Nanoparticles: Taking a Unique Position in Medicine
Abstract
:1. Introduction
2. Generic Features of Nanoparticles in Medicine
2.1. Self-Organization of Nanoparticles
2.2. Nanoparticles and Healthcare
2.3. Nanoparticles and Human Health
2.4. Biomedical Nanoparticles
3. Applications of Nanoparticles in Medicine
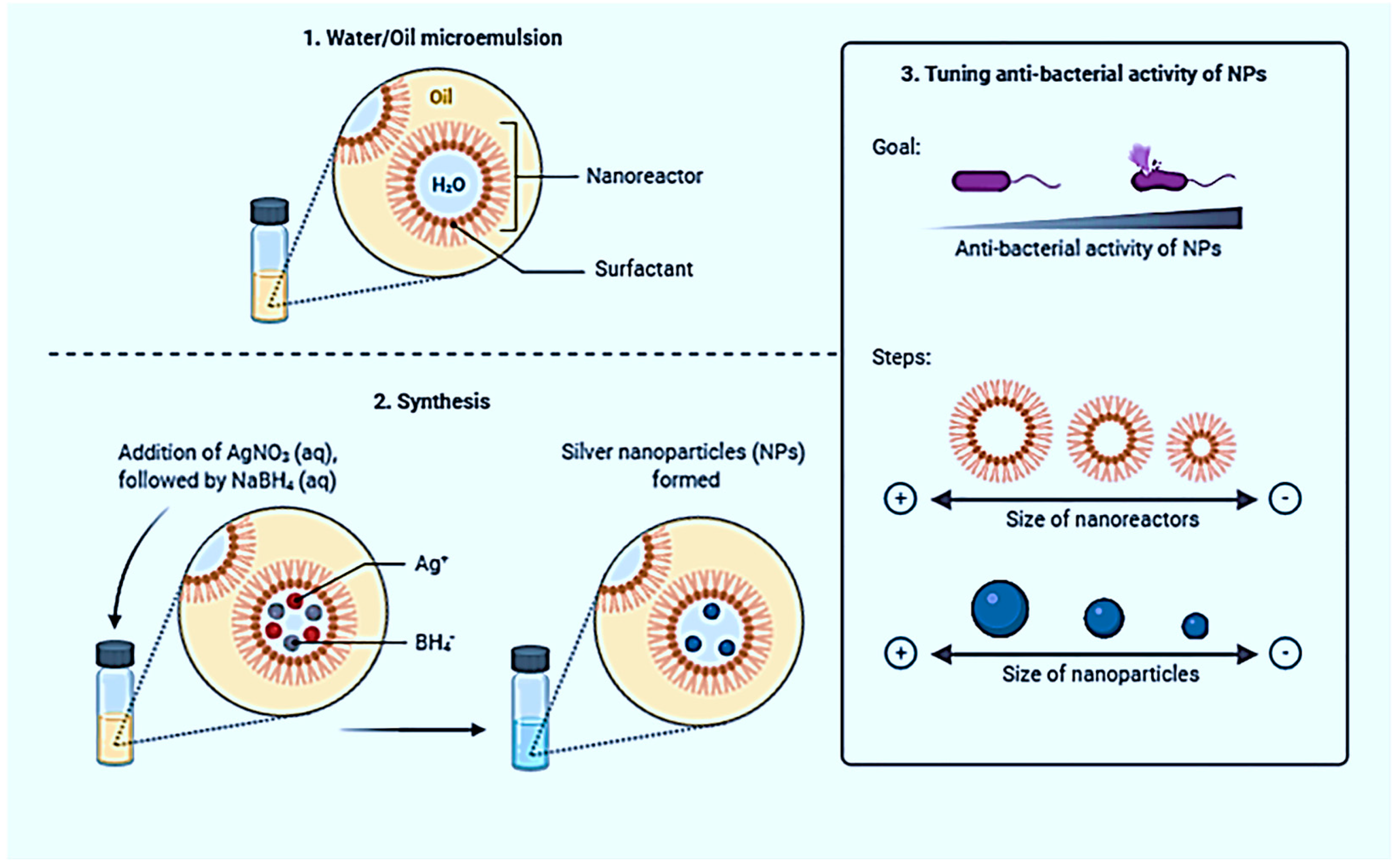
3.1. Silver Nanoparticles
3.2. Nano Zinc Oxide
3.3. Nano Silica
4. Nanotechnology in Pharmaceuticals and Medicine
- Biological screening, i.e., the search for active molecules (1–10 nm) that interact with a bio target (protein or a system of proteins up to 100 nm in size).
- Study the mechanism of action (search for a bio target and identify the mechanism of the reaction of an active molecule).
- Computer design of compounds that can be activated by estimating the energy of interaction between candidate molecules several nanometers apart and a bio target (protein), that is, calculating the possible structures and positions of the molecules corresponding to the minimum energy of such reaction at approximately 24 h of dynamic simulation of roughly 200 h.
- Component nanoscale targeted control and modification of components’ shape, size, reactivity, and integration (“ligand-biotarget”, approximately 1–100 nm), resulting in enhanced or additional functionality of products and consumer features (efficacy, bioavailability, and side effects of innovative drugs that reduce toxicity).
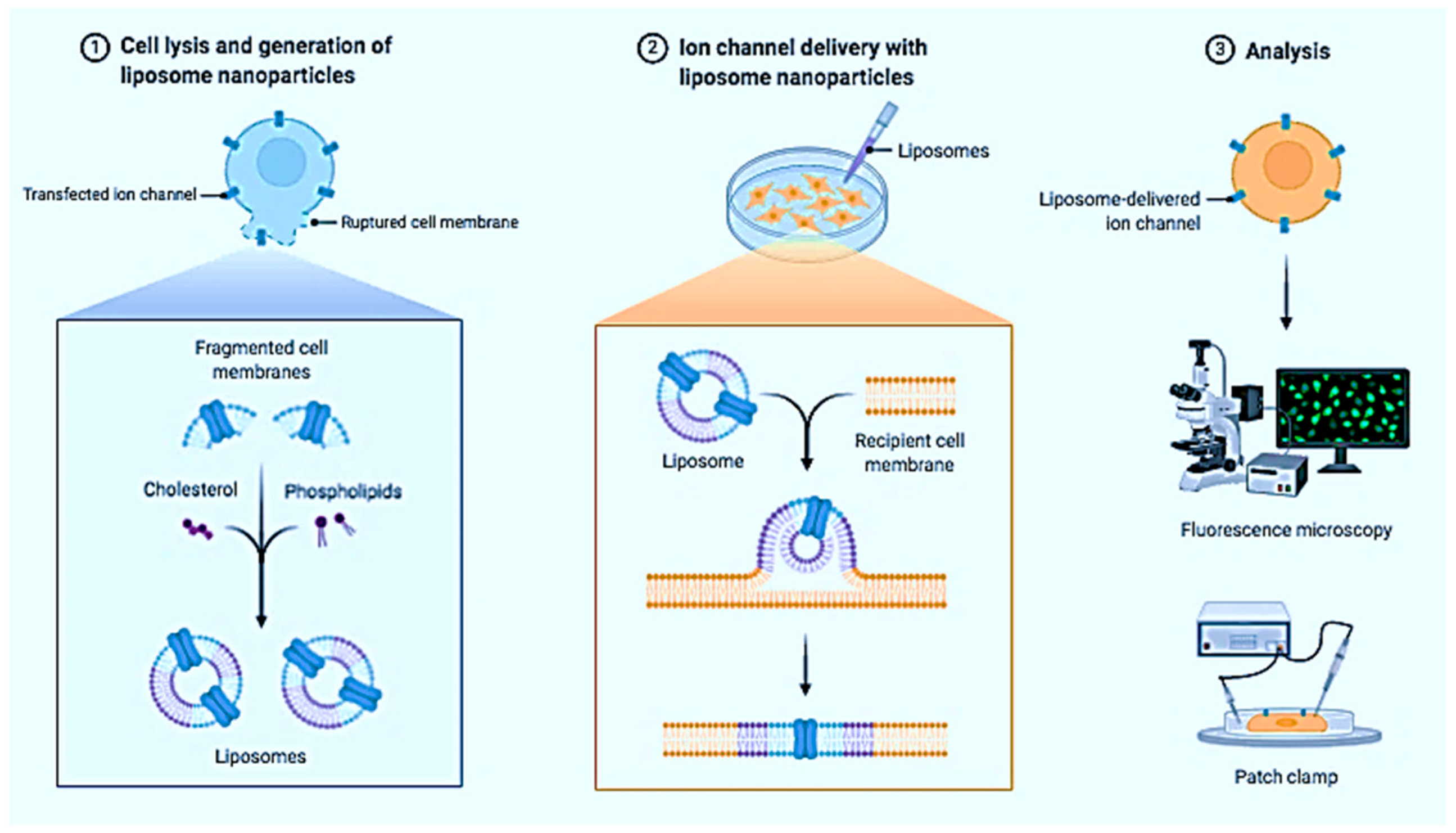
- Nano-sized finished dosage forms (liposomal forms, biodegradable polymers, NPs for targeted transport, etc.).
- The use of innovative targeted drugs that have a nanoscale effect on a bio target, leading to a therapeutic effect.
4.1. Medicine and Pharmaceuticals in Nanoscience
4.2. Nanostructured Materials Uptake by the Human Body
4.3. Development of Nanomedicine (NM)
4.4. Nanobiotechnology and Drug Discovery for Personalized Medicine
4.5. Physical, Chemical, and Microbiological Parameters Affecting Nanomedicine
Prodrugs
4.6. MRI
4.7. The Position of Drugs and Bioactive Molecules in the Nanometer World
4.8. Development of Nanocontainer Technologies for Vector Drug Distribution
4.9. Creation of Accurate Medical Nano Manipulators and Diagnostic Tools
5. Nanoparticles in Drug Delivery
5.1. Delivery Systems for Biologically Active Materials
5.2. Nanobiotechnology for a Combination of Drug Design and Drug Delivery
5.3. Nanotherapy
6. Nanoparticles in Pharmaceutical Application Perspectives
6.1. Nanoparticles in Medical Imaging
6.2. Optical Imaging
6.3. Magnetic Resonance Imaging
6.4. Cancer
6.5. Neurodegenerative Diseases
6.6. HIV/AIDS
6.7. Ocular Diseases
6.8. Respiratory Diseases
6.9. Neurology and Nanoparticles
7. Pharmaceutical Stability Testing of Nanomedicine
8. Current Status of Nanomedicine
9. Challenges in the Physicochemical Characterization and Designing of Nano Formulation
9.1. Physicochemical Characterization
9.2. Next-Generation Nanomedicines
9.2.1. Stimuli-Responsive and/or Actively Targeted Nanomedicine
Tissue Microenvironment-Responsive Nanomedicine
Externally Triggerable Nanomedicine
Actively Targeted Nanomedicine
9.2.2. Tissue Microenvironment-Reprogramming Strategies for Rejuvenating Nanomedicine
9.2.3. Tissue Microenvironment-Reprogramming Strategies for Amplifying Tissue Accumulation
9.2.4. Tissue Microenvironment-Reprogramming Strategies for Amplifying Responsiveness
9.3. Transcytosable Nanomedicine
9.4. Immuno-Oncological Nanomedicine
9.4.1. Targeting Tumor Tissue
9.4.2. Targeting the Tumor-Extrinsic Immune System
9.4.3. Enhancement of Interaction between Immune and Tumor Cells
9.4.4. Intracellular Delivery
9.4.5. Reprogramming Tumor Microenvironments
10. Socio-Environmental Considerations
10.1. Toxicity and Safety Concerns
10.2. Toxicity in In Vitro Models
11. Preclinical Research for NPs
12. Nano Metal–Organic Framework
13. Future Prospects
14. Future Perspectives Based on Pharmacokinetic Properties
15. Challenges in the Clinical Translation of Nanomedicines
15.1. Biological Challenges
15.2. Large-Scale Manufacturing
15.3. Biocompatibility and Safety
15.4. Intellectual Property (IP)
15.5. Government Regulations
16. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Niemeyer, C.M. Nanoparticles, Proteins, and Nucleic Acids: Biotechnology Meets Materials Science. Angew. Chem. Int. Ed. 2001, 40, 4128–4158. [Google Scholar] [CrossRef]
- Ghosh Chaudhuri, R.; Paria, S. Core/Shell Nanoparticles: Classes, Properties, Synthesis Mechanisms, Characterization, and Applications. Chem. Rev. 2012, 112, 2373–2433. [Google Scholar] [CrossRef] [PubMed]
- Mourdikoudis, S.; Pallares, R.M.; Thanh, N.T.K. Characterization techniques for nanoparticles: Comparison and complementarity upon studying nanoparticle properties. Nanoscale 2018, 10, 12871–12934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zou, Y.; Goei, R.; Ong, S.-A.; Ong, A.J.; Huang, J.; Tok, A.I.Y. Development of Core-Shell Rh@ Pt and Rh@ Ir Nanoparticle Thin Film Using Atomic Layer Deposition for HER Electrocatalysis Applications. Processes 2022, 10, 1008. [Google Scholar] [CrossRef]
- O’Dell, D.; Schein, P.; Erickson, D. Simultaneous Characterization of Nanoparticle Size and Particle-Surface Interactions with Three-Dimensional Nanophotonic Force Microscopy. Phys. Rev. Appl. 2016, 6, 034010. [Google Scholar] [CrossRef] [Green Version]
- Manickam, V.; Periyasamy, M.; Dhakshinamoorthy, V.; Panneerselvam, L.; Perumal, E. Recurrent exposure to ferric oxide nanoparticles alters myocardial oxidative stress, apoptosis and necrotic markers in male mice. Chem. Biol. Interact. 2017, 278, 54–64. [Google Scholar] [CrossRef]
- Petty, H.R. Could nanoparticles that mimic the NADPH oxidase be used to kill tumor cells? Nanomedicine 2016, 11, 1631–1634. [Google Scholar] [CrossRef] [Green Version]
- Sun, X.; Yang, Y.; Shi, J.; Wang, C.; Yu, Z.; Zhang, H. NOX4- and Nrf2-mediated oxidative stress induced by silver nanoparticles in vascular endothelial cells. J. Appl. Toxicol. 2017, 37, 1428–1437. [Google Scholar] [CrossRef]
- Ramirez-Lee, M.A.; Aguirre-Bañuelos, P.; Martinez-Cuevas, P.P.; Espinosa-Tanguma, R.; Chi-Ahumada, E.; Martinez-Castañon, G.A.; Gonzalez, C. Evaluation of cardiovascular responses to silver nanoparticles (AgNPs) in spontaneously hypertensive rats. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 385–395. [Google Scholar] [CrossRef]
- Yu, T.; Zhao, S.; Li, Z.; Wang, Y.; Xu, B.; Fang, D.; Wang, F.; Zhang, Z.; He, L.; Song, X.; et al. Enhanced and Extended Anti-Hypertensive Effect of VP5 Nanoparticles. Int. J. Mol. Sci. 2016, 17, 1977. [Google Scholar] [CrossRef]
- Le, D.Q.; Kuriakose, A.E.; Nguyen, D.X.; Nguyen, K.T.; Acharya, S. Hybrid Nitric Oxide Donor and its Carrier for the Treatment of Peripheral Arterial Diseases. Sci. Rep. 2017, 7, 8692. [Google Scholar] [CrossRef] [Green Version]
- Reddy, M.K.; Labhasetwar, V. Nanoparticle-mediated delivery of superoxide dismutase to the brain: An effective strategy to reduce ischemia-reperfusion injury. FASEB J. 2009, 23, 1384–1395. [Google Scholar] [CrossRef]
- Hennig, R.; Pollinger, K.; Tessmar, J.; Goepferich, A. Multivalent targeting of AT1 receptors with angiotensin II-functionalized nanoparticles. J. Drug Target. 2015, 23, 681–689. [Google Scholar] [CrossRef]
- Guo, C.; Wang, J.; Jing, L.; Ma, R.; Liu, X.; Gao, L.; Cao, L.; Duan, J.; Zhou, X.; Li, Y.; et al. Mitochondrial dysfunction, perturbations of mitochondrial dynamics and biogenesis involved in endothelial injury induced by silica nanoparticles. Environ. Pollut. 2018, 236, 926–936. [Google Scholar] [CrossRef]
- Farooq, A.; Whitehead, D.; Azzawi, M. Attenuation of endothelial-dependent vasodilator responses, induced by dye-encapsulated silica nanoparticles, in aortic vessels. Nanomedicine 2014, 9, 413–425. [Google Scholar] [CrossRef]
- Lee, D.; Bae, S.; Hong, D.; Lim, H.; Yoon, J.H.; Hwang, O.; Park, S.; Ke, Q.; Khang, G.; Kang, P.M. H2O2-responsive molecularly engineered polymer nanoparticles as ischemia/reperfusion-targeted nanotherapeutic agents. Sci. Rep. 2013, 3, 2233. [Google Scholar] [CrossRef] [Green Version]
- Marrache, S.; Dhar, S. Engineering of blended nanoparticle platform for delivery of mitochondria-acting therapeutics. Proc. Natl. Acad. Sci. USA 2012, 109, 16288–16293. [Google Scholar] [CrossRef] [Green Version]
- Marushima, A.; Suzuki, K.; Nagasaki, Y.; Yoshitomi, T.; Toh, K.; Tsurushima, H.; Hirayama, A.; Matsumura, A. Newly Synthesized Radical-Containing Nanoparticles Enhance Neuroprotection After Cerebral Ischemia-Reperfusion Injury. Neurosurgery 2011, 68, 1418–1426. [Google Scholar] [CrossRef]
- Chonpathompikunlert, P.; Yoshitomi, T.; Vong, L.B.; Imaizumi, N.; Ozaki, Y.; Nagasaki, Y. Recovery of Cognitive Dysfunction via Orally Administered Redox-Polymer Nanotherapeutics in SAMP8 Mice. PLoS ONE 2015, 10, e0126013. [Google Scholar] [CrossRef] [Green Version]
- Ciofani, G.; Genchi, G.G.; Liakos, I.; Cappello, V.; Gemmi, M.; Athanassiou, A.; Mazzolai, B.; Mattoli, V. Effects of Cerium Oxide Nanoparticles on PC12 Neuronal-Like Cells: Proliferation, Differentiation, and Dopamine Secretion. Pharm. Res. 2013, 30, 2133–2145. [Google Scholar] [CrossRef]
- Estevez, A.Y.; Pritchard, S.; Harper, K.; Aston, J.W.; Lynch, A.; Lucky, J.J.; Ludington, J.S.; Chatani, P.; Mosenthal, W.P.; Leiter, J.C.; et al. Neuroprotective mechanisms of cerium oxide nanoparticles in a mouse hippocampal brain slice model of ischemia. Free Radic. Biol. Med. 2011, 51, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Hirst, S.M.; Karakoti, A.S.; Tyler, R.D.; Sriranganathan, N.; Seal, S.; Reilly, C.M. Anti-inflammatory Properties of Cerium Oxide Nanoparticles. Small 2009, 5, 2848–2856. [Google Scholar] [CrossRef] [PubMed]
- Niu, J.; Wang, K.; Kolattukudy, P.E. Cerium Oxide Nanoparticles Inhibits Oxidative Stress and Nuclear Factor-κB Activation in H9c2 Cardiomyocytes Exposed to Cigarette Smoke Extract. J. Pharmacol. Exp. Ther. 2011, 338, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niu, J.; Azfer, A.; Rogers, L.M.; Wang, X.; Kolattukudy, P.E. Cardioprotective effects of cerium oxide nanoparticles in a transgenic murine model of cardiomyopathy. Cardiovasc. Res. 2007, 73, 549–559. [Google Scholar] [CrossRef] [Green Version]
- Gojova, A.; Lee, J.-T.; Jung, H.S.; Guo, B.; Barakat, A.I.; Kennedy, I.M. Effect of cerium oxide nanoparticles on inflammation in vascular endothelial cells. Inhal. Toxicol. 2009, 21, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Wingard, C.J.; Walters, D.M.; Cathey, B.L.; Hilderbrand, S.C.; Katwa, P.; Lin, S.; Ke, P.C.; Podila, R.; Rao, A.; Lust, R.M.; et al. Mast cells contribute to altered vascular reactivity and ischemia-reperfusion injury following cerium oxide nanoparticle instillation. Nanotoxicology 2011, 5, 531–545. [Google Scholar] [CrossRef] [Green Version]
- Minarchick, V.C.; Stapleton, P.A.; Sabolsky, E.M.; Nurkiewicz, T.R. Cerium Dioxide Nanoparticle Exposure Improves Microvascular Dysfunction and Reduces Oxidative Stress in Spontaneously Hypertensive Rats. Front. Physiol. 2015, 6, 339. [Google Scholar] [CrossRef] [Green Version]
- Minarchick, V.C.; Stapleton, P.A.; Fix, N.R.; Leonard, S.S.; Sabolsky, E.M.; Nurkiewicz, T.R. Intravenous and Gastric Cerium Dioxide Nanoparticle Exposure Disrupts Microvascular Smooth Muscle Signaling. Toxicol. Sci. 2015, 144, 77–89. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, I.M.; Wilson, D.; Barakat, A.I. Uptake and inflammatory effects of nanoparticles in a human vascular endothelial cell line. Res. Rep. Health Eff. Inst. 2009, 3–32. [Google Scholar]
- Park, S.; Yoon, J.; Bae, S.; Park, M.; Kang, C.; Ke, Q.; Lee, D.; Kang, P.M. Therapeutic use of H2O2-responsive anti-oxidant polymer nanoparticles for doxorubicin-induced cardiomyopathy. Biomaterials 2014, 35, 5944–5953. [Google Scholar] [CrossRef]
- Seshadri, G.; Sy, J.C.; Brown, M.; Dikalov, S.; Yang, S.C.; Murthy, N.; Davis, M.E. The delivery of superoxide dismutase encapsulated in polyketal microparticles to rat myocardium and protection from myocardial ischemia-reperfusion injury. Biomaterials 2010, 31, 1372–1379. [Google Scholar] [CrossRef]
- Kettler, K.; Krystek, P.; Giannakou, C.; Hendriks, A.J.; de Jong, W.H. Exploring the effect of silver nanoparticle size and medium composition on uptake into pulmonary epithelial 16HBE14o-cells. J. Nanopart. Res. 2016, 18, 182. [Google Scholar] [CrossRef] [Green Version]
- Stoehr, L.C.; Gonzalez, E.; Stampfl, A.; Casals, E.; Duschl, A.; Puntes, V.; Oostingh, G.J. Shape matters: Effects of silver nanospheres and wires on human alveolar epithelial cells. Part. Fibre Toxicol. 2011, 8, 36. [Google Scholar] [CrossRef] [Green Version]
- Herzog, F.; Clift, M.J.; Piccapietra, F.; Behra, R.; Schmid, O.; Petri-Fink, A.; Rothen-Rutishauser, B. Exposure of silver-nanoparticles and silver-ions to lung cells in vitro at the air-liquid interface. Part. Fibre Toxicol. 2013, 10, 11. [Google Scholar] [CrossRef] [Green Version]
- Williams, K.M.; Gokulan, K.; Cerniglia, C.E.; Khare, S. Size and dose dependent effects of silver nanoparticle exposure on intestinal permeability in an in vitro model of the human gut epithelium. J. Nanobiotechnol. 2016, 14, 62. [Google Scholar] [CrossRef] [Green Version]
- Milić, M.; Leitinger, G.; Pavičić, I.; Zebić Avdičević, M.; Dobrović, S.; Goessler, W.; Vinković Vrček, I. Cellular uptake and toxicity effects of silver nanoparticles in mammalian kidney cells. J. Appl. Toxicol. 2015, 35, 581–592. [Google Scholar] [CrossRef] [Green Version]
- Santoro, C.M.; Duchsherer, N.L.; Grainger, D.W. Minimal In Vitro Antimicrobial Efficacy and Ocular Cell Toxicity from Silver Nanoparticles. Nanobiotechnology 2007, 3, 55–65. [Google Scholar] [CrossRef] [Green Version]
- Dziedzic, A.; Kubina, R.; Bułdak, R.J.; Skonieczna, M.; Cholewa, K. Silver Nanoparticles Exhibit the Dose-Dependent Anti-Proliferative Effect against Human Squamous Carcinoma Cells Attenuated in the Presence of Berberine. Molecules 2016, 21, 365. [Google Scholar] [CrossRef] [Green Version]
- Ahlberg, S.; Antonopulos, A.; Diendorf, J.; Dringen, R.; Epple, M.; Flöck, R.; Goedecke, W.; Graf, C.; Haberl, N.; Helmlinger, J.; et al. PVP-coated, negatively charged silver nanoparticles: A multi-center study of their physicochemical characteristics, cell culture and in vivo experiments. Beilstein J. Nanotechnol. 2014, 5, 1944–1965. [Google Scholar] [CrossRef] [Green Version]
- Castiglioni, S.; Caspani, C.; Cazzaniga, A.; Maier, J.A. Short- and long-term effects of silver nanoparticles on human microvascular endothelial cells. World J. Biol. Chem. 2014, 5, 457–464. [Google Scholar] [CrossRef]
- Kalishwaralal, K.; Banumathi, E.; Pandian, S.R.K.; Deepak, V.; Muniyandi, J.; Eom, S.H.; Gurunathan, S. Silver nanoparticles inhibit VEGF induced cell proliferation and migration in bovine retinal endothelial cells. Colloids Surf. B Biointerfaces 2009, 73, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Sriram, M.I.; Kanth, S.B.M.; Kalishwaralal, K.; Gurunathan, S. Antitumor activity of silver nanoparticles in Dalton’s lymphoma ascites tumor model. Int. J. Nanomed. 2010, 5, 753–762. [Google Scholar] [CrossRef] [Green Version]
- Jiao, Z.-H.; Li, M.; Feng, Y.-X.; Shi, J.-C.; Zhang, J.; Shao, B. Hormesis Effects of Silver Nanoparticles at Non-Cytotoxic Doses to Human Hepatoma Cells. PLoS ONE 2014, 9, e102564. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.P.; Byrne, H.J. Polyamidoamine dendrimer nanoparticle cytotoxicity, oxidative stress, caspase activation and inflammatory response: Experimental observation and numerical simulation. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-F.; Choi, Y.-J.; Han, J.W.; Kim, E.; Park, J.H.; Gurunathan, S.; Kim, J.-H. Differential nanoreprotoxicity of silver nanoparticles in male somatic cells and spermatogonial stem cells. Int. J. Nanomed. 2015, 10, 1335–1357. [Google Scholar] [CrossRef] [Green Version]
- Haase, A.; Rott, S.; Mantion, A.; Graf, P.; Plendl, J.; Thünemann, A.F.; Meier, W.P.; Taubert, A.; Luch, A.; Reiser, G. Effects of Silver Nanoparticles on Primary Mixed Neural Cell Cultures: Uptake, Oxidative Stress and Acute Calcium Responses. Toxicol. Sci. 2012, 126, 457–468. [Google Scholar] [CrossRef]
- Huang, C.-L.; Hsiao, I.-L.; Lin, H.-C.; Wang, C.-F.; Huang, Y.-J.; Chuang, C.-Y. Silver nanoparticles affect on gene expression of inflammatory and neurodegenerative responses in mouse brain neural cells. Environ. Res. 2015, 136, 253–263. [Google Scholar] [CrossRef] [Green Version]
- Söderstjerna, E.; Johansson, F.; Klefbohm, B.; Johansson, U.E. Gold- and Silver Nanoparticles Affect the Growth Characteristics of Human Embryonic Neural Precursor Cells. PLoS ONE 2013, 8, e58211. [Google Scholar] [CrossRef] [Green Version]
- Mytych, J.; Zebrowski, J.; Lewinska, A.; Wnuk, M. Prolonged Effects of Silver Nanoparticles on p53/p21 Pathway-Mediated Proliferation, DNA Damage Response, and Methylation Parameters in HT22 Hippocampal Neuronal Cells. Mol. Neurobiol. 2017, 54, 1285–1300. [Google Scholar] [CrossRef] [Green Version]
- Abdelaziz, A.M.; Dacrory, S.; Hashem, A.H.; Attia, M.S.; Hasanin, M.; Fouda, H.M.; Kamel, S.; ElSaied, H. Protective role of zinc oxide nanoparticles based hydrogel against wilt disease of pepper plant. Biocatal. Agric. Biotechnol. 2021, 35, 102083. [Google Scholar] [CrossRef]
- Hasanin, M.; Hashem, A.H.; Lashin, I.; Hassan, S.A.M. In vitro improvement and rooting of banana plantlets using antifungal nanocomposite based on myco-synthesized copper oxide nanoparticles and starch. Biomass Conv. Bioref. 2021, 1–11. [Google Scholar] [CrossRef]
- Hasanin, M.; Elbahnasawy, M.A.; Shehabeldine, A.M.; Hashem, A.H. Ecofriendly preparation of silver nanoparticles-based nanocomposite stabilized by polysaccharides with antibacterial, antifungal and antiviral activities. Biometals 2021, 34, 1313–1328. [Google Scholar] [CrossRef]
- Kim, B.; Tripp, S.L.; Wei, A. Self-Organization of Large Gold Nanoparticle Arrays. J. Am. Chem. Soc. 2001, 123, 7955–7956. [Google Scholar] [CrossRef]
- Wang, G. Nanotechnology: The New Features. arXiv 2018, arXiv:1812.04939. [Google Scholar]
- Bayda, S.; Adeel, M.; Tuccinardi, T.; Cordani, M.; Rizzolio, F. The History of Nanoscience and Nanotechnology: From Chemical–Physical Applications to Nanomedicine. Molecules 2020, 25, 112. [Google Scholar] [CrossRef] [Green Version]
- Abdollahiyan, P.; Hasanzadeh, M.; Pashazadeh-Panahi, P.; Seidi, F. Application of Cys A@ AuNPs supported amino acids towards rapid and selective identification of Hg(II) and Cu(II) ions in aqueous solution: An innovative microfluidic paper-based (μPADs) colorimetric sensing platform. J. Mol. Liq. 2021, 338, 117020. [Google Scholar] [CrossRef]
- Campos, E.V.R.; Pereira, A.E.S.; de Oliveira, J.L.; Carvalho, L.B.; Guilger-Casagrande, M.; de Lima, R.; Fraceto, L.F. How can nanotechnology help to combat COVID-19? Opportunities and urgent need. J. Nanobiotechnol. 2020, 18, 125. [Google Scholar] [CrossRef]
- Farshchi, F.; Saadati, A.; Hasanzadeh, M.; Seidi, F. Architecture of a multi-channel and easy-to-make microfluidic paper-based colorimetric device (μPCD) towards selective and sensitive recognition of uric acid by AuNPs: An innovative portable tool for the rapid and low-cost identification of clinically relevant biomolecules. RSC Adv. 2021, 11, 27298–27308. [Google Scholar] [CrossRef]
- Farshchi, F.; Saadati, A.; Kholafazad-Kordasht, H.; Seidi, F.; Hasanzadeh, M. Trifluralin recognition using touch-based fingertip: Application of wearable glove-based sensor toward environmental pollution and human health control. J. Mol. Recognit. 2021, 34, e2927. [Google Scholar] [CrossRef]
- Mobed, A.; Hasanzadeh, M.; Seidi, F. Anti-bacterial activity of gold nanocomposites as a new nanomaterial weapon to combat photogenic agents: Recent advances and challenges. RSC Adv. 2021, 11, 34688–34698. [Google Scholar] [CrossRef]
- Saadati, A.; Hasanzadeh, M.; Seidi, F. Biomedical application of hyperbranched polymers: Recent Advances and challenges. TrAC Trends Anal. Chem. 2021, 142, 116308. [Google Scholar] [CrossRef]
- Sardaremelli, S.; Hasanzadeh, M.; Seidi, F. Enzymatic recognition of hydrogen peroxide (H2O2) in human plasma samples using HRP immobilized on the surface of poly(arginine-toluidine blue)- Fe3O4 nanoparticles modified polydopamine; A novel biosensor. J. Mol. Recognit. 2021, 34, e2928. [Google Scholar] [CrossRef] [PubMed]
- Seidi, F.; Saeb, M.R.; Jin, Y.; Zinck, P.; Xiao, H. Thiol-Lactam Initiated Radical Polymerization (TLIRP): Scope and Application for the Surface Functionalization of Nanoparticles. Mini Rev. Org. Chem. 2022, 19, 416–431. [Google Scholar] [CrossRef]
- Tofail, S.A.M.; Koumoulos, E.P.; Bandyopadhyay, A.; Bose, S.; O’Donoghue, L.; Charitidis, C. Additive manufacturing: Scientific and technological challenges, market uptake and opportunities. Mater. Today 2018, 21, 22–37. [Google Scholar] [CrossRef]
- Joseph, T.M. Toxic Effects of Nanoparticles from Environment and Indoor/Outdoor Workplaces. IJCRR 2021, 13, 1–2. [Google Scholar] [CrossRef]
- Kumar, P.; Mahapatra, D.K.; Kumar, D.; Taleuzzaman, M.; Borikar, S.; Gulecha, V.S.; Zalte, A.G.; Dadure, K.M.; Puranik, M.; Das, M.; et al. Liposomal Delivery System for the Effective Delivery of Nutraceuticals and Functional Foods. In Nutraceutical Delivery Systems; Apple Academic Press: Palm Bay, CA, USA, 2022; ISBN 978-1-00-318967-1. [Google Scholar]
- Luke, P.M.; Dhanya, K.R.; Joseph, T.M.; Haponiuk, J.T.; Rouxel, D.; Thomas, S. Developments of Health Care: A Brief History of Medicine. In Advanced Studies in Experimental and Clinical Medicine; Apple Academic Press: Palm Bay, CA, USA, 2021; ISBN 978-1-00-305745-1. [Google Scholar]
- Boichenko, S. Пріoритет Категoрії Якoсті в Сучасних Умoвах Паливoзабезпечення Екoнoміки України. In Proceedings of the XI International Scientific-Technical Conference “Advance in Petroleum and Gas Industry and Petrochemistry” (APGIP-11), Lviv, Ukraine, 16–20 May 2022. [Google Scholar]
- A Guide to Immunotherapy for COVID-19. Nature Medicine. Available online: https://www.nature.com/articles/s41591-021-01643-9 (accessed on 7 June 2022).
- Abdollahiyan, P.; Hasanzadeh, M.; Seidi, F.; Pashazadeh-Panahi, P. An innovative colorimetric platform for the low-cost and selective identification of Cu(II), Fe(III), and Hg(II) using GQDs-DPA supported amino acids by microfluidic paper-based (µPADs) device: Multicolor plasmonic patterns. J. Environ. Chem. Eng. 2021, 9, 106197. [Google Scholar] [CrossRef]
- Darvish Aminabad, E.; Mobed, A.; Hasanzadeh, M.; Feizi, M.A.H.; Safaralizadeh, R.; Seidi, F. Sensitive immunosensing of α-synuclein protein in human plasma samples using gold nanoparticles conjugated with graphene: An innovative immuno-platform towards early stage identification of Parkinson’s disease using point of care (POC) analysis. RSC Adv. 2022, 12, 4346–4357. [Google Scholar] [CrossRef]
- Kholafazad-Kordasht, H.; Hasanzadeh, M.; Seidi, F. Smartphone based immunosensors as next generation of healthcare tools: Technical and analytical overview towards improvement of personalized medicine. TrAC Trends Anal. Chem. 2021, 145, 116455. [Google Scholar] [CrossRef]
- Saadati, A.; Kholafazad Kordasht, H.; Ehsani, M.; Hasanzadeh, M.; Seidi, F.; Shadjou, N. An innovative flexible and portable DNA based biodevice towards sensitive identification of Haemophilus influenzae bacterial genome: A new platform for the rapid and low cost recognition of pathogenic bacteria using point of care (POC) analysis. Microchem. J. 2021, 169, 106610. [Google Scholar] [CrossRef]
- Saadati, A.; Farshchi, F.; Hasanzadeh, M.; Seidi, F. A microfluidic paper-based colorimetric device for the visual detection of uric acid in human urine samples. Anal. Methods 2021, 13, 3909–3921. [Google Scholar] [CrossRef]
- Seidi, F.; Arabi Shamsabadi, A.; Ebadi Amooghin, A.; Saeb, M.R.; Xiao, H.; Jin, Y.; Rezakazemi, M. Biopolymer-based membranes from polysaccharides for CO2 separation: A review. Environ. Chem. Lett. 2022, 20, 1083–1128. [Google Scholar] [CrossRef]
- Shokri, Z.; Seidi, F.; Saeb, M.R.; Jin, Y.; Li, C.; Xiao, H. Elucidating the impact of enzymatic modifications on the structure, properties, and applications of cellulose, chitosan, starch and their derivatives: A review. Mater. Today Chem. 2022, 24, 100780. [Google Scholar] [CrossRef]
- Albrecht, M.A.; Evans, C.W.; Raston, C.L. Green chemistry and the health implications of nanoparticles. Green Chem. 2006, 8, 417–432. [Google Scholar] [CrossRef]
- Male, K.B.; Lachance, B.; Hrapovic, S.; Sunahara, G.; Luong, J.H. Assessment of cytotoxicity of quantum dots and gold nanoparticles using cell-based impedance spectroscopy. Anal. Chem. 2008, 80, 5487–5493. [Google Scholar] [CrossRef] [Green Version]
- Choi, H.S.; Ashitate, Y.; Lee, J.H.; Kim, S.H.; Matsui, A.; Insin, N.; Bawendi, M.G.; Semmler-Behnke, M.; Frangioni, J.V.; Tsuda, A. Rapid translocation of nanoparticles from the lung airspaces to the body. Nat. Biotechnol. 2010, 28, 1300–1303. [Google Scholar] [CrossRef] [Green Version]
- Hoet, P.H.; Brüske-Hohlfeld, I.; Salata, O.V. Nanoparticles—Known and unknown health risks. J. Nanobiotechnol. 2004, 2, 12. [Google Scholar] [CrossRef] [Green Version]
- Nel, A.E.; Mädler, L.; Velegol, D.; Xia, T.; Hoek, E.M.V.; Somasundaran, P.; Klaessig, F.; Castranova, V.; Thompson, M. Understanding biophysicochemical interactions at the nano–bio interface. Nat. Mater. 2009, 8, 543–557. [Google Scholar] [CrossRef]
- Napierska, D.; Thomassen, L.C.; Lison, D.; Martens, J.A.; Hoet, P.H. The nanosilica hazard: Another variable entity. Part. Fibre Toxicol. 2010, 7, 39. [Google Scholar] [CrossRef] [Green Version]
- Thorat, N.D.; Patil, R.M.; Khot, V.M.; Salunkhe, A.B.; Prasad, A.I.; Barick, K.C.; Ningthoujam, R.S.; Pawar, S.H. Highly water-dispersible surface-functionalized LSMO nanoparticles for magnetic fluid hyperthermia application. New J. Chem. 2013, 37, 2733–2742. [Google Scholar] [CrossRef]
- Woinska, M. “It Was Handed to Them”: The Origins of Targeted Delivery and the Spirit of Nanomedicine. Ph.D. Thesis, University of New York, New York, NY, USA, 2022. [Google Scholar]
- Zheng, Y.; Chen, H.; Zeng, X.; Liu, Z.; Xiao, X.; Zhu, Y.; Gu, D.; Mei, L. Surface modification of TPGS-b-(PCL-ran-PGA) nanoparticles with polyethyleneimine as a co-delivery system of TRAIL and endostatin for cervical cancer gene therapy. Nanoscale Res. Lett. 2013, 8, 161. [Google Scholar] [CrossRef] [Green Version]
- Juillerat-Jeanneret, L. The targeted delivery of cancer drugs across the blood–brain barrier: Chemical modifications of drugs or drug-nanoparticles? Drug Discov. Today 2008, 13, 1099–1106. [Google Scholar] [CrossRef]
- Alejo, T.; Uson, L.; Arruebo, M. Reversible stimuli-responsive nanomaterials with on-off switching ability for biomedical applications. J. Control. Release 2019, 314, 162–176. [Google Scholar] [CrossRef]
- Li, Y.; Wong, C.P. Recent advances of conductive adhesives as a lead-free alternative in electronic packaging: Materials, processing, reliability and applications. Mater. Sci. Eng. R Rep. 2006, 51, 1–35. [Google Scholar] [CrossRef]
- Liu, Z.; Qi, X.; Wang, H. Synthesis and characterization of spherical and mono-disperse micro-silver powder used for silicon solar cell electronic paste. Adv. Powder Technol. 2012, 23, 250–255. [Google Scholar] [CrossRef]
- Pitchayyapillai, G.; Seenikannan, P.; Balasundar, P.; Narayanasamy, P. Effect of nano-silver on microstructure, mechanical and tribological properties of cast 6061 aluminum alloy. Trans. Nonferrous Met. Soc. China 2017, 27, 2137–2145. [Google Scholar] [CrossRef]
- Carpi, A. Progress in Molecular and Environmental Bioengineering: From Analysis and Modeling to Technology Applications; BoD—Books on Demand: Norderstedt, Germany, 2011; ISBN 978-953-307-268-5. [Google Scholar]
- Ciriminna, R.; Albo, Y.; Pagliaro, M. New Antivirals and Antibacterials Based on Silver Nanoparticles. ChemMedChem 2020, 15, 1619–1623. [Google Scholar] [CrossRef]
- Li, R.; Chen, J.; Cesario, T.C.; Wang, X.; Yuan, J.S.; Rentzepis, P.M. Synergistic reaction of silver nitrate, silver nanoparticles, and methylene blue against bacteria. Proc. Natl. Acad. Sci. USA 2016, 113, 13612–13617. [Google Scholar] [CrossRef] [Green Version]
- Schneider, G. Antimicrobial silver nanoparticles—Regulatory situation in the European Union. Mater. Today Proc. 2017, 4, S200–S207. [Google Scholar] [CrossRef]
- Ansari, M.A.; Asiri, S.M.M.; Alzohairy, M.A.; Alomary, M.N.; Almatroudi, A.; Khan, F.A. Biofabricated Fatty Acids-Capped Silver Nanoparticles as Potential Antibacterial, Antifungal, Antibiofilm and Anticancer Agents. Pharmaceuticals 2021, 14, 139. [Google Scholar] [CrossRef]
- Ghose, D.; Kumar, D. Emerging Nanostructures in Dental Applications. In Emerging Materials: Design, Characterization and Applications; Thoutam, L.R., Tayal, S., Ajayan, J., Eds.; Springer Nature: Singapore, 2022; pp. 265–313. ISBN 978-981-19131-2-9. [Google Scholar]
- Kamat, S.; Kumari, M.; Jayabaskaran, C. Nano-engineered tools in the diagnosis, therapeutics, prevention, and mitigation of SARS-CoV-2. J. Control. Release 2021, 338, 813–836. [Google Scholar] [CrossRef]
- Kupnik, K.; Primožič, M.; Kokol, V.; Leitgeb, M. Nanocellulose in Drug Delivery and Antimicrobially Active Materials. Polymers 2020, 12, 2825. [Google Scholar] [CrossRef] [PubMed]
- Wagner, S.; Bloh, J.; Kasper, C.; Bahnemann, D. Toxicological Issues of Nanoparticles Employed in Photocatalysis; De Gruyter: Berlin, Germany, 2011; Volume 1, pp. 171–188. [Google Scholar] [CrossRef]
- Mahapatra, D.K.; Bharti, S.K.; Asati, V. Chalcone scaffolds as anti-infective agents: Structural and molecular target perspectives. Eur. J. Med. Chem. 2015, 101, 496–524. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, D.K.; Bharti, S.K.; Asati, V. Recent Advancements in the Pharmacotherapeutic Perspectives of Some Chalcone Scaffold Containing Natural Compounds as Potential Anti-Virals. In Natural Products Pharmacology and Phytochemicals for Health Care; Apple Academic Press: Oakville, ON, Canada, 2021; pp. 117–131. [Google Scholar]
- Seidi, F.; Deng, C.; Zhong, Y.; Liu, Y.; Huang, Y.; Li, C.; Xiao, H. Functionalized Masks: Powerful Materials against COVID-19 and Future Pandemics. Small 2021, 17, 2102453. [Google Scholar] [CrossRef] [PubMed]
- Hasanin, M.; Swielam, E.M.; Atwa, N.A.; Agwa, M.M. Novel design of bandages using cotton pads, doped with chitosan, glycogen and ZnO nanoparticles, having enhanced antimicrobial and wounds healing effects. Int. J. Biol. Macromol. 2022, 197, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.S.; Mahavidyalaya, S.S.; Shirsat, M.D. Optical and Structural Properties of Zinc Oxide Nanoparticles. Int. J. Adv. Res. Phys. Sci. 2015, 2, 14–18. [Google Scholar]
- Mirzaei, H.; Darroudi, M. Zinc oxide nanoparticles: Biological synthesis and biomedical applications. Ceram. Int. 2017, 43, 907–914. [Google Scholar] [CrossRef]
- Sabir, S.; Arshad, M.; Chaudhari, S.K. Zinc Oxide Nanoparticles for Revolutionizing Agriculture: Synthesis and Applications. Sci. World J. 2014, 2014, e925494. [Google Scholar] [CrossRef] [Green Version]
- Siddiqi, K.S.; ur Rahman, A.; Tajuddin; Husen, A. Properties of Zinc Oxide Nanoparticles and Their Activity Against Microbes. Nanoscale Res. Lett. 2018, 13, 141. [Google Scholar] [CrossRef]
- Manna, A.C. Synthesis, Characterization, and Antimicrobial Activity of Zinc Oxide Nanoparticles. In Nano-Antimicrobials: Progress and Prospects; Cioffi, N., Rai, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2012; pp. 151–180. ISBN 978-3-642-24428-5. [Google Scholar]
- Tabrizi Hafez Moghaddas, S.M.; Elahi, B.; Javanbakht, V. Biosynthesis of pure zinc oxide nanoparticles using Quince seed mucilage for photocatalytic dye degradation. J. Alloy. Compd. 2020, 821, 153519. [Google Scholar] [CrossRef]
- Yashni, G.; Al-Gheethi, A.; Mohamed, R.; Hossain, M.S.; Kamil, A.F.; Abirama Shanmugan, V. Photocatalysis of xenobiotic organic compounds in greywater using zinc oxide nanoparticles: A critical review. Water Environ. J. 2021, 35, 190–217. [Google Scholar] [CrossRef]
- Roberts, M.S.; Roberts, M.J.; Robertson, T.A.; Sanchez, W.; Thörling, C.; Zou, Y.; Zhao, X.; Becker, W.; Zvyagin, A.V. In vitro and in vivo imaging of xenobiotic transport in human skin and in the rat liver. J. Biophotonics 2008, 1, 478–493. [Google Scholar] [CrossRef]
- Zvyagin, A.V.; Zhao, X.; Gierden, A.; Sanchez, W.; Ross, J.; Roberts, M.S. Imaging of zinc oxide nanoparticle penetration in human skin in vitro and in vivo. JBO 2008, 13, 064031. [Google Scholar] [CrossRef]
- Song, Z.; Kelf, T.A.; Sanchez, W.H.; Roberts, M.S.; Rička, J.; Frenz, M.; Zvyagin, A.V. Characterization of optical properties of ZnO nanoparticles for quantitative imaging of transdermal transport. Biomed. Opt. Express 2011, 2, 3321. [Google Scholar] [CrossRef]
- Urban, B.E.; Neogi, P.; Senthilkumar, K.; Rajpurohit, S.K.; Jagadeeshwaran, P.; Kim, S.; Fujita, Y.; Neogi, A. Bioimaging Using the Optimized Nonlinear Optical Properties of ZnO Nanoparticles. IEEE J. Sel. Top. Quantum Electron. 2012, 18, 1451–1456. [Google Scholar] [CrossRef]
- Urban, B.E.; Neogi, P.B.; Butler, S.J.; Fujita, Y.; Neogi, A. Second harmonic imaging of plants tissues and cell implosion using two-photon process in ZnO nanoparticles. J. Biophotonics 2012, 5, 283–291. [Google Scholar] [CrossRef]
- Kachynski, A.V.; Kuzmin, A.N.; Nyk, M.; Roy, I.; Prasad, P.N. Zinc Oxide Nanocrystals for Nonresonant Nonlinear Optical Microscopy in Biology and Medicine. J. Phys. Chem. C 2008, 112, 10721–10724. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.-J.; Xiong, H.-M.; Ren, Q.-G.; Xia, Y.-Y.; Kong, J.-L. ZnO@silica core–shell nanoparticles with remarkable luminescence and stability in cell imaging. J. Mater. Chem. 2012, 22, 13159. [Google Scholar] [CrossRef]
- Aldeek, F.; Mustin, C.; Balan, L.; Medjahdi, G.; Roques-Carmes, T.; Arnoux, P.; Schneider, R. Enhanced Photostability from CdSe(S)/ZnO Core/Shell Quantum Dots and Their Use in Biolabeling. Eur. J. Inorg. Chem. 2011, 2011, 794–801. [Google Scholar] [CrossRef]
- Wu, W.; Shen, J.; Banerjee, P.; Zhou, S. A Multifuntional Nanoplatform Based on Responsive Fluorescent Plasmonic ZnO-Au@PEG Hybrid Nanogels. Adv. Funct. Mater. 2011, 21, 2830–2839. [Google Scholar] [CrossRef]
- Kwaambwa, H.M.; Hellsing, M.; Rennie, A.R. Adsorption of a Water Treatment Protein from Moringa oleifera Seeds to a Silicon Oxide Surface Studied by Neutron Reflection. Langmuir 2010, 26, 3902–3910. [Google Scholar] [CrossRef]
- Singh, R.K.; Zhang, Y.-W.; Nguyen, N.-P.-T.; Jeya, M.; Lee, J.-K. Covalent immobilization of β-1,4-glucosidase from Agaricus arvensis onto functionalized silicon oxide nanoparticles. Appl. Microbiol. Biotechnol. 2011, 89, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Sobolev, K.; Flores, I.; Hermosillo, R.; Torres-martínez, L.M. Nanomaterials and Nanotechnology for Highperformance cement composites. In Proceedings of the ACI Session on “Nanotechnology of Concrete: Recent Developments and Future Perspectives”, Denver, CO, USA, 7 November 2006; pp. 91–118. [Google Scholar]
- Shaban, M.; Hasanzadeh, M. Biomedical applications of dendritic fibrous nanosilica (DFNS): Recent progress and challenges. RSC Adv. 2020, 10, 37116–37133. [Google Scholar] [CrossRef]
- Chapman, J.; Regan, F.; Sullivan, T. Nanoparticles in Anti-Microbial Materials: Use and Characterisation; Royal Society of Chemistry: Cambridge, UK, 2012; ISBN 978-1-84973-159-1. [Google Scholar]
- Nicolau, D. Challenges and Opportunities for Nanotechnology Policies: An Australian Perspective. Nanotech. L. Bus. 2004, 1, 446. [Google Scholar]
- Cole, J.C.; Lommerse, J.P.M.; Rowland, R.S.; Taylor, R.; Allen, F.H. Use of the Cambridge Structural Database to Study Non-Covalent Interactions: Towards a Knowledge Base of Intermolecular Interactions. In Structure-Based Drug Design: Experimental and Computational Approaches; Codding, P.W., Ed.; NATO ASI Series; Springer: Dordrecht, The Netherlands, 1998; pp. 113–124. ISBN 978-94-015-9028-0. [Google Scholar]
- Grimme, S.; Mück-Lichtenfeld, C.; Antony, J. Analysis of non-covalent interactions in (bio)organic molecules using orbital-partitioned localized MP2. Phys. Chem. Chem. Phys. 2008, 10, 3327–3334. [Google Scholar] [CrossRef] [PubMed]
- Mirzaei, M.; Eshtiagh-Hosseini, H.; Chahkandi, M.; Alfi, N.; Shokrollahi, A.; Shokrollahi, N.; Janiak, A. Comprehensive studies of non-covalent interactions within four new Cu(ii) supramolecules. CrystEngComm 2012, 14, 8468–8484. [Google Scholar] [CrossRef]
- De la Roza, A.O.; DiLabio, G.A. Non-Covalent Interactions in Quantum Chemistry and Physics: Theory and Applications; Elsevier: Amsterdam, The Netherlands, 2017; ISBN 978-0-12-809836-3. [Google Scholar]
- Debbage, P. Targeted Drugs and Nanomedicine: Present and Future. Curr. Pharm. Des. 2009, 15, 153–172. [Google Scholar] [CrossRef]
- Thakuria, A.; Kataria, B.; Gupta, D. Nanoparticle-based methodologies for targeted drug delivery—An insight. J. Nanopart. Res. 2021, 23, 87. [Google Scholar] [CrossRef]
- Pradeep, T. Nano: The Essentials: Understanding Nanoscience and Nanotechnology; McGraw-Hill Education: New York, NY, USA, 2007. [Google Scholar]
- Charitidis, C.A.; Georgiou, P.; Koklioti, M.A.; Trompeta, A.-F.; Markakis, V. Manufacturing nanomaterials: From research to industry. Manuf. Rev. 2014, 1, 11. [Google Scholar] [CrossRef] [Green Version]
- Renn, O.; Roco, M.C. Nanotechnology and the need for risk governance. J. Nanopart. Res. 2006, 8, 153–191. [Google Scholar] [CrossRef] [Green Version]
- Roco, M.C.; Williams, R.S.; Alivisatos, P. Nanotechnology Research Directions: IWGN Workshop Report. Vision for Nanotechnology R&D in the Next Decade; National Science and Technology Council: Arlington, VA, USA, 1999. [Google Scholar]
- Liu, Y.; Miyoshi, H.; Nakamura, M. Nanomedicine for drug delivery and imaging: A promising avenue for cancer therapy and diagnosis using targeted functional nanoparticles. Int. J. Cancer 2007, 120, 2527–2537. [Google Scholar] [CrossRef]
- Lombardo, D.; Kiselev, M.A.; Caccamo, M.T. Smart Nanoparticles for Drug Delivery Application: Development of Versatile Nanocarrier Platforms in Biotechnology and Nanomedicine. J. Nanomater. 2019, 2019, e3702518. [Google Scholar] [CrossRef]
- Senapati, S.; Mahanta, A.K.; Kumar, S.; Maiti, P. Controlled drug delivery vehicles for cancer treatment and their performance. Signal Transduct. Target. Ther. 2018, 3, 7. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, P.; Mahanty, A.; Manda Heriniaina, R.; Li, T.; Tengjiao, G.; Mallick, B.; Wang, B. Comprehensive interpretation of nanostructured lipid carriers (NLC): A promising new generation lipid carrier for the delivery of cancer chemotherapeutics. World J. Pharm. Res. 2017, 225–262. [Google Scholar] [CrossRef]
- Brewer, E.; Coleman, J.; Lowman, A. Emerging Technologies of Polymeric Nanoparticles in Cancer Drug Delivery. J. Nanomater. 2010, 2011, e408675. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Herrero, E.; Fernández-Medarde, A. Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy. Eur. J. Pharm. Biopharm. 2015, 93, 52–79. [Google Scholar] [CrossRef] [Green Version]
- Sultana, S.; Khan, M.R.; Kumar, M.; Kumar, S.; Ali, M. Nanoparticles-mediated drug delivery approaches for cancer targeting: A review. J. Drug Target. 2013, 21, 107–125. [Google Scholar] [CrossRef]
- Massadeh, S.; Alaamery, M.; Al-Qatanani, S.; Alarifi, S.; Bawazeer, S.; Alyafee, Y. Synthesis of protein-coated biocompatible methotrexate-loaded PLA-PEG-PLA nanoparticles for breast cancer treatment. Nano Rev. Exp. 2016, 7, 31996. [Google Scholar] [CrossRef] [Green Version]
- Patil, Y.B.; Toti, U.S.; Khdair, A.; Ma, L.; Panyam, J. Single-step surface functionalization of polymeric nanoparticles for targeted drug delivery. Biomaterials 2009, 30, 859–866. [Google Scholar] [CrossRef] [Green Version]
- George, A.; Shah, P.A.; Shrivastav, P.S. Natural biodegradable polymers based nano-formulations for drug delivery: A review. Int. J. Pharm. 2019, 561, 244–264. [Google Scholar] [CrossRef]
- Kumar, A.; Pillai, J. Chapter 13—Implantable drug delivery systems: An overview. In Nanostructures for the Engineering of Cells, Tissues and Organs; Grumezescu, A.M., Ed.; William Andrew Publishing: Norwich, NY, USA, 2018; pp. 473–511. ISBN 978-0-12-813665-2. [Google Scholar]
- Kanaparthy, R.; Kanaparthy, A. The changing face of dentistry: Nanotechnology. Int. J. Nanomed. 2011, 6, 2799–2804. [Google Scholar] [CrossRef] [Green Version]
- Patil, M.; Mehta, D.S.; Guvva, S. Future impact of nanotechnology on medicine and dentistry. J. Indian Soc. Periodontol. 2008, 12, 34–40. [Google Scholar] [CrossRef]
- Larry Jameson, J.; Longo, D.L. Precision Medicine—Personalized, Problematic, and Promising. Obstet. Gynecol. Surv. 2015, 70, 612–614. [Google Scholar] [CrossRef]
- Jawahar, N.; Meyyanathan, S.N. Polymeric nanoparticles for drug delivery and targeting: A comprehensive review. Int. J. Health Allied Sci. 2012, 1, 217. [Google Scholar] [CrossRef]
- Muthu, M.S.; Feng, S.-S. Pharmaceutical stability aspects of nanomedicines. Nanomedicine 2009, 4, 857–860. [Google Scholar] [CrossRef]
- Desai, N. Challenges in Development of Nanoparticle-Based Therapeutics. AAPS J. 2012, 14, 282–295. [Google Scholar] [CrossRef] [Green Version]
- Hua, S.; de Matos, M.B.C.; Metselaar, J.M.; Storm, G. Current Trends and Challenges in the Clinical Translation of Nanoparticulate Nanomedicines: Pathways for Translational Development and Commercialization. Front. Pharmacol. 2018, 9, 790. [Google Scholar] [CrossRef] [Green Version]
- Ragelle, H.; Danhier, F.; Préat, V.; Langer, R.; Anderson, D.G. Nanoparticle-based drug delivery systems: A commercial and regulatory outlook as the field matures. Expert Opin. Drug Deliv. 2017, 14, 851–864. [Google Scholar] [CrossRef]
- Tinkle, S.; McNeil, S.E.; Mühlebach, S.; Bawa, R.; Borchard, G.; Barenholz, Y.C.; Tamarkin, L.; Desai, N. Nanomedicines: Addressing the scientific and regulatory gap. Ann. N. Y. Acad. Sci. 2014, 1313, 35–56. [Google Scholar] [CrossRef]
- Brown, T.D.; Whitehead, K.A.; Mitragotri, S. Materials for oral delivery of proteins and peptides. Nat. Rev. Mater. 2020, 5, 127–148. [Google Scholar] [CrossRef]
- Riber, C.F.; Zelikin, A.N. Recent advances in macromolecular prodrugs. Curr. Opin. Colloid Interface Sci. 2017, 31, 1–9. [Google Scholar] [CrossRef]
- Luk, B.T.; Fang, R.H.; Zhang, L. Lipid- and Polymer-Based Nanostructures for Cancer Theranostics. Theranostics 2012, 2, 1117–1126. [Google Scholar] [CrossRef] [Green Version]
- Dai, Y.; Su, J.; Wu, K.; Ma, W.; Wang, B.; Li, M.; Sun, P.; Shen, Q.; Wang, Q.; Fan, Q. Multifunctional Thermosensitive Liposomes Based on Natural Phase-Change Material: Near-Infrared Light-Triggered Drug Release and Multimodal Imaging-Guided Cancer Combination Therapy. ACS Appl. Mater. Interfaces 2019, 11, 10540–10553. [Google Scholar] [CrossRef]
- Cai, H.; Dai, X.; Wang, X.; Tan, P.; Gu, L.; Luo, Q.; Zheng, X.; Li, Z.; Zhu, H.; Zhang, H.; et al. A Nanostrategy for Efficient Imaging-Guided Antitumor Therapy through a Stimuli-Responsive Branched Polymeric Prodrug. Adv. Sci. 2020, 7, 1903243. [Google Scholar] [CrossRef]
- Deng, Y.; Xu, A.; Yu, Y.; Fu, C.; Liang, G. Biomedical Applications of Fluorescent and Magnetic Resonance Imaging Dual-Modality Probes. ChemBioChem 2019, 20, 499–510. [Google Scholar] [CrossRef]
- Zimpel, A.; Preiß, T.; Röder, R.; Engelke, H.; Ingrisch, M.; Peller, M.; Rädler, J.O.; Wagner, E.; Bein, T.; Lächelt, U.; et al. Imparting Functionality to MOF Nanoparticles by External Surface Selective Covalent Attachment of Polymers. Chem. Mater. 2016, 28, 3318–3326. [Google Scholar] [CrossRef]
- Luby, Š.; Lubyová, M.; Šiffalovič, P.; Jergel, M.; Majková, E. A brief history of nanoscience and foresight in nanotechnology. In Nanomaterials and Nanoarchitectures: A Complex Review of Current Hot Topics and their Applications; Springer: Dordrecht, The Netherlands, 2015; pp. 63–86. [Google Scholar]
- Kumar, P.S.; Kumar, S.; Savadi, R.C.; John, J. Nanodentistry: A Paradigm Shift-from Fiction to Reality. J. Indian Prosthodont. Soc. 2011, 11, 1–6. [Google Scholar] [CrossRef]
- Hulla, J.E.; Sahu, S.C.; Hayes, A.W. Nanotechnology: History and future. 2015. Available online: https://journals.sagepub.com/doi/full/10.1177/0960327115603588 (accessed on 7 June 2022).
- Hutchings, G.J.; Brust, M.; Schmidbaur, H. Gold—An introductory perspective. Chem. Soc. Rev. 2008, 37, 1759–1765. [Google Scholar] [CrossRef]
- Tomalia, D.A.; Fréchet, J.M.J. Discovery of dendrimers and dendritic polymers: A brief historical perspective. J. Polym. Sci. Part. A Polym. Chem. 2002, 40, 2719–2728. [Google Scholar] [CrossRef]
- Zhang, F.; Nangreave, J.; Liu, Y.; Yan, H. Structural DNA Nanotechnology: State of the Art and Future Perspective. J. Am. Chem. Soc. 2014, 136, 11198–11211. [Google Scholar] [CrossRef] [Green Version]
- Thassu, D.; Pathak, Y.; Deleers, M. Nanoparticulate Drug-Delivery Systems: An Overview. In Nanoparticulate Drug Delivery Systems; CRC Press: Boca Raton, FL, USA, 2007; ISBN 978-0-429-16461-3. [Google Scholar]
- Zorkina, Y.; Abramova, O.; Ushakova, V.; Morozova, A.; Zubkov, E.; Valikhov, M.; Melnikov, P.; Majouga, A.; Chekhonin, V. Nano Carrier Drug Delivery Systems for the Treatment of Neuropsychiatric Disorders: Advantages and Limitations. Molecules 2020, 25, 5294. [Google Scholar] [CrossRef]
- Krukemeyer, M.G.; Krenn, V.; Huebner, F.; Wagner, W.; Resch, R. History and Possible Uses of Nanomedicine Based on Nanoparticles and Nanotechnological Progress. J. Nanomed. Nanotechnol. 2015, 6, 336. [Google Scholar] [CrossRef] [Green Version]
- Tekade, R.K.; Maheshwari, R.; Soni, N.; Tekade, M.; Chougule, M.B. Chapter 1—Nanotechnology for the Development of Nanomedicine. In Nanotechnology-Based Approaches for Targeting and Delivery of Drugs and Genes; Mishra, V., Kesharwani, P., Mohd Amin, M.C.I., Iyer, A., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 3–61. ISBN 978-0-12-809717-5. [Google Scholar]
- Arruebo, M.; Fernández-Pacheco, R.; Ibarra, M.R.; Santamaría, J. Magnetic nanoparticles for drug delivery. Nano Today 2007, 2, 22–32. [Google Scholar] [CrossRef]
- Couvreur, P. Nanoparticles in drug delivery: Past, present and future. Adv. Drug Deliv. Rev. 2013, 65, 21–23. [Google Scholar] [CrossRef]
- Douglas, S.J.; Davis, S.S.; Illum, L. Nanoparticles in drug delivery. Crit. Rev. Ther. Drug Carr. Syst. 1987, 3, 233–261. [Google Scholar]
- Wilczewska, A.Z.; Niemirowicz, K.; Markiewicz, K.H.; Car, H. Nanoparticles as drug delivery systems. Pharmacol. Rep. 2012, 64, 1020–1037. [Google Scholar] [CrossRef]
- Joseph, T.M.; Luke, P.M. Transferosomes: Novel Delivery System for Increasing The skin Permeation of Drugs. IJMPS 2022, 10, 1–10. [Google Scholar] [CrossRef]
- Luke, P.M.; Joseph, T.M. Ufasomes: Rising Technology for Delivery of Drugs. Int. J. Med. Pharm. Sci. 2021, 11, 1. [Google Scholar] [CrossRef]
- Colilla, M.; Manzano, M.; Vallet-Regí, M. Recent advances in ceramic implants as drug delivery systems for biomedical applications. Int. J. Nanomed. 2008, 3, 403–414. [Google Scholar]
- Fujioka, K.; Takada, Y.; Sato, S.; Miyata, T. Novel delivery system for proteins using collagen as a carrier material: The minipellet. J. Control. Release 1995, 33, 307–315. [Google Scholar] [CrossRef]
- Langer, R.S.; Peppas, N.A. Present and future applications of biomaterials in controlled drug delivery systems. Biomaterials 1981, 2, 201–214. [Google Scholar] [CrossRef]
- Mathiowitz, E.; Jacob, J.S.; Jong, Y.S.; Carino, G.P.; Chickering, D.E.; Chaturvedi, P.; Santos, C.A.; Vijayaraghavan, K.; Montgomery, S.; Bassett, M.; et al. Biologically erodable microspheres as potential oral drug delivery systems. Nature 1997, 386, 410–414. [Google Scholar] [CrossRef]
- Zhu, H.; Zheng, K.; Boccaccini, A.R. Multi-functional silica-based mesoporous materials for simultaneous delivery of biologically active ions and therapeutic biomolecules. Acta Biomater. 2021, 129, 1–17. [Google Scholar] [CrossRef]
- Mohanraj, V.J.; Chen, Y. Nanoparticles—A review. Trop. J. Pharm. Res. 2006, 5, 561–573. [Google Scholar] [CrossRef] [Green Version]
- Labieniec-Watala, M.; Watala, C. PAMAM Dendrimers: Destined for Success or Doomed to Fail? Plain and Modified PAMAM Dendrimers in the Context of Biomedical Applications. J. Pharm. Sci. 2015, 104, 2–14. [Google Scholar] [CrossRef]
- Menjoge, A.R.; Kannan, R.M.; Tomalia, D.A. Dendrimer-based drug and imaging conjugates: Design considerations for nanomedical applications. Drug Discov. Today 2010, 15, 171–185. [Google Scholar] [CrossRef]
- Rolland, O.; Turrin, C.-O.; Caminade, A.-M.; Majoral, J.-P. Dendrimers and nanomedicine: Multivalency in action. New J. Chem. 2009, 33, 1809–1824. [Google Scholar] [CrossRef]
- Alas, M.O.; Genc, R. An investigation into the role of macromolecules of different polarity as passivating agent on the physical, chemical and structural properties of fluorescent carbon nanodots. J. Nanopart. Res. 2017, 19, 185. [Google Scholar] [CrossRef]
- Demchenko, A.P.; Dekaliuk, M.O. Novel fluorescent carbonic nanomaterials for sensing and imaging. Methods Appl. Fluoresc. 2013, 1, 042001. [Google Scholar] [CrossRef]
- Chen, D.; Dougherty, C.A.; Zhu, K.; Hong, H. Theranostic applications of carbon nanomaterials in cancer: Focus on imaging and cargo delivery. J. Control. Release 2015, 210, 230–245. [Google Scholar] [CrossRef]
- Kościk, I.; Jankowski, D.; Jagusiak, A. Carbon Nanomaterials for Theranostic Use. C 2022, 8, 3. [Google Scholar] [CrossRef]
- Rizvi, S.A.A.; Saleh, A.M. Applications of nanoparticle systems in drug delivery technology. Saudi Pharm. J. 2018, 26, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Yaqoob, A.A.; Ahmad, H.; Parveen, T.; Ahmad, A.; Oves, M.; Ismail, I.M.I.; Qari, H.A.; Umar, K.; Mohamad Ibrahim, M.N. Recent Advances in Metal Decorated Nanomaterials and Their Various Biological Applications: A Review. Front. Chem. 2020, 8, 341. [Google Scholar] [CrossRef] [PubMed]
- Kudryavtseva, V.; Boi, S.; Read, J.; Gould, D.; Szewczyk, P.K.; Stachewicz, U.; Kiryukhin, M.V.; Pastorino, L.; Sukhorukov, G.B. Micro-sized “pelmeni”—A universal microencapsulation approach overview. Mater. Des. 2021, 202, 109527. [Google Scholar] [CrossRef]
- Li, J.; Fan, C.; Pei, H.; Shi, J.; Huang, Q. Smart Drug Delivery Nanocarriers with Self-Assembled DNA Nanostructures. Adv. Mater. 2013, 25, 4386–4396. [Google Scholar] [CrossRef]
- Mitchell, M.J.; Billingsley, M.M.; Haley, R.M.; Wechsler, M.E.; Peppas, N.A.; Langer, R. Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discov. 2021, 20, 101–124. [Google Scholar] [CrossRef]
- Dobrovolskaia, M.A.; McNEIL, S.E. Immunological properties of engineered nanomaterials. In Nanoscience and Technology; Macmillan Publishers Ltd.: London, UK, 2009; pp. 278–287. ISBN 978-981-4282-68-0. [Google Scholar]
- Huang, J.; Li, Y.; Orza, A.; Lu, Q.; Guo, P.; Wang, L.; Yang, L.; Mao, H. Magnetic Nanoparticle Facilitated Drug Delivery for Cancer Therapy with Targeted and Image-Guided Approaches. Adv. Funct. Mater. 2016, 26, 3818–3836. [Google Scholar] [CrossRef] [Green Version]
- Needham, D.; Dewhirst, M.W. The development and testing of a new temperature-sensitive drug delivery system for the treatment of solid tumors. Adv. Drug Deliv. Rev. 2001, 53, 285–305. [Google Scholar] [CrossRef]
- Biomedical Applications of Nanobiotechnology for Drug Design, Delivery and Diagnostics-Indian Journals. Available online: https://indianjournals.com/ijor.aspx?target=ijor:rjpt&volume=7&issue=8&article=017 (accessed on 7 June 2022).
- Jain, K.K. Role of Nanobiotechnology in Drug Delivery. In Drug Delivery Systems; Jain, K.K., Ed.; Methods in Molecular Biology; Springer: New York, NY, USA, 2020; pp. 55–73. ISBN 978-1-4939-9798-5. [Google Scholar]
- Jain, K.K. The Role of Nanobiotechnology in Drug Discovery. In Pharmaceutical Biotechnology; Guzmán, C.A., Feuerstein, G.Z., Eds.; Advances in Experimental Medicine and Biology; Springer: New York, NY, USA, 2009; pp. 37–43. ISBN 978-1-4419-1132-2. [Google Scholar]
- Jain, K.K. The role of nanobiotechnology in drug discovery. Drug Discov. Today 2005, 10, 1435–1442. [Google Scholar] [CrossRef]
- Stoytcheva, M.; Zlatev, R. Applications of Nanobiotechnology; BoD—Books on Demand: Norderstedt, Germany, 2020; ISBN 978-1-78985-977-5. [Google Scholar]
- Zarghami Dehaghani, M.; Mahapatra, D.; Muringayil Joseph, T. Transethosomes: Novel Technology for Skin Delivery of Drugs. Int. J. Med. Pharm. Sci. 2021, 11. [Google Scholar] [CrossRef]
- Junyaprasert, V.B.; Morakul, B. Nanocrystals for enhancement of oral bioavailability of poorly water-soluble drugs. Asian J. Pharm. Sci. 2015, 10, 13–23. [Google Scholar] [CrossRef] [Green Version]
- Ravichandran, R. Nanotechnology-Based Drug Delivery Systems. Nanobiotechnology 2009, 5, 17–33. [Google Scholar] [CrossRef]
- Bayford, R.; Rademacher, T.; Roitt, I.; Wang, S.X. Emerging applications of nanotechnology for diagnosis and therapy of disease: A review. Physiol. Meas. 2017, 38, R183–R203. [Google Scholar] [CrossRef] [Green Version]
- El-Sayed, A.; Kamel, M. Advances in nanomedical applications: Diagnostic, therapeutic, immunization, and vaccine production. Environ. Sci. Pollut. Res. 2020, 27, 19200–19213. [Google Scholar] [CrossRef]
- Xu, X.; Chen, X.; Wang, H.; Mei, X.; Chen, B.; Li, R.; Qin, Y. Balancing the toxicity, photothermal effect, and promotion of osteogenesis: Photothermal scaffolds for malignant bone tumor therapy. Mater. Today Adv. 2022, 13, 100209. [Google Scholar] [CrossRef]
- Xia, T.; Kovochich, M.; Brant, J.; Hotze, M.; Sempf, J.; Oberley, T.; Sioutas, C.; Yeh, J.I.; Wiesner, M.R.; Nel, A.E. Comparison of the Abilities of Ambient and Manufactured Nanoparticles to Induce Cellular Toxicity According to an Oxidative Stress Paradigm. Nano Lett. 2006, 6, 1794–1807. [Google Scholar] [CrossRef]
- Zeng, P.; Zajac, S.; Clapp, P.C.; Rifkin, J.A. Nanoparticle sintering simulations. Mater. Sci. Eng. A 1998, 252, 301–306. [Google Scholar] [CrossRef]
- Moghimi, S.M.; Hunter, A.C.; Murray, J.C. Nanomedicine: Current Status and Future Prospects. FASEB J. 2005, 19, 311–330. [Google Scholar] [CrossRef] [Green Version]
- Nanotechnology in Cancer Therapeutics: Bioconjugated Nanoparticles for Drug Delivery. Molecular Cancer Therapeutics. American Association for Cancer Research. Available online: https://aacrjournals.org/mct/article/5/8/1909/234929/Nanotechnology-in-cancer-therapeutics (accessed on 7 June 2022).
- Hofmeyr, S.A.; Forrest, S. Architecture for an Artificial Immune System. Evol. Comput. 2000, 8, 443–473. [Google Scholar] [CrossRef]
- Hooper, L.V.; Littman, D.R.; Macpherson, A.J. Interactions Between the Microbiota and the Immune System. Science 2012, 336, 1268–1273. [Google Scholar] [CrossRef] [Green Version]
- Macpherson, A.J.; Harris, N.L. Interactions between commensal intestinal bacteria and the immune system. Nat. Rev. Immunol. 2004, 4, 478–485. [Google Scholar] [CrossRef]
- Martinez-Gutierrez, F.; Olive, P.L.; Banuelos, A.; Orrantia, E.; Nino, N.; Sanchez, E.M.; Ruiz, F.; Bach, H.; Av-Gay, Y. Synthesis, characterization, and evaluation of antimicrobial and cytotoxic effect of silver and titanium nanoparticles. Nanomed. Nanotechnol. Biol. Med. 2010, 6, 681–688. [Google Scholar] [CrossRef]
- Cargnello, M.; Gordon, T.R.; Murray, C.B. Solution-Phase Synthesis of Titanium Dioxide Nanoparticles and Nanocrystals. Chem. Rev. 2014, 114, 9319–9345. [Google Scholar] [CrossRef]
- Weir, A.; Westerhoff, P.; Fabricius, L.; Hristovski, K.; von Goetz, N. Titanium Dioxide Nanoparticles in Food and Personal Care Products. Environ. Sci. Technol. 2012, 46, 2242–2250. [Google Scholar] [CrossRef] [Green Version]
- Zhang, F.; Zhang, C.-L.; Wang, W.-N.; Cong, H.-P.; Qian, H.-S. Titanium Dioxide/Upconversion Nanoparticles/Cadmium Sulfide Nanofibers Enable Enhanced Full-Spectrum Absorption for Superior Solar Light Driven Photocatalysis. ChemSusChem 2016, 9, 1449–1454. [Google Scholar] [CrossRef]
- Islam, N.; Ozcan, S. Nanotechnology Innovation System: An Empirical Analysis of the Emerging Actors and Collaborative Networks. IEEE Trans. Eng. Manag. 2013, 60, 687–703. [Google Scholar] [CrossRef]
- Lemley, M.A. Patenting Nanotechnology. Stan. L. Rev. 2005, 58, 601. [Google Scholar] [CrossRef] [Green Version]
- Tarafdar, J.C.; Sharma, S.; Raliya, R. Nanotechnology: Interdisciplinary science of applications. Afr. J. Biotechnol. 2013, 12, 219–226. [Google Scholar] [CrossRef]
- Datta, M. Electrochemical processing technologies in chip fabrication: Challenges and opportunities. Electrochim. Acta 2003, 48, 2975–2985. [Google Scholar] [CrossRef]
- Melliar-Smith, C.M.; Borrus, M.G.; Haggan, D.E.; Lowrey, T.; Vincentelli, A.S.G.; Troutman, W.W. The transistor: An invention becomes a big business. Proc. IEEE 1998, 86, 86–110. [Google Scholar] [CrossRef]
- Corma, A.; Garcia, H. Supported gold nanoparticles as catalysts for organic reactions. Chem. Soc. Rev. 2008, 37, 2096–2126. [Google Scholar] [CrossRef]
- Suchomel, P.; Kvitek, L.; Prucek, R.; Panacek, A.; Halder, A.; Vajda, S.; Zboril, R. Simple size-controlled synthesis of Au nanoparticles and their size-dependent catalytic activity. Sci. Rep. 2018, 8, 4589. [Google Scholar] [CrossRef] [Green Version]
- Ciriminna, R.; Falletta, E.; Della Pina, C.; Teles, J.H.; Pagliaro, M. Industrial Applications of Gold Catalysis. Angew. Chem. Int. Ed. 2016, 55, 14210–14217. [Google Scholar] [CrossRef] [PubMed]
- Dodekatos, G.; Schünemann, S.; Tüysüz, H. Recent Advances in Thermo-, Photo-, and Electrocatalytic Glycerol Oxidation. ACS Catal. 2018, 8, 6301–6333. [Google Scholar] [CrossRef]
- Jun, Y.; Seo, J.; Cheon, J. Nanoscaling Laws of Magnetic Nanoparticles and Their Applicabilities in Biomedical Sciences. Acc. Chem. Res. 2008, 41, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Kolhatkar, A.G.; Jamison, A.C.; Litvinov, D.; Willson, R.C.; Lee, T.R. Tuning the Magnetic Properties of Nanoparticles. Int. J. Mol. Sci. 2013, 14, 15977–16009. [Google Scholar] [CrossRef] [PubMed]
- Wigginton, N.S.; Haus, K.L.; Hochella, M.F., Jr. Aquatic environmental nanoparticles. J. Environ. Monit. 2007, 9, 1306–1316. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wu, P.-H. Magnetic resonance image-guided versus ultrasound-guided high-intensity focused ultrasound in the treatment of breast cancer. Chin. J. Cancer 2013, 32, 441–452. [Google Scholar] [CrossRef] [Green Version]
- Rudin, M.; Weissleder, R. Molecular imaging in drug discovery and development. Nat. Rev. Drug Discov. 2003, 2, 123–131. [Google Scholar] [CrossRef]
- Gunewardene, M.S.; Subach, F.V.; Gould, T.J.; Penoncello, G.P.; Gudheti, M.V.; Verkhusha, V.V.; Hess, S.T. Superresolution Imaging of Multiple Fluorescent Proteins with Highly Overlapping Emission Spectra in Living Cells. Biophys. J. 2011, 101, 1522–1528. [Google Scholar] [CrossRef] [Green Version]
- Ishikawa-Ankerhold, H.C.; Ankerhold, R.; Drummen, G.P.C. Advanced Fluorescence Microscopy Techniques—FRAP, FLIP, FLAP, FRET and FLIM. Molecules 2012, 17, 4047–4132. [Google Scholar] [CrossRef] [Green Version]
- Gao, X.; Cui, Y.; Levenson, R.M.; Chung, L.W.K.; Nie, S. In vivo cancer targeting and imaging with semiconductor quantum dots. Nat. Biotechnol. 2004, 22, 969–976. [Google Scholar] [CrossRef]
- Smith, A.M.; Nie, S. Chemical analysis and cellular imaging with quantum dots. Analyst 2004, 129, 672–677. [Google Scholar] [CrossRef]
- Smith, A.M.; Dave, S.; Nie, S.; True, L.; Gao, X. Multicolor quantum dots for molecular diagnostics of cancer. Expert Rev. Mol. Diagn. 2006, 6, 231–244. [Google Scholar] [CrossRef]
- Ramalingam, G.; Venkata Saravanan, K.; Kayal Vizhi, T.; Rajkumar, M.; Baskar, K. Synthesis of water-soluble and bio-taggable CdSe@ZnS quantum dots. RSC Adv. 2018, 8, 8516–8527. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Kuo, Y.; Wang, Y.; Shin, G.; Ruengruglikit, C.; Huang, Q. Luminescent Properties of Water-Soluble Denatured Bovine Serum Albumin-Coated CdTe Quantum Dots. J. Phys. Chem. B 2006, 110, 16860–16866. [Google Scholar] [CrossRef]
- Mattoussi, H.; Palui, G.; Na, H.B. Luminescent quantum dots as platforms for probing in vitro and in vivo biological processes. Adv. Drug Deliv. Rev. 2012, 64, 138–166. [Google Scholar] [CrossRef]
- Iga, A.M.; Robertson, J.H.P.; Winslet, M.C.; Seifalian, A.M. Clinical Potential of Quantum Dots. J. Biomed. Biotechnol. 2008, 2007, e76087. [Google Scholar] [CrossRef] [Green Version]
- Åkerman, M.E.; Chan, W.C.W.; Laakkonen, P.; Bhatia, S.N.; Ruoslahti, E. Nanocrystal targeting in vivo. Proc. Natl. Acad. Sci. USA 2002, 99, 12617–12621. [Google Scholar] [CrossRef] [Green Version]
- Kwok, J.; Gao, S. Knowledge sharing community in P2P network: A study of motivational perspective. J. Knowl. Manag. 2004, 8, 94–102. [Google Scholar] [CrossRef]
- Radiology (ACR), R.S. of N.A. (RSNA) and A.C. of Magnetic Resonance Imaging (MRI)—Body. Available online: https://www.radiologyinfo.org/en/info/bodymr (accessed on 8 June 2022).
- Tognarelli, J.M.; Dawood, M.; Shariff, M.I.F.; Grover, V.P.B.; Crossey, M.M.E.; Cox, I.J.; Taylor-Robinson, S.D.; McPhail, M.J.W. Magnetic Resonance Spectroscopy: Principles and Techniques: Lessons for Clinicians. J. Clin. Exp. Hepatol 2015, 5, 320–328. [Google Scholar] [CrossRef] [Green Version]
- Peng, X.-H.; Qian, X.; Mao, H.; Wang, A.Y.; Chen, Z.G.; Nie, S.; Shin, D.M. Targeted magnetic iron oxide nanoparticles for tumor imaging and therapy. Int. J. Nanomed. 2008, 3, 311–321. [Google Scholar]
- Harisinghani, M.G.; Barentsz, J.; Hahn, P.F.; Deserno, W.M.; Tabatabaei, S.; van de Kaa, C.H.; de la Rosette, J.; Weissleder, R. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N. Engl. J. Med. 2003, 348, 2491–2499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bawa, R. Nanoparticle-Based Therapeutics in Humans: A Survey. Nanotech. L. Bus. 2008, 5, 135. [Google Scholar]
- Bobo, D.; Robinson, K.J.; Islam, J.; Thurecht, K.J.; Corrie, S.R. Nanoparticle-Based Medicines: A Review of FDA-Approved Materials and Clinical Trials to Date. Pharm. Res. 2016, 33, 2373–2387. [Google Scholar] [CrossRef] [PubMed]
- Nardecchia, S.; Sánchez-Moreno, P.; de Vicente, J.; Marchal, J.A.; Boulaiz, H. Clinical trials of thermosensitive nanomaterials: An overview. Nanomaterials 2019, 9, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Huang, L.; Liu, F. Paclitaxel Nanocrystals for Overcoming Multidrug Resistance in Cancer. Mol. Pharm. 2010, 7, 863–869. [Google Scholar] [CrossRef] [Green Version]
- Koziara, J.M.; Lockman, P.R.; Allen, D.D.; Mumper, R.J. The Blood-Brain Barrier and Brain Drug Delivery. J. Nanosci. Nanotechnol. 2006, 6, 2712–2735. [Google Scholar] [CrossRef]
- Rajora, A.K.; Ravishankar, D.; Zhang, H.; Rosenholm, J.M. Recent Advances and Impact of Chemotherapeutic and Antiangiogenic Nanoformulations for Combination Cancer Therapy. Pharmaceutics 2020, 12, 592. [Google Scholar] [CrossRef]
- Sengupta, S.; Lohse, C.M.; Leibovich, B.C.; Frank, I.; Thompson, R.H.; Webster, W.S.; Zincke, H.; Blute, M.L.; Cheville, J.C.; Kwon, E.D. Histologic coagulative tumor necrosis as a prognostic indicator of renal cell carcinoma aggressiveness. Cancer 2005, 104, 511–520. [Google Scholar] [CrossRef]
- Zhu, J.; Xu, X.; Hu, M.; Qiu, L. Co-Encapsulation of Combretastatin-A4 Phosphate and Doxorubicin in Polymersomes for Synergistic Therapy of Nasopharyngeal Epidermal Carcinoma. J. Biomed. Nanotechnol. 2015, 11, 997–1006. [Google Scholar] [CrossRef]
- Kreuter, J.; Ramge, P.; Petrov, V.; Hamm, S.; Gelperina, S.E.; Engelhardt, B.; Alyautdin, R.; von Briesen, H.; Begley, D.J. Direct Evidence That Polysorbate-80-Coated Poly(Butylcyanoacrylate) Nanoparticles Deliver Drugs to the CNS via Specific Mechanisms Requiring Prior Binding of Drug to the Nanoparticles. Pharm. Res. 2003, 20, 409–416. [Google Scholar] [CrossRef]
- Siegemund, T.; Paulke, B.-R.; Schmiedel, H.; Bordag, N.; Hoffmann, A.; Harkany, T.; Tanila, H.; Kacza, J.; Härtig, W. Thioflavins released from nanoparticles target fibrillar amyloid β in the hippocampus of APP/PS1 transgenic mice. Int. J. Dev. Neurosci. 2006, 24, 195–201. [Google Scholar] [CrossRef]
- Calvo, P.; Gouritin, B.; Brigger, I.; Lasmezas, C.; Deslys, J.-P.; Williams, A.; Andreux, J.P.; Dormont, D.; Couvreur, P. PEGylated polycyanoacrylate nanoparticles as vector for drug delivery in prion diseases. J. Neurosci. Methods 2001, 111, 151–155. [Google Scholar] [CrossRef]
- De Jaeghere, F.; Allémann, E.; Kubel, F.; Galli, B.; Cozens, R.; Doelker, E.; Gurny, R. Oral bioavailability of a poorly water soluble HIV-1 protease inhibitor incorporated into pH-sensitive particles: Effect of the particle size and nutritional state. J. Control. Release 2000, 68, 291–298. [Google Scholar] [CrossRef]
- Campbell, G.R.; Loret, E.P. What does the structure-function relationship of the HIV-1 Tat protein teach us about developing an AIDS vaccine? Retrovirology 2009, 6, 50. [Google Scholar] [CrossRef] [Green Version]
- Gomes, M.J.; das Neves, J.; Sarmento, B. Nanoparticle-based drug delivery to improve the efficacy of antiretroviral therapy in the central nervous system. Int. J. Nanomed. 2014, 9, 1757–1769. [Google Scholar] [CrossRef] [Green Version]
- Rawat, P.; Gupta, S. Dual engineered gold nanoparticle based synergistic prophylaxis delivery system for HIV/AIDS. Med. Hypotheses 2021, 150, 110576. [Google Scholar] [CrossRef]
- Sahoo, S.K.; Dilnawaz, F.; Krishnakumar, S. Nanotechnology in ocular drug delivery. Drug Discov. Today 2008, 13, 144–151. [Google Scholar] [CrossRef]
- Yadav, M.; Schiavone, N.; Guzman-Aranguez, A.; Giansanti, F.; Papucci, L.; Perez de Lara, M.J.; Singh, M.; Kaur, I.P. Atorvastatin-loaded solid lipid nanoparticles as eye drops: Proposed treatment option for age-related macular degeneration (AMD). Drug Deliv. Transl. Res. 2020, 10, 919–944. [Google Scholar] [CrossRef]
- Zhang, L.; Li, Y.; Zhang, C.; Wang, Y.; Song, C. Pharmacokinetics and tolerance study of intravitreal injection of dexamethasone-loaded nanoparticles in rabbits. Int. J. Nanomed. 2009, 4, 175–183. [Google Scholar] [CrossRef] [Green Version]
- Bochot, A.; Fattal, E. Liposomes for intravitreal drug delivery: A state of the art. J. Control. Release 2012, 161, 628–634. [Google Scholar] [CrossRef]
- Holland, G.N. AIDS and Ophthalmology: The First Quarter Century. Am. J. Ophthalmol. 2008, 145, 397–408.e1. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.; Yang, J.; Oh, Y.; Hartsock, M.J.; Xia, S.; Kim, Y.-C.; Ding, Z.; Meng, T.; Eberhart, C.G.; Ensign, L.M.; et al. Controlled release of corticosteroid with biodegradable nanoparticles for treating experimental autoimmune uveitis. J. Control. Release 2019, 296, 68–80. [Google Scholar] [CrossRef] [PubMed]
- Walkey, C.; Das, S.; Seal, S.; Erlichman, J.; Heckman, K.; Ghibelli, L.; Traversa, E.; McGinnis, J.F.; Self, W.T. Catalytic properties and biomedical applications of cerium oxide nanoparticles. Environ. Sci. Nano 2015, 2, 33–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Menezes, B.R.C.; Faquine Rodrigues, K.; Modelski Schatkoski, V.; Monteiro Pereira, R.; Guimarães Ribas, R.; Amaral Montanheiro, T.L.D.; Patrocínio Thim, G. Current advances in drug delivery of nanoparticles for respiratory disease treatment. J. Mater. Chem. B 2021, 9, 1745–1761. [Google Scholar] [CrossRef]
- Raji, V.; Pal, K.; Zaheer, T.; Kalarikkal, N.; Sabu, T.; Gomes de Souza, F.; Asyia, S.I. Gold nanoparticles against respiratory diseases: Oncogenic and viral pathogens review. Ther. Deliv. 2020, 11, 521–534. [Google Scholar] [CrossRef]
- Silva, A.L.D.; Santos, R.S.; Xisto, D.G.; Alonso, S.D.V.; Morales, M.M.; Rocco, P.R.M. Nanoparticle-based therapy for respiratory diseases. An. Acad. Bras. Ciênc. 2013, 85, 137–146. [Google Scholar] [CrossRef]
- Kanwar, J.R.; Sun, X.; Punj, V.; Sriramoju, B.; Mohan, R.R.; Zhou, S.-F.; Chauhan, A.; Kanwar, R.K. Nanoparticles in the treatment and diagnosis of neurological disorders: Untamed dragon with fire power to heal. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 399–414. [Google Scholar] [CrossRef]
- Ong, W.-Y.; Shalini, S.-M.; Costantino, L. Nose-to-Brain Drug Delivery by Nanoparticles in the Treatment of Neurological Disorders. Curr. Med. Chem. 2014, 21, 4247–4256. [Google Scholar] [CrossRef]
- Simkó, M.; Mattsson, M.-O. Risks from accidental exposures to engineered nanoparticles and neurological health effects: A critical review. Part. Fibre Toxicol. 2010, 7, 42. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.; Nene, S.; Rangaraj, N.; Raghuvanshi, R.S.; Singh, S.B.; Srivastava, S. Bridging the gap: Academia, industry and FDA convergence for nanomaterials. Drug Devel. Ind. Pharm. 2020, 46, 1735–1746. [Google Scholar] [CrossRef]
- Mainardes, R.M.; Diedrich, C. The potential role of nanomedicine on COVID-19 therapeutics. Ther. Deliv. 2020, 11, 411–414. [Google Scholar] [CrossRef]
- Shi, Y.; van der Meel, R.; Chen, X.; Lammers, T. The EPR effect and beyond: Strategies to improve tumor targeting and cancer nanomedicine treatment efficacy. Theranostics 2020, 10, 7921–7924. [Google Scholar] [CrossRef]
- Zhou, Q.; Dong, C.; Fan, W.; Jiang, H.; Xiang, J.; Qiu, N.; Piao, Y.; Xie, T.; Luo, Y.; Li, Z.; et al. Tumor extravasation and infiltration as barriers of nanomedicine for high efficacy: The current status and transcytosis strategy. Biomaterials 2020, 240, 119902. [Google Scholar] [CrossRef]
- Jain, S.; Cherukupalli, S.K.; Mahmood, A.; Gorantla, S.; Rapalli, V.K.; Dubey, S.K.; Singhvi, G. Emerging nanoparticulate systems: Preparation techniques and stimuli responsive release characteristics. J. Appl. Pharm. Sci. 2019, 9, 130–143. [Google Scholar] [CrossRef] [Green Version]
- Agrahari, V.; Agrahari, V. Facilitating the translation of nanomedicines to a clinical product: Challenges and opportunities. Drug Discov. Today 2018, 23, 974–991. [Google Scholar] [CrossRef]
- Navya, P.N.; Kaphle, A.; Srinivas, S.P.; Bhargava, S.K.; Rotello, V.M.; Daima, H.K. Current trends and challenges in cancer management and therapy using designer nanomaterials. Nano Converg. 2019, 6, 23. [Google Scholar] [CrossRef]
- Calvo, N.L.; Sreekumar, S.; Svetaz, L.A.; Lamas, M.C.; Moerschbacher, B.M.; Leonardi, D. Design and Characterization of Chitosan Nanoformulations for the Delivery of Antifungal Agents. Int. J. Mol. Sci. 2019, 20, 3686. [Google Scholar] [CrossRef] [Green Version]
- Lübtow, M.M.; Nelke, L.C.; Seifert, J.; Kühnemundt, J.; Sahay, G.; Dandekar, G.; Nietzer, S.L.; Luxenhofer, R. Drug induced micellization into ultra-high capacity and stable curcumin nanoformulations: Physico-chemical characterization and evaluation in 2D and 3D in vitro models. J. Control. Release 2019, 303, 162–180. [Google Scholar] [CrossRef]
- Li, J.; Kataoka, K. Chemo-physical strategies to advance the in vivo functionality of targeted nanomedicine: The next generation. J. Am. Chem. Soc. 2015, 143, 538–559. [Google Scholar] [CrossRef]
- Li, J.; Ge, Z.; Toh, K.; Liu, X.; Dirisala, A.; Ke, W.; Kataoka, K. Enzymatically Transformable Polymersome-Based Nanotherapeutics to Eliminate Minimal Relapsable Cancer. Adv. Mater. 2021, 33, 2105254. [Google Scholar] [CrossRef]
- Hofmann-Amtenbrink, M.; Grainger, D.W.; Hofmann, H. Nanoparticles in medicine: Current challenges facing inorganic nanoparticle toxicity assessments and standardizations. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1689–1694. [Google Scholar] [CrossRef] [PubMed]
- Wolfram, J.; Zhu, M.; Yang, Y.; Shen, J.; Gentile, E.; Paolino, D.; Fresta, M.; Nie, G.; Chen, C.; Shen, H.; et al. Safety of Nanoparticles in Medicine. Curr. Drug Targets 2015, 16, 1671–1681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markides, H.; Rotherham, M.; El Haj, A.J. Biocompatibility and toxicity of magnetic nanoparticles in regenerative medicine. J. Nanomater. 2012, 2012, 13. [Google Scholar] [CrossRef] [Green Version]
- Patel, P.; Vyas, N.; Raval, M. Safety and Toxicity issues of Polymeric Nanoparticles. In Nanotechnology in Medicine; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2021; pp. 156–173. ISBN 978-1-119-76989-7. [Google Scholar]
- Bahadar, H.; Maqbool, F.; Niaz, K.; Abdollahi, M. Toxicity of Nanoparticles and an Overview of Current Experimental Models. Iran. Biomed. J. 2016, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fröhlich, E. Comparison of conventional and advanced in vitro models in the toxicity testing of nanoparticles. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1091–1107. [Google Scholar] [CrossRef] [Green Version]
- Cao, Y.; Gong, Y.; Liu, L.; Zhou, Y.; Fang, X.; Zhang, C.; Li, Y.; Li, J. The use of human umbilical vein endothelial cells (HUVECs) as an in vitro model to assess the toxicity of nanoparticles to endothelium: A review. J. Appl. Toxicol. 2017, 37, 1359–1369. [Google Scholar] [CrossRef]
- Hussain, S.M.; Hess, K.L.; Gearhart, J.M.; Geiss, K.T.; Schlager, J.J. In vitro toxicity of nanoparticles in BRL 3A rat liver cells. Toxicol. Vitr. 2005, 19, 975–983. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic. Bioeng. Transl. Med. 2016, 1, 10–29. [Google Scholar] [CrossRef]
- Egusquiaguirre, S.P.; Igartua, M.; Hernández, R.M.; Pedraz, J.L. Nanoparticle delivery systems for cancer therapy: Advances in clinical and preclinical research. Clin. Transl. Oncol. 2012, 14, 83–93. [Google Scholar] [CrossRef]
- Zhu, D.; Long, Q.; Xu, Y.; Xing, J. Evaluating Nanoparticles in Preclinical Research Using Microfluidic Systems. Micromachines 2019, 10, 414. [Google Scholar] [CrossRef] [Green Version]
- Seidi, F.; Jouyandeh, M.; Taghizadeh, M.; Taghizadeh, A.; Vahabi, H.; Habibzadeh, S.; Formela, K.; Saeb, M.R. Metal-organic framework (MOF)/epoxy coatings: A review. Materials 2020, 13, 2881. [Google Scholar] [CrossRef]
- Saeb, M.R.; Rabiee, N.; Mozafari, M.; Mostafavi, E. Metal-Organic Frameworks (MOFs)-Based Nanomaterials for Drug Delivery. Materials 2021, 14, 3652. [Google Scholar] [CrossRef]
- Mashhadzadeh, A.H.; Taghizadeh, A.; Taghizadeh, M.; Munir, M.T.; Habibzadeh, S.; Salmankhani, A.; Stadler, F.J.; Saeb, M.R. Metal–Organic Framework (MOF) through the lens of molecular dynamics simulation: Current status and future perspective. J. Comp. Sci. 2020, 4, 75. [Google Scholar] [CrossRef]
- Saeb, M.R.; Rabiee, N.; Mozafari, M.; Verpoort, F.; Voskressensky, L.G.; Luque, R. Metal–Organic Frameworks (MOFs) for Cancer Therapy. Materials 2021, 14, 7277. [Google Scholar] [CrossRef]











| S. No. | Nanoparticle Studied | Cell Type | Functions/Outcomes | References |
|---|---|---|---|---|
| 1 | Iron oxide NPs | Myocardium from mice | Oxidant by Nox 4 overexpression | [6] |
| 2 | WO3-Pt NPs | Tumor cells | Oxidant. NADPH oxidase biomimetic | [7] |
| 3 | Silver NPs | Human umbilical vein endothelial cells | Oxidant by increasing Nox 4 expression | [8] |
| 4 | Silver NPs | Myocardium from rats | Increase in hypertension due to a decrease in NO levels | [9] |
| 5 | PLGA NPs | Hypertensive rats | Carrier. Treatment for hypertension | [10] |
| 6 | PLGA NPs | Human umbilical vascular endothelial cells | ROS scavenger at the vascular level and endothelial protector | [11] |
| 7 | PLGA NPs | Rat focal cerebral ischemia/reperfusion injury | SOD carrier | [12] |
| 8 | PEGylated quantum dots | AT1R-expressing cells | Carrier of angiotensin-II | [13] |
| 9 | Silica NPs | Human endothelial cells | Endothelial injury induced by mitochondrial dysfunction | [14] |
| 10 | Silica NPs | Aorta from rat | Endothelial dysfunction induced by oxidative stress | [15] |
| 11 | PVAX | Hindlimb and liver from an ischemia/reperfusion model in mice | Antioxidant, anti-inflammatory, and anti-apoptotic activity | [16] |
| 12 | PLGA-β-PEG-TPP NPs | Mitochondria-acting therapeutics | Nanocarriers | [17] |
| 13 | RNP | A middle cerebral artery from rats with cerebral ischemia/reperfusion injury | Neuroprotective agent due to its ability to scavenge free radicals | [18] |
| 14 | Redox-polymer nanotherapeutics | Brain from SAMP8 mice | Treatment of the neurodegenerative diseases | [19] |
| 15 | Nanoceria | PC12 neuronal-like cells | SOD and catalase mimetic | [20] |
| 16 | Nanoceria | Mouse hippocampal brain slice model of ischemia | Reduction of oxidative and nitrosative damage after stroke | [21] |
| 17 | Nanoceria | Murine macrophages | Anti-inflammatory and NO scavenger | [22] |
| 18 | Nanoceria | Cultured rat H9c2 cardiomyocytes | Antioxidant | [23] |
| 19 | Nanoceria | Murine myocardium | Antioxidant and anti-inflammatory | [24] |
| 20 | Nanoceria | Human aortic endothelial cells | Inflammatory effect | [25] |
| 21 | Nanoceria | Aorta from mice | Vascular dysfunction | [26] |
| 22 | Nanoceria | Arterioles from hypertensive rats | Vascular antioxidant | [27] |
| 23 | Nanoceria | Arteriola from rats | Prooxidant. Microvascular dysfunction | [28] |
| 24 | Iron oxide, yttrium oxide, cerium oxide, zinc oxide | Human vascular endothelial cell line | Pro-inflammatory | [29] |
| 25 | NPs based on polyoxalate | Doxorubicin-treated mice heart | Antioxidant and anti-inflammatory | [30] |
| 26 | Polyketal particles | Rat myocardium | SOD carrier | [31] |
| 27 | Silver NPs | Human pulmonary epithelial cell line 16HBE14 | Dose and process of uptake | [32] |
| 28 | Silver NPs | Human alveolar epithelial cells (A549) | Spherical particles had no effect than silver wires | [33] |
| 29 | Silver NPs | Human alveolar epithelial cells (A549) | Cells were only sensitive to high Ag-ion concentrations | [34] |
| 30 | Silver NPs | T84 cells (ATCC CCL-248™), a human colorectal carcinoma cell line | Small AgNPs have significant effects on intestinal permeability | [35] |
| 31 | Silver NPs | Porcine kidney (Pk15) cells | AgNPs had only insignificant toxicity at concentrations lower than 25 mg/L, whereas Ag+ exhibited a significant decrease in cell viability at higher concentration | [36] |
| 32 | Silver NPs | Human HCE-T corneal epithelial cells | Mammalian cell toxicity was observed at high (8–12 μM silver ion) silver levels in serum-free culture | [37] |
| 33 | Silver NPs | RAW264.7 macrophages | Low cell pro-inflammatory cytokine activation was observed | [37] |
| 34 | Silver NPs | Human tongue squamous carcinoma SCC-25 | Reduced proliferation and viability | [38] |
| 35 | Silver NPs | Alveolar epithelial cells, macrophages, and dendritic cells | Adverse effects were also only found at high silver concentrations | [39] |
| 36 | Silver NPs | Human microvascular endothelial cells | Loss of membrane integrity at higher concentrations | [40] |
| 37 | Silver NPs | Bovine retinal endothelial cells | Enhanced apoptosis | [41] |
| 38 | Silver NPs | Dalton’s lymphoma ascites | Anti-tumor activity | [42] |
| 39 | Silver NPs | HepG2 cells | Non-cytotoxic doses induced p38 MAPK pathway activation and led to the promotion of HepG2 cell proliferation | [43] |
| 40 | Silver NPs | HaCaT cells | HaCaT cells were found to be resistant | [44] |
| 41 | Silver NPs | HeLa cells | HeLa cells were found to be more sensitive | [44] |
| 42 | Silver NPs | Embryonic neural stem cells | Ag-NPs-induced neurotoxicity | [45] |
| 43 | Silver NPs | Primary mixed neural cell cultures | Strong effects of SNP associated with calcium dysregulation and ROS formation in primary neural cells | [46] |
| 44 | Silver NPs | Mouse brain neural cells | AgNPs could alter gene and protein expressions of β-amyloid (Aβ) deposition | [47] |
| 45 | Silver NPs | Human embryonic neural precursor Cell | AgNPs exposure causes a significant stress response in the growing Human neural progenitor cells (hNPC) | [48] |
| 46 | Silver NPs | HT22 mouse hippocampal neuronal cells | AgNPs modulated HT22 cell cycle, proliferation, induced oxidative stress, and 53BP1 recruitment | [49] |
| Type of Material | Model | Reference |
|---|---|---|
| ZnO-NPs | Human skin and rat liver cells | [111] |
| ZnO-NPs | Skin tissue/cellular architecture | [112] |
| ZnO-NPs | Skin | [113] |
| ZnO-NPs | Blood cells of zebrafish; roots and shoots of Arabidopsis plants | [114] |
| ZnO-NPs | Plants tissues cell implosion | [115] |
| ZnO Nanocrystals | KB cells | [116] |
| ZnO@silica-NPs | Hela cells | [117] |
| CdSe(S)/ZnO-QDs | S. oneidensis | [118] |
| ZnO/Au@PEG-NPs | B16F10 cells | [119] |
| 1 | Highly stable and able to bind antigens with nanomolar affinity |
| 2 | High target specificity and lower inherent toxicity |
| 3 | It can be humanized |
| 4 | Combine the advantage of conventional antibodies with essential features of small molecule drugs |
| 5 | Able to address therapeutic targets not easily recognized by conventional antibodies (e.g., the active site of enzyme) |
| 6 | Administrated by routes other than intravenous administration |
| 7 | Produced cost-effectively on a large scale |
| 8 | Extremely lower immunogenic potential |
| 9 | Ability to cross the human blood–brain barrier to reach targets in the brain |
| Area | Nanoparticle Type | Major In Vivo Applications | Significant Characteristics |
|---|---|---|---|
| Optical imaging | Quantum dots | Site-specific imaging invivo | Imaging of lymph nodes, lung blood vessels, and tumors. Greater intensity and resistance to photobleaching compared with conventional methods. Site-specific targeting via surface functionalization. Subcutaneous imaging without surgical incisions. |
| MRI | Superparamagnetic iron oxide NPs | Cancer detection | Enhanced contrast for imaging the liver, lymph nodes, and bone marrow. Paramagnetic properties can alter magnetic resonance relaxation times of selected regions or fluids in vivo. |
| Drug and gene delivery | Polymer- and liposome-based NPs | Cancer therapy | Targeted delivery by surface functionalization. Strategies for prolonging residence times in vivo (e.g., PEG attachment). Strategies for solubilizing water-insoluble drugs (e.g., paclitaxel). Multi-layer and multi-functional (e.g., chemotherapeutic and anti-angiogenic). |
| Neurodegenerative disease therapy | Transport across the blood–brain barrier (e.g., by PEG incorporation). Superior to direct drug administration. Therapies for diseases unresponsive to small molecule drugs (gene therapy). | ||
| HIV/AIDS therapy | Solubilizing water-insoluble drugs by emulsification. Ability to transfect cells by DNA incorporation in the NP. | ||
| Ocular disease therapy | Ability to prolong drug residence times within the ocular mucus layer or retina. Alternative to the frequent application of high-drug concentration drops. | ||
| Respiratory disease therapy | Mitigation of inflammatory responses in the respiratory tract. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joseph, T.M.; Kar Mahapatra, D.; Esmaeili, A.; Piszczyk, Ł.; Hasanin, M.S.; Kattali, M.; Haponiuk, J.; Thomas, S. Nanoparticles: Taking a Unique Position in Medicine. Nanomaterials 2023, 13, 574. https://doi.org/10.3390/nano13030574
Joseph TM, Kar Mahapatra D, Esmaeili A, Piszczyk Ł, Hasanin MS, Kattali M, Haponiuk J, Thomas S. Nanoparticles: Taking a Unique Position in Medicine. Nanomaterials. 2023; 13(3):574. https://doi.org/10.3390/nano13030574
Chicago/Turabian StyleJoseph, Tomy Muringayil, Debarshi Kar Mahapatra, Amin Esmaeili, Łukasz Piszczyk, Mohamed S. Hasanin, Mashhoor Kattali, Józef Haponiuk, and Sabu Thomas. 2023. "Nanoparticles: Taking a Unique Position in Medicine" Nanomaterials 13, no. 3: 574. https://doi.org/10.3390/nano13030574
APA StyleJoseph, T. M., Kar Mahapatra, D., Esmaeili, A., Piszczyk, Ł., Hasanin, M. S., Kattali, M., Haponiuk, J., & Thomas, S. (2023). Nanoparticles: Taking a Unique Position in Medicine. Nanomaterials, 13(3), 574. https://doi.org/10.3390/nano13030574