.A. The Oximeter, an Instrument for Measuring Continuously the Oxygen Saturation of Arterial Blood in Man. Rev. Sci. Instrum. 1942, 13, 434–444. [Google Scholar] [CrossRef]
- Severinghaus, J.W. Takuo Aoyagi: Discovery of Pulse Oximetry. Anesth. Analg. 2007, 105, S1–S4. [Google Scholar] [CrossRef]
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G.; et al. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, Y.; Duckworth, R.; Comtois, G. A wearable reflectance pulse oximeter for remote physiological monitoring. In Proceedings of the 28th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS ‘06, New York, NY, USA, 30 August–3 September 2006; pp. 912–915. [Google Scholar]
- Chow, H.-W.; Yang, C.-C. Accuracy of Optical Heart Rate Sensing Technology in Wearable Fitness Trackers for Young and Older Adults: Validation and Comparison Study. JMIR Mhealth Uhealth 2020, 8, e14707. [Google Scholar] [CrossRef]
- Colvonen, P.J. Response To: Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit. Med. 2021, 4, 38. [Google Scholar] [CrossRef]
- Guillodo, E.; Lemey, C.; Simonnet, M.; Walter, M.; Baca-García, E.; Masetti, V.; Moga, S.; Larsen, M.; Network, H.; Ropars, J.; et al. Clinical Applications of Mobile Health Wearable–Based Sleep Monitoring: Systematic Review. JMIR Mhealth Uhealth 2020, 8, e10733. [Google Scholar] [CrossRef] [PubMed]
- Ajmal, A.; Boonya-Ananta, T.; Rodriguez, A.J.; Du Le, V.N.; Ramella-Roman, J.C. Investigation of optical heart rate sensors in wearables and the influence of skin tone and obesity on photoplethysmography (PPG) signal. In Biophotonics in Exercise Science, Sports Medicine, Health Monitoring Technologies, and Wearables II; SPIE Photonics West: San Francisco, CA, USA, 2021; p. 1163808. [Google Scholar] [CrossRef]
- Smith, J.; Bawolek, E.; Lee, Y.; O’Brien, B.; Marrs, M.; Howard, E.; Strnad, M.; Christen, J.B.; Goryll, M. Application of flexible flat panel display technology to wearable biomedical devices. Electron. Lett. 2015, 51, 1312–1314. [Google Scholar] [CrossRef]
- Pasadyn, S.R.; Soudan, M.; Gillinov, M.; Houghtaling, P.; Phelan, D.; Gillinov, N.; Bittel, B.; Desai, M.Y. Accuracy of commercially available heart rate monitors in athletes: A prospective study. Cardiovasc. Diagn. Ther. 2019, 9, 379–385. [Google Scholar] [CrossRef]
- Choi, J.; Ghaffari, R.; Baker, L.B.; Rogers, J.A. Skin-interfaced systems for sweat collection and analytics. Sci. Adv. 2018, 4, eaar3921. [Google Scholar] [CrossRef]
- Heikenfeld, J.; Jajack, A.; Rogers, J.; Gutruf, P.; Tian, L.; Pan, T.; Li, R.; Khine, M.; Kim, J.; Wang, J. Wearable sensors: Modalities, challenges, and prospects. Lab Chip 2018, 18, 217–248. [Google Scholar] [CrossRef]
- Haddara, Y.M.; Howlader, M.M.R. Integration of Heterogeneous Materials for Wearable Sensors. Polymers 2018, 10, 60. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Swetha, P.; Zhu, Y. Nanomaterial-Enabled Wearable Sensors for Healthcare. Adv. Health Mater. 2018, 7, 1700889. [Google Scholar] [CrossRef]
- Someya, T.; Bao, Z.; Malliaras, G.G. The rise of plastic bioelectronics. Nature 2016, 540, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, B.A.; Piccini, J.P. Screening for Atrial Fibrillation with a Wearable Device. JAMA 2018, 320, 139–141. [Google Scholar] [CrossRef]
- Emaminejad, S.; Gao, W.; Wu, E.; Davies, Z.A.; Nyein, H.Y.Y.; Challa, S.; Ryan, S.P.; Fahad, H.M.; Chen, K.; Shahpar, Z.; et al. Autonomous sweat extraction and analysis applied to cystic fibrosis and glucose monitoring using a fully integrated wearable platform. Proc. Natl. Acad. Sci. USA 2017, 114, 4625–4630. [Google Scholar] [CrossRef]
- Domschke, A.M. Continuous non-invasive ophthalmic glucose sensor for diabetics. Chim. Int. J. Chem. 2010, 64, 43–44. [Google Scholar] [CrossRef]
- Wang, J. Electrochemical glucose biosensors. Chem. Rev. 2008, 108, 814–825. [Google Scholar] [CrossRef]
- Rum, L.; Sten, O.; Vendrame, E.; Belluscio, V.; Camomilla, V.; Vannozzi, G.; Truppa, L.; Notarantonio, M.; Sciarra, T.; Lazich, A.; et al. Wearable Sensors in Sports for Persons with Disability: A Systematic Review. Sensors 2021, 21, 1858. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Blackburn, G.; Desai, M.; Phelan, D.; Gillinov, L.; Houghtaling, P.; Gillinov, M. Accuracy of Wrist-Worn Heart Rate Monitors. JAMA Cardiol. 2017, 2, 104–106. [Google Scholar] [CrossRef]
- Gillinov, S.; Etiwy, M.; Wang, R.; Blackburn, G.; Phelan, D.; Gillinov, A.M.; Houghtaling, P.; Javadikasgari, H.; Desai, M.Y. Variable Accuracy of Wearable Heart Rate Monitors during Aerobic Exercise. Med. Sci. Sports Exerc. 2017, 49, 1697–1703. [Google Scholar] [CrossRef]
- Rothmaier, M.; Selm, B.; Spichtig, S.; Haensse, D.; Wolf, M. Photonic textiles for pulse oximetry. Opt. Express 2008, 16, 12973–12986. [Google Scholar] [CrossRef] [PubMed]
- Available online: www.polar.com (accessed on 1 December 2021).
- Available online: welcome.moov.cc (accessed on 1 December 2021).
- Available online: cosinuss.com (accessed on 1 December 2021).
- DiMeglio, L.A.; Evans-Molina, C.; Oram, R. Type 1 diabetes. Lancet 2018, 391, 2449–2462. [Google Scholar] [CrossRef]
- Olokoba, A.B.; Obateru, O.A.; Olokoba, L.B. Type 2 Diabetes Mellitus: A Review of Current Trends. Oman Med. J. 2012, 27, 269–273. [Google Scholar] [CrossRef]
- Clarke, S.F.; Foster, J.R. A history of blood glucose meters and their role in self-monitoring of diabetes mellitus. Br. J. Biomed. Sci. 2012, 69, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, I.B.; Wright, E.E. Using Flash Continuous Glucose Monitoring in Primary Practice. Clin. Diabetes 2019, 37, 150–161. [Google Scholar] [CrossRef][Green Version]
- Krakauer, M.; Botero, J.F.; Lavalle-González, F.J.; Proietti, A.; Barbieri, D.E. A review of flash glucose monitoring in type 2 diabetes. Diabetol. Metab. Syndr. 2021, 13, 42. [Google Scholar] [CrossRef]
- Schnell, O.; Hanefeld, M.; Monnier, L. Self-Monitoring of Blood Glucose. J. Diabetes Sci. Technol. 2014, 8, 609–614. [Google Scholar] [CrossRef]
- Kirk, J.K.; Stegner, J. Self-Monitoring of Blood Glucose: Practical Aspects. J. Diabetes Sci. Technol. 2010, 4, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Hong, Y.J.; Baik, S.; Hyeon, T.; Kim, D.-H. Enzyme-Based Glucose Sensor: From Invasive to Wearable Device. Adv. Healthc. Mater. 2018, 7, 1701150. [Google Scholar] [CrossRef] [PubMed]
- Ribet, F.; Stemme, G.; Roxhed, N. Ultra-miniaturization of a planar amperometric sensor targeting continuous intradermal glucose monitoring. Biosens. Bioelectron. 2017, 90, 577–583. [Google Scholar] [CrossRef]
- Chen, C.; Zhao, X.-L.; Li, Z.-H.; Zhu, Z.-G.; Qian, S.-H.; Flewitt, A.J. Current and Emerging Technology for Continuous Glucose Monitoring. Sensors 2017, 17, 182. [Google Scholar] [CrossRef]
- Colvin, A.; Jiang, H. Increased in vivo stability and functional lifetime of an implantable glucose sensor through platinum catalysis. J. Biomed. Mater. Res. Part A 2013, 101, 1274–1282. [Google Scholar] [CrossRef]
- Kropff, J.; Choudhary, P.; Neupane, S.; Barnard, K.; Bain, S.; Kapitza, C.; Forst, T.; Link, M.; Dehennis, A.; DeVries, J. Accuracy and longevity of an implantable continuous glucose sensor in the PRECISE study: A 180-day, prospective, multicenter, pivotal trial. Diabetes Care 2017, 40, 63–68. [Google Scholar] [CrossRef] [PubMed]
- DeHennis, A.; Mortellaro, M.A.; Ioacara, S. Multisite Study of an Implanted Continuous Glucose Sensor Over 90 Days in Patients with Diabetes Mellitus. J. Diabetes Sci. Technol. 2015, 9, 951–956. [Google Scholar] [CrossRef]
- Szadkowska, A.; Zozulińska-Ziółkiewicz, D.; Walczak, M.; Cyganek, K.; Wolnik, B.; Gawrecki, A.; Myśliwiec, M. Experts opinion: Implantable continuous glucose monitoring system—innovation in the management of diabetes. Clin. Diabetol. 2019, 8, 318–328. [Google Scholar] [CrossRef]
- Rachim, V.P.; Chung, W.-Y. Wearable-band type visible-near infrared optical biosensor for non-invasive blood glucose monitoring. Sens. Actuators B Chem. 2019, 286, 173–180. [Google Scholar] [CrossRef]
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. The emerging field of mobile health. Sci. Transl. Med. 2015, 7, 283rv3. [Google Scholar] [CrossRef]
- Montón, E.; Hernandez, J.; Blasco, J.; Hervé, T.; Micallef, J.; Grech, I.; Brincat, A.; Traver, V. Body area network for wireless patient monitoring. IET Commun. 2008, 2, 215–222. [Google Scholar] [CrossRef]
- Liu, X.; Wei, Y.; Qiu, Y. Advanced Flexible Skin-Like Pressure and Strain Sensors for Human Health Monitoring. Micromachines 2021, 12, 695. [Google Scholar] [CrossRef] [PubMed]
- Ying, B.; Liu, X. Skin-like hydrogel devices for wearable sensing, soft robotics and beyond. iScience 2021, 24, 103174. [Google Scholar] [CrossRef]
- Kim, D.-H.; Lu, N.; Ma, R.; Kim, Y.-S.; Kim, R.-H.; Wang, S.; Wu, J.; Won, S.M.; Tao, H.; Islam, A.; et al. Epidermal Electronics. Science 2011, 333, 838–843. [Google Scholar] [CrossRef]
- Miyamoto, A.; Lee, S.; Cooray, N.F.; Lee, S.; Mori, M.; Matsuhisa, N.; Jin, H.; Yoda, L.; Yokota, T.; Itoh, A.; et al. Inflammation-free, gas-permeable, lightweight, stretchable on-skin electronics with nanomeshes. Nat. Nanotechnol. 2017, 12, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.; Tee, B.C.-K.; Mei, J.; Appleton, A.L.; Kim, D.H.; Wang, H.; Bao, Z. Flexible polymer transistors with high pressure sensitivity for application in electronic skin and health monitoring. Nat. Commun. 2013, 4, 1859. [Google Scholar] [CrossRef]
- Gao, W.; Emaminejad, S.; Nyein, H.Y.Y.; Challa, S.; Chen, K.; Peck, A.; Fahad, H.M.; Ota, H.; Shiraki, H.; Kiriya, D.; et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature 2016, 529, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Lipani, L.; Dupont, B.G.R.; Doungmene, F.; Marken, F.; Tyrrell, R.M.; Guy, R.; Ilie, A. Non-invasive, transdermal, path-selective and specific glucose monitoring via a graphene-based platform. Nat. Nanotechnol. 2018, 13, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Pu, X.; Jiang, C.; Liu, T.; Huang, X.; Chen, L.; Du, C.; Sun, J.; Hu, W.; Wang, Z.L. Large-Area All-Textile Pressure Sensors for Monitoring Human Motion and Physiological Signals. Adv. Mater. 2017, 29, 1703700. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Lee, J.; Hyeon, T.; Lee, M.; Kim, D.-H. Fabric-Based Integrated Energy Devices for Wearable Activity Monitors. Adv. Mater. 2014, 26, 6329–6334. [Google Scholar] [CrossRef]
- Yang, J.; Mun, J.; Kwon, S.; Park, S.; Bao, Z.; Park, S. Electronic skin: Recent progress and future prospects for skin-attachable devices for health monitoring, robotics, and prosthetics. Adv. Mater. 2019, 31, 1904765. [Google Scholar] [CrossRef]
- Ladd, C.; So, J.-H.; Muth, J.; Dickey, M.D. 3D Printing of Free Standing Liquid Metal Microstructures. Adv. Mater. 2013, 25, 5081–5085. [Google Scholar] [CrossRef]
- Byun, S.-H.; Sim, J.Y.; Zhou, Z.; Lee, J.; Qazi, R.; Walicki, M.C.; Parker, K.E.; Haney, M.P.; Choi, S.H.; Shon, A.; et al. Mechanically transformative electronics, sensors, and implantable devices. Sci. Adv. 2019, 5, eaay0418. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, J.; Chen, S.; Lei, T.; Kim, Y.; Niu, S.; Wang, H.; Wang, X.; Foudeh, A.M.; Tok, J.B.-H.; et al. Soft and elastic hydrogel-based microelectronics for localized low-voltage neuromodulation. Nat. Biomed. Eng. 2019, 3, 58–68. [Google Scholar] [CrossRef]
- Cao, Y.; Morrissey, T.G.; Acome, E.; Allec, S.I.; Wong, B.M.; Keplinger, C.; Wang, C. A Transparent, Self-Healing, Highly Stretchable Ionic Conductor. Adv. Mater. 2017, 29, 1605099. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, C.; Pfattner, R.; Yan, H.; Jin, L.; Chen, S.; Molina-Lopez, F.; Lissel, F.; Liu, J.; Rabiah, N.I.; et al. A highly stretchable, transparent, and conductive polymer. Sci. Adv. 2017, 3, e1602076. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Sim, K.; Thukral, A.; Yu, C. Rubbery electronics and sensors from intrinsically stretchable elastomeric composites of semiconductors and conductors. Sci. Adv. 2017, 3, e1701114. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Xing, G.; Chai, Z. Are carbon nanotubes safe? Nat. Nanotechnol. 2008, 3, 191–192. [Google Scholar] [CrossRef]
- Maynard, A.D. Are we ready for spray-on carbon nanotubes? Nat. Nanotechnol. 2016, 11, 490–491. [Google Scholar] [CrossRef]
- Zou, Z.; Zhu, C.; Li, Y.; Lei, X.; Zhang, W.; Xiao, J. Rehealable, fully recyclable, and malleable electronic skin enabled by dynamic covalent thermoset nanocomposite. Sci. Adv. 2018, 4, eaaq0508. [Google Scholar] [CrossRef]
- Zhao, Y.; Huang, X. Mechanisms and Materials of Flexible and Stretchable Skin Sensors. Micromachines 2017, 8, 69. [Google Scholar] [CrossRef]
- Chen, L.; Chen, X.; Zhang, Z.; Li, T.; Zhao, T.; Li, X.; Zhang, J. PDMS-Based Capacitive Pressure Sensor for Flexible Transparent Electronics. J. Sens. 2019, 2019, 1418374. [Google Scholar] [CrossRef]
- Lei, D.; Liu, N.; Su, T.; Wang, L.; Su, J.; Zhang, Z.; Gao, Y. Research progress of MXenes-based wearable pressure sensors. APL Mater. 2020, 8, 110702. [Google Scholar] [CrossRef]
- Yiu, C.; Wong, T.; Liu, Y.; Yao, K.; Zhao, L.; Li, D.; Hai, Z.; Zheng, H.; Wang, Z.; Yu, X. Skin-Like Strain Sensors Enabled by Elastomer Composites for Human–Machine Interfaces. Coatings 2020, 10, 711. [Google Scholar] [CrossRef]
- Wang, C.; Yokota, T.; Someya, T. Natural Biopolymer-Based Biocompatible Conductors for Stretchable Bioelectronics. Chem. Rev. 2021, 121, 2109–2146. [Google Scholar] [CrossRef]
- Lei, Y.; Zhao, W.; Zhang, Y.; Jiang, Q.; He, J.; Baeumner, A.J.; Wolfbeis, O.S.; Wang, Z.L.; Salama, K.N.; Alshareef, H.N. A MXene-Based Wearable Biosensor System for High-Performance In Vitro Perspiration Analysis. Small 2019, 15, e1901190. [Google Scholar] [CrossRef] [PubMed]
- Ota, H.; Chen, K.; Lin, Y.; Kiriya, D.; Shiraki, H.; Yu, Z.; Ha, T.-J.; Javey, A. Highly deformable liquid-state heterojunction sensors. Nat. Commun. 2014, 5, 5032. [Google Scholar] [CrossRef]
- Mannoor, M.S.; Tao, H.; Clayton, J.D.; Sengupta, A.; Kaplan, D.L.; Naik, R.R.; Verma, N.; Omenetto, F.G.; McAlpine, M. Graphene-based wireless bacteria detection on tooth enamel. Nat. Commun. 2012, 3, 763. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Chen, P.; Ma, Z.; Li, S.; Gao, X.; Wu, R.-X.; Pan, L.; Shi, Y. Near-Field Communication Sensors. Sensors 2019, 19, 3947. [Google Scholar] [CrossRef]
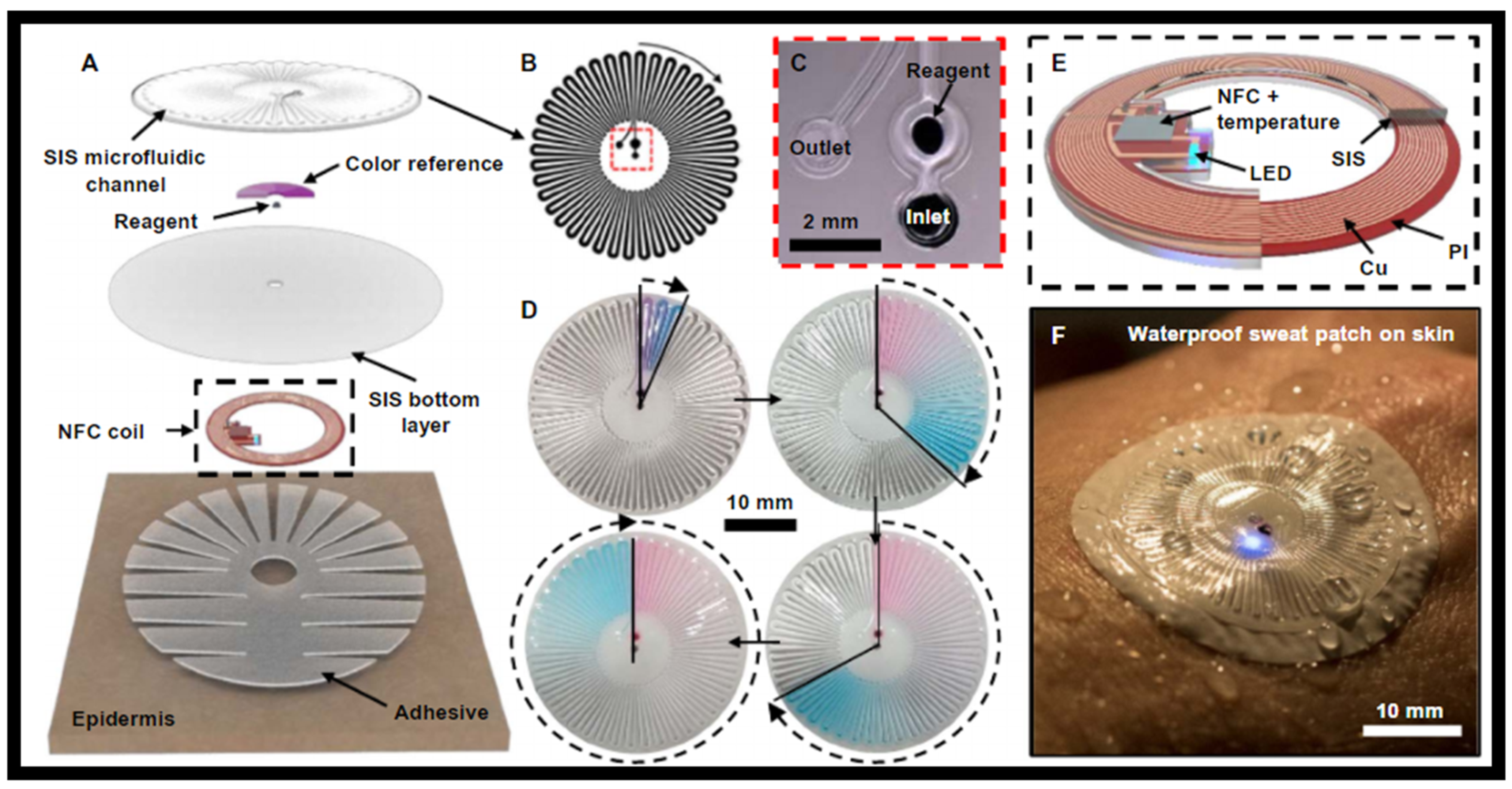
- Reeder, J.T.; Choi, J.; Xue, Y.; Gutruf, P.; Hanson, J.; Liu, M.; Ray, T.; Bandodkar, A.J.; Avila, R.; Xia, W.; et al. Waterproof, electronics-enabled, epidermal microfluidic devices for sweat collection, biomarker analysis, and thermography in aquatic settings. Sci. Adv. 2019, 5, eaau6356. [Google Scholar] [CrossRef]
- Bandodkar, A.J.; Gutruf, P.; Choi, J.; Lee, K.; Sekine, Y.; Reeder, J.T.; Jeang, W.J.; Aranyosi, A.J.; Lee, S.P.; Model, J.B.; et al. Battery-free, skin-interfaced microfluidic/electronic systems for simultaneous electrochemical, colorimetric, and volumetric analysis of sweat. Sci. Adv. 2019, 5, eaav3294. [Google Scholar] [CrossRef]
- Aguilar, S.; Vidal, R.; Gomez, C. Opportunistic Sensor Data Collection with Bluetooth Low Energy. Sensors 2017, 17, 159. [Google Scholar] [CrossRef]
- Costa, F.; Genovesi, S.; Borgese, M.; Michel, A.; Dicandia, F.; Manara, G. A Review of RFID Sensors, the New Frontier of Internet of Things. Sensors 2021, 21, 3138. [Google Scholar] [CrossRef]
- Niu, S.; Matsuhisa, N.; Beker, L.; Li, J.; Wang, S.; Wang, J.; Jiang, Y.; Yan, X.; Yun, Y.; Burnett, W.; et al. A wireless body area sensor network based on stretchable passive tags. Nat. Electron. 2019, 2, 361–368. [Google Scholar] [CrossRef]
- Kang, S.-G.; Song, M.-S.; Kim, J.-W.; Lee, J.; Kim, J. Near-Field Communication in Biomedical Applications. Sensors 2021, 21, 703. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Banks, A.; Cheng, H.; Xie, Z.; Xu, S.; Jang, K.-I.; Lee, J.W.; Liu, Z.; Gutruf, P.; Huang, X.; et al. Epidermal Electronics with Advanced Capabilities in Near-Field Communication. Small 2015, 11, 906–912. [Google Scholar] [CrossRef]
- Alruwaili, F.; Cluff, K.; Griffith, J.; Farhoud, H. Passive Self Resonant Skin Patch Sensor to Monitor Cardiac Intraventricular Stroke Volume Using Electromagnetic Properties of Blood. IEEE J. Transl. Eng. Health Med. 2018, 6, 1900709. [Google Scholar] [CrossRef] [PubMed]
- Pang, C.; Koo, J.H.; Nguyen, A.; Caves, J.M.; Kim, M.-G.; Chortos, A.; Kim, K.; Wang, P.J.; Tok, J.B.-H.; Bao, Z. Highly Skin-Conformal Microhairy Sensor for Pulse Signal Amplification. Adv. Mater. 2014, 27, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Krehel, M.; Wolf, M.; Boesel, L.; Rossi, R.; Bona, G.-L.; Scherer, L. Development of a luminous textile for reflective pulse oximetry measurements. Biomed. Opt. Express 2014, 5, 2537–2547. [Google Scholar] [CrossRef]
- Li, S.; Zhang, Y.; Wang, Y.; Xia, K.; Yin, Z.; Wang, H.; Zhang, M.; Liang, X.; Lu, H.; Zhu, M.; et al. Physical sensors for skin-inspired electronics. InfoMat 2019, 2, 184–211. [Google Scholar] [CrossRef]
- Lipomi, D.J.; Vosgueritchian, M.; Tee, B.C.K.; Hellstrom, S.L.; Lee, J.A.; Fox, C.H.; Bao, Z. Skin-like pressure and strain sensors based on transparent elastic films of carbon nanotubes. Nat. Nanotechnol. 2011, 6, 788–792. [Google Scholar] [CrossRef]
- Boutry, C.M.; Kaizawa, Y.; Schroeder, B.C.; Chortos, A.; Legrand, A.; Wang, Z.; Chang, J.; Fox, P.; Bao, Z. A stretchable and biodegradable strain and pressure sensor for orthopaedic application. Nat. Electron. 2018, 1, 314–321. [Google Scholar] [CrossRef]
- Lei, Z.; Wang, Q.; Wu, P. A multifunctional skin-like sensor based on a 3D printed thermo-responsive hydrogel. Mater. Horiz. 2017, 4, 694–700. [Google Scholar] [CrossRef]
- Wang, Y.-F.; Sekine, T.; Takeda, Y.; Yokosawa, K.; Matsui, H.; Kumaki, D.; Shiba, T.; Nishikawa, T.; Tokito, S. Fully Printed PEDOT: PSS-based Temperature Sensor with High Humidity Stability for Wireless Healthcare Monitoring. Sci. Rep. 2020, 10, 2467. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Dong, Z.; Li, Y.; Zhao, H.; Huang, X.; Zhou, Z.; Jiang, J.-W.; Long, Y.-Z.; Jiang, P.; Zhang, T.-Y.; et al. A high performance wearable strain sensor with advanced thermal management for motion monitoring. Nat. Commun. 2020, 11, 3530. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, R.; Mizuguchi, S.; Nakamura, F.; Endo, T.; Isoda, Y.; Inamori, G.; Ota, H. Highly strechable sensing array for independent detection of pressure and strain exploiting structural and resistive control. Sci. Rep. 2020, 10, 12666. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Wang, G.; Wu, Y.; Ren, X.; Gao, G. Ultrastretchable Wearable Strain and Pressure Sensors Based on Adhesive, Tough, and Self-healing Hydrogels for Human Motion Monitoring. ACS Appl. Mater. Interfaces 2019, 11, 25613–25623. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.S.; Kim, J.H.; Xie, Z.; Cho, S.; Han, H.; Jeon, S.W.; Park, M.; Namkoong, M.; Avila, R.; Song, Z.; et al. Battery-free, C continuous multi-site measurements of pressure and temperature from patients at risk for pressure injuries. Nat. Commun. 2021, 12, 5008. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.Y.; Son, D.; Katsumata, T.; Lee, Y.; Kim, Y.; Lopez, J.; Wu, H.-C.; Kang, J.; Park, J.; Gu, X.; et al. Stretchable self-healable semiconducting polymer film for active-matrix strain-sensing array. Sci. Adv. 2019, 5, eaav3097. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Harada, S.; Yamamoto, D.; Honda, W.; Arie, T.; Akita, S.; Takei, K. Printed multifunctional flexible device with an integrated motion sensor for health care monitoring. Sci. Adv. 2016, 2, e1601473. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kazanskiy, N.L.; Butt, M.A.; Khonina, S.N. Recent Advances in Wearable Optical Sensor Automation Powered by Battery versus Skin-like Battery-Free Devices for Personal Healthcare—A Review. Nanomaterials 2022, 12, 334. https://doi.org/10.3390/nano12030334
Kazanskiy NL, Butt MA, Khonina SN. Recent Advances in Wearable Optical Sensor Automation Powered by Battery versus Skin-like Battery-Free Devices for Personal Healthcare—A Review. Nanomaterials. 2022; 12(3):334. https://doi.org/10.3390/nano12030334
Chicago/Turabian StyleKazanskiy, Nikolay L., Muhammad A. Butt, and Svetlana N. Khonina. 2022. "Recent Advances in Wearable Optical Sensor Automation Powered by Battery versus Skin-like Battery-Free Devices for Personal Healthcare—A Review" Nanomaterials 12, no. 3: 334. https://doi.org/10.3390/nano12030334
APA StyleKazanskiy, N. L., Butt, M. A., & Khonina, S. N. (2022). Recent Advances in Wearable Optical Sensor Automation Powered by Battery versus Skin-like Battery-Free Devices for Personal Healthcare—A Review. Nanomaterials, 12(3), 334. https://doi.org/10.3390/nano12030334









